Abstract
The study aimed to compare the surgical outcomes of septoplasty with inferior turbinectomy between in-patient and out-patient groups. A total of 152 patients who underwent septoplasty with inferior turbinectomy between May 2012 and February 2013 were retrospectively reviewed and divided into in-patient group and out-patient group. The two groups were compared in three aspects: (i) consumption of medical resources, including National Health Insurance payments, patient surcharges, and total surgical expenses; (ii) prognostic indicators; and (iii) post-operative complications. There were no statistically significant differences between the prognostic indicators or post-operative complications in the 2 study groups except for “duration of nasal decongestant use”. The in-patient group had higher medical resource consumption in all categories. In conclusion, septoplasty with inferior turbinectomy can be performed cost-effectively as an out-patient procedure with satisfactory quality and adequate safety.
Similar content being viewed by others
Introduction
Nasal septal deviation (NSD) occurs in 77–90% of the general population1,2. Septoplasty with inferior turbinectomy is one of the most common surgeries for NSD and chronic hypertrophic rhinitis (CHR). The major goals of this operation include improving nasal flow, relieving obstructive sleep apnea, and rhinogenic headache. Although there are a number of possible approaches to conduct a septoplasty, most surgeons utilize a similar technique that includes submucosal resection of the cartilaginous nasal septum (SMR), controlled osteotomy of bony nasal septum, and concomitant inferior turbinectomy. This kind of surgery can be performed as either an ambulatory or an in-patient procedure.
Previous studies have revealed the variation in the day-surgery rate among septoplasties in different parts of the world. In 1998, it was estimated that only 2.2% of all septoplasties were performed as day cases in the United Kingdom (UK)3. In 2005, a 250-bed hospital in Italy had 69% of their septoplasties performed as ambulatory procedures4. A more recent report from Portugal demonstrated that 77% of the septoplasties were undertaken as outpatient procedures5. In Taiwan however, most septoplasties with concomitant inferior turbinectomy are still performed as in-patient procedures. The increasing trend towards day-surgery procedures due to continuous improvements in medical practices as well as economic factors has profoundly changed the management of patient hospitalization6,7,8.
Under the hypothesis that septoplasty with inferior turbinectomy would be a good candidate for day-case surgery without compromising patient safety or clinical outcome, this retrospective study is to compare the prognosis, complications, and expense associated with this surgery as an in-patient or out-patient procedure.
Methods
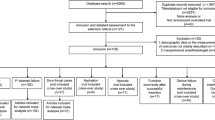
One hundred and fifty-two patients who underwent septoplasty and inferior turbinectomy at Hsinchu Cathay General Hospital, Hsinchu, Taiwan between May 2012 and February 2013 were included in this study. Every patient had nasal septal deviation and inferior turbinate hypertrophy confirmed by physical examination. A standardized pre-operative questionnaire including age, sex, and other systemic diseases was collected from every patient. Patients with major systemic co-morbidity (e.g., uremia, liver cirrhosis, or cancer) were excluded. Patients who underwent concomitant endoscopic sinus surgery or rhinoplasty (both cosmetic and functional) were also excluded from the analyses.
Preoperatively, the patients could decide whether to admit for the procedure or not. The out-patient group left the hospital almost immediately after the surgery following a brief 30-minute break in the observation room. The in-patient group were admitted to the hospital several hours before the surgery and stayed in the wards for one or two nights after the procedure (mostly one night).
All of the procedures were performed by a single surgeon (senior author) under local anesthesia using the same operative technique. Prior to the SMR surgery, lidocaine with 1:100000 adrenaline was injected to the septal mucosa on both sides. A Killian incision was made and bilateral mucoperichondrium and mucoperiosteum were elevated from the cartilaginous and bony septum. The deviated septal cartilage and bone were removed by forceps under endoscope, while preserving adequate caudal and dorsal strut. At the end of the surgery, the mucosa was closed at the incision line using one or two absorbable trans-mucosal sutures, together with potassium titanyl phosphate (KTP) laser vaporization of both inferior turbinates. As to the nasal packing, non-resolvable Merocel® (standard 8 cm, expandable polyvinyl acetate; Metronic Xomed, Jacksonville, FL) or biodegradable Nasopore (Forte plus 8 cm, Polyganics, Rozenburglaan, Groningen, The Netherlands) coated with neomycin ointment were used for nasal packing depending on the preference of the patient (we didn’t have preference from the medical professional point of view). For patients who received Merocel, the packing was removed within 24–48 hours of the operation. For patients who received Nasopore, the packing was left in the nasal cavity where it could break down spontaneously without any manipulation. Any residual fragments and crust were cleaned out during the follow-up visit (usually at day 7 post-surgery).
The post-operative regimens for the patients in the two groups were quite similar, including one-day oral antibiotic therapy (cephalexin 500 mg qid), together with topical nasal steroids. Analgesics were not routinely given. Decongestant medication was given whenever patients complained of nasal obstruction, which made it an ideal indicator for post-operative nasal airway patency. All of the patients were regularly followed-up in the clinic, and the post-operative complications were recorded in the medical charts. The end-point of follow-up was smooth nasal breathing post-operatively with no residual crust or exudates found in either nasal cavity. The better the wound healed, the shorter recovery time and the fewer decongestant medications the patient needed.
A retrospective review of medical records and data collection were conducted by an independent reviewer. Several parameters were investigated following the surgical procedure, and differences between the two study groups were compared in three aspects: (i) consumption of medical resources, including National Health Insurance payments (US dollars), patient surcharges (US dollars), and total surgical expenses (sum of the previous two items); (ii) prognostic indicators, including the duration of nasal decongestant use, number of follow-up visits, and total period to complete recovery; and (iii) post-operative complications, including post-operative hemorrhage, subsequent septal hematoma, septal perforation, nasal adhesions (synechiae), and wound infection. Post-operative hemorrhage was defined as massive bleeding that required emergency management or re-packing at any time during the follow-up period.
Statistical analysis
Statistical analyses were performed using SPSS for Windows version 16.0 (SPSS Inc., Chicago, IL). Categorical variables were analyzed using the chi-square test and Fisher’s exact test, as appropriate. Differences between the groups were analyzed using the t-test. Statistical significance was set at p < 0.05.
Ethics approval and consent to participate
The hospital Institutional Review Board (Hsinchu Cathay General Hospital, Hsinchu, Taiwan) approved this study. All experiments were performed in accordance with the Hsinchu Cathay General Hospital Research Ethics Committee guidelines and regulations. Informed consent was obtained from all the patients.
Results
Characteristics of the study subjects
The study cohort of 152 patients had a mean age of 37.0 ± 11.2 years (range, 18–65 years) and included 99 men (65.1%) and 53 women (34.9%). The two groups (in-patient and out-patient groups) were not significantly different in terms of age, gender, and packing material (shown in Table 1).
Comparison of prognostic indicators
The period to complete recovery and the number of follow-up visit showed no statistical difference between in-patient and out-patient groups (p = 0.928 and 0.579 respectively). Only the duration of nasal decongestant use was significantly different in in-patient and out-patient groups (shown in Table 2).
Incidence of post-operative complications
In terms of post-operative complications, none of them showed statistical difference between in-patient and out-patient groups, and there was no case of wound infection in either group (shown in Table 3).
Analysis according to nasal packing materials
To eliminate the influence of nasal packing, we analyzed the patients separately according to their nasal packing materials (Merocel or Nasopore). In patients using Merocel as nasal packing, we found no differences between in-patient and out-patient on prognostic indicators or post-operative complications except for the parameter “duration of nasal decongestant use”. In patients using Nasopore as nasal packing, we found similar result (shown in Tables 4 and 5).
Comparison of medical resource consumption
In comparing the medical expenses between the study groups, in-patient group had higher medical resource consumption across all categories than out-patient group. (shown in Table 6).
Discussion
The National Health Insurance (NHI) system was established in 1995 in Taiwan to cover most of the medical and health service demands of the population. Similar to the National Health Service in the UK however, increasing pressures on NHI resources has led to reassessment of many common procedures with a view to establish the feasibility and safety of performing these as day cases. The increased in-patient load also makes it difficult to guarantee beds for elective patients8,9,10.
Within the last decade, there has been a rapid expansion in ambulatory surgery with day operations already accounting for half of the surgical workload in the US and the UK. However, there are widely differing perceptions about the appropriateness of day-surgery for septoplasty. Septoplasty is being performed routinely as a day-procedure in many countries in the world, but in Taiwan, the majority of such surgeries are still in-patient procedures, with the patient staying overnight at the hospital until the nasal packing is removed the following day8,11,12,13,14. The emerging perspectives on septoplasty as a routine outpatient procedure are now under review in Taiwan, yet few studies have been performed with local data.
We found no statistically significant difference between in-patient and out-patient groups in the analyzed prognostic indicators such as the period to complete recovery and the number of follow-up visit, but the duration of nasal decongestant use. This means the two groups reached the recovery end-point at the same time but more medications were prescribed in the in-patient group. We speculated that the reason might lie on different patient behaviors in and out of the hospital. For in-patient group, decongestant prescription could be easily accessed in the ward whenever they complained of nasal obstruction, which was the most frequent complaint immediately after nasal surgery. As a result, in-patients tended to be more dependent on the decongestant medication, even after they went home. In contrast, the use of decongestant medication was significantly reduced in out-patient group during follow-up period.
Some surgeons may have concerns that an out-patient procedure without continuous nursing care may increase the risk of post-operative infection or other complications. In our study, the incidence of post-operative complications (i.e., post-operative hemorrhage, subsequent septal hematoma, septal perforation, or nasal adhesions) showed no significant difference between in-patient and out-patient groups. In addition, no wound infections were recorded in either of the study groups. During literature review, we found no previous report of more complications associated with out-patient septoplasties compared with in-patient ones.
To control for the possible influence of variant nasal packing on our current results, we seperated the patients according to the nasal packing materials (Merocel or Nasopore), and the analysis between in-patient and out-patient showed similar results as previously mentioned. Consistently, a review of the literature also indicated no difference in post-operative complications from the use of different packing materials15,16.
For medical resources consumption, our present analysis has revealed that the out-patient approach is less costly and places a lower demand on medical resources. We calculated that the total surgical expenses for the out-patient group were about one-third lower than the in-patient cases. Previous studies in other countries also showed that the shift from in-patient to out-patient procedure in performing the same surgery equates to an overall savings of 41–50% to the provider, which is consistent with our current findings7,8,17.
It is noteworthy that the guidelines for day-case surgery from the Royal College of Surgeons in the UK indicate that the unexpected admission rate should be less than 3%6. In our present study series, only one of the patients scheduled for an ambulatory procedure asked to be admitted immediately after the surgery due to anxiety and discomfort. This led to an unexpected admission rate of 2.0% (1/48), which is thus within the aforementioned guidelines. Other than this patient (unexpected change of mind on admission), we did not have any re-admission after surgery in our patient group.
Our study does have some limitations. First, owing to the retrospective nature of our present analyses, the study patients were not randomly allocated into the in-patient and out-patient groups. The patients’ preferences, general condition, or other personal factors (e.g., socioeconomic status, occupation, and insurance) that can impact the decisions regarding hospital admission may have impacted on our current findings. Second, the severities of nasal septal deviation and turbinate hypertrophy varied between patients. Despite our efforts to standardize the surgical procedures and post-operative regimens, the individual differences could still affect the prognosis and post-operative complications. Third, we didn’t have an objective measurement for post-operative nasal airway patency e.g., acoustic rhinometry or rhinomanometry. Therefore, we took “the duration of nasal decongestant use” as the prognosis indicator instead.
Conclusions
Our current study findings indicate that septoplasty with inferior turbinectomy is a good candidate for an out-patient procedure not only for the cost-effectiveness but also for the surgical quality and safety, as evidenced by the comparable prognostic indicators and post-operative complications between the in-patient and out-patient approaches.
Data Availability
The datasets generated and analyzed during the current study are not publicly available due to hospital policy but are available from the corresponding author on reasonable request.
References
Gray, L. P. Deviated nasal septum: incidence and etiology. Ann Otol Rhinol Laryngol. 87, 3–20 (1978).
Mladina, R., Cujic, E., Subaric, M. & Vukovic, K. Nasal septal deformities in ear, nose and throat patients: an international study. Am J Otolaryngol. 29, 75–82 (2008).
Brown, P. M., Fowler, S., Ryan, R. & Rivron, R. ENT day surgery in England and Wales-an audit by the Royal College of Surgeons (Eng.) Comparative Audit Service. J Laryngol Otol. 112, 161–165 (1998).
Singarelli, S., Berni, A., Coppo, G. & Fracchia, P. Day-surgery, one-day surgery: the experience of an ENT Unit in a 250 bed hospital. Acta Otorhinolaryngol Ital. 25, 365–369 (2005).
Menezes, A. S., Guimarães, J. R., Breda, M., Vieira, V. & Dias, L. Septal and turbinate surgery: is overnight essential? Eur Arch Otorhinolaryngol. 275, 131–138 (2018).
Commission on the Provision of Surgical Services. Guidelines for Day Case Surgery. A Report of the Royal College of Surgeons of England, revised edition. Royal College of Surgeons of England (London, 1992).
Hogg, R. P., Prior, M. J. & Johnson, A. P. Admission rates, early readmission rates and patient acceptability of 142 cases of day case septoplasty. Clin Otolaryngol Allied Sci. 24, 213–215 (1999).
Benson-Mitchell, R., Kenyon, G. & Gatland, D. Septoplasty as a day-case procedure – a two centre study. J Laryngol Otol. 110, 129–131 (1996).
Nieminen, P., Silvola, J., Aust, R. & Stenfors, L. E. Nasal septal surgery as an out-patient procedure. J Laryngol Otol. 111, 1034–1037 (1997).
Srinivasan, V., Arasaratnam, R. B. & Jankelowitz, G. A. Day-case septal surgery under general anaesthesia and local anaesthesia with sedation. J Laryngol Otol. 109, 614–617 (1995).
Agha, R., Heaton, S. R. & Roberts, D. Patient satisfaction with day-case septoplasty and septorhinoplasty. J One-Day Surg. 14, 22–25 (2004).
Georgalas, C., Paun, S., Zainal, A., Patel, N. N. & Mochloulis, G. Assessing day-case septorhinoplasty: prospective audit study using patient-based indices. J Laryngol Otol. 116, 707–710 (2002).
Georgalas, C., Obholzer, R., Martinez-Devesa, P. & Sandhu, G. Day-case septoplasty and unexpected re-admissions at a dedicated day-case unit: a 4-year audit. Ann R Coll Surg Engl. 88, 202–206 (2006).
Philpott, C. M. & Banerjee, A. R. Is there a role for more day-case septal surgery? J Laryngol Otol. 119, 280–283 (2005).
Wormald, P. J., Boustred, R. N., Le, T., Hawke, L. & Sacks, R. A prospective single-blind randomized controlled study of use of hyaluronic acid nasal packs in patients after endoscopic sinus surgery. Am J Rhinol. 20, 7–10 (2006).
Weber, R., Hochapfel, F. & Draf, W. Packing and stents in endonasal surgery. Rhinology. 38, 49–62 (2000).
Buckley, J. G., Mitchell, D. B., Hickey, S. A. & Fitzgerald-O’Connor, A. Submucous resection of the nasal septum as an outpatient procedure. J Laryngol Otol. 105, 544–546 (1991).
Author information
Authors and Affiliations
Contributions
First author (Yung-Yuan Chen) did the data analysis and manuscript writing. Corresponding author (Tzu-Chin Huang) did the data collection and manuscript modification.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, YY., Huang, TC. Outcome of Septoplasty with Inferior Turbinectomy as an In-patient or Out-patient Procedure. Sci Rep 9, 7573 (2019). https://doi.org/10.1038/s41598-019-44107-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-44107-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.