Abstract
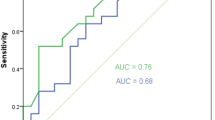
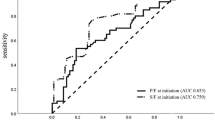
To analyze the relationship of the central venous-to-arterial carbon dioxide difference (p(cv-a)CO2) and cardiac index (CI) in patients with septic shock, an observational study was conducted in intensive care unit (ICU). 66 consecutive patients with septic shock and central venous oxygen saturation (ScvO2) ≥ 70% were included after early fluid resuscitation. Measurements were taken at a 6 h interval (T0, T6, T12, T18, T24) during first 24 h after their admission into ICU, including heart rate (HR), mean arterial pressure (MAP), central venous pressure (CVP), p(cv-a)CO2, cardiac index(CI, L/(min•m2)) and ScvO2. Patients were divided into low p(cv-a)CO2 group (n = 35) and high p(cv-a)CO2 group (n = 31) according to a threshold of 6 mmHg for p(cv-a)CO2 at T0. As a result, at T0, T6, T12, T18 and T24, there were respectively significant differences between low and high p(cv-a)CO2 groups for CI (4.1 ± 1.4 vs 2.4 ± 0.6, 4.4 ± 0.9 vs 2.8 ± 0.7, 4.1 ± 1.3 vs 2.9 ± 0.6, 4.0 ± 1.3 vs 2.7 ± 0.8, 4.2 ± 1.4 vs 2.9 ± 0.8, p < 0.001 at each time point), 28-day mortality rate was 38.7%(12/31) for high p(cv-a)CO2 group and 22.8% (8/35) for low p(cv-a)CO2 group (p > 0.05), there were significant differences for p(cv-a)CO2 (p < 0.05) between low and high p(cv-a)CO2 groups, no differences for HR, MAP, CVP, ScvO2 (p > 0.05). CI was inversely correlated with p(cv-a)CO2 value (r = −0.804, p < 0.001), but not for ScvO2(r = 0.08, p > 0.05). Receiver operating characteristic curve analysis confirmed the correlation of p(cv-a)CO2 with CI (AUC: 0.782;p < 0.001; 95% confidence interval: 0.710–0.853). The cut-off value for the best predictive value of CI ≥ 2.2 L/(min·m2) was p(cv-a)CO2 of 5.55 mmHg or lower with a sensitivity of 85.7% and specificity of 66.8%. Hence CI measured with USCOM is inversely correlated with p(cv-a)CO2 values in guiding the resuscitation of patients with septic shock.
Similar content being viewed by others
Introduction
In 2016, sepsis and septic shock was re-documented as fatal organ dysfunction caused by infection-induced host response disorders1. Infectious shock is a subtype of sepsis; its circulation abnormalities significantly increase the mortality rate. Low blood volume, antihypertensive drugs needed to maintain MAP ≥ 65 mmHg and serum lactic acid >2 mmol/L can confirm septic shock. The definition was updated to facilitate rapid identification and timely treatment. Despite the continuous progress of awareness and intervention, the mortality rate of septic shock is approaching 40% or more2. Infectious shock exists in the presence of imbalance of oxygen supply and demand as well as tissue hypoxia, early improvement of tissue hypo-perfusion is key to the treatment, a specific cluster treatment program was recommended in the guidelines of sepsis rescue action3. Central venous oxygen saturation as one of the key goals of early goal management is widely used to guide resuscitation therapy for better tissue perfusion. In fact, normal ScvO2 does not exclude tissue hypo-perfusion4,5. Carbon dioxide partial pressure difference is proportional to carbon dioxide production, and is inversely proportional to cardiac output, its normal value is 2~5 mmHg, CO of more than 6 mmHg means that peripheral blood flow is not sufficient to clear out carbon dioxide6. Numerous studies suggest that partial pressure difference of carbon dioxide may be an indicator to improve tissue perfusion for guiding early resuscitation of sepsis7,8,9. The use of continuous ultrasonic cardiac output monitor (USCOM), which is noninvasive and widely used in the severely sick patients, is convenient, fast and reproducible to monitor hemodynamics and to guarantee the accuracy of cardiac output and cardiac index10. This study was conducted to investigate the relationship between (p(cv-a)CO2) and USCOM-measuring CI in patients with septic shock.
Patients and Methods
Jan 2016 Through Dec 2017, 66 patients with septic shock were admitted into the severe medical department of Beidaihe Hospital and North China Petroleum Administration General Hospital (ICU), those patients who undertook early fluid resuscitation in 6 hours and got the value of ScvO2 ≥ 70% were included in this retrospective study following the criteria: (1) met the diagnostic criteria of septic shock issued by international sepsis and septic shock treatment guidelines for septic shock in 20113; (2) early fluid resuscitation was conducted following the cluster treatment program of the sepsis action guideline. According to the guideline, the early goal-oriented treatment was applied in our unit. (3) ScvO2 ≥ 70% was achieved 6 hours after resuscitation; (4) ≥18 years old. Patients with incomplete data were excluded. Baseline venous and arterial blood gas analysis was measured every 6 hours in 24 hours. USCOM was used to measure CI, its probe was placed on the sternum or the supra-clavicular fossa to obtain the strongest signal, and measurement was taken for 3 consecutive times, each deviation did not exceed 10% to take the average of CI. This study was approved by Ethics Committees of Baidaihe Hospital and North China Petroleum Hospital. Informed consents were obtained from the patients’ family. All procedures followed were in accordance with the ethical standards of responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions.
The patients’ age, sex, diagnosis, APACHE IIscore were obtained. Early fluid resuscitation was started, time points of 0, 6, 12, 18, 24 hours after resuscitation were T0, T6, T12, T18, T24. Data like heart rate (HR), MAP, CVP, p(cv-a)CO2, CI and ScvO2 was collected at each time point. p(cv-a)CO2 was the difference between pcvCO2 and paCO2, the normal value was less than 6 mmHg. The cut-off value of p(cv-a)CO2 at T0 was 6 mmHg, the group with <6 mmHg or with ≥6 mmHg were low p(cv-a)CO2 group (T0) or high p(cv-a)CO2 group. Based on the hemodynamic data, the relationship between CI and p (cv-a)CO2 was analyzed.
Statistical
All numeration variables were stated as median, and continuous variables were presented as means ± standard deviation and tested by normal distribution and analyzed by One-Way ANOVA; sampling rates were analyzed with x2 test, the correlation between CI and p(cv-a)CO2 and ScvO2 was analyzed by the Spearman test, the diagnostic characteristic curve (ROC curve) was used to evaluate the diagnostic value of the parameters, the value of p < 0.05 was set as significant difference. All data was analyzed by statistical software SPSS22.0 (IBM Corp, Armonk, NY, USA).
Results
For the low p(cv-a)CO2 group, 20 male and 15 female patients aged 64.9 ± 12.5 years, the number of patients with ScvO2 ≥ 70% at T0 was 24 (68.6%). For the high p(cv-a)CO2 group, 18 male and 13 female patients aged 65.5 ± 10.4 years, the number of patients with ScvO2 ≥ 70% at T0 was 16(51.6%). At T6, the number of patients with p(cv-a)CO2 ≥ 6 mmHg in the low p (cv-a)CO2 group was 3(8.6%), while this number in the high p(cv-a)CO2 group was 17(54.8%), the total number of patients with p(cv-a)CO2 ≥ 6 mmHg was 20, account for 30.3% of all patients. There were no significant differences in age, sex and APACHEIIscore between two groups (p > 0.05) (Table 1), and no difference for patients with ScvO2 ≥ 70% (p > 0.05), no difference for infection sites including lung, peritoneal cavity, urinary system and other sites. For HR, MAP, CVP, there were no significant differences between two groups (p > 0.05), 28-day mortality rate was different, which was 38.7% (12/31)for high p(cv-a)CO2 group and 22.8% (8/35) for low p(cv-a)CO2 group (p > 0.05). There were significant differences for CI at respective time point between two groups (p < 0.001) (Table 2). The value of p(cv-a)CO2 was evaluated by ROC curve to predict CI (Fig. 1). Area under ROC curve was 0.782, the sensitivity was 0.857 and the specificity was 0.668 when p(cv-a)CO2 was ≤5.55 mmHg to follow CI ≥ 2.2 L/(min•m2) (Fig. 2).
Discussion
p(cv-a)CO2 is well-accepted to study carbon dioxide partial pressure difference8, the combination of p(cv-a)CO2 and ScvO2 can guide therapeutic shock resuscitation to avert fluid overload due to pseudo-normalization of ScvO2. The clinical significance of p(cv-a)CO2 is as follows: (1) The initial increase of p(cv-a)CO2 is more than 6 mmHg, which indicates that the blood flow may be insufficient, even if the microcirculation parameters (including ScvO2) are normal. CO should be increased to improve tissue perfusion, especially in the presence of hypoxia (elevated lactate). (2) normal p(cv-a)CO2 range (<6 mmHg) is indicative that blood flow from the peripheral cycle clears out carbon dioxide, improving heart output is not the preferred treatment, even if tissue hypoxia exists9. In our study, under the condition of ScvO2 compliance after resuscitation, most patients achieved p(cv-a)CO2 ≥ 6 mmHg at T0, T6. Although after the early fluid resuscitation treatment, there are still some patients with insufficient venous blood flow to clear out CO2 in the peripheral tissue. In the early resuscitation phase, those patients may need more active and longer duration of resuscitation therapy. Leisman et al. reported that fluid resuscitation was started in these patients in 30 min, the mortality rate was only 13.3%, and that initiation of fluid resuscitation was delayed 30 min, mortality increased over the prolonged fluid resuscitation10,11,12,13. Numerous studies have shown that p(cv-a)CO2 can be one of the goals of resuscitation treatment. There were no significant differences in hemodynamic parameters respective of CI and p(cv-a)CO2 between two groups in our study, in the process of resuscitation, cardiac output is clinically lower than normal, ScvO2 cannot be low. When shock occurs, mitochondria cannot use oxygen for energy metabolism, it is cytopathic hypoxia, although this stage ScvO2 can be increased, or even abnormally increased, unrelated to more oxygen transport, it is still an important manifestation of tissue hypoxia that predicts a poor prognosis4. CI is conveniently measured with USCOM, which is a new non-invasive hemodynamic monitoring method that is continuous Doppler technology to obtain hemodynamic parameters. Compared with floating catheters and pulse-indicated continuous cardiac output with invasive operations and catheter-related complications14, USCOM is increasingly applied in the clinical practice due to its rapidity and reproducibility to monitor hemodynamics and to guarantee the accuracy of CO and CI. p(cv-a)CO2 is inversely proportional to CO, and p(cv-a)CO2 is elevated in case of tissue CO2 retention when cardiac function is not good enough to provide adequate venous blood flow. Our report demonstrated that CI in some patients was still low after successful resuscitation. Rivers et al. reported that the outcomes for an early goal-oriented treatment for sepsis and septic shock, mortality rate was decreased by 15% of patients15,16,17. Ho et al. reported that the application of key point control strategies improved the compliance of clinicians with guidelines for cluster therapy for septic shock, the ICU stay time was reduced from 9.8 days to 7.2 days, in-hospital mortality rate went down from 40.0% to 23.1%12, our study substantiated that p(cv-a)CO2 was negatively correlated with CI, not correlated with ScvO2. Valle’e et al. reported that 6 mmHg as the threshold was predictive of insufficient early resuscitation for patients to reach ScvO2 ≥ 70%18,19,20. Mallat et al. also reported that CI and p(cv-a)CO2 were negatively correlated13, our result resembled these documents though our limitation in this report was mainly due to small sample size. Low CI means that venous blood flow is not sufficient to wash out CO2 in the peripheral tissue14, Therefore, simultaneous monitoring of CI and p(cv-a)CO2 is beneficial to determine cardiac function status and whether adequate venous blood flow is provided to meet the need of CO2 clearance from peripheral tissues.
Conclusion
In sepsis, CI and p(cv-a)CO2 are negatively correlated, the latter is useful parameter to evaluate cardiac output in the course of shock resuscitation.
References
Singer, M. et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 315, 801–810 (2016).
Gasim, G. I. et al. Sepsis in Buraidah Central Hospital, Qassim, Kingdom of Saudi Arabia. Int J Health Sci (Qassim). 10(2), 175–181 (2016).
Rhodes, A. et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 43(3), 304–377 (2017).
Pope, J. V. et al. Multicenter study of central venous oxygen saturation (ScvO(2)) as a predictor of mortality in patients with sepsis. Ann Emerg Med. 55(1), 40–46 (2010).
Cecconi, M. et al. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Med. 40(12), 1795–1815 (2014).
Mallat, J., Lemyze, M., Tronchon, L., Vallet, B. & Thevenin, D. Use of venous-to-arterial carbon dioxide tension difference to guide resuscitation therapy in septic shock. World J Crit Care Med. 5(1), 47–56 (2016).
Du, W. et al. Combining central venous-to-arterial partial pressure of carbon dioxide difference and central venous oxygen saturation to guide resuscitation in septic shock. J Crit Care. 28(6), 1110.e1–5 (2013).
He, H. W., Liu, D. W., Long, Y. & Wang, X. T. High central venous-to-arterial CO2 difference/arterial-central venous O2 difference ratio is associated with poor lactate clearance in septic patients after resuscitation. J Crit Care. 31(1), 76–81 (2016).
Perner, A., Haase, N., Wiis, J., White, J. O. & Delaney, A. Central venous oxygen saturation for the diagnosis of low cardiac output in septic shock patients. Acta Anaesthesiol Scand. 54(1), 98–102 (2010).
Chong, S. W. & Peyton, P. J. A meta-analysis of the accuracy and precision of the ultrasonic cardiac output monitor (USCOM). Anaesthesia. 67(11), 1266–1271 (2012).
Cuschieri, J. et al. Central venous-arterial carbon dioxide difference as an indicator of cardiac index. Intensive Care Med 31(6), 818–822 (2005).
van Beest, P. A. et al. Central venous-arterial pCO2 difference as a tool in resuscitation of septic patients[J]. Intensive Care Med. 39(6), 1034–1039 (2013).
Mallat, J. et al. Central venous-to-arterial carbon dioxide partial pressure difference in early resuscitation from septic shock: a prospective observational study. Eur J Anaesthesiol. 31(7), 371–380 (2014).
Critchley, L. A., Lee, A. & Ho, A. M. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 111(5), 1180–1192 (2010).
Bihari, S., Prakash, S. & Bersten, A. D. Post resusicitation fluid boluses in severe sepsis or septic shock: prevalence and efficacy (price study). Shock. 40(1), 28–34 (2013).
Ho, K. M., Harding, R., Chamberlain, J. & Bulsara, M. A comparison of central and mixed venous oxygen saturation in circulatory failure. J Cardiothorac Vasc Anesth. 24(3), 434–439 (2010).
ProCESS Investigators. et al. A randomized trial of protocol-based carefor early septic shock. N Engl J Med. 370(18), 1683–1693(2014).
ARISE Investigators. et al. Goal-directed resuscitation for patients with early septic shock. N Engl J Med. 71(16),1496–1506 (2014).
PRISM Investigators. Early, goal-directed therapy for septic shock - A patient-level meta-analysis. N Engl J Med. 376(23), 2223–2234 (2017).
Vallée, F. et al. Central venous-to-arterial carbon dioxide difference: an additional target for goal-directed therapy in septic shock? Intensive Care Med. 34(12), 2218–2225 (2008).
Author information
Authors and Affiliations
Contributions
Conceived, wrote and finalized the study: Zhiqiang Guo. Revised the draft: Ming Yin, Jichang Kong. Perform the statistical analysis: Bin Wang, Kunpeng Dai. Guangyan Yu. Collected all references: Zhiyun Li, Yong Bao.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guo, Z., Yin, M., Kong, J. et al. Relationship Analysis of Central Venous-to-arterial Carbon Dioxide Difference and Cardiac Index for Septic Shock. Sci Rep 9, 8822 (2019). https://doi.org/10.1038/s41598-019-45252-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-45252-6
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.