Abstract
The in vitro interactions of isavuconazole with colistin were evaluated against 15 clinical Candida auris isolates by a microdilution checkerboard technique based on the EUCAST reference method for antifungal susceptibility testing and by agar diffusion using isavuconazole gradient concentration strips with or without colistin incorporated RPMI agar. Interpretation of the checkerboard results was done by the fractional inhibitory concentration index and by response surface analysis based on the Bliss model. By checkerboard, combination was synergistic for 93% of the isolates when interpretation of the data was done by fractional inhibitory concentration index, and for 80% of the isolates by response surface analysis interpretation. By agar diffusion test, although all MICs in combination decreased compared to isavuconazole alone, only 13% of the isolates met the definition of synergy. Essential agreement of EUCAST and gradient concentration strip MICs at +/− 2 log2 dilutions was 93.3%. Antagonistic interactions were never observed for any technique or interpretation model used.
Similar content being viewed by others
Introduction
Candida auris is an emerging, multidrug-resistant, fungal pathogen, responsible for invasive hospital-acquired infections1,2,3. The yeast was first isolated from an ear sample in Japan and described in 20094. Initially supposed to be a rare pathogen, the incidence of this Candida species has increased and cases have been reported in several countries across five continents5. The emergence of C. auris is alarming, as the species has the potential to exhibit or to develop multidrug-resistance to antifungals6,7. C. auris is associated with a cumulative mortality rate of 33% in all reported cases until 2018 despite antifungal treatment8. Antifungal combination may be an interesting therapeutic approach to improve the prognosis of the patients. Indeed, combination of two molecules may reduce toxicity, decrease antifungal dosages, improve the pharmacokinetics of one or both drugs, and more importantly achieve synergistic interactions9. Nevertheless, only few studies have evaluated in vitro combinations against C. auris10,11,12,13. First of all, the combination of micafungin with voriconazole was synergistic against all tested isolates12. Another more recent study evaluated the combination of flucytosine with amphotericin B, voriconazole or micafungin against 15 isolates and showed no antagonism10. Antifungal combinations including flucytosine were also evaluated against C. auris isolates from a New York outbreak13. Combinations of antifungals with non-antifungal drugs such as colistin have also been tested11. Colistin belongs to the family of polymyxins, from the group of polymyxins E. It targets the external membrane of the gram negative bacteria, more precisely lipid A, a lipopolysaccharide14. This leads to an alteration of the external membrane, resulting in an increased membrane permeability, finally leading to cell death15. In Candida albicans and Rhizopus arrhizus, it has been shown that colistin damages the cytoplasmic membrane16,17. This mechanism of colistin could favour the penetration of antifungals, which would make the antibiotic an interesting partner to use in combination therapy for the treatment of fungal infections. Colistin has been tested in vitro against yeasts11,17,18,19,20,21, and filamentous fungi16,17,19,20, and in vivo in animal models of invasive candidiasis18,21, and mucormycosis16 with various activities and efficacies. Isavuconazole is a new broad spectrum azole recommended for treatment of invasive aspergillosis and mucormycosis22, but has also shown in vitro activity against several yeast species including C. auris23,24. Therefore, combination of colistin with isavuconazole may be of interest against C. auris. The objective of the present study was to evaluate the in vitro interaction of isavuconazole with colistin against a collection of clinical C. auris isolates.
Results
The interactions between isavuconazole and colistin evaluated by checkerboard (interpreted by FICI or by response surface analysis) and by agar diffusion assay against the 15 C. auris isolates are presented in Table 1. Percentages of the interactions of the different techniques and interpretation models are presented in Table 2.
By microbroth dilution method, the 15 isolates exhibited MICs for isavuconazole alone ranging from 0.004 to 1 µg/mL with a MIC50, MIC90, and geometric mean MIC of 0.25, 0.5, and 0.21 µg/mL, respectively (Table 1). Between the experiments, the isavuconazole MICs were within +/− 1 log2 dilutions in 100% of the cases (data not shown). Colistin alone did not exhibit in vitro activity alone at the concentrations used for the experiment. MICs for all isolates were > 64 µg/mL. By checkerboard and interpretation by fractional inhibitory concentration index (FICI), the interaction of isavuconazole with colistin was synergistic for 93% of the isolates with FICIs ranging from 0.3125 to 0.5 with a mean FICI of 0.4.
Analysis of the checkerboard data by the response surface approach led to similar results. For the combination of isavuconazole with colistin the SUM-SYN-ANT metric ranged from − 8.94 to 58.02 (Table 1), with a mean of 32.37. Overall synergy was obtained for 80% of the isolates (Table 2).
By agar diffusion assay MICs of isavuconazole were slightly higher as by checkerboard (p = 0.013) and ranged from 0.006 to 3 µg/mL with a MIC50, MIC90, and a geometric mean MIC of 0.5, 1, and 0.47 µg/mL, respectively. Nevertheless, there was a good correlation between EUCAST and gradient concentration strip MICs with an essential agreement, at +/− 2 log2 dilutions, of 93.3%. Growth on RPMI agar was not inhibited by incorporation of 64 µg/mL of colistin for all isolates. Although all MICs in combination were lower than MICs of isavuconazole alone, only two isolates met the definition of synergy of a decrease ≥ 2 log2 dilutions compared to isavuconazole alone. Nevertheless, a decrease of 1 log2 was seen for 6 additional isolates and a decrease of 1.5 log2 for 2 further isolates.
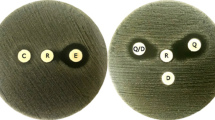
Antagonistic interactions were never observed whatever technique or method of analysis used. Figure 1 shows the synergistic interaction of isavuconazole in combination with colistin for isolate CBS 12771 by the different in vitro techniques and interpretation models used in this study. Figure 2 shows the interaction of isavuconazole in combination with colistin against all 15 isolates by agar diffusion assay.
Comparison of the in vitro techniques and interpretation models for the synergistic interaction between isavuconazole (ISAVU) and colistin (COL) against C. auris isolate CBS 12771. (A) Percentage of growth compared to the growth control on the 96 wells microplate; (B) Agar diffusion assay: left side, isavuconazole alone; right side isavuconazole + colistin at 64 µg/mL incorporated in the agar; (C) Response surface analysis, based on the Bliss model, showing the mapping of the synergy levels on the experimental combination dose–response surface; (D) Synergy distribution, in matrix format, derived from the combination dose–response and the reference dose–response; (E) Response curves of the drugs alone. Panels C, D, and E were generated with the software Combenefit, version 2.02138.
Discussion
Recently, the appearance of coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)25, led to a global health crisis, since there were only symptomatic treatment options available26. Drugs designated for other diseases were repurposed for COVID-19 to overcome this therapeutic issue. Interventions against SARS-CoV-2 included prophylaxis to augment epithelial defence (e.g. angiotensin II receptor antagonists), reduction of viral load (e.g. remdesivir), tempering inflammatory signalling and injury (e.g. dexamethasone), and inhibitors targeting the molecular mediators of the maladaptive COVID-19 immune response (e.g. IL-6)27. There are three major advantages of drug repurposing: first the use of de‐risked compounds, second the potentially lower overall development costs, and third shorter development timelines28. Already prior to the COVID-19 pandemic repurposing of drugs had become trendy. Repurposed drugs have shown activity against bacteria29, yeasts29,30, and filamentous fungi31,32,33,34. Colistin is a drug of last resort with activity against multidrug-resistant gram-negative bacteria such as Pseudomonas aeruginosa, Klebsiella pneumoniae, or Acinetobacter baumanii35; but colistin has also shown to damage the cell membrane of C. albicans17, which could make it an interesting partner in combination therapy against multidrug-resistant C. auris infections. Indeed, resistance to all four major classes of antifungals (polyenes, azoles, pyrimidines, and echinocandins) has been reported in clinical isolates of C. auris. Therefore, combination therapy may be an interesting option compared to monotherapies for management of antifungal-resistant C. auris infections.
One of the problems of assessing antifungal combinations by the FICI is the choice of the endpoint. Fifty percent of inhibition is recommended for yeasts and azoles for the determination of the MICs of antifungals alone36. Nevertheless, for combination studies, there is no consensus about which endpoint should be used, particularly when one of the partner drugs is not an antifungal, which is the case in this study. In combination studies, the major point is to look for relative growth when antifungals are tested alone and in combination. In some interaction models (such as Prichard model based on Bliss independence theory37) there is no endpoint at all, and the interaction is calculated only based on the percentage of growth at different concentrations. We additionally used an alternative model not dependent of an endpoint (surface-response based on the Bliss model38) to overcome the limitations of the FICI model. This model has already been used successfully against medically important Candida species39, including C. auris10,11.
In vitro synergy between colistin and antifungals has been reported for yeasts11,17,18,20,21, and filamentous fungi17,20. However, absence of synergy11,17,19,21, and even antagonism have also been reported19. In our study, we found in vitro synergy in the combination of isavuconazole with colistin by checkerboard, and in the interpretation of the data by two radically different approaches (FICI or response surface analysis). By agar diffusion assay no interaction of the combination was seen. This may be evidence that the synergy of the combination is weak. Nevertheless, the MICs in combination were reduced for all isolates compared to isavuconazole alone. Another evidence for a weak synergy of the combination is the relatively high mean FICI of 0.4. Additionally, the mean SUM-SYN-ANT of 32.37 was relatively low, compared to another study where a strong synergy for the combination of colistin with caspofungin with a mean SUM-SYN-ANT of 122.3 was found11. The only other study which evaluated the interaction of colistin with antifungals against C. auris demonstrated that colistin in combination with caspofungin was synergistic, and that combination with micafungin was not antagonistic11. In the same study, colistin showed no in vitro activity when used alone. Our results are in concordance to this study. Isavuconazole alone exhibited in vitro activity against C. auris by broth microdilution and by gradient concentration strips with MICs in the same range and an essential agreement between the two techniques as previously published24. Combinations of colistin with other antifungals against Candida species were mainly tested against C. albicans. Colistin combined with caspofungin was synergistic against C. albicans, in vitro and in vivo in a Galleria mellonella model of invasive candidiasis18. Combinations of colistin with echinocandins have also been tested against C. albicans and other Candida species in another study. Combinations exhibited synergy, but unfortunately, only few isolates were tested21. In an another study, the combination of colistin with the polyene amphotericin B or the azole itraconazole also showed synergistic interactions against one C. albicans isolate17.
In our study, broth microdilution MICs of colistin in combination ranged from 1 to 32 µg/mL. In patients with cystic fibrosis receiving prolonged colistin therapy, peak serum levels of 13 to 32 µg/mL were measured40, which would be sufficient to be effective against our isolates; but it has to be noted that the use of colistin in critically ill patients is limited due to its nephrotoxicity41. In critically ill patients peak levels of 0.5 to 9.4 µg/mL were reported42. Nevertheless, in vivo synergistic interactions could be present at lower concentrations than those tested in vitro. Indeed, one study evaluated the in vitro interaction of tacrolimus with amphotericin B or fluconazole against Cryptococcus neoformans by checkerboard, and synergy was obtained for both combinations. Despite lower achievable tacrolimus serum concentrations than the concentrations used in the microplates, the outcome of solid organ transplant recipients with cryptococcosis receiving tacrolimus long-term therapy and amphotericin B or fluconazole, was significantly better than the outcome of patients receiving only amphotericin B or fluconazole43.
In summary, colistin enhances the in vitro activity of isavuconazole against clinical C. auris isolates. These results warrant further in vivo experiments.
Materials and methods
Isolates
A panel of 15 clinical C. auris isolates from the collection of Westerdijk Fungal Biodiversity Institute (Utrecht, The Netherlands) was used for the experiments. All isolates have been identified by molecular biology previously4,44,45,46. The isolates were subcultured from frozen stocks on Sabouraud dextrose agar slants containing chloramphenicol and gentamycin (Bio-Rad Laboratories, Feldkirchen, Germany) for 24 h at 35 °C to ensure purity and viability. The reference strains Candida krusei ATCC 6258 and Candida parapsilosis ATCC 22,019 were included as quality controls36.
Medium preparation
As a test medium, Roswell Park Memorial Institute 1640 (RPMI) medium (with l-glutamine, with pH indicator, without bicarbonate) (Merck, Darmstadt, Germany) supplemented with d-glucose to a final concentration of 2%, buffered with 3-(N-morpholino) propanesulfonic acid (MOPS) (Merck) at a final concentration of 0.165 mol/L, and adjusted to pH 7.0 with 1 M sodium hydroxide, was used. To allow two-fold dilutions, and the preparation of RPMI petri dishes, the medium was prepared in double strength. After preparation, the medium was sterilized by vacuum filtration through a 0.22 µm pore size filter (Merck)36.
Drugs and microplate preparation
The combination was tested using the EUCAST guidelines for antifungal susceptibility testing of yeasts36, with modifications for a broth microdilution checkerboard procedure. Experiments were performed using Nunclon delta surface 96-wells microtiter plates for adherent cells (Thermo Fisher Scientific, Darmstadt, Germany). The included drugs were isavuconazole (Pfizer, Berlin, Germany) and colistin (Merck). The stock solutions of isavuconazole (3200 µg/mL) and colistin (12,800 µg/mL) were prepared in DMSO and sterile, distilled water, respectively. The drug dilutions were performed at four times the final concentration in double strength RPMI medium. The combination was studied on a two-dimensional checkerboard with two-fold dilutions. The final concentrations were 0.002 to 0.5 µg/mL and 1 to 64 µg/mL for isavuconazole and colistin, respectively. Fifty microliters of each concentration were distributed from row 1 to 8 for colistin and from column 1 to 11 for isavuconazole. Column 12 was used a as growth control and contained 100 µL of double strength RPMI medium with 1% of DMSO.
Inoculum preparation and inoculation of the microplates
Before the preparation of the inoculum, all isolates were subcultured for a second time on Sabouraud agar slants supplemented with chloramphenicol and cycloheximide and incubated at 35 °C, 95% humidity for 24 h. A few colonies were transferred to a sterile tube containing sterile distilled water. The suspension was counted in a haemocytometer and adjusted to 3.5 × 106 CFU/mL in sterile distilled water. This solution was used for the inoculation of the RPMI agar plates. The solution was further diluted to 2 × 105 CFU/mL, and 100 µL of the final inoculum were distributed in each well to inoculate the microdilution plates. The inoculum was further diluted and 100 µL were spread on a Sabouraud dextrose agar plate with a sterile Drigalski spatula. After an incubation time of 24–48 h at 35 °C, the CFU were counted to ensure the inoculum size and the viability of the yeasts. The microplates were incubated at 35 °C, 95% humidity, and the optical densities were read spectrophotometrically at 24 h at a wavelength of 530 nm with the spectrometer MultiSkan FC (Thermo Fisher Scientific). Before the reading, the microplates were shaken with the PMS-1000 Microplate Shaker (Grant Instruments, Shepreth, United Kingdom). In each set of experiments a blank microplate was included. Each well of the blank microplates was inoculated with 100 µL of sterile distilled water. Blank microplates were also incubated at 35 °C, 95% humidity for 24 h. Before calculation of the MICs, the blank plate was subtracted from the microplates inoculated with the yeasts. Experiments were run in triplicate on different days.
Interpretation of the checkerboard results
Fractional inhibition concentration index
The MICs alone and in combination were defined as the lowest concentration that gave 50% of inhibition compared to the growth control determined by spectrophotometric reading. For the calculation of the FICI, the high off-scale MICs were converted to the next log2 dilution. The FICI was calculated as follows: FICI = (MICin combination/MICalone)isavuconazole + (MICin combination/MICalone)colistin. The FICI data was interpreted following way: FICI ≤ 0.5 = synergy, FICI > 0.5–4 = no interaction, and FICI > 4.0 = antagonism47.
Response surface analysis
Response surface analysis are independent of endpoint definitions like the FICI analysis. The experimental data generated with the microplates as a percentage of growth compared to the growth control is transformed into a dose–response curve for each drug alone. Based on the Bliss model, a theoretical response surface of the combination corresponding to an indifferent interaction is calculated using the dose–response curves of both drugs. For the calculation of the synergy distribution, the modelled response surface is compared with experimental data. To visualize the results, the synergy levels were mapped onto the experimental combination dose–response surface48. To summarize the synergy distribution, the SUM-SYN-ANT metric was used, which represents the sum of synergy and antagonism observed. For the interpretation of the metric, a threshold of 24.5% was used as previously determined11. Synergy was assumed when the SUM-SYN-ANT was > 24.5%, and antagonism was assumed when and < − 24.5%. Between − 24.5 and 24.5%, no interaction was concluded. For the calculation of the SUM-SYN-ANT of the different isolates, the results of two different runs have been combined. All calculations were performed using Combenefit software38.
Preparation of the RPMI agar plates
Fifteen grams of agar were dissolved in 450 mL of distilled water. After the pH was adjusted to 7 with 0.1 M NaOH, the solution was set to 500 mL with distilled water, and autoclaved for 20 min at 121 °C and 2 bars. The liquid agar and 500 mL of double strength RPMI medium were put into a water bath at 50 °C. After the adjustment of the temperature to 50 °C, both solutions were mixed under a flow bench and stirred by a stir fish. Additionally, colistin RPMI agar plates contained the adequate volume of sterile colistin stock solution to a final of 64 µg/mL. Twenty microliters of the liquid RPMI agar or colistin RPMI agar were added to sterile petri dishes (diameter 90 mm) (Merck) under a flow bench and allowed to cool down.
Inoculation of RPMI agar plates
The RPMI agar plates were inoculated using the inoculator retro C80 (bioMérieux, Nürtingen, Germany). Briefly, a sterile cotton swap was soaked in the yeast suspension set to 3.5 × 106 CFU/mL, and excess fluid was removed by pressing the swab against the wall of the tube. A cross was gently drawn over the agar surface using the wet cotton swap. After the inoculator was turned on with maximum rotation, the cotton swap was moved from the edge of the agar surface to the middle of plate and back applying a slight pressure. After inoculation, the plates were allowed to dry and isavuconazole gradient concentration strips were placed onto the agar surface. For the activity of isavuconazole alone RPMI agar plates were used. For the activity of colistin alone, and for the combination, colistin RPMI agar plates were used. Activity of colistin alone, was tested by inoculation of the agar plate, without placement of a gradient concentration strip onto the surface. Agar plates were incubated at 35 °C and pictures were taken at 48 h. Reading of the MICs was done according to the recommendations of the manufacturer.
Interpretation of the results of RPMI agar plates
A decrease or an increase of ≥ 2 log2 dilutions in MIC compared to the most active drug has been defined as synergy or antagonism, respectively. A decrease or an increase of less than 2 log2 dilutions in MIC to the most active drug has been defined as no interaction9.
Comparison of EUCAST and gradient concentration strip MICs
Isavuconazole MICs obtained by EUCAST and gradient concentration strips were compared by a non-parametric unpaired t-test (Mann–Whitney). Essential agreement between the two methods was evaluated by calculating the percentage of the MICs, which differed by no more than 2 log2 dilutions.
Conference presentation
The results of this work (abstract number 2614) were published in the abstract book of the 30th European Congress of Clinical Microbiology and Infectious Diseases, supposed to be held 18th–21st April 2020 in Paris, France, but cancelled due to the COVID-19 pandemic.
References
Jeffery-Smith, A. et al. Candida auris: a review of the literature. Clin. Microbiol. Rev. https://doi.org/10.1128/CMR.00029-17 (2018).
Lone, S. A. & Ahmad, A. Candida auris—the growing menace to global health. Mycoses 62, 620–637. https://doi.org/10.1111/myc.12904 (2019).
Spivak, E. S. & Hanson, K. E. Candida auris: an emerging fungal pathogen. J. Clin. Microbiol. https://doi.org/10.1128/JCM.01588-17 (2018).
Satoh, K. et al. Candida auris sp. Nov., a novel ascomycetous yeast isolated from the external ear canal of an inpatient in a Japanese hospital. Microbiol. Immunol. 53, 41–44. https://doi.org/10.1111/j.1348-0421.2008.00083.x (2009).
Bidaud, A. L., Chowdhary, A. & Dannaoui, E. Candida auris: an emerging drug resistant yeast—a mini-review. J. Mycol. Med. 28, 568–573. https://doi.org/10.1016/j.mycmed.2018.06.007 (2018).
Chowdhary, A. et al. A multicentre study of antifungal susceptibility patterns among 350 Candida auris isolates (2009–17) in India: role of the ERG11 and FKS1 genes in azole and echinocandin resistance. J. Antimicrob. Chemother. 73, 891–899. https://doi.org/10.1093/jac/dkx480 (2018).
Lockhart, S. R. et al. Simultaneous emergence of multidrug-resistant Candida auris on 3 continents confirmed by whole-genome sequencing and epidemiological analyses. Clin. Infect. Dis. 64, 134–140. https://doi.org/10.1093/cid/ciw691 (2017).
Osei Sekyere, J. Candida auris: a systematic review and meta-analysis of current updates on an emerging multidrug-resistant pathogen. Microbiologyopen 7, e00578. https://doi.org/10.1002/mbo3.578 (2018).
Vitale, R. G., Afeltra, J. & Dannaoui, E. Antifungal combinations. Methods Mol. Med. 118, 143–152. https://doi.org/10.1385/1-59259-943-5:143 (2005).
Bidaud, A. L., Botterel, F., Chowdhary, A. & Dannaoui, E. In vitro antifungal combination of flucytosine with amphotericin B, voriconazole, or micafungin against Candida auris shows no antagonism. Antimicrob. Agents Chemother. https://doi.org/10.1128/AAC.01393-19 (2019).
Bidaud, A. L., Djenontin, E., Botterel, F., Chowdhary, A. & Dannaoui, E. Colistin interacts synergistically with echinocandins against Candida auris. Int. J. Antimicrob. Agents 55, 105901. https://doi.org/10.1016/j.ijantimicag.2020.105901 (2020).
Fakhim, H. et al. In vitro interactions of echinocandins with triazoles against multidrug-resistant Candida auris. Antimicrob. Agents Chemother. https://doi.org/10.1128/AAC.01056-17 (2017).
O’Brien, B., Chaturvedi, S. & Chaturvedi, V. In vitro evaluation of antifungal drug combinations against multidrug-resistant Candida auris isolates from New York outbreak. Antimicrob. Agents Chemother. https://doi.org/10.1128/AAC.02195-19 (2020).
Gregoire, N., Aranzana-Climent, V., Magreault, S., Marchand, S. & Couet, W. Clinical pharmacokinetics and pharmacodynamics of colistin. Clin. Pharmacokinet. 56, 1441–1460. https://doi.org/10.1007/s40262-017-0561-1 (2017).
Brennan-Krohn, T., Pironti, A. & Kirby, J. E. Synergistic activity of colistin-containing combinations against colistin-resistant Enterobacteriaceae. Antimicrob. Agents Chemother. https://doi.org/10.1128/AAC.00873-18 (2018).
Ben-Ami, R., Lewis, R. E., Tarrand, J., Leventakos, K. & Kontoyiannis, D. P. Antifungal activity of colistin against Mucorales species in vitro and in a murine model of Rhizopus oryzae pulmonary infection. Antimicrob. Agents Chemother. 54, 484–490. https://doi.org/10.1128/AAC.00956-09 (2010).
Yousfi, H., Ranque, S., Rolain, J. M. & Bittar, F. In vitro polymyxin activity against clinical multidrug-resistant fungi. Antimicrob. Resist. Infect. Control 8, 66. https://doi.org/10.1186/s13756-019-0521-7 (2019).
MacCallum, D. M., Desbois, A. P. & Coote, P. J. Enhanced efficacy of synergistic combinations of antimicrobial peptides with caspofungin versus Candida albicans in insect and murine models of systemic infection. Eur. J. Clin. Microbiol. Infect. Dis. 32, 1055–1062. https://doi.org/10.1007/s10096-013-1850-8 (2013).
Schemuth, H. et al. In vitro activity of colistin as single agent and in combination with antifungals against filamentous fungi occurring in patients with cystic fibrosis. Mycoses 56, 297–303. https://doi.org/10.1111/myc.12022 (2013).
Teixeira-Santos, R. et al. Unveiling the synergistic interaction between liposomal amphotericin B and colistin. Front. Microbiol. 7, 1439. https://doi.org/10.3389/fmicb.2016.01439 (2016).
Zeidler, U. et al. Synergy of the antibiotic colistin with echinocandin antifungals in Candida species. J. Antimicrob. Chemother. 68, 1285–1296. https://doi.org/10.1093/jac/dks538 (2013).
Natesan, S. K. & Chandrasekar, P. H. Isavuconazole for the treatment of invasive aspergillosis and mucormycosis: current evidence, safety, efficacy, and clinical recommendations. Infect. Drug Resist. 9, 291–300. https://doi.org/10.2147/IDR.S102207 (2016).
Arendrup, M. C., Prakash, A., Meletiadis, J., Sharma, C. & Chowdhary, A. Comparison of EUCAST and CLSI reference microdilution MICs of eight antifungal compounds for Candida auris and associated tentative epidemiological cutoff values. Antimicrob. Agents Chemother. https://doi.org/10.1128/AAC.00485-17 (2017).
Ruiz-Gaitan, A. C., Canton, E., Fernandez-Rivero, M. E., Ramirez, P. & Peman, J. Outbreak of Candida auris in Spain: a comparison of antifungal activity by three methods with published data. Int. J. Antimicrob. Agents 53, 541–546. https://doi.org/10.1016/j.ijantimicag.2019.02.005 (2019).
Zhu, N. et al. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 382, 727–733. https://doi.org/10.1056/NEJMoa2001017 (2020).
Sanders, J. M., Monogue, M. L., Jodlowski, T. Z. & Cutrell, J. B. Pharmacologic treatments for coronavirus disease (COVID-19): a review. JAMA. https://doi.org/10.1001/jama.2020.6019 (2019).
Hussman, J. P. Cellular and molecular pathways of COVID-19 and potential points of therapeutic intervention. Front. Pharmacol. https://doi.org/10.3389/fphar.2020.01169 (2020).
Pushpakom, S. et al. Drug repurposing: progress, challenges and recommendations. Nat. Rev. Drug Discov. 18, 41–58. https://doi.org/10.1038/nrd.2018.168 (2019).
Miro-Canturri, A., Ayerbe-Algaba, R. & Smani, Y. Drug repurposing for the treatment of bacterial and fungal infections. Front. Microbiol. 10, 41. https://doi.org/10.3389/fmicb.2019.00041 (2019).
Bass, J. B. Jr. et al. Treatment of tuberculosis and tuberculosis infection in adults and children. Am. J. Respir. Crit. Care Med. 149, 1359–1374. https://doi.org/10.1164/ajrccm.149.5.8173779 (1994).
Schwarz, P., Cornely, O. A. & Dannaoui, E. Antifungal combinations in Mucorales: a microbiological perspective. Mycoses https://doi.org/10.1111/myc.12909 (2019).
Schwarz, P. & Dannaoui, E. In vitro interaction between isavuconazole and tacrolimus, cyclosporin A, or sirolimus against Aspergillus Species. J. Fungi (Basel). https://doi.org/10.3390/jof6030103 (2020).
Schwarz, P., Schwarz, P. V., Felske-Zech, H. & Dannaoui, E. In vitro interactions between isavuconazole and tacrolimus, cyclosporin A or sirolimus against Mucorales. J. Antimicrob. Chemother. 74, 1921–1927. https://doi.org/10.1093/jac/dkz102 (2019).
Yousfi, H., Ranque, S., Cassagne, C., Rolain, J. M. & Bittar, F. Identification of repositionable drugs with novel antimycotic activity by screening the Prestwick Chemical Library against emerging invasive moulds. J. Glob. Antimicrob. Resist. 21, 314–317. https://doi.org/10.1016/j.jgar.2020.01.002 (2020).
Lim, L. M. et al. Resurgence of colistin: a review of resistance, toxicity, pharmacodynamics, and dosing. Pharmacotherapy 30, 1279–1291. https://doi.org/10.1592/phco.30.12.1279 (2010).
Arendrup, M. C. et al. Method for the determination of broth dilution minimum inhibitory concentrations of antifungal agents for yeasts (EUCAST definitive document E.Def 7.3.2) (2020).
Prichard, M. N. & Shipman, C. Jr. A three-dimensional model to analyze drug–drug interactions. Antiviral Res. 14, 181–205 (1990).
Di Veroli, G. Y. et al. Combenefit: an interactive platform for the analysis and visualization of drug combinations. Bioinformatics 32, 2866–2868. https://doi.org/10.1093/bioinformatics/btw230 (2016).
Te Dorsthorst, D. T. A. et al. In vitro interaction of flucytosine combined with amphotericin B or fluconazole against thirty-five yeast isolates determined by both the fractional inhibitory concentration index and the response surface approach. Antimicrob. Agents Chemother. 46, 2982–2989 (2002).
Reed, M. D., Stern, R. C., O’Riordan, M. A. & Blumer, J. L. The pharmacokinetics of colistin in patients with cystic fibrosis. J. Clin. Pharmacol. 41, 645–654. https://doi.org/10.1177/00912700122010537 (2001).
Spapen, H., Jacobs, R., Van Gorp, V., Troubleyn, J. & Honore, P. M. Renal and neurological side effects of colistin in critically ill patients. Ann. Intensive Care 1, 14. https://doi.org/10.1186/2110-5820-1-14 (2011).
Garonzik, S. M. et al. Population pharmacokinetics of colistin methanesulfonate and formed colistin in critically ill patients from a multicenter study provide dosing suggestions for various categories of patients. Antimicrob. Agents Chemother. 55, 3284–3294. https://doi.org/10.1128/AAC.01733-10 (2011).
Kontoyiannis, D. P. et al. Calcineurin inhibitor agents interact synergistically with antifungal agents in vitro against Cryptococcus neoformans isolates: correlation with outcome in solid organ transplant recipients with cryptococcosis. Antimicrob. Agents Chemother. 52, 735–738. https://doi.org/10.1128/AAC.00990-07 (2008).
Cendejas-Bueno, E. et al. Reclassification of the Candida haemulonii complex as Candida haemulonii (C. haemulonii group I), C. duobushaemulonii sp. nov. (C. haemulonii group II), and C. haemulonii var. vulnera var. nov.: three multiresistant human pathogenic yeasts. J. Clin. Microbiol. 50, 3641–3651 (2012).
Chowdhary, A. et al. New clonal strain of Candida auris, Delhi, India. Emerg. Infect. Dis. 19, 1670–1673 (2013).
Kim, M.-N. et al. Candida haemulonii and closely related species at 5 university hospitals in Korea: identification, antifungal susceptibility, and clinical features. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 48, e57-61 (2009).
Odds, F. C. Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother. 52, 1. https://doi.org/10.1093/jac/dkg301 (2003).
Otto, R. G. et al. An alternative strategy for combination therapy: interactions between polymyxin B and non-antibiotics. Int. J. Antimicrob. Agents https://doi.org/10.1016/j.ijantimicag.2018.09.003 (2018).
Acknowledgements
The authors are grateful to Pfizer for providing the drug isavuconazole for this research project. The authors wish to thank Johanna Ruehl for excellent technical assistance during the conduct of the experiments.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was supported by internal funding.
Author information
Authors and Affiliations
Contributions
P.S. performed the experiments and wrote the first draft of the manuscript. All authors analyzed the results. The figures were prepared by A-L.B. and E.D. E.D. and P.S. contributed to the revisions. All authors drafted the final article.
Corresponding author
Ethics declarations
Competing interests
Patrick Schwarz has received research grants from Basilea Pharmaceutica, Gilead and Pfizer and received travel grants from Gilead and Pfizer. During the past 5 years, Eric Dannaoui has received research grants from MSD and Gilead; travel grants from Gilead, MSD, Pfizer, and Astellas, and speaker’s fee from Gilead, MSD, and Astellas. Anne-Laure Bidaud has none to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schwarz, P., Bidaud, AL. & Dannaoui, E. In vitro synergy of isavuconazole in combination with colistin against Candida auris. Sci Rep 10, 21448 (2020). https://doi.org/10.1038/s41598-020-78588-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-78588-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.