Abstract
Lymph node metastases are common in malignant neoplasms of head and neck. Since cervical lymph nodes (cLN) are localized superficially, ultrasound (US) represents the primary imaging modality. The aim of the study is to report the value of US and contrast-enhanced ultrasound (CEUS) and their diagnostic confidence in the characterization of inconclusive cLN. A systematic review was performed using the literature data base PubMed. Results were filtered (published in a peer-reviewed journal, full-text available, published within the last ten years, species human, English or German full-text) and inclusion criteria were clearly defined (cohort with lymphadenopathy or malignancy in head and neck ≥ 50 patients, histological confirmation of malignant imaging findings, performance of CEUS as outcome variable). The results were quantified in a meta-analysis using a random-effects model. Overall, five studies were included in qualitative and quantitative analysis. The combination of non-enhanced US and CEUS enlarges the diagnostic confidence in the characterization of lymph nodes of unclear dignity. The pooled values for sensitivity and specificity in the characterization of a malignant cervical lymph node using US are 76% (95%-CI 66–83%, I2 = 63%, p < 0.01) and 80% (95%-CI 45–95%, I2 = 92%, p < 0.01), compared to 92% (95%-CI 89–95%, I2 = 0%, p = 0.65) and 91% (95%-CI 87–94%, I2 = 0%, p = 0.40) for the combination of US and CEUS, respectively. Consistent results of the included studies show improved diagnostic performance by additional CEUS. Nevertheless, more prospective studies are needed to implement CEUS in the diagnostic pathway of cLN.
Similar content being viewed by others
Introduction
Cervical lymph node (cLN) metastases are common in patients with malignant head and neck neoplasms especially in squamous cell carcinomas (HNSCC) of the upper aerodigestive tract1. In only 1% of the cases, the primary cause of cLN metastasis is found extracervical, among them in tumors of breast, lung, gastrointestinal tract, urogenital tract and central nervous system1. Besides cLN metastases and benign causes like infections, malignant lymphoma can be a cause of cervical lymphadenopathy as well and must be taken into consideration at differential diagnosis1,2. In 2016, neoplasia of oral cavity and pharynx were the eighth most frequent cancer in men and thyroid neoplasia was the fifth common cancer in women, respectively in the United States3.
Criteria for malignant cLN transformation in B-mode US are round shape, calcifications and heterogenic with hyperechogenic or cystic changes4. Leng et al. reported a sensitivity of 84% (95% CI: 67–93%) and specificity of 93% (95% CI: 90–95%) using US investigating the detection of cLN metastases in patients with esophageal carcinoma using a cut-off value of 5 mm cLN size5.
Over the last decade, the use of contrast-enhanced ultrasound (CEUS) for characterization of focal lesions especially in liver and kidney increased, representing an additional contrast-enhanced modality beside CT (computed tomography) and MRI (magnetic resonance imaging) in the diagnostic pathway for detection of malignant lesions6.
The present article highlights the additional diagnostic value of CEUS in inconclusive cLN by a systematic review of the current literature with meta-analysis.
Material and methods
Data source and literature search
The systematic literature research was performed by using the literature data base PubMed. Allowing a preferably extensive search, the request was composed with synonyms (Table 1).
Hence resulting in the following search request:
((CEUS) OR (contrast-enhanced ultrasound)) AND ((lymph node) OR (lymph nodes)) AND ((cervical) OR (neck))
The results were restricted using additional filters in PubMed: Articles being available in full text (until the 17th March 2020), published maximum 10 years ago (reflecting the rapid technical progress in CEUS), examining humans and written in English or German. All results were assessed by two authors (*blinded*) independently.
Selection of studies and criteria
Only original scientific articles being published in peer-review journals were considered. A further inclusion criterium was the patient cohort which must consist of patients with (i) cervical lymphadenopathy, (ii) malignancy in head and neck and (iii) must include a minimum of 50 patients. Histological confirmation was taken as gold standard acquired by biopsy or surgical removal. In case of benign initial imaging result, an additional sonographic follow-up of at least two years was permitted due to an overall low number of available studies addressing the issue of the present review. The studies can be designed both pro- and retrospectively. The target variable must be the diagnostic performance of CEUS, respectively in comparison to prior US.
Assessment of the risk of bias
The risk of bias was assessed using the QUADAS-2 (Quality Assessment of Diagnostic Accuracy Studies)7. Therefore, the included studies were evaluated concerning patient selection, the index test, the reference standard as well as flow and timing7.
Review of single qualitative and quantitative parameters
Individual parameters used the differentiation of malignant and benign cLN in US, CEUS and connected post-processing analyses (such as time-intensity-curve [TIC] models) were extracted from the included studies if parameters showed a significance level of α ≤ 0.05. The extraction of diagnostic accuracy from the original publications (four-field tables) was either performed by number of cLN or patients included, depending on the authors individual choices.
Meta-analysis
With the aim of quantifying the results obtained (sensitivity and specificity of the modalities to be compared), a meta-analysis was carried out comparing the modalities US, CEUS and combination of US and CEUS. For this purpose, the function “metaprop” from the R package “meta” was used and modelling was performed using a random intercept logistic regression model (random effects model)8. I2 was determined as a measure of heterogeneity as well as τ2 as a measure of between-study variance with p-value. The calculated parameters were interpreted using accepted references9,10.
Results
Choice of the included studies
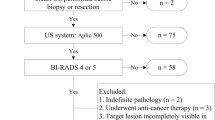
In the query a total of n = 246 publications were obtained. After application of the described filters in PubMed, n = 126 results remained. The selection procedure is visualized in a flow-chart which is based on the PRISMA-scheme (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) (Fig. 1)11.
PRISMA-scheme of the systematic literature review. Presented is the PRISMA-scheme of the systematic literature review, inspired by Moher et al.11.
Beside the 126 results found via PubMed, a publication of Chen et al. has been taken into consideration due to author’s precognition12. From these overall 127 results, ten articles have been preselected due to thematic accordance via screening of the abstracts12,13,14,15,16,17,18,19,20,21.
After screening, five studies were excluded regarding the mentioned inclusion criteria. Mansour et al. investigated ultrasonographic hypoechoic head and neck lesions with less than 50 patients with cLN disease included16. Zhan et al. did not examine the diagnostic performance of CEUS, but performed a multivariate analysis predicting LN metastasis by examining papillary thyroid cancer with CEUS13. Similar, Zhang et al. explored the prediction of LN metastases by examining papillary thyroid cancer with CEUS and must be excluded since its target variable is not the diagnostic performance of CEUS in the characterization of cLN15. Dudau et al. published a study examining if CEUS can distinguish malignant from reactive LN in patients with head and neck cancer, but had to be excluded due to the small number of patients included (n = 17)20. Wendl et al. described preoperative use of CEUS and MRI in characterizing LN, but had to be excluded due to a small cohort of only 10 patients as well21.
Finally, five remaining articles were assessed for their eligibility. All of them were judged as permissible for qualitative and quantitative assessment fulfilling all inclusion criteria mentioned above12,14,17,18,19.
Results of studies included
An overview of the included studies outlining their characteristic is given in Table 2. All studies used 1.0–2–4 mL of SonoVue® (Bracco, Milan, Italy) as contrast agent for CEUS. Quantitative results are presented in Fig. 2 and qualitative results are presented in Table 4.
Summary of the diagnostic accuracy of the compared modalities and associated forest plots. The forest plots of the individual compared modalities belonging to the meta-analysis are shown. A distinction is made between non-enhanced US (a, b), CEUS only (c, d) and their combination (e, f). In each group, the achieved sensitivities (a, c, e) and the specificities (b, d, f) are shown. The width of the individual plots lines is determined by the 95%-CI.
Poanta et al. investigated the role of CEUS in the differentiation between benign and malignant cLN in the differential diagnosis of superficial lymphadenopathy. The authors used receiver operating characteristic (ROC) analysis to receive sensitivity and specificity of sonographic parameters. The authors found CEUS to be especially useful in case of uncertain B-Mode-US investigation results19.
On the other hand, Xiang et al. researched the diagnostic value of CEUS in patients with thyroid cancer. There was no statistical analysis according to statistical significance of qualitative non-enhanced sonographic findings except cLN diameter performed, so only CEUS’ enhancement pattern is presented in this review. The authors sum up centripetal enhancement pattern, microcalcifications as well as perfusion defects as specific malignant criteria18.
Hong et al. also studied cLN in patients with papillary thyroid cancer (PTC) metastases. The results are in line with the previous studies, as centripetal enhancement, hyperenhancement and perfusion defects were also found as significant features. In addition, the authors emphasized the importance of a ring-enhancing margin in malignant cLN14.
Cui et al. examined the diagnostic value of CEUS in the differentiation between metastatic and tuberculous cLN. As described by Poanta et al. quantitative TIC parameters were also found to be significant in this particular cohort. Diagnostic accuracy was particularly enhanced by the use of CEUS, which highlights the diagnostic difficulties associated with tuberculous cLN17.
Chen et al. like Hong et al. studied a cohort with cLN metastasis from PTC. Regarding the qualitative CEUS characteristics, the results overlap with previous studies, but the authors did not find any quantitative CEUS parameters to be statistically significant12.
Assessment of the risk of bias
The assessment regarding the risk of bias in the included studies results in an overall picture of applicability. An overview of the categories and studies following the suggestions of QUADAS-27 is presented in Table 3.
The studies by Poanta et al. and Chen et al. were assessed to fit the question of the review well showing low risk of bias in all assessed categories12,19. In the study by Xiang et al. the diagnostic accuracy was evaluated according to the number of patients included, but not according to the larger number of cLN examined—nevertheless, this study fits well with the research question of the review18. In the study by Hong et al. it is striking that not all patients received the same reference standard (although it was not stated how many patients were allocated to the benign cohort solely by follow-up)14. However, it is estimated that an imaging follow-up over two years for initial suspicion of a benign cLN represents a pragmatic approach that overall fits well with the question of the review14. The study by Cui et al. generally fits well with the question of the review, but it examines a pre-selected cohort in which only tuberculous cLN were included in the benign cohort17. As a result, the patient selection is at risk of bias. Nevertheless, the present review is not limited to tuberculous cLN in the case of benign cLN—which, however, represents a decisive component of this group17.
Despite the partial risk of bias, all studies are included in the qualitative and quantitative analysis, due to the limited number of available studies and also because Whiting et al.7 describe this as preferable. Possible heterogeneities are discussed separately.
Qualitative results of the studies
The qualitative results of the studies—in the sense of image-morphological criteria of malignant cLN—are presented In Table 4. Therefore, statistically significant (p ≤ 0.05) characteristics of metastatic cLN are listed.
Meta-analysis
In addition to the qualitative results of the individual included studies as presented in Table 4, the pooled data calculated with a random effects model for the three different imaging modalities investigated are shown in Fig. 2.
For non-enhanced US, the pooled sensitivity was 76% (95%-CI 66–83%, I2 = 63%, p < 0.01) and the specificity 80% (95%-CI 45–95%, I2 = 92%, p < 0.01) showing a high heterogeneity.
Considering CEUS alone in the determination of the dignity of cLN, three of the five included studies provided results that showed increased pooled diagnostic performance. The sensitivity reached a value of 84% (95%-CI 79–88%, I2 = 0%, p = 0.61) and the specificity 87% (95%-CI 70–95%, I2 = 74%, p < 0.01). Heterogeneity decreased sharply in the case of sensitivity, whereas it remained high in the case of specificity.
A total of four of the included studies investigated diagnostic accuracy using the combination of US and CEUS. This resulted in the highest diagnostic accuracy of the present analysis represented by a sensitivity of 92% (95%-CI 89–95%, I2 = 0%, p = 0.65) and specificity of 91% (95%-CI 87–94%, I2 = 0%, p = 0.40). Overall, the heterogeneity can be assessed as low.
Discussion
The results of the present review can be summarized as follows: (I) The diagnostic performance of cLN sonography rises by using CEUS instead of US, whereas its combination constitutes the best diagnostic option among the modalities examined in this meta-analysis and is accompanied by the lowest heterogeneity among the studies included. (II) One included study found no statistically significant characteristics in non-enhanced US to determine a cLN entity in subgroup of metastatic versus tuberculous lymph nodes17. Three other studies included found different and partly contradicting results, whereas in particular a L/S-ratio < 2 (ratio of long-axis and short-axis diameter) and atypical margins form the overlapping set12,14,19. (III) As a qualitative CEUS characteristic, all but one study found inhomogeneous enhancement as a statistically significant pattern12,14,18,19. The studies which included quantitative CEUS characteristics produced different results in terms of statistical significance of TIC parameters12,17,19.
In 2014, Ying et al. published a systematic literature review examining the value of US, CEUS and elastography in the assessment of cLN22. They state that the improvement of the diagnostic performance by adding CEUS to US is evaluated as controversial with inconsistent results of the included studies22. Our results show no contradiction with enlarging sensitivity and specificity in all included studies also presented for the pooled values in the meta-analysis. Mei et al. investigated in 2018 in a meta-analysis the diagnostic accuracy of CEUS in differential diagnosis of superficial LN including head and neck area as well as axillar and groin LN23. In conclusion, they found a sensitivity of 88% (95%-CI 83–92%) and a specificity of 80% (95%-CI 74–85%) for CEUS which is a lower accuracy compared to the present results23. Additionally, we performed a comparison of US, CEUS and their combination. Nevertheless, the external validity regarding CEUS’ diagnostic accuracy in differential diagnosis of cLN can be assessed as sufficient.
In particular, analysis of perfusion using TIC parameters offers the opportunity to quantify sonographic findings, which could decrease one of the well-known disadvantages of diagnostic US—the operator dependency—by generating objective parameters. In this context, however, the partly contradictory results regarding dedicated TIC parameters of the included studies of the present review must be considered12,17,19. A possible reason for these results can be the partially different concept of data collecting: Cui et al. compared the cLN’s perfusion with the perfusion of the carotid artery’s perfusion, whereas Chen et al. captured parameters which are independent of the surrounding tissue’s perfusion such as peak intensity, time to peak, mean transit time and rise time12,17. Poanta et al. also used parameters that were independent of the enhancement of the environment19. So, these parameters could balance the examiner dependance in future, but for this purpose, it is necessary that future studies collect corresponding parameters as uniformly as possible.
Even if there is greater evidence for the usability of TIC parameters in the future, their sole use should be questioned. Ultimately, these parameters—even if their objectivity seems tempting—should always be correlated with US characteristics and patients’ history or paraclinical findings. On the one hand, CEUS is always preceded by a US examination, and on the other hand, our results suggest that the combination of both modalities should generally be considered. At the same time, we showed a significantly reduced heterogeneity of the included studies for the combined use of US and CEUS, which increases the significance of this effect (Fig. 2).
However, it has to be mentioned that the heterogeneity of the studies in the field of B-Mode US is mainly due to the deviating sensitivity and specificity reported by Cui et al.17 The increase in accuracy in combination with CEUS is then striking, so that the study joins the results of the other studies with a heterogeneity of I2 = 0% for sensitivity and specificity, respectively.
Of course, differentiation of tuberculous and malignant LN is particularly difficult. Moon et al. emphasize the particular importance of a correct diagnosis of tuberculous lymphadenitis, as this requires special therapy24. The authors investigated a specific US study protocol evaluated in an endemic area showing a sensitivity and specificity > 90% for the diagnosis of nontuberculous benign, tuberculous and malignant LN, respectively24. This is another indication of the advantageousness of using standardized protocols, as discussed above for TIC.
A general benefit of CEUS among tomographic contrast-enhanced imaging modalities is the low adverse-event rate and pulmonary elimination of injected microbubbles: Tang et al. describe in retrospective study containing more than 30 000 patients CEUS’ contrast agent as good and quantify the rate of side effects to 0.020%25. Piscaglia et al. come to a similar result and state the rate of side effects after evaluation of more than 23 000 patients to 0.0086%26.
Additionally, contrast agent of CEUS can be given to patients with chronic renal insufficiency as well since it is eliminated by the lungs27. Concerning iodine-containing contrast agents of CT, the incidence of contrast-induced nephropathy (CIN) has been described to be 2–12%28. Moreover, these contrast agents cause complicated application in patients with hyperthyroidism—additionally, in clinical practice, in younger patients the application of CT scans is more restrained because of the associated radiation exposure.
Even though these problems are completely avoided with MRI, there is a more complicated handling of imaging in patients with claustrophobia—whose event rate was quantified at 9.8%29—or in patients with pacemaker. This underlines once again why, given the good pooled diagnostic accuracy of the present review, the examination of cLN by CEUS should be pursued, as this modality can facilitate and expedite procedures. As recently published, CEUS showed superior cost effectiveness compared to contrast-enhanced CT and MRI in the characterization of focal lesions on the example of cystic renal lesions30.
Despite the promising results and the low calculated heterogeneity in the case of the combination of US and CEUS, the present review is primarily limited regarding the low number of included studies and therefore the low number of patients examined. However, this limitation can be somewhat appeased: Jackson et al. described that at least five studies are needed to map into a random effects model with an overall larger effect than the individual included studies31. Nevertheless, each of the included studies also described an increase in diagnostic accuracy using CEUS (Fig. 2).
Uniting the small patient numbers and the promising results, larger prospective studies are needed to confirm present results. Newer applications such as shear wave elastography (SWE) should also be captured to generate more quantitative sonographic parameters. Since this tool is easy to perform and free of side effects, it should be registered in an approach of multiparametric ultrasound (mpUS) as well6.
Indeed, mpUS would not remove histology as gold standard, but could reduce the number of necessary invasive diagnostic interventions.
In conclusion, the present review shows an increased diagnostic accuracy when adding CEUS to standard US examinations in the assessment of inconclusive cLN. If further prospective studies show congruence, they could form the foundation for an improved sonographic characterization.
Abbreviations
- CEUS:
-
Contrast-enhanced ultrasound
- cLN:
-
Cervical lymph node
- CT:
-
Computed tomography
- HNSCC:
-
Head and neck squamous cell carcinoma
- LN:
-
Lymph node
- MRI:
-
Magnetic resonance imaging
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- PTC:
-
Papillary thyroid cancer
- QUADAS:
-
Quality assessment of diagnostic accuracy studies
- ROC:
-
Receiver operating characteristic
- SWE:
-
Shear wave elastography
- TIC:
-
Time intensity curve
- US:
-
Ultrasound
References
Lopez, F. et al. Cervical lymph node metastases from remote primary tumor sites. Head Neck 38(Suppl 1), E2374–E2385 (2016).
Nagarkar, R., Wagh, A., Kokane, G., Roy, S. & Vanjari, S. Cervical lymph nodes: A hotbed for metastasis in malignancy. Indian J. Otolaryngol. Head Neck Surg. 71, 976–980 (2019).
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2016. CA. Cancer J. Clin. 66, 7–30 (2016).
Lee, D. W. et al. Roles of ultrasonography and computed tomography in the surgical management of cervical lymph node metastases in papillary thyroid carcinoma. Eur. J. Surg. Oncol. 39, 191–196 (2013).
Leng, X.-F. et al. Accuracy of ultrasound for the diagnosis of cervical lymph node metastasis in esophageal cancer: A systematic review and meta-analysis. J. Thorac. Dis. 8, 2146–2157 (2016).
Sidhu, P. S. Multiparametric ultrasound (MPUS) imaging: Terminology describing the many aspects of ultrasonography. Ultraschall Med. 36, 315–317 (2015).
Whiting, P. F. et al. QUADAS-2: A revised tool for the quality assessment of diagnostic accuracy studies. Ann. Intern. Med. 155, 529–536 (2011).
R Core Team (2020). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
Sedgwick, P. How to read a forest plot in a meta-analysis. BMJ 351, h4028 (2015).
Higgins, J. P. T., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 6, e1000097 (2009).
Chen, L., Chen, L., Liu, J., Wang, B. & Zhang, H. Value of qualitative and quantitative contrast-enhanced ultrasound analysis in preoperative diagnosis of cervical lymph node metastasis from papillary thyroid carcinoma. J. Ultrasound Med. 39, 73–81 (2019).
Zhan, J., Diao, X., Chen, Y., Wang, W. & Ding, H. Predicting cervical lymph node metastasis in patients with papillary thyroid cancer (PTC)—Why contrast-enhanced ultrasound (CEUS) was performed before thyroidectomy. Clin. Hemorheol. Microcirc. 72, 61–73 (2019).
Hong, Y.-R. et al. Role of contrast-enhanced ultrasound in the pre-operative diagnosis of cervical lymph node metastasis in patients with papillary thyroid carcinoma. Ultrasound Med. Biol. 43, 2567–2575 (2017).
Zhang, Y. et al. Values of ultrasound features and MMP-9 of papillary thyroid carcinoma in predicting cervical lymph node metastases. Sci. Rep. 7, 6670 (2017).
Mansour, N. et al. Differentiation of ultrasonographic hypoechoic head and neck lesions. Laryngorhinootologie 98, 701–707 (2019).
Cui, Q.-L. et al. Diagnostic value of contrast-enhanced ultrasonography and time-intensity curve in differential diagnosis of cervical metastatic and tuberculous lymph nodes. J. Ultrasound Med. 37, 83–92 (2018).
Xiang, D. et al. Contrast-enhanced ultrasound (CEUS) facilitated US in detecting lateral neck lymph node metastasis of thyroid cancer patients: diagnosis value and enhancement patterns of malignant lymph nodes. Eur. Radiol. 24, 2513–2519 (2014).
Poanta, L. et al. The place of CEUS in distinguishing benign from malignant cervical lymph nodes: A prospective study. Med. Ultrason. 16, 7–14 (2014).
Dudau, C. et al. Can contrast-enhanced ultrasound distinguish malignant from reactive lymph nodes in patients with head and neck cancers?. Ultrasound Med. Biol. 40, 747–754 (2014).
Wendl, C. M. et al. High resolution contrast-enhanced ultrasound and 3-tesla dynamic contrast-enhanced magnetic resonance imaging for the preoperative characterization of cervical lymph nodes: First results. Clin. Hemorheol. Microcirc. 52, 153–166 (2012).
Ying, M., Bhatia, K. S. S., Lee, Y. P., Yuen, H. Y. & Ahuja, A. T. Review of ultrasonography of malignant neck nodes: Greyscale, Doppler, contrast enhancement and elastography. Cancer Imaging 13, 658–669 (2014).
Mei, M., Ye, L., Quan, J. & Huang, P. Contrast-enhanced ultrasound for the differential diagnosis between benign and metastatic superficial lymph nodes: A meta-analysis. Cancer Manag. Res. 10, 4987–4997 (2018).
Moon, I. S., Kim, D. W. & Baek, H. J. Ultrasound-based diagnosis for the cervical lymph nodes in a tuberculosis-endemic area. Laryngoscope 125, 1113–1117 (2015).
Tang, C. et al. Safety of sulfur hexafluoride microbubbles in sonography of abdominal and superficial organs: Retrospective analysis of 30,222 cases. J. Ultrasound Med. 36, 531–538 (2017).
Piscaglia, F. & Bolondi, L. The safety of Sonovue in abdominal applications: Retrospective analysis of 23188 investigations. Ultrasound Med. Biol. 32, 1369–1375 (2006).
Greis, C. Ultrasound contrast agents as markers of vascularity and microcirculation. Clin. Hemorheol. Microcirc. 43, 1–9 (2009).
Tao, S. M. et al. Contrast-induced nephropathy in CT: Incidence, risk factors and strategies for prevention. Eur. Radiol. 26, 3310–3318 (2016).
Napp, A. E. et al. Analysis and Prediction of claustrophobia during MR imaging with the claustrophobia questionnaire: An observational prospective 18-month single-center study of 6500 patients. Radiology 283, 148–157 (2017).
Spiesecke, P. et al. Cost-effectiveness analysis of multiple imaging modalities in diagnosis and follow-up of intermediate complex cystic renal lesions. BJU Int. 128, 575–585 (2021).
Jackson, D. & Turner, R. Power analysis for random-effects meta-analysis. Res. Synth. Methods 8, 290–302 (2017).
Acknowledgements
The authors thank Ms. Bettina Herwig for proofreading of the manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Study design: P.S. and M.H.L. Analysis and interpretation of data: P.S., K.N. and M.H.L. Drafting the manuscript: P.S. and M.H.L. Revising the manuscript critically for important intellectual content: P.S., K.N., K.W. and M.H.L. Final approval of the manuscript submitted: P.S., K.N., K.W. and M.H.L.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Spiesecke, P., Neumann, K., Wakonig, K. et al. Contrast-enhanced ultrasound (CEUS) in characterization of inconclusive cervical lymph nodes: a meta-analysis and systematic review. Sci Rep 12, 7804 (2022). https://doi.org/10.1038/s41598-022-11542-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-11542-9
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.