Abstract
Study design:
Observational population-based cohort study.
Objectives:
The main aim of this study was to examine the relative effect of hereditary spastic paraplegia (HSP) on the health-related quality of life (HRQoL).
Methods:
HRQoL was evaluated using a RAND 36-Item Health Survey 1.0 questionnaire. Fifty-eight patients received a questionnaire through mail and signed an informed consent. The results for the control group were obtained from the RAND-36 data collected in 2004 in the European Social Survey. R2.9.0 and Statistica 6.1 were used to analyze the RAND-36 data.
Setting:
The study was performed in Estonia, a country with a population of 1.3 million.
Results:
Completed questionnaires were received from 49 participants (response rate was 84.5%). The control group consisted of 549 individuals from the Estonian population. Patients with HSP had lower mean scores in all categories as compared with the control group. Six of the eight categories showed significant differences, with P<0.0001. For the vitality category, the P-value ranged from 0.000006 from 0.002, and the P-value for the mental health category ranged from 0.001 to 0.055.
Conclusions:
The HRQoL in patients with HSP was found to be significantly worse than that for the general population. The level of education might affect the HRQoL experienced by HSP patients.
Similar content being viewed by others
Introduction
Hereditary spastic paraplegia (HSP) is a chronic neurodegenerative disorder marked by clinical and genetic heterogeneity. It has been classified into two forms, ‘pure’ and ‘complex’. Purer HSP presents with spasticity and motor deficits in the legs, brisk reflexes and Babinski's signs; deep sensory impairment and sphincter disturbances are also common. For cases of complex HSP, other neurological or extra-neurological features can be present.1 Like many chronic neurological disorders, it is suspected, but has not yet been shown evidentially, that HSP affects the everyday life of the patients. Due to the disorder's clinical variability, HSP can not only affect aspects related to mobility, but also the patient's mental and emotional capacities. Correspondingly, the health-related quality of life (HRQoL) in HSP patients is probably significantly worse than that of the healthy population. Despite this, we are not aware of any published studies evaluating the HRQoL of persons with HSP. At the same time other diseases, mainly multiple sclerosis (MS) and spinal cord injury (SCI), which can be clinically very similar to HSP, have been investigated. These are non-fatal disorders that can extend over many years and often involve spastic paraparesis with or without additional neurological features. Furthermore, the degree of paresis can vary considerably in all of the above-mentioned conditions. Studies evaluating HRQoL in MS and SCI showed a deterioration of patients’ HRQoL for most of the categories evaluated, with physical health being particularly more affected.2, 3 Westgren and Levi4 found that the HRQoL in individuals with SCI was significantly lower in all subscales as compared with a normative population. Whiteneck et al.5 studied a large group of people with SCI to determine the relative impact of their reported environmental barriers, demographic and injury-related characteristics, and activity limitations in predicting variation in participation and life satisfaction, which is a subjective component of HRQoL. They found that environmental factors did not have a major effect on participation but were major predictors of life satisfaction. Their study also supported previous research findings that life satisfaction is more strongly related to participation than to impairment or activity limitations.6
When performing HRQoL studies, several measurement tools are available. RAND-36 is a free analogous version of the Medical Outcomes Study (MOS) 36-Item-Short-Form Health Survey (SF-36).7, 8, 9 The latter one is showed to be an acceptable tool for evaluating HRQoL in SCI and, consequently, it has a promising potential for research in HSP as well.10 The RAND-36 questionnaire is probably one of the most widely used generic HRQoL instruments.11 Although the RAND version has a slightly different scoring method, it allows results from the MOS SF-36 and RAND-36 questionnaires to be compared. The design of these questionnaires (consisting of eight categories) is based on a proposed structural model of HRQoL.12 At the same time most of the studies using RAND-36 do not investigate the internal relations between the different categories within this questionnaire. However, some authors highlight discrepancies between scores on individual categories and their summaries—physical and mental health.13, 14, 15 It has been hypothesized that physical and mental health subscales are not independent, in other words, that these subscales do not have divergent validity. Specifically, mental health scores can be inflated due to poor physical health; poor mental health can increase scores on physical health by inadequate self-assessment; negatively weighted mental health subscales can offset the positive contribution of physical health categories and both summaries can have a wider-than-expected range of scores.16 A strong correlation between a pair of categories could suggest the effect of one category on another or a common variable simultaneously affecting both of the categories. Different methodological approaches can be applied to investigate the latter hypotheses. While examining the internal structure of the SF-36 using principal-component analysis, Cronbach α-coefficients and item-to-domain correlation analysis Gee et al.17 found the domain structure of the questionnaire to be robust and the discriminatory ability of the measure disappointing. Upon examining the relative effect of MS and Parkinson's disease on the HRQoL, Riazi et al. performed multiple linear regression analysis for investigating the extent to which one or more predictive variables (independent variables) predict an outcome variable (dependent variable). The authors suggested that the SF-36 mental health dimension has limited validity and it underestimates the effect of the disease on mental health.2 While looking for associations between the scores of the individual categories, Wight et al. used correlation analysis and found correlations to be present: a high correlation was found between the dimension scores. Specifically, the different physical dimensions were highly correlated with each other, as were the mental/emotional dimensions. However, correlation between physical and mental dimensions was less clear.18 The results of such analysis could help to understand better and interpret the results of an HRQoL study. Furthermore it is under-investigated whether being a patient rather than a control would coincide with a systematically lower score in any of the RAND-36 categories (regardless of the person's age, sex or education). This question can be investigated using conditional logistic regression analysis—a method more widely used in epidemiological research but not so in HRQoL research at present.
Therefore, the aims of this study were:
-
To identify differences in the health profile of HSP patients versus that of the general Estonian population,
-
To examine the relative effect of HSP on the HRQoL experienced by the HSP population in Estonia by comparing the results of the RAND-36 questionnaire19 between patient and control groups,
-
To investigate the possible associations between the RAND-36 categories in both the groups,
-
To investigate, while controlling for confounding variables (age, sex and education), how well the categories of RAND-36 differentiate between the patients and the controls.
Materials and methods
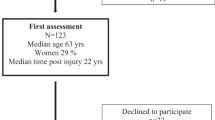
All of the total of 59 patients clinically diagnosed with HSP identified in Estonia were invited to participate in this study and signed the informed consent. Contact information was acquired from the Estonian epidemiological study database, which contains patient data collected between 2001 and 2005 using a multi-source approach.20 Of the 59 HSP cases, only one was ineligible to participate in the study due to her age (11 years) as the questionnaire is designed for persons who are 14 years and older.21 The remaining 58 available patients received a questionnaire through mail.
The HRQoL was evaluated using a RAND 36-Item Health Survey 1.0 questionnaire validated in both Estonian and Russian languages. The detailed structure and scoring of the RAND questionnaire is described elsewhere;7 however, in brief, a higher score represents better patient health. The format of the RAND-36 assesses the state of a patient's health according to eight categories:
-
PF (physical functioning)—limitations of physical functioning due to health problems
-
RP (role-physical)—limitations in usual activities due to physical health problems
-
RE (role-emotional)—limitations in usual activities due to emotional problems
-
BP (bodily pain)
-
SF (social functioning)—limitations of social functioning due to physical or emotional problems
-
GH (general health)—based on patient perception
-
VT (vitality)—energy and fatigue
-
MH (mental health)—psychological distress and well-being.
An additional category, health change, evaluates a patient's change in health over a 1-year period. This was the only category that was not compared with the control group, but rather was compared among the participants of the HSP group. The results for the control group (n=549) were obtained from the RAND-36 data collected in 2004 in the European Social Survey.22
Statistical analysis
None of the categories were distributed normally across the groups (as verified by the Shapiro–Wilk test). Therefore, the Mann–Whitney U-test was applied using Statistica 6.1 (Statsoft, 2004) to compare the mean scores for each of the eight categories between the patient and the control groups (representing two independent groups). To eliminate the effect of group magnitude differences on the results of the Mann–Whitney U-tests, a comparison was made between one patient and one randomly selected control subject matched by age and sex. To substantiate these results, this procedure of matched comparison was repeated four times with different control subjects each time.
To analyze the mutual relatedness of the RAND-36 categories, correlation coefficients were calculated between all of the categories. Due to the non-interval nature of the data, Spearman correlation coefficients were computed using Statistical Analysis Systems, version 9.1 (SAS Institute, Cary, NC, USA). To investigate the discriminability of the RAND-36 questionnaire between the groups, while controlling for potential confounding variables, conditional logistic regression was applied using the statistical software R2.9.0—A Language and Environment (The R Development Core Team, 2009). Patients (n=49) were matched to controls (n=549) on the basis of age (as a continuous variable) and sex, with 4–22 controls corresponding to each patient. Odds ratios (ORs) and their 95% confidence intervals with and without adjustment to the level of patient education were calculated using conditional logistic regression to further investigate the differences between the RAND-36 scores of the patients and the control subjects. The scores from each category were divided into 3–5 scoring intervals depending on the distribution of individual scores in a certain dimension, and so that equal proportions would be present in each scoring interval. Furthermore, if the dependency between the OR and the score increase was non-monotonic, the number of intervals was increased to five to provide more detail. In the RE category, only four levels of scores appeared in the data, and therefore, each were treated as an interval. For all analyses, statistical significance was defined as P<0.05 (two-sided).
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. This study was approved by the Ethics Review Committee on Human Research of the University of Tartu (Tartu, Estonia).
Results
A total of 58 patients with HSP were eligible to participate in the study and received a RAND-36 questionnaire. Completed questionnaires were received from 49 participants, resulting in a response rate of 84.5%. The control group consisted of 549 individuals from the Estonian population (Table 1).
Differences in mean scores
Overall, patients with HSP had lower mean scores in all eight categories evaluated by the RAND-36 questionnaire as compared with the control group. RAND-36 scores were distributed non-normally across the study groups. Therefore, for the presentation of data, the medians and extreme quartiles were chosen as more informative (Figure 1).
The PF and RP categories had the largest differences in scores between the HSP patients and the control group, whereas differences in the RE, SF, BP and GH categories also had substantial differences. The smallest differences were found between the two groups for the VT and MH categories. The magnitude of difference and the most conservative P-value from the results of the four Mann–Whitney U-tests performed for each dimension are presented in Table 2.
Six of the eight categories showed significant differences with P<0.0001. Similar results were obtained from the four matched comparisons analyzed by Mann–Whitney U-tests. For the VT category, the P-value ranged from 0.000006 to 0.002 and the P-value for the MH category ranged from 0.001 to 0.055. The average health change score for the patient group was 27.0±19.7 points, with 22.5% of the patients scoring 0, 51% of the patients scoring 25, 22.5% of the patients scoring 50 and 4% of the patients scoring 75.
Correlation analyses
Correlation coefficients were calculated between all categories for both groups. In the control group, all eight categories were associated with a positive correlation at a significance of P<0.0001. In contrast, the PF and RP categories displayed weaker, yet still significant, positive correlations with the remaining categories (Table 3).
Conditional logistic regression
Analysis of conditional logistic regression identified cases, which were less likely to score as high as the age- and sex-matched controls in any category of the RAND-36 questionnaire. For most dimensions, associations were more pronounced after adjusting for education. However, for the VT and MH categories, this association was not monotonic. The ORs for the score distributions for each of the RAND-36 categories are presented in Table 4. The OR values indicate to what extent the patient score is lower than the control score for the lowest score interval of a category. For example, the score difference between the patient and the control groups was the greatest in the PF category, where the OR for patients and controls receiving a score of 95–100 points was 633.88 times smaller relative to the OR of those receiving a score of 0–54 (95% confidence interval=79.06–5082.20). Alternatively, the smallest and the most unsystematic difference between the scoring distribution for the patient and the control groups was found for the VT and MH categories, where the ORs were 6.10 (95% confidence interval=2.38–15.62) and 4.42 (95% confidence interval=1.89–10.30), respectively, for the highest scoring interval compared with the lowest scoring interval. Furthermore, in these two categories, the patients were more likely to have a score in the highest scoring interval relative to the second-highest scoring interval. These results indicate that the subscales for the VT and MH categories are not adequate to discriminate between HSP patients and controls.
Discussion
This study compared HRQoL scores among patients with HSP versus the general Estonian population using the RAND-36 questionnaire. Responses to the questionnaire reflected the effect of HSP from the patient's perspective, as well as an estimate of the relative disease burden. As a result, the HRQoL in patients with HSP was found to be significantly worse than that for the general population in all categories, except for MH. In addition, more HSP patients than controls had completed either of the two highest levels of education. As a result, for most categories, differences between scores for the patient group versus the control group were more pronounced after adjusting for education, suggesting that the level of education might affect the HRQoL experienced by HSP patients. Specifically, persons with HSP who have achieved higher levels of education may fare better in terms of HRQoL than those with lower levels of education.
There were some differences noted in the extent of the variations detected. For example, the largest contrasts were associated with the two physical domains of the RAND-36 profile, PF and RP. Correlation analyses of the patient group data also showed that the PF and RP categories showed significant, yet weaker, positive correlations with the other categories. While these results would be predicted for the neurological involvement associated with this type of disease, it has not been shown previously for HSP. In addition, there was no statistically significant difference between the mean responses from the patient versus the control groups in the MH category, and the smallest statistically significant difference was associated with the VT category. Conditional logistic regression analysis further identified the smallest, as well as unsystematic, difference between the patient and the control groups for the VT and MH categories. Similar results for the MH category were previously described in patients with MS: Nortvedt et al.15 concluded from their study, that MH summary scales appear to overestimate mental health in patients with MS. We hypothesize that this result is related to a response shift where changes in internal standards, values and conceptualizations of health status have occurred in response to changes in health and physical function resulting from chronic disease.23 Another possible explanation is the limited validity of the questionnaire to measure mental health for all diseases, as previously speculated.2 The results could also represent the true effect of the disease where physical function is affected more significantly than the mental health of the patient. The average health change score for the patient group reflects the overall estimation of the health change experienced by HSP patients over 1 year. In this study, the patient responses reflected that a stable progression of the disease was experienced, which is consistent with the nature of HSP.
As the first study to evaluate the HRQoL in persons with HSP, a comparison with previous data is not possible. However, as the RAND-36 questionnaire is a generic measure, it is possible to compare the influence of different disorders on patients’ HRQoL. Diseases that are clinically very similar to HSP, and have been relatively well-studied regarding patient's HRQoL, include SCI and MS (mainly the primary progressive form). Especially the latter one was associated with the poorest levels of functioning among numerous neurological conditions.24 Our results are consistent with those from studies of SCI and MS patients that showed a deterioration of patients’ HRQoL for most of the categories evaluated, with physical health being particularly more affected.2, 3 Lower scores in the physical categories are expected on the basis of the nature of these neurological disorders. HRQoL studies of SCI patients have also shown different results regarding the influence of the patient's level of education. While some studies showed that there was a weak association between HRQoL and education level, other studies have found that a higher level of education was associated with higher HRQoL ratings.3, 25, 26 A proposed explanation for these observations is that more physically demanding work is typically associated with a lower level of education, and would be more difficult to manage after an SCI.3 However, this is less likely to be the case for patients with HSP as the disease does not have a sudden onset, but rather is slowly progressive.
There are limitations associated with this study. The number of patients that participated in this study is somewhat low. A larger study (possibly including patients with other similar conditions) would have been more robust for statistical analyses, and therefore, more conclusive. Also the results could not be directly compared with those of other named disorders as the same settings were not used. Therefore, we cannot directly evaluate whether HSP affects patients’ HRQoL more or less than other disorder(s). In addition, any comparisons made to other clinical situations are indirect, and not entirely conclusive.
In conclusion, the results from this study suggest the need for further research on the HRQoL experienced by HSP patients (including an assessment of healthcare needs). The information provided by this particular study and by studies still to come can help practitioners to address the needs, which would be met by persons with HSP. To ensure the reproducibility of the results presented here, future studies should include an evaluation of the eight parameters addressed by the RAND-36 questionnaire. That knowledge would also help to ascertain whether there are predictor variables that can be altered by professional care providers.
References
Depienne C, Stevanin G, Brice A, Durr A . Hereditary spastic paraplegias: an update. Curr Opin Neurol 2007; 20: 674–680.
Riazi A, Hobart JC, Lamping DL, Fitzpatrick R, Freeman JA, Jenkinson C et al. Using the SF-36 measure to compare the health impact of multiple sclerosis and Parkinson's disease with normal population health profiles. J Neurol Neurosurg Psychiatry 2003; 74: 710–714.
Ku JH . Health-related quality of life in patients with spinal cord injury: review of the short form 36-health questionnaire survey. Yonsei Med J 2007; 48: 360–370.
Westgren N, Levi R . Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil 1998; 79: 1433–1439.
Whiteneck G, Meade MA, Dijkers M, Tate DG, Bushnik T, Forchheimer MB . Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch Phys Med Rehabil 2004; 85: 1793–1803.
Dijkers M . Quality of life after spinal cord injury: a meta analysis of the effects of disablement components. Spinal Cord 1997; 35: 829–840.
Hays RD, Sherbourne CD, Mazel RM . The RAND 36-Item Health Survey 1.0. Health Econ 1993; 2: 217–227.
McHorney CA, Ware Jr JE, Lu JF, Sherbourne CD . The MOS 36-Item Short Form Health Survey (SF-36): III Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care 1994; 32: 40–66.
Ware JE, Sherbourne CD . The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care 1992; 30: 473–483.
Andresen EM, Fouts BS, Romeis JC, Brownson CA . Performance of health-related quality-of-life instruments in a spinal cord injured population. Arch Phys Med Rehabil 1999; 80: 877–884.
Hays RD, Morales LS . The RAND-36 measure of health-related quality of life. Ann Med 2001; 33: 350–357.
Bollen KA . Structural Equations with Latent Variables. John Wiley & Sons: New York NY, 1989.
Buchholz A, Krol A, Rist F, Nieuwkerk PT, Schippers GM . An assessment of factorial structure and health-related quality of life in problem drug users using the Short Form 36 Health Survey. Qual Life Res 2008; 17: 1021–1029.
Taft C, Karlsson J, Sullivan M . Do SF-36 summary component scores accurately summarize subscale scores? Qual Life Res 2001; 10: 395–404.
Nortvedt MW, Riise T, Myhr KM, Nyland HI . Performance of the SF-36, SF-12, and RAND-36 summary scales in a multiple sclerosis population. Med Care 2000; 38: 1022–1028.
Anagnostopoulos F, Niakas D, Tountas Y . Comparison between exploratory factor-analytic and s.e.m.-based approaches to constructing SF-36 summary scores. Qual Life Res 2009; 18: 53–63.
Gee L, Abbott J, Conway SP, Etherington C, Webb AK . Validation of the SF-36 for the assessment of quality of life in adolescents and adults with cystic fibrosis. J Cyst Fibros 2002; 1: 137–145.
Wight JP, Edwards L, Brazier J, Walters S, Payne JN, Brown CB . The SF36 as an outcome measure of services for end stage renal failure. Qual Health Care 1998; 7: 209–221.
Ware JE, Snow KK, Kosinski M, Gandek B . SF-36 Health Survey Manual and Interpretation Guide. New England Medical Center, The Health Institute: Boston, MA, 1993.
Braschinsky M, Lüüs S-M, Gross-Paju K, Haldre S . The prevalence of hereditary spastic paraplegia and the occurrence of SPG4 mutations in Estonia. Neuroepidemiology 2009; 32: 89–93.
Ware Jr JE, Gandek B . Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol 1998; 51: 903–912.
Euroopa sotsiaaluuringu 2004 Eesti raport. European Social Survey 2004, Report of Estonia, http://www.tai.ee/failid/ESS04_Eesti_raport_uus.pdf, accessed 12 January 2009.
King M . Adaptation to changing health: response shift in quality of life research. Qual Life Res 2002; 11: 185–187.
Sprangers MAG, de Regt EB, Andries F, van Agt HM, Bijl RV, de Boer JB et al. Which chronic conditions are associated with better or poorer quality of life? J Clin Epidemiol 2000; 53: 895–907.
Haran MJ, Lee BB, King MT, Marial O, Stockler MR . Health status rated with the medical outcomes study 36-Item short-form health survey after spinal cord injury. Arch Phys Med Rehabil 2005; 86: 2290–2295.
Kreuter M, Siösteen A, Erkholm B, Byström U, Brown DJ . Health and quality of life of persons with spinal cord lesion in Australia and Sweden. Spinal Cord 2005; 43: 123–129.
Acknowledgements
This study was supported by the Estonian Science Foundation (research grant number ETF5680). We thank Krista Fischer, PhD (MRC Biostatistics Unit, Cambridge, UK; University of Tartu, Tartu, Estonia) for valuable comments and suggestions on the statistical methodology.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Braschinsky, M., Rannikmäe, K., Krikmann, Ü. et al. Health-related quality of life in patients with hereditary spastic paraplegia in Estonia. Spinal Cord 49, 175–181 (2011). https://doi.org/10.1038/sc.2010.61
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.61
Keywords
This article is cited by
-
Development and validation of TreatHSP-QoL: a patient-reported outcome measure for health-related quality of life in hereditary spastic paraplegia
Orphanet Journal of Rare Diseases (2024)
-
Experienced complaints, activity limitations and loss of motor capacities in patients with pure hereditary spastic paraplegia: a web-based survey in the Netherlands
Orphanet Journal of Rare Diseases (2020)
-
Non-motor symptoms are relevant and possibly treatable in hereditary spastic paraplegia type 4 (SPG4)
Journal of Neurology (2020)
-
Urinary symptoms, quality of life, and patient satisfaction in genetic and sporadic hereditary spastic paraplegia
Journal of Neurology (2019)
-
Health survey of adults with hereditary spastic paraparesis compared to population study controls
Orphanet Journal of Rare Diseases (2016)


