Abstract
Septoplasty is one of the most common otolaryngological surgical procedures. The causes of persistent septal deviation after primary septoplasty vary. The purpose of this study was to identify factors associated with failure of primary septoplasty, operative techniques that correct residual septal deviation, and surgical outcomes. Seventy-four adults who underwent revision septoplasty to treat persistent septal deviations were enrolled. The level of hospital in which primary septoplasty was performed, type of septal deviation, septal portion exhibiting persistent deviation, and techniques used to correct the deviation were evaluated. Outcomes were measured subjectively using a visual analog scale (VAS), and objectively using acoustic rhinometry. The first septoplasties were usually performed in primary and secondary hospitals. C-shaped deviations were more common than S-shaped ones in both the anteroposterior and cephalocaudal dimensions. The most common region of persistent septal deviation was the caudal septum (44.6%), followed by multiple sites (20.3%). The corrective techniques included excision of the remnant deviated portion (70.3%), septal cartilage traction suturing (27.0%), spreader grafting (13.5%), and cross-suturing (6.8%). The VAS score improved significantly 6 months after surgery. The minimal cross-sectional area and nasal cavity volume of the convex side increased significantly after revision septoplasty. Patients who underwent septoplasty in primary and secondary hospitals were more likely to require revision septoplasty. The caudal septum was the most common site of persistent septal deviation. Careful preoperative evaluation of the caudal septal deviation and selection of an appropriate surgical technique may reduce the need for revision septoplasty.
Similar content being viewed by others
Introduction
Nasal obstruction is one of the most common symptoms encountered by otolaryngologists in general practice. Although the etiologies vary, a deviated nasal septum is the most common cause of unilateral nasal obstruction1; it can make breathing difficult and trigger frequent nosebleeds and repeated sinus infections, as well as headaches, snoring, sleep disturbances, and worsening sleep apnea2. Various septoplasty techniques have been used to deal with septal deviations at various sites. Septoplasty can be performed via an endonasal approach or open rhinoplasty.
Septoplasty is one of the most common otolaryngological surgical procedures3. However, over 15% of patients who undergo primary septoplasty experience no symptom relief1,4,5. Persistent nasal obstruction may be attributable to unrecognized nasal valve issues, inappropriate management of turbinate hypertrophy, exacerbation of allergic rhinitis, and residual or recurrent septal deviation. However, incomplete correction of septal deviation is the main cause of persistent septal deviation after primary septoplasty.
Here, we review the long-term outcomes of revision septoplasty in patients with persistent nasal obstruction after septoplasty. We aimed to identify factors affecting the failure of the primary septoplasty, and evaluated the surgical techniques used to correct residual septal deviation and the postoperative outcomes using subjective symptoms and acoustic rhinometric data.
Subjects and methods
Subjects
We retrospectively reviewed the medical records and endoscopic findings of 96 patients who underwent revision septoplasty at Pusan National University Hospital from March 2011 to February 2020. All patients were aged ≥ 18 years and underwent revision septoplasty because of clinically significant residual septal deviations despite prior septoplasty. The exclusion criteria included contemporaneous endoscopic sinus surgery (ESS), nasal valve surgery or nasal polypectomy, a history of facial trauma, a history or clinical evidence of allergic rhinitis, rhinosinusitis, atrophic rhinitis, septal perforation, bleeding or disorder/anticoagulant therapy, pregnancy, and any severe medical or neuropsychiatric disorder. This study protocol was approved by the Institutional Review Board of Pusan National University Hospital (H-2105-007-102) and performed in accordance with relevant guidelines and regulations. Informed consent was waived by the Institutional Review Board of Pusan National University Hospital (H-2105-007-102) due to retrospective nature of study.
Surgical procedure
All revision septoplasties were endoscopically performed under general anesthesia, using an endonasal approach or external rhinoplasty approach. The latter approach was used only when it was important to maximize visualization and access because of a need for particularly complex septal reconstruction. Various techniques were used to correct the residual septal deviations. Patients with turbinate hypertrophy underwent inferior turbinate out-fracture and volume reduction using a microdebrider. Silicone nasal splints were inserted and removed at 7 days postoperatively. Routine postoperative saline nasal irrigation and debridement were performed.
Data collection and outcome assessment
We obtained clinical data including age, gender, side of nasal obstruction, level of the hospital where primary septoplasty was performed, time between primary and revision septoplasty, surgical approach, use of combined procedures, techniques used to correct residual deviation, and any complications.
The septal deviation type and region of persistent septal deviation were defined using computed tomography (CT). Both S- and C-shaped deviations were divided into the anteroposterior and cephalocaudal dimensions (Fig. 1).
The locations of persistent septal deviation were classified as follows: caudal septum (caudal end of the cartilaginous septum), anterior septum (cartilaginous septum except the caudal septum), middle septum (septum around the cartilage/bone junction), posterior septum (bony septum), maxillary crest, and multiple sites (Fig. 2).
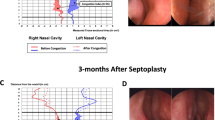
Each patient was evaluated preoperatively and at the 6-month follow-up. Subjective outcomes were measured using a visual analog scale (VAS). VAS scores ranged from 0 to 10 (0, no obstruction; 10, complete obstruction). Objective outcomes were evaluated by measuring the minimal cross-sectional area (MCA) and volume of both nasal cavities using acoustic rhinometry.
Statistical analysis
Data are presented as mean ± standard deviation. Statistical significance was determined using the paired t-test, performed with SPSS software (ver. 23.0; SPSS Inc., Chicago, IL, USA). A p-value ˂ 0.05 was considered to indicate statistical significance.
Results
Of 96 patients who underwent revision septoplasty, 19 (19.8%) were excluded because they underwent simultaneous ESS. Two patients had experienced prior septal perforations and one was excluded because of a nasal bone fracture; we finally analyzed seventy-four patients. The 66 (89.2%) males and 8 (10.8%) females ranged in age from 18 to 70 years (mean age = 37.5 years). Thirty-nine (52.7%) and thirty-five (47.3%) patients had unilateral and bilateral obstructions, respectively. The first septoplasty had been performed in primary (32/74, 43.2%), secondary (32/74, 43.2%), and tertiary (10/74, 13.6%) hospitals. The interval between primary and revision septoplasty was 11.30 ± 5.82 years (range: 1 ~ 39 years). Sixty-one patients (82.4%) underwent revision endonasal septoplasty and thirteen (17.6%) underwent septorhinoplasty using an external approach. Inferior turbinate out-fracture and turbinoplasty were combined in 45 patients (73.8%) who had undergone septoplasty and 5 who had undergone septorhinoplasty (38.5%). Only one patient developed a postoperative complication (septal perforation) during the 6-month follow-up. The patients’ characteristics are summarized in Table 1.
Anteroposterior C-shaped deviations were apparent in 59 patients (79.7%), and S-shaped deviations in 15 (20.3%). In the cephalocaudal dimensions, 65 patients (87.8%) had C-shaped deviations and 9 (12.2%) had S-shaped deviations. The most common location of persistent septal deviations was the caudal septum (44.6%), followed by multiple sites (20.3%), the anterior septum (14.9%), the middle septum (12.1%), the posterior septum (6.8%), and the maxillary crest (1.3%) (Table 2). The corrective techniques included excision of remnant deviated portions (70.3%), septal cartilage traction suturing (27.0%), spreader grafting (13.5%), and cross-suturing (6.8%) (Table 3).
The symptomatic VAS scores for nasal obstruction decreased significantly from 7.84 ± 1.92 to 2.70 ± 2.62 at 6 months postoperatively (p < 0.001). The mean MCA and nasal cavity volume of the convex sides increased significantly from 0.39 ± 0.24 cm2 and 5.38 ± 2.20 cm3 to 0.66 ± 0.19 cm2 and 8.04 ± 3.57 cm3 at 6 months post-surgery, respectively (p = 0.002 and p = 0.025, respectively). However, the mean MCA and nasal cavity volume of the concave side did not differ pre- and post-operatively (Table 4).
Discussion
Septoplasty is typically indicated when patients complain of unilateral or bilateral nasal obstruction attributable to structurally deviated cartilaginous or bony portions of the nasal septum. Although various surgical techniques are used to correct septal deviation, the success rates of primary septoplasty range from 43 to 85%1,5,7,8. The most common cause of septoplasty failure is residual or recurrent septal deviation attributable to inadequate correction of the deformity6. Revision septoplasty is safe for patients with ongoing nasal obstructions and persistent septal deviations after prior septoplasty. We found that patients who had undergone septoplasty in primary and secondary hospitals were more likely to require revision septoplasty than those initially treated in tertiary hospitals. The higher septoplasty failure rates in primary and secondary hospitals may reflect incomplete correction because of a lack of surgical skill or concerns about cosmetic complications such as tip ptosis and saddle nose deformity.
A few studies have explored the sites of persistent septal deviation after primary septoplasty. Gillman et al.1 reported that residual deviation was most common in the dorsal septum. However, Becker et al.4 found that multiple sites of deviation was most commonly encountered during revision surgery, followed by caudal deviation. Another study found that the middle septum was the most common site of persistent deviation, followed by the caudal septum6. In the present study, C-shaped deviations were more common than S-shaped ones in both the anteroposterior and cephalocaudal dimensions as revealed by CT. The most common regions of persistent septal deviation were the caudal septum, followed by multiple sites and the anterior and middle septum.
Caudal septal deviation is a deviation of the most anterior part of the nasal septum; it may cause severe nasal obstruction and significant cosmetic deformities of the nasal base9,10,11. A deviated caudal septum may change the relationship between the lobule and columella, thereby significantly affecting nasal tip position and symmetry10. Correction of such a deviation may be difficult; even a small residual deviation may cause severe nasal obstruction and the intrinsic cartilage-bending memory is hard to break11. Furthermore, weakening of the caudal septum and separation thereof from the anterior nasal spine can lead to overcorrection, saddle nose deformity, and tip ptosis12. Although various techniques have been used to manage caudal septal deviations, this region, along with high septal deviation, is one of the most difficult to surgically correct.
Surgical approaches to revision septoplasty include endonasal and open rhinoplasty. Many techniques (e.g., the “swinging door” method, septal batten or spreader grafting, cutting and suturing, and extracorporeal septoplasty) have been used to correct residual septal deviations, depending on the characteristics thereof and surgeon preferences6,13,14. In previous studies, the open approach was more common than the endonasal approach [4.6]. However, 61 (82.4%) and 13 (17.6%) of our patients underwent endonasal and open approaches, respectively. To correct remnant septal deviation, careful excision of residual deviated cartilaginous or bony portions is typically performed. Septal cartilage traction suturing (Seo et al.)15 was performed in 20 cases with a deviated caudal septum, and cross-suturing (Joo et al.)16 was performed in 5 cases. Spreader grafts were placed in 10 patients to correct deviations of the anterior septum that reached the dorsal septum; an open approach was employed. Revision septoplasty significantly improved subjective symptoms as measured by the VAS. Objective nasal obstruction improvements were measured by acoustic rhinometry. The MCA and nasal cavity volume of the convex side increased significantly 6 months after surgery. However, the MCA and nasal cavity volume of the concave side also increased, probably reflecting volume reduction of the inferior turbinate.
Although this study had the inherent limitations of a retrospective review, we believe that our prospectively collected, validated outcome measurements support the utility of revision septoplasty for patients with persistent nasal obstructions following primary septoplasty. Furthermore, remodeling may play an important role in shaping the final anatomical contour of the nasal septum due to the long interval between primary and revision surgery. Additional well-designed randomized controlled prospective studies are needed to confirm our findings.
Conclusion
Patients who underwent septoplasty in primary and secondary hospitals were more likely to require revision septoplasty than those seen in tertiary hospitals, typically because of incomplete correction of the caudal septal deviation. Careful evaluation of the caudal septal deviations and selection of appropriate primary surgery techniques may reduce the need for revision septoplasty.
Data availability
The datasets used and/or analysed during the current study are deidentified and included in this published article (and its Supplementary Information files).
References
Gillman, G. S., Egloff, A. M. & Rivera-Serrano, C. M. Revision septoplasty: a prospective disease-specific outcome study. Laryngoscope. 124, 1290–1295 (2014).
Teixeira, J., Certal, V., Chang, E. T. & Camacho, M. Nasal septal deviations: A systematic review of classification systems. Plast. Surg. Int. 2016, 1–8 (2016).
Manoukian, P. D., Wyatt, J. R., Leopold, D. A. & Bass, E. B. Recent trends in utilization of procedures in otolaryngolgy-head and neck surgery. Laryngoscope. 107, 472–477 (1997).
Becker, S. S., Dobratz, E. J., Stowell, N., Barker, D. & Park, S. S. Revision septoplasty: Review of sources of persistent nasal obstruction. Am. J. Rhinol. 22, 440–444 (2008).
Siegel, N. S., Gliklich, R. E., Taghizadeh, F. & Chang, Y. Outcomes of septoplasty. Otolaryngol. Head Neck Surg. 122, 228–232 (2000).
Jin, H. R., Kim, D. W. & Jung, H. J. Common sites, etiology, and solutions of persistent septal deviation in revision septoplasty. Clin. Exp. Otorhinolaryngol. 11, 288–292 (2018).
Illum, P. Septoplasty and compensatory inferior turbinate hypertrophy: long-term results after randomized turbinoplasty. Eur. Arch. Otorhinolaryngol. 254(Suppl 1), S89-92 (1997).
Fjermedal, O., Saunte, C. & Pedersen, S. Septoplasty and/or submucous resection? 5 years nasal septum operations. J. Laryngol. Otol. 102, 796–798 (1988).
Voizard, B., Theriault, M., Lazizi, S. & Moubayed, S. P. North American survey and systematic review on caudal septoplasty. J. Otolaryngol. Head Neck Surg. 49, 38 (2020).
Sedwick, J. D., Lopez, A. B., Gajewski, B. J. & Simons, R. L. Caudal septoplasty for treatment of septal deviation: aesthetic and functional correction of the nasal base. Arch. Facial Plast. Surg. 7, 158–162 (2005).
Jang, Y. J., Yeo, N. K. & Wang, J. H. Cutting and suture technique of the caudal septal cartilage for the management of caudal septal deviation. Arch. Otolaryngol. Head Neck Surg. 135, 1256–1260 (2009).
Kim, D. Y., Nam, S. H., Alharethy, S. E. & Jang, Y. J. Surgical outcomes of bony batten grafting to correct caudal septal deviation in septoplasty. JAMA Facial Plast. Surg. 19, 470–475 (2017).
Atespare, A. & Boyaci, Z. The use of spreader grafts in revision septoplasty. J. Craniofac. Surg. 27, 1656–1660 (2016).
Sillers, M. J., Cox, A. J. & Kulbersh, B. Revision septoplasty. Otolaryngol. Clin. North Am. 42, 261–278 (2009).
Seo, H. S. et al. Septal cartilage traction suture technique for correction of caudal septal deviation. Laryngoscope. 130, E758–E763 (2020).
Joo, Y. H., Cho, H. J., Jeon, Y. J. & Kim, S. W. Use of a crossing suture to correct caudal septal deviations. Int. Forum Allergy Rhinol. 9(8), 939–943 (2016).
Author information
Authors and Affiliations
Contributions
D.-J.L.: Writing - original draft, Prepared figure 1-2 H.J.: Data curation, Investigation, Resources H.-N.K.: Data curation J.-H.P.: Methodology, Software S.-D.K.: Validation, Investigation K.-S.C.: Conceptualization, Project administration, Writing - review & editing, Supervision
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, DJ., Jo, H., Kwon, HN. et al. Causes and management of persistent septal deviation after septoplasty. Sci Rep 12, 19574 (2022). https://doi.org/10.1038/s41598-022-23772-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-23772-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.