Abstract
The few published studies on the relationship between Helicobacter pylori infection and metabolic homeostasis were relatively small and yielded inconsistent results. We examined the prevalence of metabolic syndrome in relation to H. pylori infection and its symptoms in a large and unselected population. Coded data from the computerised database of a large health maintenance organisation in Israel were accessed for 147,936 individuals 25–95 years of age who performed the urea breath test during 2002–2012. The classification of metabolic syndrome followed a modified definition of the international diabetes federation. Prevalences of H. pylori infection and metabolic syndrome were 52.0% and 11.4% respectively. H. pylori infected patients had increased likelihood of metabolic syndrome: adjusted odds ratio (aOR) 1.15 (95% confidence intervals (CI) 1.10–1.19), as did patients with gastric ulcer: aOR 1.15 (95% CI 1.03–1.28) vs patients without these conditions. Duodenal ulcer was associated with metabolic syndrome only in persons aged 25–34 years: aOR 1.59 (95% CI 1.19-2.13), but not in older persons (P = 0.001 for heterogeneity). In conclusion, the likelihood of metabolic syndrome appeared significantly increased in relation to H. pylori infection and gastric and duodenal ulcers. These findings suggest that H. pylori long-term gastric inflammation might play a role in metabolic homeostasis.
Similar content being viewed by others
Introduction
Metabolic syndrome is a cluster of metabolic factors that increase the risk for atherosclerotic cardiovascular disease and type 2 diabetes mellitus1. Metabolic syndrome consists of atherogenic dyslipidaemia, elevated blood pressure; and elevated fasting blood glucose levels2,3, which lead to a prothrombotic and pro-inflammatory state1.
It has been postulated that some infectious agents might play a role in the pathogenesis of metabolic syndrome, as they can induce persistent inflammation. Helicobacter pylori, a gram-negative bacterium, is of particular interest, given its ability to induce long-standing gastric inflammation4. H. pylori colonizes the human gastric mucosa and causes persistent inflammation, usually without causing apparent disease, but in some individuals H. pylori causes peptic ulcer disease and even adenocarcinoma of the stomach5,6. The pathogenesis of peptic disease and gastric cancer usually involves strong and persistent inflammatory response that does not clear the infection (reviewed in5).
H. pylori infection has been linked to health conditions in areas outside the stomach, collectively known as extragastric diseases7,8. H. pylori infection was reported to be associated with increased prevalence of the metabolic syndrome4,9,10,11,12. However, conflicting findings exist regarding such association12,13, its magnitude14 and specificity15. Namely, it is unclear whether the observed association is specific to H. pylori infection or is the result of exposure to infectious agents in general, such as Chlamydia pneumoniae, herpes simplex virus 1 and cytomegalovirus15.
The aims of the current study were to examine the prevalence of metabolic syndrome in relation to H. pylori infection, and to peptic ulcer disease, as a proxy for gastric inflammation. If H. pylori infection and gastric inflammation are important in the development of metabolic syndrome, a stronger association is expected in symptomatic H. pylori patients.
Results
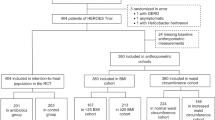
Data for 147,936 persons (60.7% females) who performed the urea breath test (UBT) and met the inclusion criteria were analysed. The age at UBT ranged from 25–95 years, with a mean of 42.8 years (standard deviation (SD) 12.7). H. pylori tested positive by UBT in 76,965 (52.0%; [95% CI 51.8–52.3]) persons.
Overall, 104,626 persons (70.7%) had information on at least one parameter of metabolic syndrome (in addition to body mass index [BMI]); this percentage was significantly higher in the older age groups, residents of low socioeconomic status towns and those who were born abroad compared to persons who were born in Israel(Supplementary Table S1). Accordingly, we conducted the weighted analysis; yielding a 11.4% weighted prevalence of metabolic syndrome.
Prevalence of metabolic syndrome according to socio-demographic factors
The prevalence of metabolic syndrome was higher in men than in women, it increased progressively with age (P for trend < 0.001), and decreased as residential economic rank increased (P for trend <0.001). Individuals who were born in Israel had lower prevalence of metabolic syndrome (9.7%) than those who were born in other countries (13.3–15.0%). Smokers and non-smokers had similar prevalence of metabolic syndrome (Table 1).
The prevalence of metabolic syndrome according to H. pylori infection, and gastric and duodenal ulcers
Overall, metabolic syndrome prevalence was slightly higher in H. pylori positive (by UBT) than negative persons (P < 0.001), but the difference was of greater magnitude in patients who had gastric and duodenal ulcers compared to those without a diagnosis code of these illnesses (Table 2). Adjusting for age resulted in strengthening the relationship of H. pylori with the metabolic syndrome, and attenuating the relationships of both gastric and duodenal ulcers with the metabolic syndrome.
Stratification by age groups showed higher prevalences of metabolic syndrome in people with H. pylori infection, gastric ulcer or duodenal ulcer compared to people without these conditions in most age groups (Table 3).
Pooled and age-stratified multivariable analyses were fitted. The pooled analyses showed that H. pylori infected persons had significantly increased likelihood of metabolic syndrome compared to uninfected patients; adjusted odds ratio (aOR) 1.15 [95% CI 1.10–1.19]). The strength of association between gastric ulcer and metabolic syndrome was weakened following adjustment for age, country of birth and residential economic rank (Table 4). Similarly, the relationship between duodenal ulcer and metabolic syndrome was of weaker magnitude after adjusting for the abovementioned sociodemographic factors. Positive adjusted associations (P < 0.05) remained in the age groups 25–34, 35–44 and 45–54 years, among whom H. pylori infected persons had 1.20 and 1.18 and 1.12-fold increased likelihood, respectively, to have metabolic syndrome. Persons aged 25–34 who had duodenal ulcer had 1.56 higher odds for metabolic syndrome than persons without duodenal ulcer, P = 0.001 for heterogeneity by age (Table 4). The adjusted association between gastric ulcer and metabolic syndrome remained significant in the pooled analysis (aOR 1.15 [95% CI 1.00-1.28]) of all age groups; the associations was stronger in the age group 35–44 (aOR 1.38 [95% CI 1.08–1.77]) and 55–64 (aOR 1.24 [95% 1.00–1.51]), respectively (Table 4), but the heterogeneity test was not significant.
Discussion
We examined the prevalence of metabolic syndrome in relation to H. pylori infection and peptic ulcers. Overall, H. pylori infected persons had higher prevalence of metabolic syndrome than uninfected ones. Similarly, a positive association was found between gastric ulcer and the metabolic syndrome. The strength of these associations was modest. The associations of duodenal ulcer was significantly modified by age, showing significantly 1.59-fold increased likelihood to have metabolic syndrome, in patients with versus without this condition, only in the age group 25–34 years. Collectively these findings suggest complex relationships between infection with H. pylori infection and the metabolic syndrome, as well as of gastric and duodenal ulcers with the metabolic syndrome. Sociodemographic confounders appear to explain such associations only partially, thus suggesting that H. pylori might have an independent and specific role in the metabolic syndrome.
A limited number of investigations have assessed the prevalence of the metabolic syndrome according to infection with H. pylori11,12,13,14,15,16,17,18. Mostly, they were conducted in East Asia11,12,14,16,17,18 and two studies were undertaken in Middle Eastern countries (Lebanon and Iran)13,15. Except for Naja et al.13, all the studies demonstrated significantly higher prevalence of the metabolic syndrome in persons infected with H. pylori compared to uninfected ones11,12,14,15,16,17,18. The sample size in these studies ranged from 308 to 7394 persons. They employed various detection techniques of H. pylori and various classification criteria for the metabolic syndrome. Most of these studies reported results from adjusted models. A recent meta-analysis combining results from these studies19 yielded a pooled OR of 1.34 (95% CI 1.17–1.53), with significant heterogeneity across the studies19. Our study provides the largest sample size to date, in which we used a uniform classification of both the exposure and outcome variables, as well as adjusted for possible confounders. The magnitude of the association in our study was modest with an aOR of 1.15 (95% CI 1.1–1.19). A similar association was found in relation to gastric ulcer, while duodenal ulcer showed a stronger association in the age group 25–34 years. These illnesses are caused by H. pylori through persistent gastric inflammation induced by the bacterium5. Our observations are in agreement with findings reported by Chen et al.17, who demonstrated significantly increased likelihood of the metabolic syndrome in persons positive versus negative for H. pylori IgG serum antibody in young adults, although the magnitude of association in our study is much smaller. Shin et al. have shown14 a stronger association between H. pylori infection with metabolic syndrome, if the infection status was determined based on histology, but they found no significant association when using serological assay. Collectively, these and our findings suggest that H. pylori infected persons had higher prevalence of metabolic syndrome than uninfected ones. The association between gastroduodenal disease and the metabolic syndrome might suggest that more severe gastric inflammation might be involved in metabolic imbalance. Indeed, it was shown that H. pylori infection, and eradication of the infection, can alter ghrelin and leptin levels20,21 (reviewed by Haj et al.4), two hormones expressed in the stomach and involved in metabolic homoeostasis22,23. Additionally, it is possible that the long-term gastric inflammation might enhance the pro-inflammatory state related to metabolic syndrome.
Given the cross-sectional study design, we cannot determine whether observed associations are causal; nonetheless, they are of public health importance, as H. pylori infection and peptic diseases might serve as markers to identify patients with increased likelihood for metabolic syndrome. The interaction between age and peptic ulcer might be due to poorer survival of old symptomatic H. pylori infected patients, compared to survivors who were included in the cohort.
Limitations of our study should be acknowledged. Electronic health and demographic data from a health maintenance organisation (HMO) database were utilized. These data accumulate as part of patients’ care; specifically, in our study, in regard to patients who were referred to UBT by their physicians. Thus, our sample represents patients with gastrointestinal symptoms. Data collection on variables such as BMI and smoking might be different in the various clinics across the country. Other than smoking, information was missing in low percentages for such confounders as country of birth, socioeconomic status and BMI. Importantly, the study database lacks information on waist circumference; a surrogate marker of central obesity, therefore, we used obesity (BMI ≥30 kg/m2) as a proxy for central obesity. The cutoffs of waist circumference of 102 cm and 88 cm for men and women, respectively, are associated with increased risk of cardiovascular diseases, and they were driven by correlation with BMI >30 (24, reviewed in25). BMI and waist circumference are strongly correlated with correlations coefficients ranging from 0.80 to 0.9526. Therefore, if misclassification of metabolic syndrome exists, because of using BMI ≥30 kg/m2 as a proxy for central obesity, it is expected to be non-differential, thus suggesting that our findings are conservative.
In addition, non-differential misclassification of gastric ulcer and duodenal ulcer might have occurred since the presence of these conditions was determined based on diagnostic codes in medical records. Diagnosis code of peptic ulcers disease showed a high positive predictive value of >90%27,28. Such misclassification might have led the measure of association towards the null hypothesis.
Strengths of our study include using UBT results to determine the presence of H. pylori infection. UBT is highly sensitive and specific for H. pylori identification compared to gold standard tests29. The study sample size was very large, which allowed identification of a relatively modest association between infection with H. pylori and metabolic syndrome prevalence, with effect modification by age. In addition, the definition of diabetes mellitus30 and hypertension31 relied on the same criteria throughout the study period. These definitions combine physicians’ diagnoses, results of blood biochemical analyses (e.g., fasting blood glucose and glycated haemoglobin in diabetes), buying medications to treat these conditions (antidiabetic and blood lowering agents), and several blood pressure measurements. Moreover, a standard definition was employed for the metabolic syndrome. Lastly, all laboratory tests were performed in one laboratory during the study period.
In conclusion, persons infected with H. pylori and those with peptic ulcer disease have significantly higher likelihood of the metabolic syndrome compared to persons without these conditions. These findings suggest that H. pylori long-term gastric inflammation might play a role in metabolic homeostasis.
Methods
Study design and population
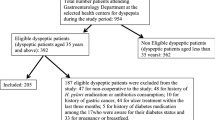
A prevalence study was undertaken employing health and demographic information obtained from the computerised database of Maccabi Health Services (MHS) HMO. MHS is ranked as the second largest HMO in Israel, insuring about two million people, i.e., about one-quarter of the population. The study cohort has been described in detail32. Briefly, we accessed deidentified information of persons aged 25 years or older who underwent UBT during 2002–2012. Persons with bariatric surgery and cancer diagnosis (within two years of the UBT) and documented purchase of anti-H. pylori therapy or proton pump inhibitors within one month of the UBT were excluded from the study.
Definitions of the study variables
Sociodemographic data were collected on patients’ age (grouped as 25–34, 35–44, 45–54, 65–95 years), sex, town of residence and country of birth (grouped as Israel, North Africa/Asia, Former Soviet Unions, Europe/Americas and other).
The definition of socioeconomic status relied on residential economic rank; i.e. of town of residence33. This aggregative index reflects certain features of a specific geographical area, including income, housing, cars (i.e. motorization level), education and employment33. Persons living in towns with residential economic ranks of 1–5 were categorised as living in low socioeconomic areas, and those living in towns with 6–7 and 8–10 socioeconomic ranks were categorised as living in intermediate and high socioeconomic areas, respectively.
Persons with a UBT result >3.5 per thousand were classified as infected with H. pylori, and those having lower UBT results were classified as negatives or uninfected. The international Classification of Disease codes-9th revision with clinical modifications (ICD-9) was employed to determine whether patients had gastric ulcer or duodenal ulcers.
Data were collected on smoking (categorised as never smoked, ever smokers, and smoking status unknown) and on BMI, which is calculated as weight in kilograms (kg)/height2 in meters (m)).
Laboratory results were obtained on triglycerides, high-density lipoproteins (HDL), and fasting plasma glucose levels. Data on purchasing statins and anti-diabetic medications was also retrieved. A modified classification of the International Diabetes Federation1,34 was employed to identify persons with metabolic syndrome. Obesity defined as BMI ≥30 kg/m2 was used as a proxy for central obesity given the lack of information on waist circumference. Obesity in addition to two or more of the following criteria defined metabolic syndrome: raised triglycerides (>150 mg/dL or statins use); low HDL levels (<40 mg/dL in men and <50 mg/dL in women), hypertension (defined based on MHS registry31); or raised plasma glucose levels (≥100 mg/dL or a diagnosis of diabetes based on MHS registry30).
Statistical analysis
Differences in sociodemographic factors between patients with and without information on at least one parameter of metabolic syndrome (beyond BMI) were examined using chi square test. Patients who had information on metabolic syndrome parameters differed significantly in sociodemographic variables compared to patients lacking such information (Supplementary Table 1), therefore we used inverse probability weighting method35, where the weights were assigned as the inverse probability obtained from multiple logistic regression model predicting having information on metabolic syndrome parameters.
Differences in the prevalence of the metabolic syndrome according to sociodemographic variables, H. pylori infection and its related gastroduodenal diseases were examined by chi square test. Age-adjusted associations between the infection and metabolic syndrome were examined using Cochran’s Mantel-Haenszel test.
Using Generalized Estimating Equations we examined adjusted relationships of H. pylori infection (determined as UBT result >3.5), gastric ulcer and duodenal ulcer with metabolic syndrome, while adjusting for sociodemographic factors. Adjusted ORs (and 95% confidence intervals [CIs]) were obtained from these models. Pooled and aged stratified analyses were performed. Heterogeneity across age groups was assessed using the chi square test for heterogeneity. The significance level was determined as two-sided P < 0.05. Analysis of data was performed using IBM-SPSS version 23 (IBM, Armonk, New York, USA) and Winpepi36.
Ethical consideration
Ethical approval was obtained from the institutional review board (IRB) (Helsinki committee) of Assuta Medical Centre and from the ethics committee of Tel Aviv University. An exempt from informed consent was granted due to the retrospective study design and the use of de-identified data (anonymized) from medical files. The study was conducted in accordance with the ethical guidelines of the Declaration of Helsinki.
Data availability statement
The data used in our study accumulated as part of patients’ care. These data were not collected for research purposes. The datasets cannot be made publicly available, and access to individual level data is not possible, since lawful and ethical limitations exist for secondary usage of these data in research.
References
Alberti, K. G., Zimmet, P. & Shaw, J. Metabolic syndrome–a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet. Med. 23, 469–480, https://doi.org/10.1111/j.1464-5491.2006.01858.x (2006).
Grundy, S. M. et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Curr. Opin. Cardiol. 21, 1–6 (2006).
Grundy, S. M. et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 112, 2735–2752, https://doi.org/10.1161/CIRCULATIONAHA.105.169404 (2005).
Haj, S., Raviv, M. & Muhsen, K. In Extradigestive Manifestations of Helicobacter pylori Infection - An Overview (ed Bruna Maria Roesler) Ch. 6, 141-164 (INTECH, 2016).
Atherton, J. C. The pathogenesis of Helicobacter pylori-induced gastro-duodenal diseases. Annu. Rev. Pathol. 1, 63–96, https://doi.org/10.1146/annurev.pathol.1.110304.100125 (2006).
Suerbaum, S. & Michetti, P. Helicobacter pylori infection. N. Engl. J. Med. 347, 1175-1186, https://doi.org/10.1056/NEJMra020542347/15/1175 (2002).
Roubaud Baudron, C., Franceschi, F., Salles, N. & Gasbarrini, A. Extragastric diseases and Helicobacter pylori. Helicobacter. 18(Suppl 1), 44–51, https://doi.org/10.1111/hel.12077 (2013).
Hudak, L., Jaraisy, A., Haj, S. & Muhsen, K. An updated systematic review and meta-analysis on the association between Helicobacter pylori infection and iron deficiency anemia. Helicobacter. 22, https://doi.org/10.1111/hel.12330 (2017).
Polyzos, S. A. & Kountouras, J. Novel advances in the association between Helicobacter pylori infection, metabolic syndrome, and related morbidity. Helicobacter. 20, 405–409, https://doi.org/10.1111/hel.12228 (2015).
Franceschi, F., Gasbarrini, A., Polyzos, S. A. & Kountouras, J. Extragastric Diseases and Helicobacter pylori. Helicobacter. 20(Suppl 1), 40–46, https://doi.org/10.1111/hel.12256 (2015).
Chen, T. P. et al. Helicobacter pylori infection is positively associated with metabolic syndrome in Taiwanese adults: a cross-sectional study. Helicobacter. 20, 184–191, https://doi.org/10.1111/hel.12190 (2015).
Gunji, T. et al. Helicobacter pylori infection is significantly associated with metabolic syndrome in the Japanese population. Am. J. Gastroenterol. 103, 3005–3010, https://doi.org/10.1111/j.1572-0241.2008.02151.x (2008).
Naja, F. et al. Association of H. pylori Infection with insulin resistance and metabolic syndrome among Lebanese adults. Helicobacter. 17, 444–451, https://doi.org/10.1111/j.1523-5378.2012.00970.x (2012).
Shin, D. W. et al. Association between metabolic syndrome and Helicobacter pylori infection diagnosed by histologic status and serological status. J. Clin. Gastroenterol. 46, 840–845, https://doi.org/10.1097/MCG.0b013e3182522477 (2012).
Nabipour, I., Vahdat, K., Jafari, S. M., Pazoki, R. & Sanjdideh, Z. The association of metabolic syndrome and Chlamydia pneumoniae, Helicobacter pylori, cytomegalovirus, and herpes simplex virus type 1: the Persian Gulf Healthy Heart Study. Cardiovasc. Diabetol. 5, 25, https://doi.org/10.1186/1475-2840-5-25 (2006).
Chen, L. W. et al. The associations between Helicobacter pylori infection, serum vitamin D, and metabolic syndrome: a community-based study. Medicine. 95, e3616, https://doi.org/10.1097/MD.0000000000003616 (2016).
Chen, L. W. et al. Helicobacter pylori infection increases insulin resistance and metabolic syndrome in residents younger than 50 years old: a community-based study. PloS One. 10, e0128671, https://doi.org/10.1371/journal.pone.0128671 (2015).
Yang, W. & Xuan, C. Influence of Helicobacter pylori Infection on Metabolic Syndrome in Old ChinesePeople. Gastroenterol. Res. Pract. 2016, 6951264, https://doi.org/10.1155/2016/6951264 (2016).
Upala, S., Jaruvongvanich, V., Riangwiwat, T., Jaruvongvanich, S. & Sanguankeo, A. Association between Helicobacter pylori infection and metabolic syndrome: a systematic review and meta-analysis. J. Dig. Dis. 17, 433–440, https://doi.org/10.1111/1751-2980.12367 (2016).
Roper, J. et al. Leptin and ghrelin in relation to Helicobacter pylori status in adult males. J. Clin. Endocrinol. Metab. 93, 2350–2357, https://doi.org/10.1210/jc.2007-2057 (2008).
Isomoto, H. et al. Impact of Helicobacter pylori infection on ghrelin and various neuroendocrine hormones in plasma. World J. Gastroenterol. 11, 1644–1648 (2005).
Kojima, M. et al. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 402, 656–660, https://doi.org/10.1038/45230 (1999).
Bado, A. et al. The stomach is a source of leptin. Nature. 394, 790–793 (1998).
Lean, M. E. J., Han, T. S. & Morrison, C. E. Waist circumference as a measure for indicating need for weight management. Brit. Med. J. 311, 158–161, https://doi.org/10.1136/bmj.311.6998.158 (1995).
Klein, S. et al. Waist circumference and cardiometabolic risk: a consensus statement from shaping America’s health: Association for Weight Management and Obesity Prevention; NAASO, The Obesity Society; the American Society for Nutrition; and the American Diabetes Association. Am. J. Clin. Nutr. 85, 1197–1202 (2007).
Ford, E. S., Mokdad, A. H. & Giles, W. H. Trends in waist circumference among US adults. Obes. Res. 11, 1223–1231, https://doi.org/10.1038/Oby.2003.168 (2003).
Viborg, S., Sogaard, K. K. & Jepsen, P. Positive predictive value of peptic ulcer diagnosis codes in the Danish National Patient Registry. Clin. Epidemiol. 9, 261–266, https://doi.org/10.2147/CLEP.S132628 (2017).
Margulis, A. V., Garcia Rodriguez, L. A. & Hernandez-Diaz, S. Positive predictive value of computerized medical records for uncomplicated and complicated upper gastrointestinal ulcer. Pharmacoepidemiol. Drug. Saf. 18, 900–909, https://doi.org/10.1002/pds.1787 (2009).
Ferwana, M. et al. Accuracy of urea breath test in Helicobacter pylori infection: meta-analysis. World J. Gastroenterol. 21, 1305–1314, https://doi.org/10.3748/wjg.v21.i4.1305 (2015).
Heymann, A. D. et al. The implementation of managed care for diabetes using medical informatics in a large Preferred Provider Organization. Diabetes Res. Clin. Pr. 71, 290–298, https://doi.org/10.1016/j.diabres.2005.07.002 (2006).
Weitzman, D., Chodick, G., Shalev, V., Grossman, C. & Grossman, E. Prevalence and factors associated with resistant hypertension in a large health maintenance organization in Israel. Hypertension. 64, 501–507, https://doi.org/10.1161/Hypertensionaha.114.03718 (2014).
Haj, S. et al. Associations of Helicobacter pylori infection and peptic disease with diabetic mellitus: Results from a large population-based study. PloS One. 12, e0183687, https://doi.org/10.1371/journal.pone.0183687 (2017).
Israel Central Bureau of Statistics. Characterization and classification of geagraphic units by the socio-economic level of the population 2008. Publication number 1530 (2013).
International Diabetes Federation. The IDF consensus worldwide definition of the metabolic syndrome (2006). Availabe from: https://www.idf.org/e-library/consensus-statements/60-idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html, Accessed date: August 4, (2017).
Seaman, S. R. & White, I. R. Review of inverse probability weighting for dealing with missing data. Statis. Meth. Med. Res. 22, 278–295, https://doi.org/10.1177/0962280210395740 (2013).
Abramson, J. H. Winpepi updated: computer programs for epidemiologists, and their teaching potential. Epidemiol. Perspec. Innov 8, 1, https://doi.org/10.1186/1742-5573-8-1 (2011).
Acknowledgements
This study was done in partial fulfilment of the requirements for a Master in Science (M.Sc.) degree of Rotem Refaeli, at the School of Public Health, Sackler Faculty of Medicine, Tel Aviv University. We are very grateful for the assistance received from Ms. Racheli Katz from Maccabi Health Services in data curation. This study was partially funded by the Council for Higher Education- Israel (KM-PI).
Author information
Authors and Affiliations
Contributions
K.M., G.C.h. and V.S. designed the research, R.R., S.H., G.C.h., S.G. and K.M. performed the research, R.R., S.H., G.C.h., S.G., V.S. and K.M. analysed the data. K.M. wrote the first draft of the manuscript. All authors reviewed the manuscript and contributed to finalizing the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Refaeli, R., Chodick, G., Haj, S. et al. Relationships of H. pylori infection and its related gastroduodenal morbidity with metabolic syndrome: a large cross-sectional study. Sci Rep 8, 4088 (2018). https://doi.org/10.1038/s41598-018-22198-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-22198-9
This article is cited by
-
Association of Helicobacter pylori infection with the risk of metabolic syndrome and insulin resistance: an updated systematic review and meta-analysis
Diabetology & Metabolic Syndrome (2021)
-
Differences in glycated hemoglobin levels and cholesterol levels in individuals with diabetes according to Helicobacter pylori infection
Scientific Reports (2021)
-
Helicobacter pylori infection as a risk factor for serum bilirubin change and less favourable lipid profiles: a hospital-based health examination survey
BMC Infectious Diseases (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.