Abstract
The dual effects of co-infection of Plasmodium spp. and hookworm on malaria remain under debate. This study investigated prevalence, prevalence odds ratio (POR) of co-infection and impact of co-infection on malaria parasite density and haemoglobin levels in comparison to Plasmodium mono-infection. The protocol for this systematic review and meta-analysis is registered at PROPERO under ID: CRD42020202156. Relevant literatures were obtained from PubMed, ISI Web of Science, and Scopus on 25 December 2020. Mean difference (MD) and confidence interval (CI) of malaria parasite density and haemoglobin were compared using a random effect model. Heterogeneity was assessed using Cochrane Q and I2 statistics. Publication bias was determined by visualising funnel plot asymmetry. Of 1756 articles examined, 22,191 malaria cases across 37 studies included 6096 cases of co-infection of Plasmodium spp. and hookworm. The pooled prevalence was 20% (95% CI 15–26%, I2 99.6%, 37 studies) and was varied in terms of geographical region. Co-infection occurred by chance (OR 0.97, p 0.97, 95% CI 0.73–1.27, I2 95%, 30 studies). The mean malaria parasite density for co-infection (478 cases) was similar to Plasmodium mono-infection (920 cases) (p 0.24, MD 0.86, 95% CI − 0.58–2.29, I2 100%, 7 studies). The mean haemoglobin level for co-infection (90 cases) was similar to Plasmodium mono-infection (415 cases) (p 0.15, MD − 0.63, 95% CI − 1.49–0.23, I2 98%, 4 studies). Co-infection was common and occurred by chance but varied by geographic region. Further studies are required to investigate the mechanism of hookworm infection on malaria severity. Additionally, detection of hookworm infections among patients with malaria in endemic areas of both diseases is recommended to prevent severe malaria.
Similar content being viewed by others
Introduction
The most common soil-transmitted helminths (STHs) that cause human intestinal helminthiasis are Ascaris lumbricoides, Trichuris trichiura and hookworms (Necator americanus and Ancylostoma duodenale)1. STHs are common in areas where the capability to provide basic healthcare is limited, such as Sub-Saharan Africa (SSA)2,3,4,5. However, malaria remains the most devastating health problem in the SSA, causing an estimated 40,000 deaths each year6. In the SSA, the main cause of death of children younger than five is malaria induced by Plasmodium falciparum7. As malaria and STHs overlap in geographical distribution, co-infection of Plasmodium spp. and hookworm in the same individuals has frequently occurred. Various studies have demonstrated the impact of Plasmodium spp. and hookworm infection on the severity of malaria, including parasite density and severe anaemia8,9,10,11,12,13, demonstrating that the mean haemoglobin concentration is lower in patients with co-infection than those with either hookworm or malaria infection alone8,9. Additionally, the prevalence odds ratio (POR) of anaemia was higher in patients with co-infection than those with either hookworm or malaria infection alone10. A previous study demonstrated that a higher prevalence of only hookworm infection among patients with malaria and most of the coinfected patients had moderate (25%) or heavy (13%) hookworm infections11. Another study showed a positive interaction between hookworm infections with Plasmodium densities12 and that patients with heavy hookworm infection had a higher malaria parasite density than those with low or moderate hookworm infection12,13. A previous study suggested that the intensity of hookworm infection steadily increased with age, which indicated that hookworms might suppress host immune responses14. Nevertheless, according to one report, no association between hookworm infection and clinical malaria was found, even with heavy hookworm infection15. Various studies compared the magnitude of Plasmodium spp. and STHs’ co-infection between malaria and STHs16,17,18,19. A previous study found that although p. falciparum infection could induce a higher level of proinflammatory markers than those with S. haematobium infection, no effect of S. haematobium was found on patients with P. falciparum gametocyte carriage16. Another study reported that S. haematobium infection could induce immunity against malaria by regulation of proinflammatory cytokines, such as IL-10 and IFN-γ production18. Interestingly, a previous study found that S. haematobium infection could increase the risk of Plasmodium infection in children if Trichuris trichiura or hookworm infection was the concurrent infection20. This indicates that multiple infections of STH could affect malaria. Furthermore, a previous study suggested that helminth infections can stimulate type 2 immune responses, which are important for the induction and development of humoral immune responses for controlling malaria parasites in the blood and protecting the patients against severe malaria21.
As the occurrence of co-infection will influence the planning of integrated intervention strategies for malaria and hookworm, data on Plasmodium spp. and hookworm infection is crucial for developing integrated control efforts for disease elimination. Although various studies aimed to assess the magnitude of Plasmodium spp. and STH co-infection, there are no adequate reports that explain the correlation of Plasmodium spp. and hookworm co-infection with the level of malaria parasitaemia and haemoglobin level.
Objectives
This study aimed to determine the effect of hookworm infection on Plasmodium parasitaemia and haemoglobin levels using the meta-analysis approach.
Methods
Protocol and registration
The present systematic review and meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Checklist S1). The protocol was registered at the International Prospective Register of Systematic Reviews (PROSPERO) with registration ID: CRD42020202156.
Definitions of co-infections
Co-infections were defined as these criteria: (a) presence of both parasites in the study subjects; (b) presence of helminths in patients with malaria; or (c) presence of Plasmodium in patients with helminths infection.
Literature search
Searches for relevant articles were performed in PubMed, Web of Science and Scopus. The following combination of keywords were checked for a Medical Subject Heading term: ‘(malaria OR Plasmodium) AND (hookworm OR Ancylostoma OR Necator)’, as shown in Supplementary Table S1.
Eligibility criteria
The inclusion criteria were prevalence studies (descriptive cross-sectional) that met the definition of co-infection. Case–control studies were excluded because their reported prevalence of co-infection could not be pooled for meta-analysis. The following studies were also excluded: review articles, in vitro or in vivo studies, intervention studies and randomised control trials. Other exclusion criteria were articles written in non-English language, studies without the full-text available, studies for which the data could not be extracted, books or book chapter, studies on the same group of participants, case reports or case series, protocol and questionnaires.
Study selection and data extraction
Two independent authors (AM, MK) selected the potentially relevant studies based on eligibility criteria. Any discrepancy between the two reviewers was resolved by discussion or request of the second author (FM) for the conclusion. Data extraction was performed by the same authors. The following data were extracted for the pilot standardised datasheet: the name of the first author, publication year, study location, year that the study was conducted, study design, characteristics and number of participants, number of malaria cases, number of hookworm cases, number of co-infection, number of single infections, malaria parasite density and haemoglobin level.
Quality of included studies
The quality of the included studies was assessed using the Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses (Supplementary Table S2). NOS provided a star system for judging the included studies based on the selected study groups, comparability of the groups and ascertainment of either exposure or outcome of interest22. The comparability criteria that are not applicable to most study types were defined as “not applicable” since no data from control groups were unavailable. For this study, any included study rated more than 6 out of 7 stars indicated a high-quality study. Any included study rated 4–5 stars indicated moderate quality, whereas any study rated below 3 stars indicated poor quality.
Outcomes
The outcomes of the study were (i) magnitudes of co-infection, (ii) magnitude of parasitaemia, (iii) magnitude of malaria severity (anaemia).
Statistical analysis
The pooled prevalence of Plasmodium spp. and hookworm co-infection was estimated by the random effect model using the number of patients with co-infection and the total number of patients with malarial infection. The pooled prevalence odds ratio (POR) of hookworm infection in patients with malaria and in patients without malaria were estimated by the random effect model based on the number of patients infected with hookworm per all malaria cases, and the number of patients with hookworm per non-malaria cases. The mean parasite density and haemoglobin level among patients with co-infection and patients with Plasmodium spp. mono-infection were compared and shown as the weight mean difference with a 95% confidence interval (CI). If the included studies reported the median and interquartile range of parasite density or haemoglobin level, the mean and standard deviation were calculated by a formulation published elsewhere23. A statistical model for pooling the data was the random effect model in the case of substantial heterogeneity (I2 > 50% or Cochrane Q < 0.05) across the included studies and the fixed effect model in the case that heterogeneity across the included studies was not substantial (I2 < 50% or Cochrane Q > 0.05). Meta-regression analysis was performed to identify the source(s) of heterogeneity of the outcomes.
Publication bias
Publication bias among the included studies was assessed through visualisation of the funnel plot asymmetry and Egger’s test. The funnel plot demonstrated the effect size and standard error of the effect size. The significance of Egger's test (p < 0.05) demonstrated the asymmetrical distribution of the funnel plot and suggested that publication bias was caused by the small-study size.
Results
Search results
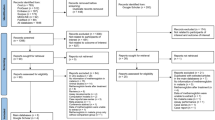
The searches retrieved 522, 769 and 465 articles from PubMed, Scopus and ISI Web of Science, respectively. Of the 1756 studies screened, 712 were duplicates and were removed. Of the 1044 articles screened for titles and abstracts, 796 articles were excluded due to irrelevant articles. Of the 248 articles examined for full texts, 211 articles were excluded for the following reasons: 55 showed no report on co-infection, 42 were review articles, 22 showed co-infection but the data could not be extracted, 18 were in vitro, 16 were intervention studies/randomised control trials, 13 were published in local languages, 12 were not full-text, 6 were not malarial case, 5 were in vivo, 4 were co-infection with other nematodes, 4 were model prediction, 4 were case–control studies, 3 were books, 3 were studies on the same group of participants, 2 were case reports/case series, 1 was protocol and 1 was a questionnaire. Finally, 37 studies met the inclusion criteria and were included in the analysis (Fig. 1).
Characteristics of the included studies
Characteristics of the included studies are shown in Table 1. Most of the included studies were cross-sectional studies (35/37, 94.6%). Most of the included studies reported Plasmodium spp. and hookworm co-infection in Africa (34/37, 91.9%)8,9,10,11,12,13,20,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50 while the remaining studies were from Asia (1 Thai-Burmese border, 1 Indonesia)51,52 or South America (Brazil)53. Most of the included studies conducted in Africa were in Nigeria (8/34, 23.5%)11,24,28,32,33,45,46,50, followed by Ethiopia (6/34, 17.6%)8,9,12,13,31,42, Tanzania (4/34, 11.8%)38,39,40,49, Uganda (4/34, 11.8%)34,36,44,47, Coˆted’Ivoire (3/34, 8.8%)10,41,48, Ghana (3/34, 8.8%)26,27,35, Kenya (2/34, 5.88%)30,37, Gabon (2/34, 5.88%)20,25 and Cameroon. One study covered three countries, including Kenya, Ethiopia and Uganda29.
Most of the included studies were conducted in school-age children (19/37, 51.4%)9,20,24,29,30,35,36,37,38,39,40,41,42,43,44,45,49,52,53, pregnant women (7/37, 18.9%)25,28,32,33,34,46,51, residents in the community (6/37, 16.2%)10,11,26,27,47,48, and acute febrile patients (4/37, 10.8%)8,12,13,31, while 1 study was conducted in voluntary donors50. Of the 37 studies included in the present analysis, 22,191 participants were confirmed to have malaria infection. Among those malarial patients, 6096 cases were patients with Plasmodium spp. and hookworm co-infection.
Prevalence of Plasmodium spp. and hookworm co-infection
The pooled prevalence of Plasmodium spp. and hookworm co-infection was estimated from 37 studies. The result demonstrated the pooled prevalence of Plasmodium spp., and hookworm co-infection was 20% (95% CI 15–26%, I2 99.6%). The meta-regression analysis was performed to identify the source (s) of heterogeneity of the prevalence. The meta-regression analysis using participant types as covariates showed that differences in participant type were not the source of heterogeneity of the pooled prevalence of Plasmodium spp. and hookworm co-infection (p > 0.05). A subgroup analysis of participants demonstrated that the pooled prevalence of co-infection was highest in residents in the community (37%, 95% CI 10–64%, I2 99.9%), acute febrile patients (21%, 95% CI 6–37%, I2 98.9%), pregnant women (20%, 95% CI 9–31%, I2 97.5%) and school-age children (14%, 95% CI 10–18%, I2 98.8%). One study conducted on voluntary donors demonstrated 45% (95% CI 40–50) co-infection50. The results of the individual study demonstrated that the prevalence of Plasmodium spp. and hookworm co-infection was highest in a study by Amoani et al. (52%)27, Hillier et al. (51%)34, Humphries et al. (48%)35 and Babamale et al. (47%)11, respectively (Fig. 2).
The meta-regression analysis using countries as covariates showed that differences in participant type were a source of heterogeneity of the pooled prevalence of Plasmodium spp. and hookworm co-infection (p < 0.05). Further subgroup analysis of countries yielded the following results: Nigeria (20%, 95% CI 9–30%, I2 97.9%), Gabon (2%, 95% CI 1–2%, I2 99.7%), Ghana (35%, 95% CI 2–69%, I2 99.1%), Kenya (20%, 95% CI 19–22%, I2 99.5%), Ethiopia (18%, 95% CI 8–28%, I2 98.1%), Uganda (27%, 95% CI 9–45% I2 99.7%), Coˆted’Ivoire (26%, 95% CI 0–72%, I2 99.9%), Tanzania (8%, 95% CI 4–12%, I2 77.2%) (Fig. 3).
Quality of the included studies
Ten studies8,9,11,13,24,28,38,40,50,53 were rated as high-quality studies, since they reported the outcomes of interest, whereas the rest of the studies were rated as moderate quality, since they reported only the data of co-infection cases but not data on haemoglobin and malaria parasite density (Supplementary Table S2).
POR of Plasmodium spp. and hookworm co-infection
The number of hookworm infections in malaria-positive patients and malaria-negative patients were analysed to determine if co-infection occurred by chance. Overall, the meta-analysis of 30 studies demonstrated that co-infection occurred by chance (p 0.94, OR 0.99, 95% CI 0.81–1.22, I2 92.5%). A subgroup analysis of participants demonstrated that studies conducted among residents in communities increased the pooled POR of co-infection (p 0.023, OR 1.93, 95% CI 1.10–3.38, I2 96.3%). Three studies by Salim et al.49, Amoani et al.27 and Babamale et al.11 demonstrated increased POR for co-infection, while 5 studies by Adedoja et al.24, Kinung’hi et al.38, Mazigo et al.39, Muller et al.41 and Degarege et al.31 demonstrated decreased POR of co-infection (Fig. 4).
Plasmodium spp. and hookworm co-infection and malaria parasite density
The pooled MD of malaria parasite density between patients with co-infection (478 cases) and Plasmodium mono-infection (920 cases) was estimated from 7 studies11,13,24,28,40,50,53. The results demonstrated no difference in the mean malaria parasite density between patients with co-infection and Plasmodium mono-infection when a random effect model was used (p 0.22, MD 885.1, 95% CI − 518.9–2289.1, I2 100%). Four studies13,24,40,50 demonstrated a higher mean of malaria parasite density in co-infection than in Plasmodium mono-infection, while two studies28,53 demonstrated a lower mean of malaria parasite density in co-infection than in Plasmodium mono-infection (Fig. 5). When excluding the study by Getaneh et al.13, which reported a high mean parasite density in patients with co-infection (outliner), no difference in the mean malaria parasite density was found between patients with co-infection and Plasmodium mono-infection (p 0.54, MD 449, 95% CI − 1000–1898.2, I2 100%) (Supplementary Fig. 1).
Plasmodium spp. and hookworm co-infection and haemoglobin level
The pooled MD of haemoglobin between patients with co-infection (90 cases) and Plasmodium mono-infection (415 cases) was estimated from four studies8,9,38,53. The results demonstrated no difference in the mean haemoglobin level between patients with co-infection and Plasmodium mono-infection when a random effect model was used (p 0.152, MD − 0.63, 95% CI − 1.49–0.23, I2 98.3%). Two studies8,9 demonstrated a lower mean haemoglobin level in co-infection than in Plasmodium mono-infection, whereas one study38 demonstrated a higher mean haemoglobin level in co-infection than in Plasmodium mono-infection (Fig. 6). The pooled MD of haemoglobin between patients with co-infection (79 cases) and without any infection (645 cases) was estimated from three studies8,9,38. The results demonstrated no difference in the mean haemoglobin level between patients with co-infection and without any infection when a random effects model was used (p 0.062, MD − 1.4, 95% CI − 2.87 to 0.07, I2 98.8%) (Fig. 7).
Publication bias
Publication bias was assessed using the funnel plot demonstrating the effect size (pooled OR) and selogES from 30 studies (Fig. 8). Egger’s test demonstrated that no small-study effect was found (p 0.128, coefficiency 6.77, standard error 4.31). Visualisation of the funnel plot and the result of Egger’s test demonstrated asymmetrical distribution of the funnel plot, and no small-study effect was found among the included studies, respectively.
Discussion
The effects of Plasmodium spp. co-infection with other diseases can cause serious clinical outcomes54,55,56,57,58. Co-infection of Plasmodium spp. and hookworm occurs in SSA; however, the mechanism and impact of the co-infection on the severity of malaria disease remain unknown. The present study demonstrated that 91.9% of the included studies reported Plasmodium spp. and hookworm co-infection in Africa, including Nigeria, Ethiopia, Tanzania, Uganda, Coˆted’Ivoire, Ghana, Kenya, Gabon and Cameroon. Some studies reported Plasmodium spp. and hookworm in the Thai-Burmese border51, Indonesia52 and Brazil53. In Africa, the highest pooled prevalence of co-infection was reported in Ghana (35%), Uganda (27%), Coˆted’Ivoire (26%), Nigeria (20%), Kenya (20%) and Ethiopia (18%), while a low pooled prevalence of co-infection was reported in Tanzania (8%), Gabon (2%) and Cameroon (1%). Based on those results, the difference in pooled prevalence was the difference in geographic area, which introduce different environmental factors, or the occurrence of malaria or hookworm per population in each area. The difference in the prevalence of co-infection suggested a difference in the geographic region, which have different environmental factors for hookworm infection. Previous studies showed that hookworm prevalence in SSA (14–43%) varied9,59,60. For example, previous studies demonstrated that hookworm is endemic in some communities of Ghana, with a high prevalence rate up to 59%35,61, and was correlated with a high prevalence of co-infection as estimated in the present study. In malaria-endemic areas, it is plausible that hookworm infection might suppress the inflammatory responses caused by Plasmodium spp., thereby reducing the risk of severe malaria62. Another contributing factor for a difference in the pooled prevalence of co-infection might be the participants investigated. The subgroup analysis of participants demonstrated that the pooled prevalence of co-infection was highest in residents in the community (37%), acute febrile patients (21%), pregnant women (20%), school-age children (14%) and voluntary donors (45%). Curiously, the higher prevalence of Plasmodium spp. and hookworm co-infection was more common among residents in the community than in school-age children. The present pooled analysis observed a high rate of co-infection in pregnant women (20%). Among pregnant women, the highest rate of co-infection was demonstrated in the study by Hillier et al. (51%)34 and Boel et al. (37%)51. A possible explanation for the high rate of co-infection in these participants may be attributed to the impairment of immunity during pregnancy63. A study demonstrated that that pregnant women are more susceptible to Plasmodium spp. and hookworm infections in their first pregnancy, which might cause nutrient deficiency in subjects, which would lead to poor pregnancy outcomes33.
The co-infection of Plasmodium spp. and hookworm might occur by chance. The pooled analysis of this study suggested that underlying infection by hookworms may not increase the chance of being infected with malaria. Nevertheless, the meta-analysis for each subgroup of participants demonstrated that hookworm infections of people within communities increased the risk of malaria infection. Previous studies showed that rural communities are associated with poverty, poor sanitation and personal hygiene, and in turn, are related to soil-transmitted-helminth infection, including hookworm infection64,65,66. Four studies conducted in school-age children demonstrated that hookworm infection decreased susceptibility to malaria infection24,38,39,41. As for the study in school-age children, another study conducted in acutely febrile patients demonstrated that hookworm infection decreased susceptibility to malaria infection31. On the contrary, previous studies conducted in school-age children and residents in communities demonstrated that hookworm infection increased susceptibility to malaria infection11,27,29,37,49. The protective or risk factors for malaria infection by hookworm infection were poorly understood. A previous study suggested that immunological interactions, micro-geographical variation, socioeconomic variables and spatial distribution of environmental conditions favour the transmission of multiple species25,34,62,67. Moreover, a previous study revealed considerable variation in the probability of Plasmodium and hookworm co-infection by geographic location, and the co-infection occurred frequently in zones where the prevalence of hookworm and P. falciparum infection were highest34. Regarding STH co-infection with Plasmodium spp., previous studies demonstrated that co-infection was more common among boys, less common with increasing age and highest among children from poor households29,48,68,69. Therefore, the risk of Plasmodium spp. and hookworm might be associated with access to sanitation and clean water, recent deworming and living in urban settings69, as in these areas, children are exposed to open defecation grounds, which is a major source of hookworm transmission infection70.
The present meta-analysis demonstrated that there was no difference in malaria parasite density among patients with co-infection when compared to patients with Plasmodium spp. mono-infection. Only two studies demonstrated that a higher hookworm intensity was positively correlated with higher malaria parasite density13,50. Previous studies demonstrated that a higher hookworm intensity was positively correlated with a higher malaria parasite density, whereas it was negatively correlated with a lower malaria parasite density when malaria was co-infected with A. lumbricoides12,13. The possible association of hookworm with protection from severe malaria was that infection of helminth modulates inflammatory factors and immunoglobulin E-induced nitric oxide (NO) production and is related to reduced parasite sequestration, which protects against severe malaria71,72. In addition, helminth may decrease cytophilic IgG1 and IgG3 antibodies, which protect the host from malaria disease. Moreover, helminth infection can increase the non-cytophilic IgG2, IgG4 and IgM antibodies, thereby accelerating the severity of malaria73.
Anaemia caused by malaria and hookworm is attributable to a combination of chronic blood loss, haemolysis, and haemopoietic suppression52. In addition, children with asymptomatic Plasmodium infection demonstrated impaired intestinal iron absorption, which may play an important role in the development of anaemia74. Previous studies demonstrated that hookworm infection is more prevalent in older children than in young children, and is associated with chronic intestinal blood loss62,75. In areas where co-infection was low, co-infection was related to anaemia and its effect on the child's health and development62. The mechanisms by which Plasmodium spp. causes anaemia involve decreased red blood cell production by bone marrow suppression and increased red blood cell destruction through rupturing, phagocytosis and hypersplenism76,77, while hookworm infection contributes to anaemia through chronic blood loss in the intestine78. The present study found no association between co-infection and malaria parasite density or haemoglobin level among the included studies. A possible explanation is that the impact of co-infection on these parameters might be due to an increase in the number of intestinal helminths species than only hookworm co-infection12,71. In addition, when compared to other intestinal helminth infections, the mean Plasmodium density in co-infected individuals with hookworm was lower than in malarial patients co-infected with A. lumbricoides alone, S. mansoni alone or T. trichiura alone31. Another explanation for the difference in contradicting reports about parasite density among co-infected patients is the variation among the included studies, such as the difference in participants, study design, methodology, level of parasite endemicity and local climate. These variations impact the differences in Plasmodium spp. and hookworm interactions and influence the heterogeneity among the includes studies. Another explanation suggested by a previous study was that hookworm infection was not associated with anaemia if low infection intensities were detected in the studied population38,79. The non-impact of Plasmodium spp. and hookworm co-infection on anaemia in the present study suggested that the anaemia was most likely due to dietary deficiency. Therefore, more studies are needed to explore the impact of co-infection on anaemia.
This study has several limitations. First, several important sources of databases, such as ScienceDirect and OVID, were not included in the search. Therefore, some relevant studies may have been missed from the search. Second, the source of heterogeneity across the included studies in the pooled prevalence analysis cannot be explored due to the limited data on the included studies. Therefore, a pooled analysis needed to be interpreted with caution. Third, the number of included studies that reported the mean or median haemoglobin and mean malarial parasite density was limited, which caused imprecision in the estimate for a pooled analysis of the mean haemoglobin and mean parasite density between patients with Plasmodium spp. and hookworm infection. Third, only studies published in English were included. For this reason, studies in Latin America are absent in this review, although this region has high malaria and hookworm endemicity.
In conclusion, co-infection of Plasmodium spp. and hookworm was common and it most likely occurred by chance. The meta-analysis demonstrated no difference in the malaria parasite density and haemoglobin level in patients with co-infection compared to Plasmodium monoinfection. However, these results were based on the limited number of studies included for meta-analysis. Therefore, for a more comprehensive review, further meta-analysis studies should include non-English literature or case–control studies. Additionally, further studies are needed to investigate the mechanism of hookworm infection on malaria severity. Finally, the detection of hookworm infections among patients with malaria in endemic areas of both diseases is recommended to prevent severe malaria.
Data availability
All data supporting the findings of this study are available within the article and its supplementary files.
References
Parija, S. C., Chidambaram, M. & Mandal, J. Epidemiology and clinical features of soil-transmitted helminths. Trop. Parasitol. 7, 81–85. https://doi.org/10.4103/tp.TP_27_17 (2017).
Muslim, A., Mohd Sofian, S., Shaari, S. A., Hoh, B. P. & Lim, Y. A. Prevalence, intensity and associated risk factors of soil transmitted helminth infections: A comparison between Negritos (indigenous) in inland jungle and those in resettlement at town peripheries. PLoS Negl. Trop. Dis. 13, e0007331. https://doi.org/10.1371/journal.pntd.0007331 (2019).
Cepon-Robins, T. J. et al. Soil-transmitted helminth infection and intestinal inflammation among the Shuar of Amazonian Ecuador. Am. J. Phys. Anthropol. 170, 65–74. https://doi.org/10.1002/ajpa.23897 (2019).
Dahal, A. S., Francis, E. O., Francis, J. E. & Wamtas, F. I. Soil-transmitted helminths and associated risk factors among elementary school pupils in Dadin Kowa, Jos. Niger. Med. J. 60, 181–185. https://doi.org/10.4103/nmj.NMJ_62_19 (2019).
Kunwar, R., Acharya, L. & Karki, S. Trends in prevalence of soil-transmitted helminth and major intestinal protozoan infections among school-aged children in Nepal. Trop. Med. Int. Health 21, 703–719. https://doi.org/10.1111/tmi.12700 (2016).
WHO. World malaria report 2019, https://www.who.int/publications/i/item/9789241565721 (2019). Accessed December 15, 2021.
WHO. Malaria, https://www.who.int/news-room/fact-sheets/detail/malaria (2020). Accessed December 15, 2021.
Demissie, F., Kebede, A., Shimels, T. & Beyene, P. Assessment of public health implication of malaria-geohelminth co-infection with an emphasis on hookworm-malaria anemia among suspected malaria patients in asendabo, southwest Ethiopia. Ethiop. Med. J. 47, 153–158 (2009).
Hailu, T., Yimer, M., Mulu, W. & Abera, B. Synergetic effects of Plasmodium, hookworm, and Schistosoma mansoni infections on hemoglobin level among febrile school age children in Jawe Worda, Northwest Ethiopia. J. Parasitol. Res. 2018, 9573413. https://doi.org/10.1155/2018/9573413 (2018).
Hurlimann, E. et al. Antagonistic effects of Plasmodium-helminth co-infections on malaria pathology in different population groups in Cote d’Ivoire. PLoS Negl. Trop. Dis. 13, 24. https://doi.org/10.1371/journal.pntd.0007086 (2019).
Babamale, O. A., Ugbomoiko, U. S. & Heukelbach, J. High prevalence of Plasmodium falciparum and soil-transmitted helminth co-infections in a periurban community in Kwara State, Nigeria. J. Infect. Public Health 11, 48–53. https://doi.org/10.1016/j.jiph.2017.03.002 (2018).
Degarege, A., Animut, A., Legesse, M. & Erko, B. Malaria severity status in patients with soil-transmitted helminth infections. Acta Trop. 112, 8–11. https://doi.org/10.1016/j.actatropica.2009.05.019 (2009).
Getaneh, F., Zeleke, A. J., Lemma, W. & Tegegne, Y. Malaria Parasitemia in febrile patients mono- and coinfected with soil-transmitted helminthiasis attending Sanja Hospital, Northwest Ethiopia. J. Parasitol. Res. 2020, 9891870. https://doi.org/10.1155/2020/9891870 (2020).
Hotez, P. J. et al. Hookworm infection. N. Engl. J. Med. 351, 799–807. https://doi.org/10.1056/NEJMra032492 (2004).
Shapiro, A. E. et al. Epidemiology of helminth infections and their relationship to clinical malaria in southwest Uganda. Trans. R. Soc. Trop. Med. Hyg. 99, 18–24. https://doi.org/10.1016/j.trstmh.2004.02.006 (2005).
Ateba-Ngoa, U. et al. Cytokine and chemokine profile of the innate and adaptive immune response of Schistosoma haematobium and Plasmodium falciparum single and co-infected school-aged children from an endemic area of Lambarene, Gabon. Malar. J. 14, 94. https://doi.org/10.1186/s12936-015-0608-4 (2015).
Ateba-Ngoa, U. et al. Associations between helminth infections, Plasmodium falciparum parasite carriage and antibody responses to sexual and asexual stage malarial antigens. Am. J. Trop. Med. Hyg. 95, 394–400. https://doi.org/10.4269/ajtmh.15-0703 (2016).
Diallo, T. O. et al. Schistosomiasis coinfection in children influences acquired immune response against Plasmodium falciparum malaria antigens. PLoS One 5, e12764. https://doi.org/10.1371/journal.pone.0012764 (2010).
Esen, M. et al. Reduced antibody responses against Plasmodium falciparum vaccine candidate antigens in the presence of Trichuris trichiura. Vaccine 30, 7621–7624. https://doi.org/10.1016/j.vaccine.2012.10.026 (2012).
Dejon-Agobe, J. C. et al. Schistosoma haematobium effects on Plasmodium falciparum infection modified by soil-transmitted helminths in school-age children living in rural areas of Gabon. PLoS Negl. Trop. Dis. 12, 17. https://doi.org/10.1371/journal.pntd.0006663 (2018).
Nacher, M. Worms and malaria: Noisy nuisances and silent benefits. Parasite Immunol. 24, 391–393. https://doi.org/10.1046/j.1365-3024.2002.00470.x (2002).
Wells, G. A. et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (2021). Accessed December 1, 2021.
Hozo, S. P., Djulbegovic, B. & Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 5, 13. https://doi.org/10.1186/1471-2288-5-13 (2005).
Adedoja, A. et al. Co-endemicity of Plasmodium falciparum and intestinal helminths infection in school age children in rural communities of Kwara State Nigeria. PLoS Negl. Trop. Dis. 9, e0003940. https://doi.org/10.1371/journal.pntd.0003940 (2015).
Adegnika, A. A. et al. Epidemiology of parasitic co-infections during pregnancy in Lambaréné, Gabon. Trop. Med. Int. Health 15, 1204–1209. https://doi.org/10.1111/j.1365-3156.2010.02598.x (2010).
Adu-Gyasi, D. et al. Epidemiology of soil transmitted helminth infections in the middle-belt of Ghana, Africa. Parasite Epidemiol. Control 3, e00071. https://doi.org/10.1016/j.parepi.2018.e00071 (2018).
Amoani, B. et al. Levels of serum eosinophil cationic protein are associated with hookworm infection and intensity in endemic communities in Ghana. PLoS One 14, e0222382. https://doi.org/10.1371/journal.pone.0222382 (2019).
Babamale, O. A., Shittu, O., Danladi, Y. K., Abdulraheem, J. Y. & Ugbomoiko, U. S. Pattern of Plasmodium-intestinal helminth co-infection among pregnant women in a high transmission zone of malaria in Nigeria. Asian Pac. J. Trop. Dis. 6, 424–428. https://doi.org/10.1016/S2222-1808(16)61060-5 (2016).
Brooker, S. J. et al. Plasmodium-helminth coinfection and its sources of heterogeneity across East Africa. J. Infect. Dis. 205, 841–852. https://doi.org/10.1093/infdis/jir844 (2012).
Bustinduy, A. L. et al. Impact of polyparasitic infections on anemia and undernutrition among Kenyan children living in a Schistosoma haematobium-endemic area. Am. J. Trop. Med. Hyg. 88, 433–440. https://doi.org/10.4269/ajtmh.12-0552 (2013).
Degarege, A., Legesse, M., Medhin, G., Animut, A. & Erko, B. Malaria and related outcomes in patients with intestinal helminths: A cross-sectional study. BMC Infect. Dis. 12, 291. https://doi.org/10.1186/1471-2334-12-291 (2012).
Egwunyenga, A. O., Ajayi, J. A., Nmorsi, O. P. & Duhlinska-Popova, D. D. Plasmodium/intestinal helminth co-infections among pregnant Nigerian women. Mem. Inst. Oswaldo Cruz 96, 1055–1059. https://doi.org/10.1590/s0074-02762001000800005 (2001).
Ekejindu, I. M. et al. Malaria and hookworm co-infection among pregnant and non-pregnant women in a semi-urban area in Anambra state, Nigeria. World J. Med. Sci. 5, 62–64 (2010).
Hillier, S. D. et al. Plasmodium falciparum and helminth coinfection in a semi urban population of pregnant women in Uganda. J. Infect. Dis. 198, 920–927. https://doi.org/10.1086/591183 (2008).
Humphries, D. et al. Hookworm infection among school age children in Kintampo north municipality, Ghana: Nutritional risk factors and response to albendazole treatment. Am. J. Trop. Med. Hyg. 89, 540–548. https://doi.org/10.4269/ajtmh.12-0605 (2013).
Kabatereine, N. B. et al. Integrated prevalence mapping of schistosomiasis, soil-transmitted helminthiasis and malaria in lakeside and island communities in Lake Victoria, Uganda. Parasit. Vectors 4, 14. https://doi.org/10.1186/1756-3305-4-232 (2011).
Kepha, S. et al. Epidemiology of coinfection with soil transmitted helminths and Plasmodium falciparum among school children in Bumula District in western Kenya. Parasit. Vectors 8, 314. https://doi.org/10.1186/s13071-015-0891-5 (2015).
Kinung’hi, S. M., Magnussen, P., Kaatano, G. M., Kishamawe, C. & Vennervald, B. J. Malaria and helminth co-infections in school and preschool children: A cross-sectional study in Magu district, north-western Tanzania. PLoS One 9, e86510. https://doi.org/10.1371/journal.pone.0086510 (2014).
Mazigo, H. D. et al. Co-infections with Plasmodium falciparum, Schistosoma mansoni and intestinal helminths among schoolchildren in endemic areas of northwestern Tanzania. Parasit. Vectors 3, 44. https://doi.org/10.1186/1756-3305-3-44 (2010).
Mboera, L. E. et al. Plasmodium falciparum and helminth coinfections among schoolchildren in relation to agro-ecosystems in Mvomero District, Tanzania. Acta Trop. 120, 95–102. https://doi.org/10.1016/j.actatropica.2011.06.007 (2011).
Müller, I. et al. Effect of schistosomiasis and soil-transmitted helminth infections on physical fitness of school children in côte d’ivoire. PLoS Negl. Trop. Dis. https://doi.org/10.1371/journal.pntd.0001239 (2011).
Mulu, A. et al. Epidemiological and clinical correlates of malaria-helminth co-infections in Southern Ethiopia. Malar. J. 12, 227. https://doi.org/10.1186/1475-2875-12-227 (2013).
Nkuo-Akenji, T. K., Chi, P. C., Cho, J. F., Ndamukong, K. K. & Sumbele, I. Malaria and helminth co-infection in children living in a malaria endemic setting of mount Cameroon and predictors of anemia. J. Parasitol. 92, 1191–1195. https://doi.org/10.1645/ge-895r.1 (2006).
Oboth, P., Gavamukulya, Y. & Barugahare, B. J. Prevalence and clinical outcomes of Plasmodium falciparum and intestinal parasitic infections among children in Kiryandongo refugee camp, mid-Western Uganda: A cross sectional study. BMC Infect. Dis. 19, 295. https://doi.org/10.1186/s12879-019-3939-x (2019).
Ojurongbe, O. et al. Asymptomatic falciparum malaria and intestinal helminths co-infection among school children in Osogbo, Nigeria. J. Res. Med. Sci. 16, 680–686 (2011).
Ojurongbe, O. et al. Prevalence and associated factors of Plasmodium falciparum and soil transmitted helminth infections among pregnant women in Osun state, Nigeria. Afr. Health Sci. 18, 542–551. https://doi.org/10.4314/ahs.v18i3.11 (2018).
Pullan, R. L., Kabatereine, N. B., Bukirwa, H., Staedke, S. G. & Brooker, S. Heterogeneities and consequences of Plasmodium species and hookworm coinfection: A population based study in Uganda. J. Infect. Dis. 203, 406–417. https://doi.org/10.1093/infdis/jiq063 (2011).
Righetti, A. A. et al. Interactions and potential implications of Plasmodium falciparum-hookworm coinfection in different age groups in south-central Côte d’Ivoire. PLoS Negl. Trop. Dis. 6, e1889. https://doi.org/10.1371/journal.pntd.0001889 (2012).
Salim, N. et al. Distribution and risk factors for Plasmodium and helminth co-infections: A cross-sectional survey among children in Bagamoyo district, coastal region of Tanzania. PLoS Negl. Trop. Dis. 9, e0003660. https://doi.org/10.1371/journal.pntd.0003660 (2015).
Shittu, O. et al. Overlapping distribution of Plasmodium falciparum and soil transmitted helminths in a malaria hyperendemic region, North-Central Nigeria. Asian Pac. J. Trop. Dis. 7, 732–737. https://doi.org/10.12980/apjtd.7.2017D7-226 (2017).
Boel, M. et al. Complex interactions between soil-transmitted helminths and malaria in pregnant women on the Thai-Burmese border. PLoS Negl. Trop. Dis. 4, e887. https://doi.org/10.1371/journal.pntd.0000887 (2010).
Burdam, F. H. et al. Asymptomatic vivax and falciparum parasitaemia with helminth co-infection: Major risk factors for anemia in early life. PLoS One 11, e0160917. https://doi.org/10.1371/journal.pone.0160917 (2016).
Melo, G. C. et al. Concurrent helminthic infection protects schoolchildren with Plasmodium vivax from anemia. PLoS One 5, e11206. https://doi.org/10.1371/journal.pone.0011206 (2010).
Kotepui, K. U., Masangkay, F. R., De Jesus Milanez, G. & Kotepui, M. Prevalence and outcomes of malaria as co-infection among patients with human African trypanosomiasis: A systematic review and meta-analysis. Sci. Rep. 11, 23777. https://doi.org/10.1038/s41598-021-03295-8 (2021).
Wilairatana, P. et al. Prevalence, probability, and outcomes of typhoidal/non-typhoidal Salmonella and malaria co-infection among febrile patients: A systematic review and meta-analysis. Sci. Rep. 11, 21889. https://doi.org/10.1038/s41598-021-00611-0 (2021).
Wilairatana, P. et al. Prevalence and characteristics of malaria co-infection among individuals with visceral leishmaniasis in Africa and Asia: A systematic review and meta-analysis. Parasit. Vectors 14, 545. https://doi.org/10.1186/s13071-021-05045-1 (2021).
Wilairatana, P., Masangkay, F. R., Kotepui, K. U., Milanez, G. J. & Kotepui, M. Prevalence and characteristics of malaria among COVID-19 individuals: A systematic review, meta-analysis, and analysis of case reports. PLoS Negl. Trop. Dis. 15, e0009766. https://doi.org/10.1371/journal.pntd.0009766 (2021).
Mahittikorn, A., Kotepui, K. U., De Jesus Milanez, G., Masangkay, F. R. & Kotepui, M. A meta-analysis on the prevalence and characteristics of severe malaria in patients with Plasmodium spp. and HIV co-infection. Sci. Rep. 11, 16655. https://doi.org/10.1038/s41598-021-95591-6 (2021).
Degarege, A., Animut, A., Legesse, M. & Erko, B. Malaria and helminth co-infections in outpatients of Alaba Kulito Health Center, southern Ethiopia: A cross sectional study. BMC Res. Notes 3, 143. https://doi.org/10.1186/1756-0500-3-143 (2010).
Erosie, L. et al. Prevalence of hookworm infection and hemoglobin status among rural elementary school children in Southern Ethiopia. Ethiop. J. Health Dev. 16, 113–115 (2002).
Humphries, D. et al. Effectiveness of albendazole for hookworm varies widely by community and correlates with nutritional factors: A cross-sectional study of school-age children in Ghana. Am. J. Trop. Med. Hyg. 96, 347–354. https://doi.org/10.4269/ajtmh.16-0682 (2017).
Mwangi, T. W., Bethony, J. M. & Brooker, S. Malaria and helminth interactions in humans: An epidemiological viewpoint. Am. J. Trop. Med. Hyg. 100, 551–570. https://doi.org/10.1179/136485906x118468 (2006).
Hartgers, F. C. et al. Responses to malarial antigens are altered in helminth-infected children. J. Infect. Dis. 199, 1528–1535. https://doi.org/10.1086/598687 (2009).
Ajayi, I. O., Dada-Adegbola, H. & Falade, C. O. Prevalence of asymptomatic malaria and intestinal helminthiasis co-infection among children living in selected rural communities in Ibadan Nigeria. Am. J. Epidemiol. Infect. Dis. 3, 15–20 (2015).
Dada-Adegbola, H. & Falade, C. Asymptomatic malaria and intestinal helminth co-infection among children in a rural community in Southwest Nigeria. Malaria World J. 4, 1–6 (2013).
Campbell, S. J. et al. Water, sanitation and hygiene related risk factors for soil-transmitted helminth and Giardia duodenalis infections in rural communities in Timor-Leste. Int. J. Parasitol. 46, 771–779. https://doi.org/10.1016/j.ijpara.2016.07.005 (2016).
Booth, M. The role of residential location in apparent helminth and malaria associations. Trends Parasitol. 22, 359–362. https://doi.org/10.1016/j.pt.2006.06.007 (2006).
Bisanzio, D. et al. Cross-sectional study of the burden of vector-borne and soil-transmitted polyparasitism in rural communities of Coast Province, Kenya. PLoS Negl. Trop. Dis. 8, e2992. https://doi.org/10.1371/journal.pntd.0002992 (2014).
Yapi, R. B. et al. Infection and co-infection with helminths and Plasmodium among school children in Côte d’Ivoire: Results from a national cross-sectional survey. PLoS Negl. Trop. Dis. https://doi.org/10.1371/journal.pntd.0002913 (2014).
Schmidlin, T. et al. Effects of hygiene and defecation behavior on helminths and intestinal protozoa infections in Taabo, Cote d’Ivoire. PLoS One 8, e65722. https://doi.org/10.1371/journal.pone.0065722 (2013).
Nacher, M. et al. Intestinal helminth infections are associated with increased incidence of Plasmodium falciparum malaria in Thailand. J. Parasitol. 88, 55–58. https://doi.org/10.1645/0022-3395(2002)088[0055:IHIAAW]2.0.CO;2 (2002).
Hobbs, M. R. et al. A new NOS2 promoter polymorphism associated with increased nitric oxide production and protection from severe malaria in Tanzanian and Kenyan children. Lancet 360, 1468–1475. https://doi.org/10.1016/S0140-6736(02)11474-7 (2002).
Druilhe, P., Tall, A. & Sokhna, C. Worms can worsen malaria: Towards a new means to roll back malaria?. Trends Parasitol. 21, 359–362. https://doi.org/10.1016/j.pt.2005.06.011 (2005).
de Mast, Q. et al. Increased serum hepcidin and alterations in blood iron parameters associated with asymptomatic P. falciparum and P. vivax malaria. Haematologica 95, 1068–1074. https://doi.org/10.3324/haematol.2009.019331 (2010).
Bethony, J. et al. Soil-transmitted helminth infections: Ascariasis, trichuriasis, and hookworm. Lancet 367, 1521–1532 (2006).
Price, R. N. et al. Factors contributing to anemia after uncomplicated falciparum malaria. Am. J. Trop. Med. Hyg. 65, 614–622. https://doi.org/10.4269/ajtmh.2001.65.614 (2001).
Abdalla, S. H. Hematopoiesis in human malaria. Blood Cells 16, 401–416 (1990) (discussion 417–409).
Tan, X. et al. Hookworm infection caused acute intestinal bleeding diagnosed by capsule: A case report and literature review. Korean J. Parasitol. 55, 417–420. https://doi.org/10.3347/kjp.2017.55.4.417 (2017).
Stoltzfus, R. J. et al. Hemoquant determination of hookworm-related blood loss and its role in iron deficiency in African children. Am. J. Trop. Med. Hyg. 55, 399–404. https://doi.org/10.4269/ajtmh.1996.55.399 (1996).
Acknowledgements
This research was supported by the New Strategic Research (P2P) Project Fiscal Year 2022, Walailak University, Thailand.
Author information
Authors and Affiliations
Contributions
M.K., A.M., G.D.M., F.R.M., and S.K. participated in the study design, data analysis, and writing of the paper. All authors have read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahittikorn, A., Masangkay, F.R., De Jesus Milanez, G. et al. Prevalence and effect of Plasmodium spp. and hookworm co-infection on malaria parasite density and haemoglobin level: a meta-analysis. Sci Rep 12, 6864 (2022). https://doi.org/10.1038/s41598-022-10569-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10569-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.