Abstract
Acquired immune deficiency virus, caused by the human immunodeficiency virus, is a significant global health concern. Sub-Saharan Africa particularly Ethiopia faces a high prevalence of human immunodeficiency virus. In low-income settings like Ethiopia, early mortality rates are elevated due to severe opportunistic infections and advanced disease at Anti-retroviral treatment initiation. Despite available treatments, delayed treatment initiation among Human Immunodeficiency Virus -infected individuals in Africa, including Ethiopia, leads to disease progression and increased mortality risk. This study aimed to identify the factors contributing to the death of HIV patients under treatment at second line regimen in public hospitals of North Wollo and Waghemira Zones. A retrospective cohort study with 474 patients was conducted in selected hospitals of North Wollo and Waghemira Zones. A parametric Weibull regression model was employed, and the adjusted hazard ratio served as the measure of association. Variables significantly affected the outcome of the study was determined at a p-value < 0.05, along with a 95% confidence interval for the variables. The patients were within the average age of 38.6(standard deviation ± 12.5) years and majority (45.57%) had no formal education. The overall death incidence rate among second-line anti-retroviral treatment patients was 1.98 per 100-person years [95% CI 1.4—2.9%]. Poor adherence to antiretroviral treatment, male gender, and being underweight significantly increased the hazard of death. Conversely, increased anti-retroviral treatment duration had a significant and negative impact, reducing the hazard of death among patients. The study reveals a high incidence of death among second line anti-retroviral treatment users. Independent predictors include poor adherence, male gender, and underweight status, all significantly increasing the risk of death. On the positive side, the hazard of death decreases with longer anti-retroviral treatment duration. A critical concern and counseling should be given for better ART adherence, to change their nutritional status and for males.
Similar content being viewed by others
Introduction
Acquired immunodeficiency syndrome (AIDS) was recognized as a new disease in 1981, marked by higher death rates among young homosexual men due to uncommon infections and rare cancers1. AIDS is an infectious disease caused by Human Immune Deficiency Virus (HIV), primarily targeting the immune system2. It's a major global health concern, with 25.8 million people living with HIV in Sub-Saharan Africa3,4. Ethiopia, similar to other Sub-Saharan nations, hosts one of the globe's largest populations of individuals living with HIV, with approximately 1.2 million infected individuals5. Despite ART progress and treatment-as-prevention efforts, around 2 million new HIV infections occur yearly6. Ethiopia is one of the most affected countries in Sub-Saharan Africa by the HIV epidemic, with an estimated 617,921 individuals living with HIV, where 78% of adults and children receive ART7. Ethiopia is severely impacted by the HIV pandemic, ranking among the most affected sub-Saharan African nations8. Second-line regimens are employed when first-line treatments fail, determined by factors such as the patient's CD4 cell count, HIV viral load, or clinical indicators9.
In low-income settings, early mortality rates were higher due to more severe opportunistic infections and advanced disease at ART initiation10. ART globally saved millions of lives and significantly reduced illness and death in people living with HIV/AIDS (PLWHA)9. HIV/AIDS remains a pressing issue, particularly in resource-limited nations, leading to significant morbidity and mortality11. Income Disparity Influences Mortality Rates in Adults on ART: Higher Mortality in Low-Income Countries. Mortality of adult patients who are on antiretroviral therapy (ART) is higher in low-income than in high-income countries10.
By the end of 2020, over 26 million individuals living with HIV globally had received antiretroviral therapy (ART), leading to a notable decrease in HIV-related illness and deaths12. Despite the considerable decrease in mortality and illness among individuals with HIV due to Highly Active Antiretroviral Therapy (HAART), some patients still experience mortality even after beginning ART13. Around 1.7 million individuals died from AIDS-related causes globally, with 70% of these occurrences happening in Sub-Saharan Africa, as per the 2012 UNAIDS report8,14.
ART's introduction linked to global reduction in HIV-Attributed Deaths. In resource-constrained settings, there has been notable high early mortality following the initiation of ART15. Despite available treatments, many HIV-infected individuals, notably in Africa like Ethiopia, delay treatment, leading to disease progression and higher risk of mortality2. Patients in resource-limited countries face a higher risk of mortality compared to those in high-income nations16. The government of Ethiopia has been working on the scaling up of ART for all people to reduce AIDS-related morbidity and death. Despite the scale-up of ART, early mortality is a major challenge. High rates of early mortality were reported from a number of Sub-Saharan African ART programs17. The advent of combination antiretroviral therapy (cART) significantly improved AIDS prognosis. However, discontinuation of ART in some HIV patients can contribute to adverse outcomes, including death18. Third-line regimens, being expensive and scarce in resource-limited settings, make second-line treatment the final available option for many patients in these regions19.
Limited access to treatment, poverty, and ignorance has all contributed to the elevated mortality rates associated with this illness in the area20. Most studies focus on baseline predictors. Although previous studies have identified the factors that influence mortality, it is important to note that these determinants can vary greatly depending on the context, setting and change over time. Research findings can be influenced by contextual factors or specific population characteristics. Moreover, cohort studies provide insights into the dynamics and trajectories of phenomena (death) and can help identify temporal patterns or causal relationships that may not be apparent in cross-sectional studies. This study aimed to identify the factors contributing to the death of HIV patients under treatment at second line regimen in public hospitals in North Wollo and Waghemira Zones. This can help identify the potential impact of contextual factors on the generalizability of research findings.
This may help programmers to tackle the cause of death through the cohort of HIV patients based in second line ART treatment. Studies are limited on the incidence and predictors of death during follow up period.
Methodology
Study design and setting
Retrospective cohort study was conducted in three hospitals of North Wollo and Waghemira Zones. The three hospitals included in this study were Woldia Comprehensive Specialized Hospital, St. Lalibella General Hospital, and Tefera Hailu Memorial Hospitals. These hospitals were selected because they are the only hospitals which provide second line ART.
Sampling technique, inclusion and exclusion, sample size and data collection
This study was conducted based on secondary source data which was from patients medical records and charts.
A consecutive sampling method was applied and all HIV/AIDS patients who had followed up from September 2016 and April 2020 and who had minimum of 6 month on treatment of ART were included and incomplete charts were excluded. The patients who had followed up in the specified period was our study population. A total of 474 HIV/AIDS patients were used for this study.
Data extraction checklist was prepared based on literatures. An initial preliminary review was conducted to modify the extraction tool.
Variables of the study
The outcome variable of this study was time from second – line ART initiation to death.
The independent variables included for this study was marital status, sex, age, education status, lost to follow up, opportunistic infections, BMI, functional status, duration of ART, WHO stage, virological failure, second line ART regimen, comorbidity, ART adherence and HIV disclosure and these variables were screened by bi-variable analysis.
Operational definitions
Event
The event of interest for this study is the death of HIV/AIDS patients in second line ART treatment.
Censored
This study include those patients who are lost to follow up, live beyond the study period and deaths unrelated to their diseases.
ART adherence
The level of ART drug adherence was classified as good if ≥ 95% adherence by pill count, fair if 85% to 94% adherence by pill count, or poor if < 85% adherence by pill count.
Data management and analysis
The collected data was entered by EpiData-3.3.1. The entered data was exported to Stata version 17 for further statistical analysis. According to the proportion of missing to be managed, missing data was managed by imputation method using R software.
Descriptive statistics was reported using text, table and graph. Specific to survival analysis, data were presented by Kaplan Meier survival curve. In this study survival analysis was done to identify predictors of incidence of death. Survival analysis is a statistical method used to analyze time-to-event data, where the event of interest is typically death, failure, or any other occurrence that marks the end of the observation period. In survival analysis, parameter estimation involves estimating the parameters of a survival model that describes the relationship between covariates and survival times. There are some commonly used parameter estimation methods for survival analysis. For parameter estimation, there are different survival models to be considered, these are semi-parametric (cox regression model) and parametric models (Exponential, Weibull, Gamma, Log normal,Loglogistic). The summary of formula of each parametric model is described as follows:
The commonly used parametric distributions and parameters:
Distributions | f(t) | S(t) | h(t) |
|---|---|---|---|
Exponential | λexp(-λt) | exp (− λt) | λ |
Weibull | \({\lambda pt}^{p-1}\) exp(\({-\lambda t}^{p}\)) | exp (\({-\lambda t}^{p})\) | \({\lambda pt}^{p-1}\) |
Log-logistic | \(\frac{{\lambda pt}^{p-1}}{{(1+{\lambda t}^{p})}^{2}}\) | \(\frac{1}{1+{\lambda t}^{p}}\) | \(\frac{{\lambda pt}^{p-1}}{1+{\lambda t}^{p}}\) |
where λ is the location parameter, p is shape parameter.
In this study, proportional hazard assumption was checked using graph, global tests and adding time varying covariates.
Model fitness was checked using AIC and a model with lower AIC value was selected as the best fitted model. Bi-variable analysis was done and variables with p-value less than 0.25 were entered into multivariable analysis. Finally to assess the association of incidence of death and its predictors among second line ART patients, a parametric weibull regression model was done. A measure of association using Adjusted hazard ratio (AHR) was used and the variable significantly affected the variable of the study was determined at a p-value < 0.05, along with a 95% confidence interval for the variables.
Ethics approval and consent to participate
To conduct the study, ethical approval was obtained from Woldia University institutional review board (WDUIRB). Since the study was secondary data and which was not directly obtained from patients, permission letter to access the charts and records was given for selected hospitals of North Wollo and Waghemira zone.
Result
Socio- demographic characteristics of participants
Regarding their demographic status, almost half 238(50.21%) of HIV/AIDS patients were in the age group 41 and above years old. Majority had no formal education (45.57%) and few (18.35%) were attended secondary and above education. Males were the dominant HIV/AIDS patients on second-line ART in this study which accounts 54.85%. Near to half of the patients were married (46.2%) (Table1).
HIV related and other clinical important variables
Most 406 (85.65%) of patients had working functional status. Around 185 (39.03%) were underweight, 261 (55.06%) normal and 28 (5.91%) overweight/obese. Majority were in WHO T-stage one which accounts 358 (75.53%) and 26 (5.49%) had lost to follow up. There was considerable magnitude of virological failure which accounts about 73 (15.40%). Majority 393 (82.91%) had good adherence and almost all 316 (91.59%) disclose their HIV status (Table 2).
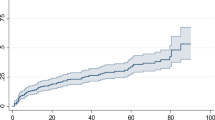
Kaplan–Meier estimates
The Kaplan-Maier curve provides a useful summary of survival data and can be used to estimate median survival time. The curve showed that the data had no median survival time. This indicated that the number of censored is greater than event of interest (Fig. 1).
Incidence of death
There were 29 deaths and the person time of death was 1461.5 years. The overall incidence rate of death among second line ART patients were 1.98 [95% CI of 1.4 & 2.9%] per 100- person year.
Factors associated with incidence of death
Initially cox proportional hazard assumptions were assessed. The graph showed that the assumption was violated. In order to confirm the violation of the assumption, a global test was used (phtest) and indicated that there was enough evidence to reject the hypothesis of proportional hazard assumption at p-value less than 0.05 (Global test p- value = 0.049). In addition, the information criteria support that the proportional hazard model was not the best fitted model. Therefore, parametric models were considered such as exponential, Weibull, Log normal, Log logistic and Gompertz.The best fitted model was parametric Weibull model and selected using information criteria such as log likelihood ratio test, AIC and BIC (Table 3).
Lastly, multivariable Weibull regression model was used to assess the predictors of death. In multivariable Weibull regression, ART adherence, ART duration and BMI were significantly associated with incidence of death among second line ART patients. Patients who had poor ART adherence were 3.59 times more hazard of death as compared to those with good adherence [AHR = 3.59, 95% 1.39,9.24]. Sex of patients was significantly associated incidence of death, being male increased the hazard of death by 2.36 times as compared to males [AHR = 2.36, 95% CI 1.06, 5.29]. Regarding duration of ART, increasing the duration of ART by one year decreases the hazard of death by 0.97 times [AHR = 0.97, 95% CI 0.96, 0.98]. Patients who are underweight had more hazard of death by 3.12 times as compared with those normal BMI [AHR = 3.12, 95% CI 1.37, 7.12] (Table 4).
Discussion
This study was aimed to identify the predictors of incidence of death among second line ART patients. Around two present of patients were died during their second line ART follow up. This finding was lower than a study finding of Tanzania, Dessie, Metema, Amhara region, Gofa Zone of SNNPs, Aksum4,10,12,13,21,22. This study was in lined with a study conducted in Harari hospital Ethiopia16. This study finding was also below the study result of Nekemte, Gondar and Debre Markos Comprehensive Specialized Hospital23,24,25. The possible variation might be the difference in study sample size or denominator and the characteristics of study participants in relation to socio demographic, socio economic and cultural variations.
Regarding predictors, those patients who had poor ART adherence were significantly and positively associated with the risk of death. This is in line with a study conducted in selected hospitals of Amhara region and Dessie referral hospital12,21. Other studies also support this finding like studies conducted in Harar, Africa and Asia point out that HIV-infected patients with poor ART adherence had a higher risk of death as compared to those who had good ART adherence16,19.Similarly a study conducted in West Amhara, Gofa zone of SNNPs, Tanzania and Sub-Saharan African Sites showed that poor ART adherence had the highest risk of death than adherent patients2,22,26,27. Study conducted in Nekemte showed that poor ART adherence was found to be an independent predictor of death25. However, in contrary to the study finding conducted at Gondar that fair adherence level had high hazard of death23. The reason might be because poor adherence leads to low levels of drug, driving to viral replication, drug resistance, and viral rebound. That in turn causes low CD4 count which leads to morbidity and death28.
Being male also significant predictor and increased the incidence of death of HIV/AIDS patients on second line ART. This finding is in line with the study conducted in Uganada, Iran and Zambia29,30,31. However this is in contrast with the study finding of Tennessee32. Other study conducted in China and Nepal showed that men have a significantly higher risk of death than female33,34. There is no scientific evidence on the mechanism how males are more prone to risk of death than females. But different studies point out possible reasons for their death as males have less health care access than female might be due to high workloads. Males delay in treatment adherence and may not have better recovery of immune system as compared to females35,36.
Increasing ART duration by one year reduced the risk of incidence of death during their follow up. This finding is comparable with the study conducted in southern India37. This is also supported by the study conducted in Debre Tabor and Southern Oromiyaa region indicated that the death rate of patients in the earlier months of ART initiation was high and it declined in the later months of follow-up20,38. The study conducted in Korea and Nepal showed that the risk of death was lower in late ART follow up (1–5 years later) than the first year of ART duration which is similar to this study finding34,39. The explanation could be that with a longer duration of antiretroviral therapy (ART), there is a potential for an increase in CD4 count, improved viral suppression, and a reduced likelihood of co-infection compared to the early stages of ART initiation. In the initial phases of ART, there might not be significant improvements in patient immunity, making them more susceptible to infections. However, as the duration of ART progresses, these factors may diminish, leading to a lower risk of death.
Nutritional status is the other key significant predictor that those patients who are underweight face the risk of death as compared to those normal BMI range. This finding was supported by the study conducted in Metema, Tanzania, East Africa and Nigeria, Sub-Saharan African Sites and found that being underweight patents were at high risk of death8,13,26,40. Being underweight increases the likelihood of negative clinical results and serves as a predictor for the development of opportunistic infections (OIs) in individuals with HIV/AIDS, ultimately leading to death41.
Conclusion
The incidence of death among HIV/AIDS patients on second line ART was high. The risk of death was significant among patients with poor adherence and those who are male and underweight. However, the hazard of death decreased as the duration of ART increased. Therefore, a critical concern and counseling should be given for better ART adherence, to change their nutritional status and for males.
Strengths and limitations of the study
As compared to cross-sectional survey, this study has strengths related to the design. This study was conducted by retrospective cohort design. Therefore, temporal relationships can be determined for the outcome variable and its predictors. Even though this study had strengths,there was limitations related to the source which was secondary nature of the data. Since the data was from patient records and charts, some important variables were not available.
Data availability
The data used for this study is available in the manuscript. It also available at the hand of all authors and can be given upon reasonable request.
Abbreviations
- AHR:
-
Adjusted hazard ratio
- ART:
-
Anti-retroviral treatment
- BMI:
-
Body mass index
- HAART:
-
Highly active antiretroviral therapy
- HIV:
-
Human immunodeficiency virus
- OIs:
-
Opportunistic infections
- SNNPs:
-
South Nations Nationalist and People
- WHO:
-
World health organization
References
Sharp, P. M. & Hahn, B. H. Origins of HIV and the AIDS pandemic. Cold Spring Harbor Perspect. Med. https://doi.org/10.1101/cshperspect.a006841 (2011).
Alemu, G. G., Nigussie, Z. M., Amlak, B. T. & Achamyeleh, A. A. Survival time and predictors of death among HIV infected under five children after initiation of anti-retroviral therapy in West Amhara Referral Hospitals, Northwest Ethiopia. BMC Pediatr. 22(1), 670 (2022).
Ethiopia FMoH. National guidelines for comprehensive HIV prevention, care and treatment View (2014).
Misgina, K. H. et al. Predictors of mortality among adult people living with HIV/AIDS on antiretroviral therapy at Suhul Hospital, Tigrai, Northern Ethiopia: A retrospective follow-up study. J. Health Popul. Nutr. 38, 1–10 (2019).
Biset, A. M. Mortality and its predictors among HIV infected patients taking antiretroviral treatment in Ethiopia: A systematic review. AIDS Res. Treat. 2017, 1–10 (2017).
Pandey, A. & Galvani, A. P. The global burden of HIV and prospects for control. Lancet HIV 6(12), e809–e811 (2019).
Ethiopian Public Health Institute. HIV Estimates and projection for the year 2020 and 2021. Addis Abeba, Ethiopia: EPHI. https://ephi.gov.et/wp-content/uploads/2021/06/HIV-Estimates-and-projection-for-the-year-2020-and-2021.pdf (Accessed 27 April 2022) (2021).
Damtew, B., Mengistie, B. & Alemayehu, T. Survival and determinants of mortality in adult HIV/Aids patients initiating antiretroviral therapy in Somali Region, Eastern Ethiopia. Pan Afr. Med. J https://doi.org/10.11604/pamj.2015.22.138.4352 (2015).
Tsegaye, A. T., Wubshet, M., Awoke, T. & Alene, K. A. Predictors of treatment failure on second-line antiretroviral therapy among adults in northwest Ethiopia: A multicentre retrospective follow-up study. BMJ Open 6(12), e012537 (2016).
Tadesse, K., Haile, F. & Hiruy, N. Predictors of mortality among patients enrolled on antiretroviral therapy in Aksum hospital, northern Ethiopia: A retrospective cohort study. PLoS One 9(1), e87392 (2014).
Gunda, D. W., Nkandala, I., Kilonzo, S. B., Kilangi, B. B. & Mpondo, B. C. Prevalence and risk factors of mortality among adult HIV patients initiating ART in rural setting of HIV care and treatment services in North Western Tanzania: A retrospective cohort study. J. Sex. Transm. Dis. 2017, 1–8 (2017).
Wedajo, S., Degu, G., Deribew, A. & Ambaw, F. Treatment failure, death, and predictors among PLWHIV on second-line antiretroviral therapy in Dessie Comprehensive Specialized Hospital, northeast Ethiopia: A retrospective cohort study. PLoS One 17(6), e0269235 (2022).
Workie, K. L., Birhan, T. Y. & Angaw, D. A. Predictors of mortality rate among adult HIV-positive patients on antiretroviral therapy in Metema Hospital, Northwest Ethiopia: A retrospective follow-up study. AIDS Res. Ther. 18(1), 1–11 (2021).
Granich, R. et al. Trends in AIDS deaths, new infections and ART coverage in the top 30 countries with the highest AIDS mortality burden; 1990–2013. PLoS One 10(7), e0131353 (2015).
Chakravarty, J. et al. Determinants of survival in adult HIV patients on antiretroviral therapy in Eastern Uttar Pradesh: A prospective study. Indian J. Med. Res. 140(4), 491 (2014).
Birhanu, A., Dingeta, T. & Tolera, M. Predictors of mortality among adult HIV-infected patients taking antiretroviral therapy (art) in Harari hospitals, Ethiopia. HIV/AIDS-Res. Palliat. Care 13, 727–36 (2021).
Setegn, T., Takele, A., Gizaw, T., Nigatu, D. & Haile, D. Predictors of mortality among adult antiretroviral therapy users in southeastern Ethiopia: Retrospective cohort study. AIDS Res. Treat. 2015, 1–8 (2015).
Aemro, A., Wassie, M. & Chekol, B. Incidence and predictors of mortality within the first year of antiretroviral therapy initiation at Debre-Markos Referral Hospital, Northwest Ethiopia: A retrospective follow up study. PLoS One 16(5), e0251648 (2021).
Pujades-Rodríguez, M., Balkan, S., Arnould, L., Brinkhof, M. A. & Calmy, A. Treatment failure and mortality factors in patients receiving second-line HIV therapy in resource-limited countries. JAMA 304(3), 303–312 (2010).
Alemu, A. W. & Sebastián, M. S. Determinants of survival in adult HIV patients on antiretroviral therapy in Oromiyaa, Ethiopia. Glob. Health Act. 3(1), 5398 (2010).
Tsegaye, A. T., Alemu, W. & Ayele, T. A. Incidence and determinants of mortality among adult HIV infected patients on second-line antiretroviral treatment in Amhara region, Ethiopia: A retrospective follow up study. Pan Afr. Med. J. https://doi.org/10.11604/pamj.2019.33.89.16626 (2019).
Kebede, A., Tessema, F., Bekele, G., Kura, Z. & Merga, H. Epidemiology of survival pattern and its predictors among HIV positive patients on highly active antiretroviral therapy in Southern Ethiopia public health facilities: A retrospective cohort study. AIDS Res. Ther. 17, 1–8 (2020).
Teshale, A. B., Tsegaye, A. T. & Wolde, H. F. Incidence of mortality and its predictors among HIV positive adults on antiretroviral therapy in University of Gondar comprehensive specialized Hospital Northwest Ethiopia. HIV/AIDS-Res. Palliat. Care 13, 31–39 (2021).
Alebel, A., Sibbritt, D., Petrucka, P. & Demant, D. Association between body mass index variation and early mortality among 834 ethiopian adults living with HIV on ART: A joint modelling approach. Infect. Dis. Ther. 12(1), 227–244 (2023).
Hambisa, M. T., Ali, A. & Dessie, Y. Determinants of mortality among HIV positives after initiating antiretroviral therapy in Western Ethiopia: A hospital-based retrospective cohort study. Int. Sch. Res. Not. 2013, 1–7 (2013).
Palombi, L. et al. Incidence and predictors of death, retention, and switch to second-line regimens in antiretroviral-treated patients in sub-Saharan African Sites with comprehensive monitoring availability. Clin. Infect. Dis. 48(1), 115–122 (2009).
Hawkins, C. et al. Switching to second-line ART in relation to mortality in a large Tanzanian HIV cohort. J. Antimicrob. Chemother. 72(7), 2060–2068 (2017).
Kiwuwa-Muyingo, S. et al. Dynamic logistic regression model and population attributable fraction to investigate the association between adherence, missed visits and mortality: A study of HIV-infected adults surviving the first year of ART. BMC Infect. Dis. 13, 1–14 (2013).
Alibhai, A. et al. Gender-related mortality for HIV-infected patients on highly active antiretroviral therapy (HAART) in rural Uganda. Int. J. Women’s Health https://doi.org/10.2147/IJWH.S9408 (2010).
Gheibi, Z., Dianatinasab, M., Haghparast, A., Mirzazadeh, A. & Fararouei, M. Gender difference in all-cause mortality of people living with HIV in Iran: Findings from a 20-year cohort study. HIV Med. 21(10), 659–667 (2020).
Kerkhoff, A. D. et al. Mortality estimates by age and sex among persons living with HIV after ART initiation in Zambia using electronic medical records supplemented with tracing a sample of lost patients: a cohort study. PLoS Med. 17(5), e1003107 (2020).
Lemly, D. C. et al. Race and sex differences in antiretroviral therapy use and mortality among HIV-infected persons in care. J. Infect. Dis. 199(7), 991–998 (2009).
Chen, M. et al. Gender differences in outcomes of antiretroviral treatment among HIV-infected patients in China: A retrospective cohort study, 2010–2015. JAIDS J. Acquir. Immune Defic. Syndr. 76(3), 281–288 (2017).
Angdembe, M. R., Rai, A., Bam, K. & Pandey, S. R. Predictors of mortality in adult people living with HIV on antiretroviral therapy in Nepal: A retrospective cohort study, 2004–2013. PLoS One 14(4), e0215776 (2019).
Nash, D. et al. Long-term immunologic response to antiretroviral therapy in low-income countries: Collaborative analysis of prospective studies: The antiretroviral therapy in lower income countries (ART-LINC) collaboration of the international epidemiological databases to evaluate AIDS. AIDS (Lond. Engl.) 22(17), 2291 (2008).
Lee, M. P. et al. Impact of gender on long-term treatment outcomes of highly active antiretroviral therapy (HAART) in the TREAT Asia HIV observational database. AIDS Patient Care STDs 29(5), 229–231 (2015).
Joseph, N., Sinha, U., Tiwari, N., Ghosh, P. & Sindhu, P. Prognostic factors of mortality among adult patients on antiretroviral therapy in India: A hospital based retrospective cohort study. BioMed. Res. Int. 2019, 1–10 (2019).
Belay, D. B. & Derebe, K. Determinant factors associated with time to death of HIV/AIDS patients: An application of parametric shared frailty models. Sci. Afr. 15, e01104 (2022).
Lee, S. H. et al. Causes of death and risk factors for mortality among HIV-infected patients receiving antiretroviral therapy in Korea. J. Korean Med. Sci. 28(7), 990–997 (2013).
Johannessen, A. et al. Predictors of mortality in HIV-infected patients starting antiretroviral therapy in a rural hospital in Tanzania. BMC Infect. Dis. 8, 1–10 (2008).
Assefa, M. G., Deksisa, A., Abdo, M., Alemayehu, O. T. & Daka, D. W. Predictors of underweight among adult patients receiving antiretroviral therapy in Bishoftu general hospital, central Ethiopia: Case-control study. PLoS One 18(9), e0291602 (2023).
Acknowledgements
We would like to thank the data collectors, data clerks in ART clinic for their support and hospital administrators for their willingness and permission to access patient records.
Funding
This research was funded by Woldia University.
Author information
Authors and Affiliations
Contributions
AA and SA: conceptualized the study and was involved in the design, analysis, interpretation, and manuscript writing. FK: manuscript writing and editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kidie, A.A., Masresha, S.A. & Bizuneh, F.K. Statistical analysis on the incidence and predictors of death among second-line ART patients in public hospitals of North Wollo and Waghemira Zones, Ethiopia, 2021. Sci Rep 14, 10893 (2024). https://doi.org/10.1038/s41598-024-60119-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-60119-1
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.