Abstract
The combination of noradrenergic (reboxetine) plus antimuscarinic (oxybutynin) drugs (reb-oxy) reduced obstructive sleep apnea (OSA) severity but no data are available on its effects on cardiac autonomic modulation. We sought to evaluate the impact of 1-week reb-oxy treatment on cardiovascular autonomic control in OSA patients. OSA patients were randomized to a double-blind, crossover trial comparing 4 mg reboxetine plus 5 mg oxybutynin to a placebo for OSA treatment. Heart rate (HR) variability (HRV), ambulatory blood pressure (BP) monitoring (ABPM) over 24 h baseline and after treatment were performed. Baroreflex sensitivity was tested over beat-to-beat BP recordings. 16 subjects with (median [interquartile range]) age 57 [51–61] years and body mass index 30 [26–36]kg/m2 completed the study. The median nocturnal HR was 65 [60–69] bpm at baseline and increased to 69 [64–77] bpm on reb-oxy vs 66 [59–70] bpm on placebo (p = 0.02). The mean 24 h HR from ABPM was not different among treatment groups. Reb-oxy administration was not associated with any modification in HRV or BP. Reb-oxy increased the baroreflex sensitivity and did not induce orthostatic hypotension. In conclusion, administration of reb-oxy did not induce clinically relevant sympathetic overactivity over 1-week and, together with a reduction in OSA severity, it improved the baroreflex function.
Similar content being viewed by others
Introduction
Obstructive sleep apnea (OSA) is one of the most common sleep disorders affecting one-third of the population aged 30–70 years in Europe1. The repetitive collapse of the pharyngeal airway characteristic of OSA leads to intermittent oxygen desaturations and sleep fragmentation with downstream consequences, including an increased risk of cardiovascular disease, daytime sleepiness, and sympathetic nervous system over-activity2,3. Intermittent hypoxemia and arousals from sleep activate the sympathetic nervous system, being them the major contributors to the blood pressure (BP) and heart rate (HR) elevation, together with the release of inflammatory mediators2,4. Thus, untreated OSA may lead to cardiovascular, neurocognitive, metabolic, and daytime functional consequences over time, resulting in increased morbidity and mortality5.
In the last 40 years, the gold standard for OSA treatment has been nocturnal ventilation through continuous positive airway pressure (CPAP), which acts to pneumatically splint the pharynx open. If regularly employed, CPAP therapy might reduce cardiovascular risk and overall mortality rate6,7, partially by attenuating sympathetic over-activity8,9 and improving arterial baroreflex sensitivity, depressed by OSA10,11,12. Although OSA is effectively alleviated by this treatment, CPAP is poorly tolerated by many patients, with a consequent very low adherence13,14. Hence, there is an urgent need for alternative interventions that are safe and well-tolerated15,16,17.
Reduced pharyngeal dilator muscle tone and responsiveness during sleep are key contributors to OSA pathogenesis18,19. Responsible for the latter is a loss of noradrenergic drive and muscarinic inhibition to the upper airway muscles20,21. In the last years, these findings have stimulated research on pharmacological solutions aimed at improving neural control of pharyngeal muscle tone. In such a context, pharmacotherapy for OSA is moving its first steps with promising results provided by single-night studies17,22. We have recently performed a study aimed at expanding the knowledge on these pharmacological possibilities by conducting a randomized controlled trial to evaluate for the first time the effectiveness of the combination of reboxetine (a noradrenaline reuptake inhibitor agent) and oxybutynin (an antimuscarinic compound), administered over a 1-week period, versus placebo on patients with moderate-to-severe OSA with promising results23.
As known, noradrenaline is the main neurotransmitter of the sympathetic nervous system and muscarinic receptors are responsible for the vagal activity. Thus, a pending issue, not yet explored, is the possibility that the administration of noradrenergic reboxetine together with antimuscarinic oxybutynin might negatively affect the autonomic control of circulation24,25. On the other hand, the substantial decrease of the apnea-hypopnea index (AHI) with the resulting improvement of nocturnal hypoxemia induced by reb-oxy, might be also associated with beneficial effects on sympathetic over-activity, thus counterbalancing the direct sympathetic stimulation of these noradrenergic and antimuscarinic drugs.
The sympathetic and parasympathetic cardiovascular modulation can be assessed with direct measurements, or thanks to non-invasive reliable tools such as BP by 24 h ambulatory monitoring (ABPM), HR variability (HRV), and baroreceptor sensitivity (BRS)24,26,27,28.
In order to assess the effect of reboxetine plus oxybutynin (reb-oxy) on cardiovascular autonomic modulation in OSA patients, we performed 24 h ABPM and estimated BRS and HRV after 1-week of treatment in the frame of our randomized controlled cross-over trial. The outcomes were evaluated as the change from baseline during the week of reb-oxy administration and compared to placebo.
Methods
Patients and study design
We performed a randomized, double-blind, placebo-controlled, cross-over, single-center study of the combination of reb-oxy in adults with OSA documented by polysomnography (PSG). Participants were enrolled from July 2020 to October 2020 through our sleep clinic (Istituto Auxologico Italiano, Milan, Italy) and the trial ended when the previously calculated sample size of 16 patients was reached. Participants were randomized (1:1 ratio) to first receive a 4 mg reboxetine plus 5 mg oxybutynin or a matching placebo, and then to switch to the other treatment arm after a washout of 7–10 days. Study participants matching eligibility criteria performed a one-night inpatient PSG test, which served as the baseline measure for AHI. Subjects started taking the study drug the day after the baseline PSG, immediately before bedtime, and continued for 7 days in total. On the final dosing night of each week, participants performed in-lab PSG. The study was approved by the Ethics Committee on 18/02/2020 (approval n. 2020_02_18_03) and by the Italian drug agency AIFA (Agenzia Italiana del Farmaco) on 22/04/2020 (EudraCT n 2019-004917-15) and all methods were performed in accordance with the guidelines and regulations. Informed consent in writing was obtained from all study participants. The study was first registered at ClinicalTrials.gov (NCT04449133) on 26/06/2020.
Measurements
Overnight in-lab polysomnography
PSG recording and data interpretation was performed in accordance with the American Academy of Sleep Medicine (AASM) scoring manual29. All studies were scored by the same specialized sleep clinician, blinded to treatment assignment, according to AASM scoring criteria30.
Heart rate variability
The beat-by-beat series of R-R intervals were extracted from 1 ECG channel of each PSG through a derivative-and-threshold algorithm, selecting a segment of at least 10-min duration without respiratory events in the supine position during non-REM stage 2 (N2) sleep for the HRV analysis. Premature beats were visually identified and manually removed, obtaining series of normal-to-normal intervals (NNI). Time-domain indexes of HRV were the root-mean-square of successive differences (RMSSD) and the percentage of beats with NNI value at least 50 ms longer or shorter than NNI of their preceding beat (pNN50)28. For the frequency-domain analysis, the NNI series was resampled evenly at 5 Hz linearly interpolating possibly missing beats. The Welch periodogram was estimated using 50% overlapped Hanning windows of 120 s length. The powers in the very-low-frequency (VLF, between 0.0025 and 0.04 Hz), low-frequency (LF, between 0.04 and 0.15 Hz), and high-frequency (HF, between 0.15 and 0.40 Hz) bands, as well as the LF/HF powers ratio, were obtained by integrating the periodogram28. The breathing rate was estimated from the fluctuations of QRS-complex amplitude of the ECG reflecting the respiratory movements of the thorax31. The series of the R peaks resampled at 5 Hz were high-pass filtered at 0.05 Hz to remove oscillations too long to be generated by respiratory movements; the Welch periodogram was calculated and the breathing rate measured as the frequency of the highest spectral peak.
Ambulatory blood pressure monitoring
ABPM was performed using a validated oscillometric device (TM2430; A&D Medical, Japan) to evaluate blood pressure (BP) changes for 24 h. Blood pressure was evaluated every 20 min during the day and every 30 min during the night. Day and night sub-periods were defined according to the personal logbook. 24 h, daytime and night-time average Systolic BP (SBP), Diastolic BP (DBP) and heart rate (HR), day and night SBP and DBP standard deviations (SD) were quantified to assess BP variability, SBP and DBP nocturnal falls, night/day ratios, average morning (7–11 a.m.) values and morning surge (defined as the difference between the lowest SBP or DBP value before the morning rise and the highest SBP or DBP value after awakening). The ABPM monitoring was assessed in the pre-screening visit at least 2 days before baseline PSG and between the 2nd and the 5th night of the two weeks of treatment to avoid disturbing the PSG night sleep.
Baroreflex function
ECG and non-invasive BP were measured by a Nexfin® device (BMEYE, Amsterdam, The Netherlands). Patients underwent measurements at rest, without coffee intake in the previous 3 h and at the same time of the day before the PSG. Recordings were performed in a silent room without speaking and without any disturbing elements for 10 min while patients were lying supine, and then for 10 min while they were standing. The beat-by-beat values of SBP and DBP, derived from the continuous BP, recordings, and NNI from the ECG lead, were interpolated evenly at 5 Hz for spectral analysis. The sensitivity of the baroreflex control of heart rate (BRS) was estimated by the sequence technique32 (BRSSEQ), the transfer function technique (HLF)33, and the spectral method (αLF)34. As to BRSSEQ, the beat-to-beat series were scanned in search of sequences of 3 or more consecutive heartbeats in which a progressive SBP increase was followed, with a lag of zero, one or two beats, by a progressive NNI lengthening or, vice versa, in which a progressive SBP reduction was followed by a progressive NNI shortening. The slope of the regression line between SBP and NNI values in each sequence was taken as a local BRS estimate. The local estimates were averaged over the supine and standing periods separately to obtain the final BRSSEQ values. As to the spectral and transfer function estimates, the SBP and NNI power spectra, and SBP-NNI cross-spectrum and coherency spectrum were calculated from the evenly resampled series at 5 Hz using 50% overlapped Hann data windows of 120s length. SBP and NNI powers were calculated over the LF band and the root square of the SBP/ NNI powers ratio evaluated only for spectral lines with squared coherence modulus > 0.3 provided the αLF estimate of BRS. The ratio between the SBP-NNI cross-spectrum and NNI spectrum was calculated considering again only spectral lines with squared coherence modulus > 0.3 and averaged over the LF band, providing the HLF estimate of BRS.
The DBP power spectrum was similarly estimated by the Welch periodogram. The baroreflex resonance was quantified by integrating the DBP and SBP power spectra over the LF band (DBPLF and SBPLF). These indexes measure the power of the 10-s oscillations in arterial BP, which are considered a surrogate measure of sympathetic activity35.
For each index, the difference (delta Δ) between supine position and standing was also calculated.
Statistical analysis
Categorical data were summarized by proportions, while continuous data by median [interquartile range] values. Percent changes in study variables from baseline after 1-week of placebo and after 1-week of reb-oxy were compared as continuous variables by using a two-tailed Wilcoxon matched-pairs signed-rank test. The effect of the drug combination on the cardiovascular autonomic nervous system reported here was a prespecified exploratory outcome, while the primary outcome was AHI change as reported in our previous publication23. According to study design, a sample size of 16 subjects was powered to detect an AHI reduction with Reb-Oxy than placebo (alpha 5%, power 80%), plus a ≈ 20% dropout{Perger, 2022 #223}.
A p-value of <0·05 was considered statistically significant. Statistical analyses were performed using Statistical Analysis Software (SAS Cary, NC, USA).
Results
The anthropometric and clinical characteristics of the 16 participants are presented in Table 1. None had beta-blockers as chronic therapy. No serious adverse events occurred. The main sleep and OSA severity metrics are summarized in Table 2. Other results of this trial have been previously published23.
Heart rate and blood pressure
Median nocturnal heart rate (HR) during the PSG increased from 65 [60–69] bpm at baseline to 69 [64–77] bpm on reb-oxy and to 66 [59–70] bpm on placebo (p=0.02 for reb-oxy versus placebo) (Table 2). However, 24 h HR measured by ABPM was not significantly different between treatment groups, as shown in Table 3.
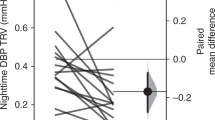
Reb-oxy did not significantly modify 24 h, daytime, and night-time DBP and SBP (Table 3). Morning surge was not increased on reb-oxy as compared to placebo and BP variability was not significantly different during the day and the night between groups.
Based on both time and frequency domain analyses, reb-oxy administration was not associated with any modifications in HRV (Table 2). The respiratory frequencies remained in the HF band in both groups.
Baroreflex sensitivity and resonance
Table 4 reports the estimates of baroreflex sensitivity and the measures of baroreflex resonance in BP spectral powers at baseline, after 1 week of placebo, and after 1 week of reb-oxy treatment. In the supine position, both the spectral and the transfer function estimates of baroreflex sensitivity were significantly greater after reb-oxy administration than on placebo. A similar effect was observed in standing position: both αLF and HLF increased more after treatment with reb-oxy than after the placebo treatment, the difference being significant for the spectral estimates. Figure 1 shows the corresponding percent changes from baseline recordings. The percent changes in αLF from supine to standing were similar on placebo (+ 49% [+ 32 to + 60] %) and on reb-oxy (+4 6% [+ 33 to + 66] %, p = 0.58). The percent changes in HLF from supine to standing were similar on placebo (+ 49% [+ 30 to + 59] %) and on reb-oxy (+ 47% [+ 39 to + 69] %, p 0.42). When considering changes from baseline to treatment, no differences between placebo and reb-oxy were found for BRSSEQ (Table 1 and Figure 2). The percent changes in BRSSEQ from supine to standing were also similar between placebo (+ 36% [+ 26 to + 53] %) and reb-oxy (+ 54% [+ 34 to + 71] %, p 0.13).
Baroreflex sensitivity by the spectral method. αLF percent change (left) and HLF percent change (right) from baseline under placebo (white bar) and reb-oxy (grey bar) in supine and standing positions. Data are shown as medians (median absolute deviation); the * indicates statistical significance between reb-oxy and placebo. See Table 4 for the original values.
Baroreflex sensitivity by the sequence method. BRSSEQ percent change from baseline under placebo (white bar) and reb-oxy (grey bar) in supine and standing positions. Data are shown as medians (standard error). See Table 4 for the original values. BRSSEQ percent change from baseline under placebo (white bar) and reb-oxy (grey bar) in supine and standing positions. Data are shown as medians (median absolute deviation).
Regarding the baroreflex resonance in BP spectral powers, SBPLF and DBPLF were significantly and substantially lower after reb-oxy treatment than on placebo in both postures (Table 1 and Figure 3). The percent changes in SBPLF from supine to standing were similar on placebo (− 86% [− 204 to − 28]) and on reb-oxy (− 108.1% [− 266 to − 35], p = 0.60). This was the case also for the percent changes in DBPLF from supine to standing (placebo: − 101% [− 153 to − 31] %; reb-oxy: − 72% [− 101 to − 43] %, p 0.52).
Baroreflex resonance. Percent changes of spectral powers in the low-frequency band for systolic (SBPLF, left) and diastolic (DBPLF, right) blood pressure from baseline in placebo (white bar) and reb-oxy (grey bar) in the supine and standing positions separately: data as medians (median absolute deviation). See Table 4 for the original values. The symbol * indicates statistical significance between reb-oxy and placebo.
Reb-oxy did not induce orthostatic hypotension nor any modification of parasympathetic activity indices. The respiratory frequencies remained in the HF band in all treatment groups.
Discussion
We recently demonstrated that one-week bedtime administration of reboxetine plus oxybutynin reduces OSA severity23. Here, we add that, in OSA patients, this treatment is not associated with short-term autonomic dysregulation. Particularly, during indirect evaluations, the tested drug combination does not induce either sympathetic overactivity or orthostatic hypotension as it could be expected by the reboxetine mechanism of action.
Our results show that one-week administration of reboxetine plus oxybutynin: (i) did not increase BP during the day or the night; (ii) did not enhance cardiac sympathetic modulation as reflected by nighttime HRV; (iii) did not impair but rather increased the sensitivity of the baroreflex control of heart rate; and (iv) decreased the baroreflex resonance in BP spectra, a surrogate measure for the vascular sympathetic modulation. To date, this is the first evaluation of the impact of the new OSA pharmacologic therapy on cardiovascular autonomic regulation.
Reboxetine is highly selective for norepinephrine transporters and has a low affinity with muscarinic, histamine-H1, and adrenergic α1 receptors36. Reboxetine is prescribed for major depressive diseases, dysthymia, and attention-deficit/hyperactivity disorder, its antidepressant effects being related to the sustained increase in norepinephrine levels in the central nervous system37. As a noradrenergic drug, reboxetine would be expected to increase sympathetic activity. In fact, in previous studies on healthy volunteers, 4 mg of reboxetine has been associated with an increase in HR38,39. Oxybutynin is an anticholinergic drug used for bladder over-activity. Its effect on muscarinic cardiac receptors determines inhibition of vagal activity with an increase in HR40. HR is indeed primarily modulated by the opposing autonomic influences of parasympathetic and sympathetic activity. Thus, theoretically, the administration of this drug combination would be expected to inhibit cardiac parasympathetic stimulation together with a direct sympathomimetic effect.
Reb-oxy and HR/BP levels in OSA
A previous pharmacological trial for OSA treatment showed that a single-night administration of atomoxetine plus oxybutynin in OSA patients led to a small (2.6 bpm) overnight increase in HR22. Similarly, in our study, HR during the night only slightly increased (by 3.7 bpm) on reb-oxy versus placebo during PSG. Moreover, the 24 h HR evaluated during the ABPM was similar in the two groups. Previous studies in healthy subjects reported an increase in SBP and DBP after reboxetine administration38,39,41, whereas neutral effects on BP have been reported in long-term treatment with reboxetine37,42,43. In our patients, BP did not differ between placebo and reb-oxy and we did not observe orthostatic hypotension after 1 week of reb-oxy administration, confirming the neutral effect previously reported even in a population of OSA patients. Morning surge and BP variability, additional markers of sympathetic activity, did not increase during reb-oxy administration, which, again, represents a reassuring clinical result considering the administration of a noradrenergic drug.
Reb-oxy and HRV in OSA
Using HRV analysis, OSA patients were shown to be characterized by a predominance of sympathetic markers and by a reduction in parasympathetic indices44,45,46. This is in line with the demonstration that sympathetic overactivity is a key mediator of adverse cardiovascular consequences in OSA47. In fact, autonomic derangement and sympathovagal imbalance are associated with arrhythmias, which are often observed in patients with OSA, contributing to their cardiovascular mortality48. Previous studies showed that reboxetine influences the autonomic nervous system by reducing the HF power of HRV in healthy volunteers39. Oxybutynin, in turn, showed an anti-cholinergic effect according to HRV indexes40. By contrast, our study points out that in OSA patients one week of reb-oxy did not increase sympathetic activity, as shown by no changes in the HRV spectral index of sympathovagal balance, i.e., the LF/HF power ratio, and had no significant influence on HRV indexes of parasympathetic cardiac control: RMSSD, pNN50, and the HF power.
Reb-oxy and arterial baroreflex cardiovascular modulation in OSA
An unbalanced cardiac baroreflex modulation has been shown to favor cardiovascular complications and arrhythmias. Particularly, in OSA patients the known reduction in BRS during both wake and sleep is associated with the development of arterial hypertension and with excessive daytime sleepiness24,49. Our study does not report any worsening of BRS after reb-oxy treatment, as it could be theoretically expected considering the autonomic effects of the noradrenergic reboxetine and anticholinergic oxybutynin. On the contrary, our data show a significantly improved sensitivity of arterial baroreflex modulation of HR, in particular in the LF band (αLF and HLF). It has been shown that αLF and HLF reflect baroreflex modulation of HR through both the sympathetic and the parasympathetic neural influences. Conversely, BRSSEQ mainly reflects the vagal HR modulation50. Thus, our findings of increased αLF and HLF accompanied by no changes in BRSSEQ suggest that one-week treatment with reb-oxy improved BRS mainly through a reduction of cardiac sympathetic modulation, with no evident changes in vagal control of HR.
Moreover, our study demonstrates that reb-oxy largely decreased the power of SBP and DBP oscillations at LF, which have been suggested to be an expression of the resonance in the baroreflex loop at a frequency of 0.1 Hz, considered a surrogate measure for sympathetic vascular regulation. Thus, when considering all the above findings, our study suggests the occurrence of a reduction in the overactivity of sympathetic cardiovascular control induced by sleep apneas in OSA patients after one week of reb-oxy treatment. This reduction, however, was not accompanied by major alterations in posture-induced changes in cardiovascular control, as demonstrated by the lack of orthostatic hypotension and other signs of autonomic imbalance.
The improvement in baroreflex cardiac modulation we observed during wake is likely to represent a positive consequence of nocturnal apneas reduction, as previously reported after long-term OSA treatment with CPAP12. Thus, similarly to what happens with CPAP treatment, it might be supposed that the beneficial effect of drug combination on the severity of OSA would have mitigated the sympathetic hyperactivity induced by OSA events9,12,51. The reduction of the hypoxic burden, together with a reduced frequency of arousals from sleep determined by reb-oxy, might have determined the beneficial effect on the apnea-hypopnea-related sympathetic overflow52,53.
Limitations
Even if the present study offers unique data on the effects of a novel drug treatment for OSA over the longest administration period tested so far, we acknowledge a few limitations. First, our findings on the short-term impact of Reb-Oxy on cardiac autonomic modulation in OSA patients cannot be generalize to other populations and need to be confirmed over a longer period. Second, the relatively small sample size was powered to detect significant changes in AHI, not in baroreflex or HRV indices, possibly precluding the detection of smaller effects of the treatment. Third, by study design we evaluated cardiovascular autonomic modulations only by indirect measures, as direct measures of sympathetic activity such as norepinephrine spillover or muscle sympathetic nerve traffic were excluded.
Conclusions
We demonstrate for the first time that the combination of the noradrenergic drug reboxetine and the anticholinergic drug oxybutynin could safely be administrated in OSA patients, who are typically characterized by sympathetic overactivity due to sleep apnea per se. Being efficacious on OSA severity, these drugs could also positively act to improve the deranged cardiovascular autonomic modulation typical of OSA. Future intervention trials, including a larger number of OSA patients followed over longer treatment periods are needed to assess whether these favorable clinical and pathophysiological effects are also associated with a reduction in cardiovascular morbidity and mortality.
Data availability
Data used for this study are available from the corresponding author upon reasonable request.
References
Benjafield, A. V. et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 7, 687–698. https://doi.org/10.1016/s2213-2600(19)30198-5 (2019).
Somers, V. K., Dyken, M. E., Clary, M. P. & Abboud, F. M. Sympathetic neural mechanisms in obstructive sleep apnea. J. Clin. Invest. 96, 1897–1904. https://doi.org/10.1172/jci118235 (1995).
Nieto, F. J. et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 283, 1829–1836. https://doi.org/10.1001/jama.283.14.1829 (2000).
Sánchez-de-la-Torre, M., Campos-Rodriguez, F. & Barbé, F. Obstructive sleep apnoea and cardiovascular disease. Lancet Respir. Med. 1, 61–72. https://doi.org/10.1016/s2213-2600(12)70051-6 (2013).
Shahar, E. et al. Sleep-disordered breathing and cardiovascular disease: Cross-sectional results of the Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 163, 19–25. https://doi.org/10.1164/ajrccm.163.1.2001008 (2001).
Somers, V. K. et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College Of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council On Cardiovascular Nursing. In collaboration with the National Heart, Lung, and Blood Institute National Center on Sleep Disorders Research (National Institutes of Health). Circulation 118, 1080–1111. https://doi.org/10.1161/circulationaha.107.189375 (2008).
Marin, J. M., Carrizo, S. J., Vicente, E. & Agusti, A. G. N. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: An observational study. Lancet 365, 1046–1053. https://doi.org/10.1016/S0140-6736(05)71141-7 (2005).
Roche, F. et al. Reduced cardiac sympathetic autonomic tone after long-term nasal continuous positive airway pressure in obstructive sleep apnoea syndrome. Clin. Physiol. 19, 127–134. https://doi.org/10.1046/j.1365-2281.1999.00163.x (1999).
Bonsignore, M. R. et al. Baroreflex control of heart rate during sleep in severe obstructive sleep apnoea: Effects of acute CPAP. Eur. Respir. J. 27, 128–135. https://doi.org/10.1183/09031936.06.00042904 (2006).
Parati, G. et al. Autonomic cardiac regulation in obstructive sleep apnea syndrome: Evidence from spontaneous baroreflex analysis during sleep. J. Hypertens 15, 1621–1626. https://doi.org/10.1097/00004872-199715120-00063 (1997).
Parati, G. et al. Evaluation of the baroreceptor-heart rate reflex by 24-hour intra-arterial blood pressure monitoring in humans. Hypertension 12, 214–222. https://doi.org/10.1161/01.hyp.12.2.214 (1988).
Bonsignore, M. R. et al. Continuous positive airway pressure treatment improves baroreflex control of heart rate during sleep in severe obstructive sleep apnea syndrome. Am. J. Respir. Crit. Care Med. 166, 279–286. https://doi.org/10.1164/rccm.2107117 (2002).
Archbold, K. H. & Parthasarathy, S. Adherence to positive airway pressure therapy in adults and children. Curr. Opin. Pulm. Med. 15, 585–590 (2009).
Rapelli, G. et al. Improving CPAP adherence in adults with obstructive sleep apnea syndrome: A scoping review of motivational interventions. Front Psychol 12, 705364. https://doi.org/10.3389/fpsyg.2021.705364 (2021).
Perger, E., Jutant, E. M. & Redolfi, S. Targeting volume overload and overnight rostral fluid shift: A new perspective to treat sleep apnea. Sleep Med. Rev. 42, 160–170. https://doi.org/10.1016/j.smrv.2018.07.008 (2018).
Taranto-Montemurro, L., Messineo, L. & Wellman, A. Targeting endotypic traits with medications for the pharmacological treatment of obstructive sleep apnea. A review of the current literature. J. Clin. Med. 8, 1. https://doi.org/10.3390/jcm8111846 (2019).
Perger, E. & Taranto-Montemurro, L. Upper airway muscles: Influence on obstructive sleep apnoea pathophysiology and pharmacological and technical treatment options. Curr. Opin. Pulm. Med. https://doi.org/10.1097/mcp.0000000000000818 (2021).
Eckert, D. J., White, D. P., Jordan, A. S., Malhotra, A. & Wellman, A. Defining phenotypic causes of obstructive sleep apnea. Identification of novel therapeutic targets. Am. J. Respir. Crit. Care Med. 188, 996–1004. https://doi.org/10.1164/rccm.201303-0448OC (2013).
Pini, L. et al. Phenotyping OSAH patients during wakefulness. Sleep Breath https://doi.org/10.1007/s11325-021-02551-5 (2022).
Chan, E., Steenland, H. W., Liu, H. & Horner, R. L. Endogenous excitatory drive modulating respiratory muscle activity across sleep-wake states. Am. J. Respir. Crit. Care Med. 174, 1264–1273. https://doi.org/10.1164/rccm.200605-597OC (2006).
Grace, K. P., Hughes, S. W. & Horner, R. L. Identification of the mechanism mediating genioglossus muscle suppression in REM sleep. Am. J. Respir. Crit. Care Med. 187, 311–319. https://doi.org/10.1164/rccm.201209-1654OC (2013).
Taranto-Montemurro, L. et al. The combination of atomoxetine and oxybutynin greatly reduces obstructive sleep apnea severity. A randomized, placebo-controlled, double-blind crossover trial. Am. J. Respir. Crit. Care Med. 199, 1267–1276. https://doi.org/10.1164/rccm.201808-1493OC (2019).
Perger, E. et al. Reboxetine plus oxybutynin for obstructed sleep apnea treatment A 1-week randomized, placebo-controlled, double-blind crossover trial. Chest https://doi.org/10.1016/j.chest.2021.08.080 (2021).
Cortelli, P., Lombardi, C., Montagna, P. & Parati, G. Baroreflex modulation during sleep and in obstructive sleep apnea syndrome. Auton. Neurosci. 169, 7–11. https://doi.org/10.1016/j.autneu.2012.02.005 (2012).
Tank, J. et al. Selective impairment in sympathetic vasomotor control with norepinephrine transporter inhibition. Circulation 107, 2949–2954. https://doi.org/10.1161/01.CIR.0000072786.99163.FE (2003).
Parati, G., Mancia, G., Di Rienzo, M. & Castiglioni, P. Point: Cardiovascular variability is/is not an index of autonomic control of circulation. J. Appl. Physiol. (1985) 101, 676–678. https://doi.org/10.1152/japplphysiol.00446.2006 (2006) (discussion 681–672).
La Rovere, M. T., Pinna, G. D. & Raczak, G. Baroreflex sensitivity: Measurement and clinical implications. Ann. Noninvasive Electrocardiol. 13, 191–207. https://doi.org/10.1111/j.1542-474X.2008.00219.x (2008).
Electrophysiology, T. F. o. t. E. S. o. C. t. N. A. S. o. P. Heart rate variability. Circulation 93, 1043–1065, https://doi.org/10.1161/01.CIR.93.5.1043 (1996).
Sateia, M. J. International classification of sleep disorders-third edition: Highlights and modifications. Chest 146, 1387–1394. https://doi.org/10.1378/chest.14-0970 (2014).
Rosenberg, R. S. & Van Hout, S. The American academy of sleep medicine inter-scorer reliability program: Respiratory events. J. Clin. Sleep Med. 10, 447–454. https://doi.org/10.5664/jcsm.3630 (2014).
Moody, G. B. et al. Clinical Validation of the ECG-Derived Respiration (EDR) Technique; Computers in Cardiology, vol. 13, pp. 507–510 (Washington, DC: IEEE Computer Society Press, 1986).
Parati, G. Arterial baroreflex control of heart rate: Determining factors and methods to assess its spontaneous modulation. J. Physiol. 565, 706–707. https://doi.org/10.1113/jphysiol.2005.086827 (2005).
Robbe, H. W. et al. Assessment of baroreceptor reflex sensitivity by means of spectral analysis. Hypertension 10, 538–543. https://doi.org/10.1161/01.HYP.10.5.538 (1987).
Pagani, M. et al. Changes in autonomic regulation induced by physical training in mild hypertension. Hypertension 12, 600–610. https://doi.org/10.1161/01.HYP.12.6.600 (1988).
Julien, C. The enigma of Mayer waves: Facts and models. Cardiovasc. Res. 70, 12–21. https://doi.org/10.1016/j.cardiores.2005.11.008 (2006).
Wong, E. H. et al. Reboxetine: A pharmacologically potent, selective, and specific norepinephrine reuptake inhibitor. Biol. Psych. 47, 818–829. https://doi.org/10.1016/s0006-3223(99)00291-7 (2000).
Fossa, A. A. et al. Improved preclinical cardiovascular therapeutic indices with long-term inhibition of norepinephrine reuptake using reboxetine. Toxicol Appl. Pharmacol. 264, 343–350. https://doi.org/10.1016/j.taap.2012.09.010 (2012).
Schroeder, C. et al. Selective norepinephrine reuptake inhibition as a human model of orthostatic intolerance. Circulation 105, 347–353. https://doi.org/10.1161/hc0302.102597 (2002).
Penttilä, J., Syvälahti, E., Hinkka, S., Kuusela, T. & Scheinin, H. The effects of amitriptyline, citalopram and reboxetine on autonomic nervous system. Psychopharmacology 154, 343–349. https://doi.org/10.1007/s002130000664 (2001).
Akbari, E., Zare, A. H. & Alipour, A. The effect of oxybutynin on cardiac autonomic modulation in healthy subjects. Clin. Auton. Res. 24, 167–174. https://doi.org/10.1007/s10286-014-0247-9 (2014).
Denolle, T., Pellizzoni, C., Jannuzzo, M. G. & Poggesi, I. Hemodynamic effects of reboxetine in healthy male volunteers. Clin. Pharmacol. Ther. 66, 282–287. https://doi.org/10.1016/s0009-9236(99)70036-6 (1999).
Riahi, F., Tashakori, A., Izadi-Mazidi, S. & Salehi-Veysi, M. Effectiveness of reboxetine in treatment of outpatient children and adolescents with attention deficit-hyperactivity disorder with comorbid anxiety disorders. Iran J. Psych. 8, 195–200 (2013).
Agelink, M. W., Ullrich, H., Baumann, B., Strum, S. & Majewski, T. Effects of reboxetine, a selective norepinephrine reuptake inhibitor, on sympathetic and parasympathetic outflow to the heart: Preliminary data. Psychopharmacology 163, 151–156. https://doi.org/10.1007/s00213-002-1146-7 (2002).
Sequeira, V. C. C., Bandeira, P. M. & Azevedo, J. C. M. Heart rate variability in adults with obstructive sleep apnea: A systematic review. Sleep Sci. 12, 214–221. https://doi.org/10.5935/1984-0063.20190082 (2019).
Taranto-Montemurro, L. et al. Cardiac sympathetic hyperactivity in patients with chronic obstructive pulmonary disease and obstructive sleep apnea. COPD 13, 706–711. https://doi.org/10.1080/15412555.2016.1199668 (2016).
Vena, D. et al. Heart rate variability responses of individuals with and without saline-induced obstructive sleep apnea. J. Clin. Sleep Med. 14, 503–510. https://doi.org/10.5664/jcsm.7032 (2018).
Javaheri, S. et al. Sleep apnea: Types, mechanisms, and clinical cardiovascular consequences. J. Am. Coll. Cardiol. 69, 841–858. https://doi.org/10.1016/j.jacc.2016.11.069 (2017).
May, A. M., Van Wagoner, D. R. & Mehra, R. OSA and cardiac arrhythmogenesis: Mechanistic insights. Chest 151, 225–241. https://doi.org/10.1016/j.chest.2016.09.014 (2017).
Lombardi, C. et al. Daytime sleepiness and neural cardiac modulation in sleep-related breathing disorders. J. Sleep Res. 17, 263–270. https://doi.org/10.1111/j.1365-2869.2008.00659.x (2008).
Silva, L. E. V., Dias, D. P. M., da Silva, C. A. A., Salgado, H. C. & Fazan, R. Revisiting the sequence method for baroreflex analysis. Front. Neurosci. 1, 3. https://doi.org/10.3389/fnins.2019.00017 (2019).
Narkiewicz, K. et al. Nocturnal continuous positive airway pressure decreases daytime sympathetic traffic in obstructive sleep apnea. Circulation 100, 2332–2335. https://doi.org/10.1161/01.cir.100.23.2332 (1999).
Ferreira, C. B., Schoorlemmer, G. H., Rocha, A. A. & Cravo, S. L. Increased sympathetic responses induced by chronic obstructive sleep apnea are caused by sleep fragmentation. J. Appl. Physiol. 129, 163–172. https://doi.org/10.1152/japplphysiol.00811.2019 (2020).
Azarbarzin, A. et al. The hypoxic burden of sleep apnoea predicts cardiovascular disease-related mortality: The osteoporotic fractures in men study and the sleep heart health study. Eur. Heart J. 40, 1149–1157. https://doi.org/10.1093/eurheartj/ehy624 (2019).
Funding
Apnimed Inc. (20 Holyoke St, Cambridge, MA 02138) financially supported the realization of the study and partially supported by the Italian Ministry of Health.
Author information
Authors and Affiliations
Contributions
E.P., C.L., and G.P. contributed to study design, E.P., D.R., S.V. contributed to study execution. E.P., P.C., D.S., A.Z., A.F., C.L., P.M., S.C and C.B contributed to data analysis. E.P. and L.P. contributed to drafting of the manuscript. P.C., D.S., P.M., A.A., S.C, C.B. and A.F. contributed to revision and G.P., P.C. and C.L. contributed to final drafting of the manuscript.
Corresponding author
Ethics declarations
Competing interests
E.P., P.C., D.S., A.Z., D.R., S.V., A.F., P.M., L.P., S.C, C.B., C.L., and G.P. have no conflict of interest related to the current project. A.A. served as consultant for Somnifix, Apnimed, Inspire, and LinguaFlex and reports grants from Somnifix, outside the current work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Perger, E., Castiglioni, P., Faini, A. et al. Impact of reboxetine plus oxybutynin treatment for obstructive sleep apnea on cardiovascular autonomic modulation. Sci Rep 13, 3178 (2023). https://doi.org/10.1038/s41598-023-29436-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-29436-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.