Key Points
-
First epidemiological paper to assess the prevalence of two types of dental neglect (DN) (neglect of dental prevention and of dental treatment) for adolescents in a deprived inner city setting.
-
May open debate among dental health professionals about the recognition of DN prevalence among young people in the UK and that failure to obtain dental treatment for children in the UK could amount to DN.
Abstract
Objective To assess the prevalence of two types of dental neglect (DN) for adolescents attending secondary schools in a deprived inner city area: neglect of the prevention of oral disease (DPN) and neglect of dental treatment (DTN).
Design This study used cross-sectional data from Phase III of the research with East London adolescents community health survey (RELACHS); a longitudinal school-based epidemiological study that followed up a representative random sample of pupils in 29 secondary schools across three boroughs of inner North East London. Participants were clinically examined and answered a supervised questionnaire. DN was assessed in relation to DPN (measured by reference to experience of dental conditions and/or dental pain) and DTN (measured by reference to experience of at least one untreated dental condition and/or dental pain). Dental conditions included dental caries and traumatic dental injuries.
Results Four in ten adolescents in the study experienced DPN and five in ten experienced DTN. Adolescents with special educational needs without a statement, refugee and those 'looked after' by a local authority experienced a higher proportion of both types of DN.
Conclusions In an inner city deprived area, the proportion of adolescents with DN (either DPN or DTN) was of significance. Refugee adolescents and looked after children may be more at risk of DN.
Similar content being viewed by others
Introduction
The neglect of young people's health has received little public attention until relatively recently. Dental neglect (DN) is a form of medical neglect, which constitutes one aspect of child and adolescent neglect. DN has been described as parental failure to seek and follow through the dental treatment required to maintain a child's oral health so as to ensure adequate function and freedom from pain and infection.1 Similarly, the National Institute of Clinical Excellence in the UK (NICE) considers a (child) to be neglected 'if parents or carers have access to, but persistently fail to obtain, National Health System (NHS) treatment for their child's dental caries (tooth decay)'.2 The prevalence of neglected dental disease in children is of major concern around the world. In the UK, the prevalence of untreated dental caries among children and adolescents is high.3 Similarly, in the US, among parents reporting their children's unmet medical needs, 57% reported unmet dental needs – nearly five times the number reporting the need for glasses for optical conditions.4 Previous studies have also reported a high prevalence of traumatic dental injuries (TDIs) needing treatment, ranging from 12-85% in populations of children studied.5,6,7 Traditionally, the neglect of health has been found to be related to deprivation and poverty:8,9 In the UK, it is estimated that 95% of children and adolescents on child protection registers come from families living below the poverty line.10 Similarly, a number of dental studies have shown well-documented socio-economic and ethnic differences in dental health,3,11,12 with some suggesting that these differences are greater for untreated dental diseases than for the total dental disease experience. Previous research13,14,15 into dental neglect has focused on the concept of 'dental avoidance' and the development of scales to assess behaviours and/or attitudes related to the undervaluing of the importance of oral health which, in turn, has been found to predict poor oral health in children and adults.
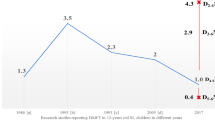
Traditionally, most definitions of DN have focused exclusively on unmet treatment needs and little attention has been given to both the need for promotion of oral health and the primary prevention of dental disease. This study aims to report the prevalence of two types of DN (DPN and DTN) as defined by clinical indicators of poor oral health and a measure of adolescents' oral-health-related impact among adolescents attending secondary schools in a deprived inner city area. This study followed a holistic perspective of oral health, involving both dental prevention neglect (DPN) – defined as the neglect of the prevention of oral disease which results in the experience of dental conditions (measured by treated and untreated dental caries and/or TDIs and/or dental pain); and dental treatment neglect (DTN) – defined as the neglect of necessary dental treatment that results in the experience of untreated dental caries and/or TDIs and/or dental pain (Fig. 1).
Methods
Study design
The present study used cross-sectional data from Phase III of the research with East London adolescents community health survey (RELACHS). RELACHS is a longitudinal school-based epidemiological study that followed up a representative random sample of pupils in secondary schools across North East London. The pupils were 11-12 years old in 2001 (Phase I), 13-14 years old in 2003 (Phase II) and 15-16 years old in 2005 (Phase III). Ethical approval was obtained from the East London and City Local Research Ethics Committee. Written informed consent was sought from each school's head teacher and from each adolescent (who signed a consent form): parents were fully informed about the study and given the opportunity to opt out. The minimum required sample size for the assessment of DPN and DTN was estimated to be 330 and 398 adolescents respectively. Both sample sizes were calculated on the basis of achieving a statistical power of 80% when demonstrating a statistically significant difference at the level of 5%, if an odds ratio of 2.00 or more was observed using the EPI INFO computer package. Previous studies5,16 were used to estimate the minimum prevalence of DPN and DTN (40% and 30% in the exposed group respectively).
Setting
Inner North East London is characterised by high unemployment rates, low levels of education and poor housing, and presents the highest child poverty rate in the UK.17
Recruitment
Pupils were selected using stratified two-stage cluster sampling in 2001. All 42 eligible schools were stratified by borough and school type (comprehensive, voluntary, others). Thirty schools were randomly selected and balanced to ensure representation from both single-sex and co-educational schools. In each of the 28 schools that agreed to participate, two representative mixed-ability classes from Year 7 were selected.
Data collection
DPN was indicated by the experience of at least one dental condition and/or dental pain; and DTN by the presence of at least one untreated dental condition and/or experience of dental pain. Dental conditions included dental caries experience and TDIs.
Data collection was performed in school classrooms and included an oral examination and the adolescent's supervised answers to a self-completed questionnaire. Two trained and calibrated examiners (GS, PE) carried out the oral clinical examinations on participants seated in an adjustable chair, using a no. 4 plain mouth mirror and blunt probe, illuminated by a Daray X100 inspection lamp. Participants' teeth were not brushed or professionally cleaned before examination. Diagnosis of tooth condition was visual and no radiographs were taken. Dental caries was recorded by tooth, following WHO criteria.18 TDIs were recorded according to the classification described by Glendor et al. (2006)19, which is similar to the one proposed by Ellis and Davey.18 Clinical examinations were duplicated in 50 adolescents to test for reliability.
Data analysis
Borough weights were applied in order to preserve the representativeness of the sample from the study population of schoolchildren (15-16 years old) attending mainstream secondary schools in the three boroughs of inner North East London.
The validity of the composite outcomes (DPN, DTN) was not compromised by inconvenience. For the purposes of this analysis, we included the following socio-demographic information: gender, borough of residence, special educational needs (SEN) status (obtained from school records), being a looked after child (LAC) (self-reported), refugee status and eligibility for free school meals (FSMs) (obtained from school records). The questions relating to dentistry included the timing of their last visit to the dentist and experience of dental pain.
Results
The cross-sectional response rate for Phase III of longitudinal RELACHS was 71% (n = 1,030). The analysis of DPN included all adolescents with complete dental-related information (dental clinical data, and answers regarding experience of dental pain and last dental visit) (n = 965). The weighted sample consisted of 309 adolescents attending secondary schools in Tower Hamlets, 468 in Newham and 188 in Hackney. The analysis of DTN included only participants who had prior experience of dental conditions, as DTN is only relevant for participants with disease experience (n = 397).
Intra-examiner agreement was good, and ranged from 0.79 to 0.87 for dental caries and from 0.87 to 0.91 for TDIs. Inter-examiner agreement was 0.80 for both conditions.
The prevalence of DPN and DTN was 41.0% and 45.1% respectively. As the two types of DN overlap, some adolescents in the study experienced both DPN and DTN.
Although the three boroughs of inner north east London (Hackney, Newham and Tower Hamlets) are very different in terms of socio-cultural profile, all are deprived and there was no significant difference between the three boroughs in the experience of either DPN or DTN for the adolescents in the study (Tables 1 and 2).
Dental prevention neglect (DPN)
Boys and girls did not differ significantly in the proportion of DPN experience (Table 1). A significantly higher proportion of adolescents with SEN but without statements experienced DPN (OR 1.59 [1.02, 2.48]) compared to adolescents without SEN status (Table 1).
In the sample, 32 out of 965 adolescents were living in care or without a parent (either biological or step-parent) or other family member and were regarded as 'looked after' children (LAC). One in two LAC in the study was found to experience DPN: 51.7% of them experienced dental caries, 10% TDIs and 12.5% dental pain (Table 1, Fig. 2).
Another vulnerable group, refugee adolescents, was twice as likely to experience DPN compared to their counterparts (OR 2.11 [1.03, 4.33]). Conversely, although more adolescents eligible for FSMs (44.4%) experienced DPN compared to adolescents who were not eligible (37.8%), this difference was of marginal statistical significance (Table 1).
Dental treatment neglect (DTN)
In the sub-sample of 397 adolescents with experience of dental conditions, 45.1% of them had DTN. The vast majority of adolescents who had not visited the dentist within the last year experienced DTN. Specifically, adolescents who had last been to the dentist over a year ago were more than four times as likely to experience DTN compared to those who were dental attendees within the last year (OR 4.20 [2.41, 8.10]) (Table 2).
As with DPN, a higher proportion of LAC (64.7%) and refugee adolescents (58.3%) experienced DTN compared to adolescents living with their families (44.2%) and non-refugee adolescents (44.9%). However, FSM eligibility was not a discriminating factor in explaining the experience of DTN among adolescents in the sample as almost similar proportions of adolescents with or without FSM eligibility experienced DTN (Table 2).
Lastly, by using a detailed description of the adolescent's last dental attendance pattern, we found that one in three adolescents who had been to the dentist within the last month still experienced DTN (Table 3).
Discussion
To our knowledge, this is the first study that has looked at two types of DN (DPN, DTN) as measured by clinical indicators and impact on oral health-related impact and considered any oral health outcomes for LAC, who are known to be a vulnerable group. The sample was composed of a large representative group of adolescents attending secondary mainstream schools in a deprived and multicultural area of inner North East London.
We found that four out of ten adolescents in the sample experienced DPN and five out of ten DTN. For the sample of adolescents who lived in a deprived and multicultural area, the following groups had a higher risk of experiencing DPN: those who had SEN but were without statements; refugees; or those who were LAC. A higher proportion of refugee and LAC adolescents were also found to experience DTN than their counterparts. Family deprivation, as measured by eligibility for FSMs was only marginally related to DPN but not to DTN.
We are not aware of any previous research that has looked comprehensively at the experience of DN among young people, so no comparative data was found regarding these outcomes (DPN and DTN). The proportion of adolescents with DPN (41.0%) was lower than the prevalence of dental caries experience in 15-year-olds in inner London (58%),3 whereas the frequency of DTN (45.1%) was higher than that of untreated dental caries (32%)3 and dental pain (20%)3 in UK adolescents. Adolescents in the study may have experienced untreated TDIs and/or dental pain while having been free of untreated dental caries.
This study revealed that adolescents who had SEN without statements were at a significantly higher risk of experiencing DPN compared to adolescents without SEN. This finding accords with previous studies20,21 that showed that the poor oral health of young people with learning disabilities has been attributed more to their poor dietary and oral health behavioural habits than to the status of their learning disabilities.22 The nature of the process for obtaining a statement of SEN for children in the UK23 may explain these results to some extent and it may be confounded by other socio-demographic factors, such as parental educational status and area of residence.24 A higher proportion of vulnerable adolescents, such as refugee adolescents and LAC were found to experience both DPN and DTN compared to their counterparts. Refugee adolescents in this study were at a significantly higher risk of experiencing DPN, which accords with previous research. However, the proportion of refugee adolescents with DPN (58.4%) was lower than the proportion of refugee children in Holland with a history of dental caries25 (85%), of newly arriving refugee children with significant oral health problems in Massachusetts26 (64%) and of migrant children needing dental care in Los Angeles27 (81%).
To our knowledge, no data exist in relation to the oral health of LAC in the UK, although authors28,29,30,31,32,33 have previously found that LAC have unmet physical and mental needs, including dental needs. One in five (20%) children on the English child protection registers in 2001 was LAC by local authorities34 and their oral health has been overlooked: they were not included in the UK or BASCD children's dental health or local surveys. The only information related to LAC's oral health in the UK was that 89% of them had received a dental check as a part of general health assessment.35
Eligibility status for FSMs was only marginally significantly related to DPN and not related to DTN. This may have been due to the character of our sample, namely that the children came from a uniformly deprived background. The inclusion of a group of affluent adolescents (affluence being defined by socio-economic indicators such as family income), or the use of a more detailed parental socio-economic classification, may further elucidate whether there is a bipolar or a social gradient in the association between socio-economic status and adolescents' DN.
There are two potential weaknesses in this study. Firstly, the cross-sectional study design adopted did not enable causality to be established. Secondly, assessment of two other dental conditions (dental erosion and orthodontic treatment needs) together with an oral health quality of life measure of adolescents' perceived need for dental treatment would ideally provide additional information about adolescents' experience of DN.
Conclusions
To conclude, what are the implications of recognising DN as a clinical outcome for children and young people? Recently, DN has been recognised internationally as a new area of oral health concern. As a first step, the recognition of DN in young people places their fundamental right to an optimum level of oral health onto the public health agenda. Further, it may offer a better framework for addressing the underlying social determinants of dental conditions and may avoid the unnecessary dissipation of resources associated with research and interventions, which are tailored to addressing different aspects of the neglect of oral health. Testing the relative impact of both prevention and treatment of neglected dental conditions for children and young people has theoretical as well as clinical importance: each type of DN has direct policy implications for the design of preventive or therapeutic dental interventions, especially for adolescents living in a deprived and multicultural environment. Adolescents have already been recognised as a vulnerable group in terms of their tendency to experience neglect.36 They have distinct dental needs due to a potentially high rate of caries, increased risk of TDIs, a tendency towards poor nutritional habits and the initiation of tobacco use, eating disorders as well as unique social and psychological needs.37,38,39 Public dental health interventions to address DN may be more relevant for deprived adolescents whose dental needs are at greater risk of neglect than for adolescents across the population as a whole. Finally, as DN may overlap with other types of child neglect, resources could be more efficiently allocated.
Although this descriptive study provides some interesting information in an area of research that is becoming highly relevant, further research is necessary to address questions which have not been answered here.
References
American Academy of Pediatric Dentistry. Guideline on adolescent oral health care. Pediatr Den 2005–2006; 27(7 Suppl): 72–79.
National Institute of Clinical Excellence. When to suspect child maltreatment. Clinical guideline 89. London: NICE, 2009.
Office for National Statistics. National Children's Dental Health Survey 2003. London: ONS, 2004.
Edelstein B L . Disparities in oral health and access to care: findings of national surveys. Ambul Pediatr 2002; 2: 141–147.
Marcenes W, Murray S . Social deprivation and traumatic dental injuries among 14-year-old schoolchildren in Newham, London. Dent Traumatol 2001; 17: 17–21.
Hamilton F A, Hill F J, Holloway P J . An investigation of dento-alveolar trauma and its treatment in an adolescent population. Part 1: the prevalence and incidence of injuries and the extent and adequacy of treatment received. Br Dent J 1997; 182: 91–95.
Hunter M L, Hunter B, Kingdon M, Addy M, Dummer P M, Shaw W C . Traumatic injury to maxillary incisor teeth in a group of South Wales school children. Endod Dent Traumatol 1990; 6: 260–264.
Belsky J . The determinants of parenting: a process model. Child Dev 1984; 55: 83–96.
Bradshaw J . Child poverty: comparison of industrial and transition economics. In Hutton S, Redmond R. (eds) Poverty in transition economies. pp 191–207. London: Routledge, 2000.
Department of Health. Child protection: messages from research. London: HMSO, 1995.
Pitts N B, Boyles J, Nugent Z J, Thomas N, Pine C M . The dental caries experience of 5-year-old children in England and Wales. Surveys coordinated by the British Association for the Study of Community Dentistry in 2001/2002. Community Dent Health 2003; 20: 45–54.
Edelstein B L, Chinn C H . Update on disparities in oral health and access to dental care for America's children. Acad Pediatr 2009; 9: 415–419.
Coolidge T, Heima M, Johnson E K, Weinstein P . The Dental Neglect Scale in adolescents. BMC Oral Health 2009; 9: 2.
Thomson W M, Spencer A J, Gaughwin A . Testing a child dental neglect scale in South Australia. Community Dent Oral Epidemiol 1996; 24: 351–356.
Skaret E, Raadal M, Berg E, Kvale G . Dental anxiety and dental avoidance among 12 to 18 year olds in Norway. Eur J Oral Sci 1999; 107: 422–428.
Pitts N B, Boyles J, Nugent Z J, Thomas N, Pine C M . BASCD Survey Report: The dental caries experience of 14-year-old children in England and Wales. Surveys coordinated by the British Association for the Study of Dentistry in 2002/2003. Community Dent Health 2004; 21: 45–57.
Office of the Deputy Prime Minister. The English Indices of Deprivation 2004 (revised). London: Office of the Deputy Prime Minister, 2004.
World Health Organization. Oral health surveys: basic methods. 4th ed. Geneva: WHO, 1997.
Glendor U, Marcenes W, JO. Andreasen (2007). Classification, Epidemiology and Etiology of Traumatic Dental Injuries. In: Textbook and Color Atlas of Traumatic Injuries to the Teeth. 4th edition. Blackwell Munksgaard.
Mitsea A G, Karidis A G, Donta-Bakoyianni C, Spyropoulos N D . Oral health status in Greek children and teenagers, with disabilities. J Clin Pediatr Dent 2001; 26: 111–118.
Dicks J L . Outpatient dental services for individuals with mental illness: a program description. Spec Care Dentist 1995; 15: 239–242.
Gabre P, Ganhnberg L . Dental health status of mentally retarded adults with various living arrangements. Spec Care Dentist 1994; 14: 203–207.
Special Educational Needs and Disability Act, 2001. London: Crown Copyright, 2001. Online Act available at http://www.equalityhumanrights.com/uploaded_files/special_educational_needs_and_disability_act_2001.pdf (accessed October 2012).
Office for National Statistics. Special educational needs in England 2005. London: ONS, 2005.
Kalsbeek H, Zijlstra-Remon N, Filedt Kok-Weimar T L . Oral health and dental care in refugee children. Ned Tijdschr Tandheelkd 2001; 108: 404–407.
Geltman P L, Radin M, Zhang Z, Cochran J, Meyers A F . Growth status and related medical conditions among refugee children in Massachusetts, 1995–1998. Am J Public Health 2001; 91: 1800–1805.
Mulligan R, Seirawan H, Faust S, Barzaga C . Dental caries in underprivileged children of Los Angeles. J Health Care Poor Undeserved 2011; 22: 648–662.
Mather M, Humphrey J, Robson J . The statutory medical and health needs of looked after children: time for a radical review? Adoption and Fostering 1997; 21: 36–40.
Polnay, L, Cawthron, P, Coutts J et al. Report of programme team for health needs of young people in residential care 1992–1997. Nottingham: Nottingham Community Health NHS Trust, Nottingham HealthCare NHS Trust, University of Nottingham and Nottinghamshire County Council Social Services, 1997.
Brodie I, Berridge, D, Beckett W . The health of children looked after by local authorities. Br J Nurs 1997; 6: 386–390.
Mather M . Adoption: a forgotten paediatric speciality. Arch Dis Child 1999; 81: 492–495.
McCann J B, James A, Wilson S, Dunn G . Prevalence of psychiatric disorders in young people in the care system. BMJ 1996; 313: 1529–1530.
Rodrigues V C . Health of children looked after by the local authorities. Public Health 2004; 118: 370–376.
Department of Health. Children and young people on child protection registers 2000-01. London: DH, 2001.
Department for Children, Schools and Families. DCSF: outcome indicators for children looked after, twelve months to 30 September 2007. England: DCSF 2008. Online article available at http://www.education.gov.uk/rsgateway/DB/SFR/s000785/index.shtml (accessed October 2012).
National Society of Prevention of Cruelty against Children (NSPCC). Child Protection Research Brief: child neglect. UK: NSPCC, 2007.
Macgregor I D, Regis D, Balding J . Self concept and dental health behaviours in adolescents. J Clin Periodontol 1997; 24: 335–339.
Yu S M, Bellamy H A, Kogan M D, Dunbar J L, Schwalberg R H, Schuster M A . Factors that influence receipt of recommended preventive pediatric health and dental care. Pediatrics 2002; 110: e73.
American Academy of Pediatric Dentistry. Guideline on adolescent oral health care. US: AAPD, 2010.
Acknowledgements
The RELACHS study was commissioned by the East London and City Health Authority to inform the Health Action Zone (http://www.wolfson.qmul.ac.uk/relachs/). We are grateful for the support of the schools, parents and students involved in this study. We also thank the RELACHS field research team (http://www.wolfson.qmul.ac.uk/relachs/).
This study was part of Dr Sarri's research for the completion of her doctorate at the Institute of Dentistry, Barts and The London, Queen Mary University of London. The views expressed in this publication are those of the authors and not those of the Royal College of Physicians.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Sarri, G., Evans, P., Stansfeld, S. et al. A school-based epidemiological study of dental neglect among adolescents in a deprived area of the UK. Br Dent J 213, E17 (2012). https://doi.org/10.1038/sj.bdj.2012.1042
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2012.1042
This article is cited by
-
Looked after children: an overview for the dental team
BDJ Team (2023)
-
Looked after children: an overview for the dental team
British Dental Journal (2023)
-
An exploratory study investigating the barriers to reporting child dental neglect concerns among general medical practitioners in Greater Manchester
British Dental Journal (2022)
-
Cost-effectiveness Analysis of the Dental RECUR Pragmatic Randomized Controlled Trial: Evaluating a Goal-oriented Talking Intervention to Prevent Reoccurrence of Dental Caries in Children
Applied Health Economics and Health Policy (2022)
-
The development of a designated dental pathway for looked after children
British Dental Journal (2014)