Abstract
Introduction Very little is known about the burden of childhood oral diseases in protracted humanitarian settings.
Aim This study aimed to assess the prevalence of oral diseases in Syrian refugee children living in Lebanon and to investigate their relationship with the duration of displacement.
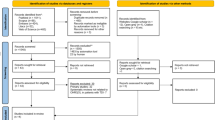
Methods Data from Miles for Smiles programme for Syrian refugee schoolchildren in Bekaa/Lebanon were used (n = 823). A dental examination was performed to assess the presence of dental caries and abscess. A clinical form was used to collect data on the presence, intensity and duration of dental pain.
Results The majority (90%) had dental caries, 57% had dental pain (of which 55% had moderate/severe pain and 38% had pain for more than a month) and 9% had dental abscess. After adjusting for age and gender, children in protracted displacement were significantly more likely to have a higher number of decayed teeth compared to their counterparts who had been displaced for less than five years (RR = 1.19; 95% CI = 1.09-1.29; P <0.001).
Conclusions The burden of oral diseases in Syrian refugee children living in Lebanon was high, particularly among those living in a protracted situation. There is a need for evidence-based effective public health interventions to improve this population's oral health.
Key points
-
The burden of oral diseases in protracted humanitarian settings is high. Nearly 90% of Syrian refugee children living in informal settlements in Bekaa, Lebanon had untreated dental caries and 57% had dental pain.
-
Children in a protracted displacement situation were significantly more likely to have a higher number of decayed teeth compared to their counterparts who had been displaced for less than five years.
-
There is a need for evidence-based effective public health interventions to improve this population's oral health.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 24 print issues and online access
$259.00 per year
only $10.79 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
The World Bank. Fragility, conflict and violence overview. 2018. Available at https://www.worldbank.org/en/topic/fragilityconflictviolence/overview (accessed April 2021).
The UN Refugee Agency. Global trends: Forced displacement in 2019. Geneva: United Nations High Commissioner for Refugees, 2020.
Ay M, Arcos G P, Castro D R. The Perceived Barriers of Access to Health Care Among a Group of Non-camp Syrian Refugees in Jordan. Int J Health Serv 2016; 46: 566-589.
Hermans M P J, Kooistra J, Cannegieter S C, Rosendaal F R, Mook-Kanamori D O, Nemeth B. Healthcare and disease burden among refugees in long-stay refugee camps at Lesbos, Greece. Eur J Epidemiol 2017; 32: 851-854.
Johnston V, Smith L, Roydhouse H. The health of newly arrived refugees to the Top End of Australia: results of a clinical audit at the Darwin Refugee Health Service. Aust J Prim Health 2012; 18: 242-247.
Van Berlaer G, Bohle Carbonell F, Manantsoa S et al. A refugee camp in the centre of Europe: clinical characteristics of asylum seekers arriving in Brussels. BMJ Open 2016; DOI: 10.1136/bmjopen-2016-013963.
Almerich-Silla J M, Montiel-Company J M, Ruiz-Miravet A. Caries and dental fluorosis in a western Saharan population of refugee children. Eur J Oral Sci 2008; 116: 512-517.
Beltrán E, Cherrett H, Hobdell M, Jaramillo F, Robison V. Tanzania Site Assessments: Refugee Camps. 2006. Available at https://www.cdc.gov/oralhealth/publications/library/pdf/tanzania_site_assessments.pdf (accessed April 2021).
Cassar C, Sigger G. The health of unaccompanied minors in the UK: trends, needs and ways forward. Arch Dis Child 2016; 101: A2-A3.
Cote S, Geltman P, Nunn M, Lituri K, Henshaw M, Garcia R I. Dental caries of refugee children compared with US children. Pediatrics 2004; DOI: 10.1542/peds.2004-0496.
Geltman P L, Radin M, Zhang Z, Cochran J, Meyers A F. Growth status and related medical conditions among refugee children in Massachusetts, 1995-1998. Am J Public Health 2001; 91: 1800-1805.
Mutch R C, Cherian S, Nemba K et al. Tertiary paediatric refugee health clinic in Western Australia: analysis of the first 1026 children. J Paediatr Child Health 2012; 48: 582-587.
Nicol P, Anthonappa R, King N, Slack-Smith L, Cirillo G, Cherian S. Caries burden and efficacy of a referral pathway in a cohort of preschool refugee children. Aust Dent J 2015; 60: 73-79.
Shah A Y, Suchdev P S, Mitchell T et al. Nutritional status of refugee children entering DeKalb County, Georgia. J Immigr Minor Health 2014; 16: 959-967.
Benzian H, Bergman M, Cohen L K, Hobdell M, Mackay J. The UN High-level Meeting on Prevention and Control of Non-communicable Diseases and its significance for oral health worldwide. J Public Health Dent 2012; 72: 91-93.
Kassebaum N J, Bernabé E, Dahiya M, Bhandari B, Murray C J, Marcenes W. Global burden of untreated caries: a systematic review and metaregression. J Dent Res 2015; 94: 650-658.
World Health Organisation. Oral health surveys: basic methods. 5th ed. 2013. Available online at https://www.who.int/oral_health/publications/9789241548649/en/ (accessed April 2021).
Cote C J, Lerman J, Anderson B. A practice of anaesthesia for infants and children. 5th ed. London: Elsevier Health Sciences, 2013.
Garra G, Singer A J, Taira B R et al. Validation of the Wong-Baker F A C ES Pain Rating Scale in Paediatric Emergency Department Patients. Acad Emerg Med 2010; 17: 50-54.
World Health Organisation. Health of refugee and migrant children: Technical guidance. 2018. Available at https://www.euro.who.int/__data/assets/pdf_file/0011/388361/tc-health-children-eng.pdf (accessed April 2021).
Ballouk M A, Dashash M. Caries prevalence and dental health of 8-12-year-old children in Damascus city in Syria during the Syrian Crisis; a cross-sectional epidemiological oral health survey. BMC Oral Health 2019; 19: 16.
Pani S C, Al-Sibai S A, Rao A S, Kazimoglu S N, Mosadomi H A. Parental perceptions of the oral health-related quality of life of Syrian refugee children. J Int Soc Prev Community Dent 2017; 7: 191-196.
Nicol P, Al-Hanbali A, King N, Slack-Smith L, Cherian S. Informing a culturally appropriate approach to oral health and dental care for pre-school refugee children: a community participatory study. BMC Oral Health 2014; 14: 69.
Prowse S, Schroth R J, Wilson A et al. Diversity considerations for promoting early childhood oral health: a pilot study. Int J Dent 2014; 2014: 175084.
Riggs E, Davis E, Gibbs L et al. Accessing maternal and child health services in Melbourne, Australia: reflections from refugee families and service providers. BMC Health Serv Res 2012; 12: 117.
Riggs E, Gibbs L, Kilpatrick N et al. Breaking down the barriers: a qualitative study to understand child oral health in refugee and migrant communities in Australia. Ethn Health 2015; 20: 241-257.
Operational Portal: Refugee Situations. Research project proposal application - Oral Health Survey of Child Refugees. 2017. Available at https://data2.unhcr.org/en/needs-assessment/1276 (accessed April 2021).
EMPHNET. EMPHNET and UNICEF complete integrated school health project in Syrian refugee camps in Jordan. 2017. Available at http://emphnet.net/en/media-center/news/2017/emphnet-and-unicef-complete-integrated-school-health-project-in-syrian-refugee-camps-in-jordan/ (accessed April 2021).
Ogunbodede E O, Mickenautsch S, Rudolph M J. Oral health care in refugee situations: Liberian refugees in Ghana. J Refug Stud 2000; 13: 328-335.
Roucka T M. Access to dental care in two long-term refugee camps in western Tanzania; programme development and assessment. Int Dent J 2011; 61: 109-115.
Htoon H M, Mickenautsch S. Oral Health Care in Camps for Refugees and Displaced Persons. 2000. Available at https://apps.who.int/iris/bitstream/handle/10665/66506/WHO_NMH_MNC_ORH_00.1.pdf (accessed April 2021).
World Dental Federation. Dentists can help provide oral healthcare for displaced persons from their own communities. 2017. Available online at https://www.fdiworlddental.org/latest-news (accessed April 2021).
Saltaji H, Alfakir H, Shibly O. Oral health guidelines in humanitarian settings. Br Dent J 2016; 220: 2.
Tyrer R A, Fazel M. School and community-based interventions for refugee and asylum-seeking children: a systematic review. PLoS One 2014; DOI: 10.1371/journal.pone.0089359.
Acknowledgements
The authors express their gratitude to all Syrian children and parents/guardians who participated in Global Miles for Smiles. Also, the authors thank all staff and students from the University at Buffalo and Saint Joseph University of Beirut who participated in Global Miles for Smiles and Dr Bahaa Alhafar. Many thanks to Henry Schein Cares Foundation for providing the materials.
Author information
Authors and Affiliations
Contributions
EJ conceived the manuscript, planned and conducted data analysis and interpretation, drafted the whole manuscript and critically revised the manuscript for important intellectual content. RM contributed to data acquisition and clinical forms review. JCAC contributed to examiners' training and data acquisition. OS is the director of Global Miles for Smiles programme. He designed and led the oral health needs assessment and data acquisition, and critically revised the manuscript for important intellectual content. All authors approved the final version submitted for publication.
Corresponding author
Ethics declarations
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Joury, E., Meer, R., Chedid, J. et al. Burden of oral diseases and impact of protracted displacement: a cross-sectional study on Syrian refugee children in Lebanon. Br Dent J (2021). https://doi.org/10.1038/s41415-021-2960-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-021-2960-9