Abstract
Physical activity (PA) is critical to improving health factors such as weight, adiposity, and aerobic fitness. However, children who meet PA guideline recommendations demonstrate developmental differences in health-related outcomes. To investigate prospective associations between PA behaviour (overall PA and PA intensity) and trajectories of health-related factors among physically active children. This prospective study (2.5 years) included 391 children (baseline age: 8.1 ± 1.4 years; girls 36.3%) from ten public schools. All children performed 60-min or more of moderate-to-vigorous physical activity (MVPA) per day objectively measured. Trajectories of BMI, waist circumference, and aerobic fitness were constructed with a group-based multi-trajectory model. Three trajectory subgroups were identified: ‘high fitness/normal weight’ (48.4% of children), ‘moderate fitness /normal weight’ (42.5% of children), and ‘low fitness/overweight-obese’ (9.1% of children). Children performing higher overall PA, were less likely of being classified as members of the ‘Low Fitness/Overweight-Obese’ [Relative Risk Ratio (RRR and 95% CI) = 0.56 (0.37 to 0.85) compared to ‘high fitness/normal weight’ subgroup. Each additional 5% in light PA time was associated with approximately twofold [RRR 2.12 (1.24–3.61)] increased risk of being in the ‘low fitness/overweight-obese’ trajectory relative to the ‘high fitness/normal weight’ trajectory. Each additional 2% in vigorous-PA time was associated with a 42% and 85% reduced risk (relative to ‘high fitness/normal weight’) of being in the ‘moderate fitness/normal weight’ [RRR 0.58 (0.38–0.96)] and ‘low fitness/overweight-obesity’ [RRR 0.15 (0.06–0.37)] trajectory, respectively. Overall PA and additional time in vigorous-PA was associated with improved health-related outcomes, while light PA was negatively associated with health-related outcomes among children who adhere to PA guideline recommendations. Vigorous PA was the strongest predictor of the health trajectories. All PA guidelines for children should place greater emphasis on the importance of vigorous PA.
Similar content being viewed by others
Introduction
Insufficient physical activity (PA) is the fourth leading cause of global mortality, representing about 6% of premature deaths1. In 2013, physical inactivity was estimated to cost the global health-care system $53.8 billion2. Improving PA behaviour is therefore a cornerstone strategy to prevent, manage, and treat many chronic diseases3. Even from a young age, high levels of PA are associated with improved cardiorespiratory fitness and reduced cardiometabolic risk4,5,6. Consequently, health guidelines recommend that young people engage in at least 60 min of moderate-to-vigorous PA (MVPA) per day7. Yet, less than half of children between 6 and 19 years meet health-related PA guideline recommendations8,9,10.
In addition to the challenge posed by the relatively low number of individuals meeting health-related PA guidelines, there is large heterogeneity in response to PA in both adults and children. For example, the average increase in aerobic fitness following a 24-week aerobic exercise programme was approximately 25%, however individual responses ranged from 0 to 100% in adults11,12. Work from our group13,14 and others15,16 has demonstrated similar heterogeneous responses in young people at risk of chronic disease. The variation in PA response presents a challenge from a public health standpoint, as health-related PA guidelines focussing on time in MVPA are unlikely to be efficient for all children17.
Considering the strong and consistent associations between low fitness, elevated waist circumference and high BMI in childhood with increased health risk factors18, these measures are often used as health-related outcomes in children19. A recent study reported that one in 10 children who met PA guideline recommendations follow unfavorable health trajectories characterised by overweight/obesity and low aerobic fitness20. This suggests that PA guideline recommendations may be insufficient to mitigate health risk factors in some children. Identifying modifiable factors including PA characteristics that predict health outcomes, would benefit health-related PA prescription. Therefore, this study aimed to investigate the prospective association between PA behaviour (overall PA and PA intensity) and health-related trajectories of aerobic fitness, waist circumference, and BMI in children meeting health-related physical activity guidelines.
Methods
Study design and participants
Data from the Childhood Health, Active, and Motor Performance School Study Denmark (CHAMPS Study-DK) were used. The study sample and procedures of this quasi-experimental study have been published elsewhere21,22. Between 2008 and 2011, 10 public schools participated in the study. The current analysis was restricted to (1) participants who performed a minimum of 60 min of daily MVPA at 12 months and 22 months, which represents 43.2% of the original sample, and (2) participants who have a minimum of three time point measurements for health trajectories variables (cardiorespiratory fitness, waist circumference, and body mass index). Anthropometric variables were measured at baseline and at 6, 12, 18, 24, 30 months, while cardiorespiratory fitness was measured at baseline, 6, 12, 18, and 30 months. The rationale for differences in the above measurements’ time points was to accommodate logistic challenges related to the original investigation. Reporting of this secondary analysis of the CHAMPS Study-DK follows the STROBE statement23.
Physical activity was measured using Actigraph GT3X accelerometers (Actigraph, Pensacola Florida). Trained research staff instructed children and parents on how to wear the device. Children wore the accelerometer on the right hip using a customized elastic belt from waking in the morning until they went to bed, except when bathing or swimming.
A customized software program (Propero, version 1.0.18, University of Southern Denmark, Odense, Denmark) processed all accelerometry data. Accelerations were recorded every 2 s and subsequently collapsed into 10-s epochs. Although, some data suggest shorter epochs length to quantify PA in children, a10-second epoch was selected based on the rationale that other data using shorter epochs length showed an overestimation of sedentary behaviour in children. Therefore, to optimize the accuracy of the sedentary data without compromising the vigorous PA data, we used the 10-s epochs. Digitalized accelerometer signals were filtered with 0.25–2.5 HZ band limits. This filter process is a mathematical weighting function that contribute to alter movement of low or high frequency above or below these limits and therefore help eliminating accelerations not associated with human movement (e.g., vibration). To distinguish inactivity from periods of non-wear, we interpreted readings of zero activity lasting at least 30 consecutive minutes as ‘accelerometer non-worn’. Although, other suggest length of 45–60 min, others have been suggesting 30 min of zero activity as non-wear time in children for more accuracy24. Therefore, we decided to use the 30 min to enhance accuracy. Data included in this study were limited to children who wore the accelerometer for at least 10 h per day on 4 or more days during each week of measurement. To represent overall PA, average counts per minute (CPM) were calculated by the following formula: (total counts/minutes of wear time). Proportion of the day spent in sedentary time (0–25 counts), light (26–573 counts), moderate (574–1002 counts), and vigorous (≥ 1003 counts) PA intensities were identified using pre-established and validated cut-points according to Evenson et al.25 As our data were collected in 2-s epochs, they were re-integrated in 10-s epochs and Evenson’s cut-points were scaled to ensure they mirrored the cut-points proposed by Evenson et al. All PA outcomes were averaged across the two measurement periods.
Cardiorespiratory fitness was measured with the Andersen test. This is an intermittent maximal indirect indoor running test developed for children and youth26. Briefly, children ran as fast as possible down a 20 m lane, touched behind the line with one hand, and turned and ran back in the opposite direction. After 15 s, children stopped immediately when hearing a whistle. Following 15 s of rest, the process repeated, with children attempting to cover the greatest distance possible. The test outcome was total distance run by each child in 10 min, and this was monitored by trained research staff. This test has good test–retest reliability and concurrent validity when compared with direct VO2max testing in children27.
Anthropometric measurements including height and weight were measured with children barefoot, wearing light clothes, without hats or helmets, and with empty pockets. Height was measured to the nearest 0.5 cm with a portable stadiometer (SECA 214, Seca Corporation, Hanover, MD, USA), and weight to the nearest 0.1 kg using a calibrated Tanita BWB-800S digital scale (Tanita Corporation, Tokyo, Japan). Body mass index (BMI) was calculated as: weight (kg)/height (m)2 and categorized as normal weight, overweight, or obese according to International Obesity Task Force criteria28.
Waist circumference was measured to the nearest 0.5 cm with a tape measure placed at the level of the umbilicus following normal expiration. The measure was taken twice, and if differences greater than 1 cm were observed, a third measure was obtained. The mean of the two closest measurements was reported. Waist circumference outcomes were used to classify children as normal weight, overweight, or obese using sex and age-adjusted criteria29.
Statistical analyses
The multi-trajectory modeling has been reported in detail elsewhere20. Briefly, we constructed a group-based multi-trajectory model that identified clusters of children who followed similar patterns of concurrent change (i.e., trajectories) in BMI, waist circumference, and aerobic fitness30. For the trajectory model, we excluded participants with less than three outcome measures. Otherwise, missing data were estimated with maximum likelihood estimation which results in asymptotically unbiased parameter estimates when data are missing at random31. We identified 3 health-related trajectory subgroups: (1) high fitness/normal weight’, (2) ‘moderate fitness /normal weight’, and (3) ‘low fitness/overweight-obese’.
Descriptive data were presented as mean ± SD and N (%) for categorical variables unless otherwise stated. We used multinomial logistic regression models with robust standard errors to investigate the associations between the PA variables (CPM, proportion of day spent in sedentary time, and light, moderate, and vigorous activity) and the three health-related trajectory subgroups. Results were reported as relative risk ratios (RRR) and 95% confidence intervals (CI). RRR were reported for every 25% time spent in sedentary behaviour; every 5% time spent in light and moderate PA, and every 2% time spent in vigorous PA and MVPA. All percentages (5%, 25%, and 2%) represent proportion of the day. CPM was reported per standard deviation unit (SD: 137.7). These numbers were arbitrary selected to enhance the interpretability of the analyses. Data management and statistical analyses were performed using STATA Version 15.0 software (StataCorp, College Station, TX, USA). A p ≤ 0.05 was considered significant for all inferential analyses.
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki, approved by the Regional Scientific Ethical Committee of Southern Denmark (ID S-20080047), and registered on January 3, 2008 with the Danish Data Protection Agency (J.nr. 2008-41-2240). All children gave verbal assent and all parents provided written informed consent to participate before study enrollment.
Results
In total, 522 children achieved 60 min of daily MVPA at each of the measurement periods. From this population, 131 children had less than 3 measures of BMI, waist circumference, or aerobic fitness. Therefore, data from 391 physically active children were included in the study analyses (Fig. 1). In total, 48.4% of children were classified as members of the ‘high fitness/normal weight’, 42.5% with ‘moderate fitness/normal weight’, and 9.1% with ‘low fitness/overweight-obese’ trajectory subgroups (Fig. 2).
Tables 1 and 2 describe the baseline characteristics of the sample and the PA and sedentary behaviour of the cohort as well as each trajectory subgroup. Briefly, physically active children were 8.1 ± 1.4 years old and 36.3% were girls. Mean accelerometer wear time was 797.5 ± 30.9 min/day. On average, children spent about 468.5 ± 45.3 min per day in sedentary behaviour, 50.4 ± 7.7 min in moderate PA, and 31.6 ± 8.3 min in vigorous PA.
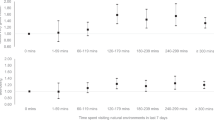
Figure 3 reports the associations between sedentary behaviour and PA and the health-related trajectory subgroups. There were no associations between total sedentary behaviour or time in moderate intensity physical activity and trajectory group membership (Fig. 3A,B). Children who spent more time in light intensity PA were more likely to be classified as members of the ‘moderate fitness/ normal weight’ [RRR (95% CI) = 1.41 (1.06 to 1.86) per 5% increase] and ‘low fitness/ overweight-obese’ [RRR (95% CI) = 2.12 (1.24 to 3.61) per 5% increase] subgroups than children following a ‘high fitness/normal weight’ trajectory. Conversely, children who spent more time in MVPA were less likely to be classified as members of the ‘moderate fitness/normal weight’ [RRR (95% CI) = 0.74 (0.57 to 0.96) per 5% increase] and ‘low fitness/overweight-obese’ [RRR (95% CI) 0.40 (0.24–0.64) per 5% increase] subgroups than children following a ‘high fitness/normal weight’ subgroup. Children who spent more time in vigorous PA were less likely to be classified as members of the ‘moderate fitness/normal weight’ subgroup [RRR (95% CI) = 0.58 (0.38 to 0.96) per 2% increase] and ‘low fitness/overweight-obese’ [RRR (95% CI) 0.15 (0.06–0.37) per 2% increase] subgroups compared to ‘high fitness/normal weight’. Children with more CPM were less likely to be classified as members of the ‘Low Fitness/ Overweight-Obese’ [RRR (95% CI) = 0.56 (0.37 to 0.85) per 1SD increase in CPM compared to ‘high fitness/normal weight’.
Relative risk ratios of being in the moderate fitness/ normal weight or in the low fitness/overweight-obese trajectory according to physical activity intensities. Data are presented as relative risk ratios (RRR) and (95% confidence intervals). RRR for sedentary behaviour is reported for every 25% time spent; light and moderate PA is reported for every 5% time spent, while vigorous PA and MVPA are reported for every 2% time spent at that intensity, CPM is reported per standard deviation (SD:137.7496); Reference group is children assigned to the ‘high fitness/normal weight’ trajectory.
Discussion
The aim of this study was to investigate the prospective associations between PA behaviour (overall PA and PA intensity) and trajectories of health-related factors in children meeting PA guideline recommendations. Among PA guideline concordant children, PA behaviours were associated with membership in the health-related trajectory subgroups. Children who performed more PA overall were less likely to be classified as members of the unfavorable health trajectory. This result aligns closely with the world health organization guideline on PA and sedentary behaviour32 suggesting that every step counts for overall health. In addition, our results suggest that children who spent more time in MVPA and vigorous PA were less likely to be classified as members of the unfavorable health trajectory. Conversely, children who spent more time engaged in light intensity PA were more likely to follow an unfavourable health trajectory. These results suggest that (1) a small increase in overall PA or (2) even a small increase in PA intensity in children who adhere to the national recommendation of PA may have important health benefits. For example, 8 min of MVPA and 6 min of vigorous PA appears beneficial to reduce the risk of following an unfavourable health trajectory.
The main finding of this study is the strong association between the reduced risk of being in the ‘low fitness/overweight-obese’ trajectory and time spent in MVPA, particularly vigorous PA. In a cross-sectional study of 29,734 children, Tarp et al., investigated PA patterns in children and found that intensity rather than duration was the strongest predictor of a reduction in BMI33. These results highlighted that in children PA should be promoted especially at higher intensities. Similarly, results from a cross-sectional study performed by Hay et al. showed a 44% reduction in the likelihood of being overweight for every 7 min of vigorous PA34. Finally, a meta-analysis of cross-sectional studies investigated the reallocation of sedentary time to MVPA and observed a reduction in the percent body fat, although a reduction in BMI and waist circumference was not observed35. The results of our study are important as they provide longitudinal evidence that a small addition of vigorous PA of about 6 min, appears to reduce the risk of following an unhealthy trajectory in children meeting the national recommendation of PA. The current study adds to the whole body of knowledge on exercise response by providing prospective evidence that vigorous PA predicts developmental health trajectories in children meeting PA guideline recommendations.
PA mainly reduces chronic disease risk by reducing adiposity and increasing cardiorespiratory fitness19. Based on our results, vigorous PA is the strongest predictor of such improvements. Vigorous PA confers beneficial physiological adaptations that increase cardiorespiratory fitness and reduce adiposity and waist circumference. For example, vigorous PA may increase cardiorespiratory fitness through enhanced oxygen extraction capacity in the skeletal muscles36. Furthermore, vigorous PA is associated with a greater release of catecholamines compared to lighter PA, which activate adipose tissue lipolysis via hormone sensitive lipase, especially in the abdominal area37. Therefore, these mechanisms may explain some of the improvements in adiposity and waist circumference associated with vigorous PA.
In the current study, we observed that PA guideline concordant children demonstrate measurable inter-individual variation in their development of BMI, waist circumference, and aerobic fitness. This aligns with results from other studies performed in children, suggesting that although many children benefit from PA interventions, some children do not experience health-related benefits13,14,15,16. For example, A prospective 6 month study involving 79 sedentary children at risk of Type 2 diabetes, reported large heterogeneity in cardiorespiratory fitness and adiposity following a PA program13. Despite implementing well-controlled procedures, the inter-individual variation in several adiposity measures ranged from a decrease of 69% to an increase of 55%13. Results from the current study support the concept of heterogeneity in exercise response in children, and build on our previous findings by virtue of including a large cohort of children meeting the national PA recommendations.
Although this study revealed important findings, several limitations need to be discussed. First, the relatively small number of children in the ‘low fitness/overweight-obese’ trajectory did not allow us to adjust for multiple covariates simultaneously including socioeconomic status and education. Second, accelerometers worn at the hip level do not capture movements such as cycling or swimming which may have impacted our results. Third, habitual PA was not quantified throughout the study, which would have informed us on participant’s PA level between the two time-point measurement, which could have impacted our results. Fourth, no information in terms of diet quality and energy intake were available and we did not account for weekend time PA which might contribute the explanation of our results. Finally, since only about a third of our sample was composed of girls, our data are more representative of active boys. Despite these limitations, our study is strengthened by the prospective design, the relatively large sample size and objective measure of PA. In addition, using a novel multi-trajectory approach, our study used multiple concurrent health outcomes to explore PA predictors in active children.
Conclusion
In conclusion, our results suggest that amongst physically active children, those children belonging to the low aerobic fitness and overweight-obese trajectory had lower overall PA, spend less time in MVPA and more time in light-intensity PA. In particular, the amount of vigorous PA was associated with better health trajectories in these children and was the strongest predictor of maintaining a better health trajectory. Globally, PA guidelines should consider the importance of vigorous PA as part of their daily PA in children.
Data availability
Data are available from the CHAMPS Study Steering Committee upon reasonable request. Legal and ethical restrictions apply. Interested parties may contact Dr. Niels Christian Møller (nmoller@health.sdu.dk), and the following information will be required at the time of application: a description of how the data will be used, securely managed, and permanently deleted.
References
WHO. Global Recommendation on Physical Activity for Health (WHO, 2010).
Ding, D. et al. The economic burden of physical inactivity: A global analysis of major non-communicable diseases. Lancet 388, 1311–1324. https://doi.org/10.1016/s0140-6736(16)30383-x (2016).
Pedersen, B. K. & Saltin, B. Exercise as medicine: Evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand. J. Med. Sci. Sports 25(Suppl 3), 1–72. https://doi.org/10.1111/sms.12581 (2015).
Ekelund, U. et al. Independent associations of physical activity and cardiorespiratory fitness with metabolic risk factors in children: The European youth heart study. Diabetologia 50, 1832–1840. https://doi.org/10.1007/s00125-007-0762-5 (2007).
Cristi-Montero, C. et al. Cardiometabolic risk through an integrative classification combining physical activity and sedentary behavior in European adolescents: HELENA study. J. Sport Health Sci. 8, 55–62. https://doi.org/10.1016/j.jshs.2018.03.004 (2019).
Skrede, T. et al. Does cardiorespiratory fitness moderate the prospective association between physical activity and cardiometabolic risk factors in children?. Int. J. Obes. (Lond.) 42, 1029–1038. https://doi.org/10.1038/s41366-018-0108-z (2018).
Tremblay, M. S., Carson, V. & Chaput, J. P. Introduction to the Canadian 24-hour movement guidelines for children and youth: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 41, iii–iv. https://doi.org/10.1139/apnm-2016-0203 (2016).
Colley, R. C. et al. Physical activity of Canadian children and youth: Accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 22, 15–23 (2011).
Riddoch, C. J. et al. Physical activity levels and patterns of 9- and 15-yr-old European children. Med. Sci. Sports Exerc. 36, 86–92. https://doi.org/10.1249/01.Mss.0000106174.43932.92 (2004).
Roman-Vinas, B. et al. Proportion of children meeting recommendations for 24-hour movement guidelines and associations with adiposity in a 12-country study. Int. J. Behav. Nutr. Phys. Act. 13, 123. https://doi.org/10.1186/s12966-016-0449-8 (2016).
Bouchard, C. Individual differences in the response to regular exercise. Int. J. Obes. Relat. Metab. Disord. 19(Suppl 4), S5-8 (1995).
Bouchard, C. Physical activity and health: Introduction to the dose-response symposium. Med. Sci. Sports Exerc. 33, S347-350 (2001).
Senechal, M. et al. Fitness is a determinant of the metabolic response to endurance training in adolescents at risk of type 2 diabetes mellitus. Obesity (Silver Spring) 23, 823–832. https://doi.org/10.1002/oby.21032 (2015).
Blizzard LeBlanc, D. R. et al. Exercise-induced irisin release as a determinant of the metabolic response to exercise training in obese youth: The EXIT trial. Physiol. Rep. 5, e12539. https://doi.org/10.14814/phy2.13539 (2017).
Alvarez, C., Ramirez-Campillo, R., Ramirez-Velez, R. & Izquierdo, M. Prevalence of non-responders for glucose control markers after 10 weeks of high-intensity interval training in adult women with higher and lower insulin resistance. Front. Physiol. 8, 479. https://doi.org/10.3389/fphys.2017.00479 (2017).
Alvarez, C. et al. Metabolic effects of resistance or high-intensity interval training among glycemic control-nonresponsive children with insulin resistance. Int. J. Obes. (Lond.) 42, 79–87. https://doi.org/10.1038/ijo.2017.177 (2018).
Parrish, A. M. et al. Comparing and assessing physical activity guidelines for children and adolescents: A systematic literature review and analysis. Int. J. Behav. Nutr. Phys. Act. 17, 16. https://doi.org/10.1186/s12966-020-0914-2 (2020).
Klakk, H. et al. Prospective association of adiposity and cardiorespiratory fitness with cardiovascular risk factors in healthy children. Scand. J. Med. Sci. Sports 24, e275-282. https://doi.org/10.1111/sms.12163 (2014).
Andersen, L. B., Riddoch, C., Kriemler, S. & Hills, A. P. Physical activity and cardiovascular risk factors in children. Br. J. Sports Med. 45, 871–876. https://doi.org/10.1136/bjsports-2011-090333 (2011).
Hebert, J. J. et al. Developmental trajectories of body mass index, waist circumference, and aerobic fitness may identify distinct responses to physical activity in children (CHAMPS Study-DK). Sports Med. 50, 2253–2261 (2020).
Wedderkopp, N. et al. Study protocol. The childhood health, activity, and motor performance school study Denmark (The CHAMPS-study DK). BMC Pediatr. 12, 128. https://doi.org/10.1186/1471-2431-12-128 (2012).
Moller, N. C. et al. Do extra compulsory physical education lessons mean more physically active children–findings from the childhood health, activity, and motor performance school study Denmark (The CHAMPS-study DK). Int. J. Behav. Nutr. Phys. Act. 11, 121. https://doi.org/10.1186/s12966-014-0121-0 (2014).
von Elm, E. et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 61, 344–349. https://doi.org/10.1016/j.jclinepi.2007.11.008 (2008).
Vanhelst, J. et al. Comparison and validation of accelerometer wear time and non-wear time algorithms for assessing physical activity levels in children and adolescents. BMC Med. Res. Methodol. 19, 72. https://doi.org/10.1186/s12874-019-0712-1 (2019).
Evenson, K. R., Catellier, D. J., Gill, K., Ondrak, K. S. & McMurray, R. G. Calibration of two objective measures of physical activity for children. J. Sports Sci. 26, 1557–1565. https://doi.org/10.1080/02640410802334196 (2008).
Andersen, L. B., Andersen, T. E., Andersen, E. & Anderssen, S. A. An intermittent running test to estimate maximal oxygen uptake: The Andersen test. J. Sports Med. Phys. Fitness 48, 434–437 (2008).
Ahler, T., Bendiksen, M., Krustrup, P. & Wedderkopp, N. Aerobic fitness testing in 6- to 9-year-old children: Reliability and validity of a modified Yo-Yo IR1 test and the Andersen test. Eur. J. Appl. Physiol. 112, 871–876. https://doi.org/10.1007/s00421-011-2039-4 (2012).
Cole, T. J., Bellizzi, M. C., Flegal, K. M. & Dietz, W. H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 320, 1240–1243 (2000).
Fredriks, A. M., van Buuren, S., Fekkes, M., Verloove-Vanhorick, S. P. & Wit, J. M. Are age references for waist circumference, hip circumference and waist-hip ratio in Dutch children useful in clinical practice?. Eur. J. Pediatr. 164, 216–222. https://doi.org/10.1007/s00431-004-1586-7 (2005).
Nagin, D. S., Jones, B. L., Passos, V. L. & Tremblay, R. E. Group-based multi-trajectory modeling. Stat. Methods Med. Res. 27, 2015–2023. https://doi.org/10.1177/0962280216673085 (2018).
Nagin, D. S. & Odgers, C. L. Group-based trajectory modeling in clinical research. Annu. Rev. Clin. Psychol. 6, 109–138. https://doi.org/10.1146/annurev.clinpsy.121208.131413 (2010).
WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour. https://apps.who.int/iris/bitstream/handle/10665/336656/9789240015128-eng.pdf?sequence=1&isAllowed=y (2020).
Tarp, J. et al. Physical activity intensity, bout-duration, and cardiometabolic risk markers in children and adolescents. Int. J. Obes. (Lond.) 42, 1639–1650. https://doi.org/10.1038/s41366-018-0152-8 (2018).
Hay, J. et al. Physical activity intensity and cardiometabolic risk in youth. Arch. Pediatr. Adolesc. Med. 166, 1022–1029. https://doi.org/10.1001/archpediatrics.2012.1028 (2012).
Garcia-Hermoso, A., Saavedra, J. M., Ramirez-Velez, R., Ekelund, U. & Del Pozo-Cruz, B. Reallocating sedentary time to moderate-to-vigorous physical activity but not to light-intensity physical activity is effective to reduce adiposity among youths: A systematic review and meta-analysis. Obes. Rev. 18, 1088–1095. https://doi.org/10.1111/obr.12552 (2017).
Gibala, M. J. & Little, J. P. Physiological basis of brief vigorous exercise to improve health. J. Physiol. 598, 61–69. https://doi.org/10.1113/jp276849 (2020).
Poirier, P. & Despres, J. P. Exercise in weight management of obesity. Cardiol. Clin. 19, 459–470. https://doi.org/10.1016/s0733-8651(05)70229-0 (2001).
Acknowledgements
The authors gratefully acknowledge the valuable work of numerous students who assisted with data collection in the CHAMPS study DK. We also thank the participating children, their parents, and teachers in the schools involved in the project. We are grateful for the cooperation with The Svendborg Project, Sport Study Sydfyn, and the Municipality of Svendborg. Finally, we wish to acknowledge members of the CHAMPS-study DK not listed as co-authors in this paper: E. Jespersen, M. Heidemann, C.T. Rexen, and C. Franz.
Author information
Authors and Affiliations
Contributions
J.J.H., M.S., T.F., and N.W. conceived the research questions and designed the analysis. N.C.M., H.K., and N.W. acquired data. J.J.H. conducted the data analysis and drafted the original manuscript. All authors interpreted the data, provided critical revisions of the manuscript, and approved the final version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sénéchal, M., Hebert, J.J., Fairchild, T.J. et al. Vigorous physical activity is important in maintaining a favourable health trajectory in active children: the CHAMPS Study-DK. Sci Rep 11, 19211 (2021). https://doi.org/10.1038/s41598-021-98731-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-98731-0
This article is cited by
-
Physical activity and its impact on cardiovascular health in pediatric kidney transplant recipients
Pediatric Nephrology (2024)
-
The association between childhood motor performance and developmental trajectories of sport participation over 5 years in Danish students aged 6–16-year-old
Scientific Reports (2023)
-
Reference values for wrist-worn accelerometer physical activity metrics in England children and adolescents
International Journal of Behavioral Nutrition and Physical Activity (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.