Abstract
The objective of this study is to evaluate the effectiveness of different rivaroxaban dosage regimens in preventing ischemic stroke and systemic thromboembolism among Asians. A retrospective cohort study was conducted on data from nationwide insurance claims in Taiwan. Patients with non-valvular atrial fibrillation under warfarin or rivaroxaban therapy were included. Propensity score matching was used to balance the covariates, and Cox-proportional hazard models were applied to compare the effectiveness and safety of each treatment group. Rivaroxaban was associated with a significantly lower risk of venous thromboembolism (hazard ratio [HR]: 0.51; 95% confidence interval [CI]: 0.29–0.92, P = 0.02) and intracranial hemorrhage (HR: 0.48; 95% CI: 0.32–0.72, P < 0.001) than warfarin. Rivaroxaban 20 mg and 15 mg were associated with a significantly lower risk of ischemic stroke (20 mg, HR: 0.48; CI: 0.29–0.80, P = 0.005; 15 mg, HR: 0.69; CI: 0.53–0.90, P = 0.005), but rivaroxaban 10 mg was not. In the subgroup analysis of patients older than 65 years, the results were generally the same, except that rivaroxaban had a significantly lower risk of ischemic stroke than warfarin.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF), the most common type of arrhythmia, increases the risk of ischemic stroke and systemic thromboembolism five-fold and contributes to 15% of all ischemic stroke cases1,2. Appropriate anticoagulation therapy can effectively lower the risk of thromboembolism3. For decades, vitamin K antagonists were the only option of oral anticoagulant treatment. However, the narrow therapeutic index and multiple drug-drug and drug-food interactions of warfarin complicate its use4. The launch of non-vitamin K antagonist oral anticoagulants (NOACs) is a landmark in preventing ischemic stroke among AF patients. Rivaroxaban, a factor Xa inhibitor, has been shown to be associated with a comparable risk of ischemic stroke and systemic thromboembolism and a lower risk of intracranial hemorrhage (ICH) than warfarin5.
Even though the efficacy and safety of rivaroxaban have been proven, data for the Asian population is inadequate, especially for different dose levels. According to the Rivaroxaban Once Daily Oral Direct Factor Xa Inhibition Compared with Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation for Japanese (J-ROCKET AF) study, rivaroxaban 15 mg was as effective as warfarin in preventing ischemic stroke and systemic thromboembolism6. On the other hand, the subgroup analysis of the East Asian population in the global ROCKET AF study which used rivaroxaban 20 mg did not show any difference in efficacy and safety7. Therefore, the optimal regimen of rivaroxaban therapy for Asians is still under discussion.
In addition to trials, several observational studies have investigated the effectiveness and safety of NOACs in clinical use among non-valvular AF patients8,9,10, but to our knowledge, the real-world data for rivaroxaban, with a specific focus on different dosages, are sparse. This issue is particularly important because Asians have several demographic characteristics that differ from other ethnic groups. For example, Asians have a lower prevalence of AF but carry a specific increased risk of ischemic stroke, are more sensitive to warfarin, and more prone to suffer from warfarin-related bleeding. All these characteristics may lead to a change in the effectiveness and safety profile of anticoagulant therapy7,11,12,13,14,15,16,17. Thus, we aimed to conduct a nationwide, population-based study by using the National Health Insurance (NHI) claims database in Taiwan to investigate the effectiveness and safety of rivaroxaban at different dose levels in real-world practice, with a specific focus on different dosing regimens.
Methods
Data source
This study was conducted using claims data from the NHI program that includes more than 23 million enrollees, about 99.9% of the population in Taiwan. Comprehensive information about outpatients, inpatients, prescriptions, and insurance enrolment is included in the claims database. Data from between 2010 and 2015 were used for this study. The Research Ethics Committee of National Taiwan University Hospital approved the study.
Study Design and Patients
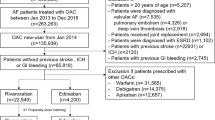
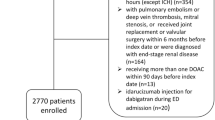
This was a retrospective cohort study with a new-user design. Patients who were at least 20 years old; had at least 1 inpatient or 2 separate outpatient diagnoses of AF, identified according to the International Classification of Diseases, Ninth Revision, and Clinical Modification (ICD-9-CM) code 427.31; and were prescribed rivaroxaban or warfarin from June 1, 2012 to December 31, 2015, fulfilled the inclusion criteria. Patients were excluded if they had a prosthetic heart valve or mitral valve disease during the study period18, were pregnant, diagnosed with cancer, or under chronic dialysis within 12 months prior to the index date. The index date was defined as the date of the first anticoagulant prescription observed on or after June 1, 2012, the date that rivaroxaban treatment began to be reimbursed in the NHI program. Chronic dialysis was defined as 1) having at least two separate outpatient procedure codes indicating dialysis treatment was undergone for more than 90 days, or 2) being enrolled in the “registry for patients with catastrophic illness” of the NHI program because of chronic renal dialysis19,20.
Two study groups were obtained in our study, rivaroxaban users and warfarin users. Only patients newly prescribed with rivaroxaban or warfarin were included for analysis. Patients were considered as newly on the study drugs if they did not receive any prescriptions for the study drugs for at least 12 months before the index date. A rivaroxaban user was determined by the very first rivaroxaban prescription after June 1, 2012. Warfarin users were those who received a warfarin prescription from June 1, 2012, to December 31, 2015, without receiving a prescription for NOAC during the study period.
Outcome Measures
Clinical effectiveness and safety were assessed separately in the follow-up period. Effectiveness was defined as the occurrence of ischemic stroke, venous thromboembolism (VTE), or transient ischemic attack (TIA). Safety was defined as the occurrence of ICH, gastrointestinal (GI) bleeding, or other bleeding. Primary diagnoses during hospitalization were applied for the assessment of the study outcomes. Since patients diagnosed with TIA may not require hospitalization, the primary diagnoses during emergency room visits were also included to detect TIA. Other bleeding was defined as patients that visited the emergency room or required hospitalization due to hemoptysis, epistaxis, hematuria, hemarthrosis, or hemopericardium. We identified ischemic stroke by ICD-9-CM codes (ICD-9-CM: 433, 434), which were validated by health insurance data in Taiwan21.
Patients were followed from the index date to whichever of the following events came first: 1) occurrence of the outcome of interest, 2) switching to an alternative oral anticoagulant, 3) discontinuation of the index anticoagulant, or 4) the end of the observation period (December 31, 2015). Medication discontinuation was defined as either discontinuing oral anticoagulation therapy or having a > 30-day gap between the end of an oral anticoagulant prescription and the next prescription22,23.
Baseline Characteristics and Covariates
The covariates adjusted were those factors known to affect anticoagulant treatment and study outcomes, including age, gender, annual stroke risk, specific comorbidities, and concomitant medications24,25,26. Comorbidities were identified by diagnoses made within 12 months before the index date, the date when the first anticoagulant was prescribed. Concomitant medications were identified by at least one prescription within 90 days preceding the index date24,25.
The baseline risk of ischemic stroke was assessed by using the CHA2DS2-VASc scoring system. The calculated score was categorized into low risk (0 points), moderate risk (1 point), and high risk (≥2 points). In contrast, the baseline bleeding risk was assessed by using the HAS-BLED scoring system.
Statistical Analysis
One-to-one propensity score matching using a greedy matching algorithm was applied to balance the covariates between the comparison groups. Absolute standardized mean differences were applied to compare the between-group balance of the baseline characteristics. An absolute standardized difference of less than 0.1 was recognized as indicating no significant difference. Cox-proportional hazard models were applied to determine the relationship between anticoagulant treatment and the study outcomes. The effectiveness and safety of rivaroxaban were first compared to warfarin in the main analysis. Subgroup analyses were performed in different dosage groups (e.g., rivaroxaban 10 mg, 15 mg, and 20 mg), and age groups (e.g., ≥65 years and ≥80 years). Two-sided tests with an α < 0.05 were defined as statistically significant. All statistical analyses were performed with SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA).
Data availability
The data that support the findings of this study are available from the Health and Welfare Data Science Center, Ministry of Health and Welfare in Taiwan; however, restrictions apply to the availability of the data, which were used under license for the current study and so are not publicly available. Data are available from the authors upon reasonable request and with permission from the Health and Welfare Data Science Center, Ministry of Health and Welfare in Taiwan.
Results
A total of 24,101 patients were enrolled in this study, of which 10,609 (44%) were rivaroxaban users and 13,942 were warfarin users. Before the propensity score matching, patients in the rivaroxaban group were older; had higher CHA2DS2-VASc scores; and had higher rates of VTE, hypertension, and concomitant use of antiplatelet drugs and statins. The demographics and the clinical characteristics of the study groups were all balanced after propensity score matching was performed (Table 1).
After propensity score matching, the final sample contained a total of 9,637 rivaroxaban-warfarin matched pairs. The average follow-up duration was 0.96 years for the rivaroxaban group and 1.18 years for the warfarin group. The observed event rates and the hazard ratios (HRs) of the rivaroxaban and warfarin groups after propensity score matching are displayed in Table 2. Overall, rivaroxaban was associated with a significantly lower risk of composite effectiveness outcomes (HR: 0.79; 95% confidence interval [CI]: 0.66–0.94, P = 0.01) and safety outcomes (HR 0.83; 95% CI: 0.71–0.97, P = 0.02) than warfarin. In detail, rivaroxaban was associated with a significantly lower risk of VTE (HR: 0.51; 95% CI: 0.29–0.92, P = 0.02) and ICH (HR: 0.48; 95% CI: 0.32–0.72, P < 0.001) and a comparable risk for ischemic stroke, TIA, GI bleeding, and other bleeding.
When we stratified our analysis by dose, we identified 1,509 pairs in the rivaroxaban 20 mg group, 5,996 pairs in the rivaroxaban 15 mg group, and 3,104 pairs in the rivaroxaban 10 mg group. The baseline characteristics of each group were all balanced after propensity score matching (Supplementary Tables S1 to S4). The adjusted HR among different doses of rivaroxaban and warfarin are displayed in Table 3. Use of rivaroxaban at doses of 20 mg and 15 mg was associated with a significantly lower risk of ischemic stroke (20 mg, HR: 0.48; 95% CI: 0.29–0.80, P = 0.005; 15 mg, HR: 0.69; 95% CI: 0.53–0.90, P = 0.005) and ICH (20 mg, HR: 0.24; 95% CI: 0.07–0.84, P = 0.03; 15 mg, HR: 0.36; 95% CI: 0.21–0.62, P < 0.001). Moreover, treatment with 20 mg rivaroxaban was associated with a lower risk of GI bleeding (HR: 0.47; 95% CI: 0.24–0.90, P = 0.02). In contrast, treatment with 10 mg rivaroxaban did not result in significant differences with regard to any of the effectiveness and safety outcomes. Figures 1 and 2 demonstrate the comparisons of effectiveness and safety outcomes between different doses of rivaroxaban.
The results of subgroup analyses among the elderly patients are displayed in Figs 3 and 4. The risk of ischemic stroke and ICH was significantly lower among rivaroxaban users versus warfarin users in the two age groups. The HR for ischemic stroke was 0.71 (95% CI: 0.56–0.89, P = 0.003) in patients aged ≥65 years and 0.65 (95% CI: 0.46–0.91, P = 0.01) in patients aged ≥80 years. The HR of ICH was 0.45 (95% CI: 0.29–0.69, P = <0.001) and 0.41 (95% CI: 0.21–0.83, P = 0.01) in the group of patients aged ≥65 years and ≥80 years, respectively. Notably, rivaroxaban was associated with a significantly lower risk of VTE (HR: 0.51; 95% CI: 0.28–0.93, P = 0.03) only among users aged ≥65 years.
Discussion
To the best of our knowledge, this is the first population-based observational study, which focuses specifically on Asians to assess the effectiveness and safety of rivaroxaban at different dosage regimens. In the present study, we observed a significantly lower risk of VTE and ICH for rivaroxaban compared to warfarin. Furthermore, rivaroxaban at a dose ≥15 mg was associated with a significantly lower risk of ischemic stroke. The risk of GI bleeding was generally comparable between rivaroxaban and warfarin users across all different dosage and age groups, except for the rivaroxaban 20 mg group, which showed a significantly lower risk of GI bleeding than the warfarin group.
Before propensity score matching, patients in the rivaroxaban group were older, more commonly diagnosed with systemic thromboembolism and hypertension, and had higher CHA2DS2-VASc scores than the warfarin group. This can be attributed to the reimbursement criteria for the NOACs in the NHI program: patients need to be ≥75 years old, have a history of ischemic stroke, systemic thromboembolism, or congestive heart failure. For patients aged between 65 and 74 years, at least one diagnosis of diabetes, hypertension, or coronary artery disease is required. The majority of patients in this study were prescribed low dose rivaroxaban (15 mg and 10 mg). The reasons for this prescription pattern are multifocal. First, Asians, compared to non-Asians, are more liable to experience warfarin-related bleeding, even under lower intensity anticoagulant therapy27. Therefore, physicians tend to be more conservative in Taiwan. Second, patients under NOAC therapy in Taiwan were older than warfarin users due to the restrictions in the NHI program. Elderly patients were more prone to receive a renal adjusted dose, as the glomerular filtration rate reduces with age. Third, physicians may prescribe rivaroxaban according to the Japanese labelling6.
Regarding the effectiveness, we observed a dose-related response. As the rivaroxaban dose increased from 10 to 15 and 20 mg, the risk of ischemic stroke became significantly lower than for warfarin and the risk reduction was even more prominent for the 20 mg group. This suggests that in the Asian population, the standard dosing regimen (i.e., 20 mg daily) is potentially more appropriate and should be considered in patients with no concern of increased bleeding risk. In the ROCKET AF and J-ROCKET AF study, however, the risk of ischemic stroke was comparable between the rivaroxaban and warfarin groups. Patients in the present study had less baseline risk for thromboembolism as indicated by lower average CHADS2 scores (the present study, 2.64; J-ROCKET AF, 3.27; ROCKET AF, 3.2), which may explain the more prominent effectiveness of rivaroxaban in our data. We also observed a significantly lower risk of VTE in the rivaroxaban group. AF has been shown to increase the risk of future development of VTE28. The efficacy of rivaroxaban in secondary VTE prevention has been proven previously in a well-controlled study29. Our results imply that rivaroxaban treatment is effective in preventing VTE among AF patients; however, further prospective studies that exclusively enrol AF patients may be warranted.
Regarding safety as reported in the ROCKET AF study, we observed a significantly lower risk of ICH and a comparable risk of GI bleeding in patients treated with rivaroxaban. In addition, our data showed that 20 mg was paradoxically associated with a reduced risk of GI bleeding. In contrast, rivaroxaban 10 mg did not significantly reduce the risk of ICH. These results may be explained by the between-group variation. In the present study, physicians determined the dosage regimen based on their judgment in the clinical setting. Therefore, patients in the rivaroxaban 20 mg group tended to be more robust, have a lower risk of bleeding as indicated by lower HAS-BLED scores, and experienced fewer GI bleeding episodes. On the other hand, patients in the rivaroxaban 10 mg group were more fragile, as indicated by older age, a higher prevalence of renal dysfunction, hypertension, and higher CHA2DS2-VASc and HAS-BLED scores, which led to a less prominent reduction in the risk for ICH.
The results of the subgroup analysis for the elderly patients were consistent with the main analysis. Rivaroxaban was associated with a lower risk of VTE and ICH than warfarin. The prominent risk reduction associated with rivaroxaban in ischemic stroke did not change in the elderly population. Elderly patients generally have a higher risk of ischemic stroke, systemic thromboembolism, and bleeding, and a higher prevalence of comorbidities and polypharmacy, but lower mobility for frequent laboratory monitoring30,31. Our results also indicated that even in patients of advanced age (i.e., age ≥80), rivaroxaban use remains effective and safe. Rivaroxaban may be an alternative to warfarin given its superior effectiveness profile and lower risk of ICH for both elderly (i.e., age ≥65) and very elderly (i.e., age ≥80) patients.
We acknowledge the following limitations in our study. First, laboratory results were not available in the claims data from the NHI program; therefore, we were unable to evaluate the proportion of time spent in the therapeutic international normalized ratio (INR) range (i.e., time in therapeutic range, TTR). Sub-optimal TTR in the warfarin group can lead to an over-estimation of the effectiveness of rivaroxaban. However, we censored the patients who discontinued oral anticoagulation therapy or had a > 30-day gap between the end of an oral anticoagulant prescription and the next prescription to ensure persistent use of oral anticoagulants. We assumed that the persistent use of warfarin would reflect a minimum level of anticoagulant use and therefore ensured a certain level of time in therapeutic range in warfarin users. Second, we did not directly compare the outcomes across different rivaroxaban dose groups. The dose relationship was a result of an indirect comparison and thus can potentially suffer from selection bias due to the different baseline characteristics of the three dose groups. Given that the paradoxical relationship between rivaroxaban dose and the risk of ICH, we suspected that unmeasured variables may possibly exist. Therefore, some biases may still remain in the results in spite of propensity score matching. Third, we were unable to evaluate the adherence. Nevertheless, patients who did not refill their medications for more than 30 days were censored from this study. With an uncertain status of adherence, our data still showed improved effectiveness and an improved safety profile with rivaroxaban. Finally, only baseline demographics within 12 months before the index date were included for propensity score matching. Medical conditions that occurred more than one year prior to the index date were not taken into consideration, which may have resulted in an underestimation of the baseline risk for thrombosis and bleeding. Nevertheless, previous studies have applied the 12 month period to validate the CHA2DS2-VASc scoring system32, and the same approach has also been used in several observational studies investigating the effectiveness and safety of NOACs10,23,33. Comorbidities, such as heart failure, hypertension, and diabetes mellitus, were considered as chronic diseases and would be detected by claims data as long as patients re-visited their physician and refilled medications. Since patients with chronic conditions generally need long-term management, it is most likely that these patients will continuously use health services and thus be recorded in the claims database. Therefore, we should be able to identify the pre-existing conditions correctly even if the conditions were first diagnosed outside the one-year per-index period.
In conclusion, rivaroxaban was associated with a lower risk of VTE and ICH than warfarin in patients with non-valvular AF. At doses over 15 mg, rivaroxaban was associated with a significantly lower risk of ischemic stroke. Our study supports rivaroxaban as an effective and safe choice even among the elderly population.
References
Wolf, P. A., Abbott, R. D. & Kannel, W. B. Atrial fibrillation: a major contributor to stroke in the elderly. The Framingham Study. Arch. Intern. Med. 147, 1561–1564 (1987).
Kannel, W. B., Wolf, P. A., Benjamin, E. J. & Levy, D. Prevalence, incidence, prognosis, and predisposing conditions for atrial fibrillation: population-based estimates. Am. J. Cardiol. 82, 2n–9n (1998).
January, C. T. et al. AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation 130, 2071–2104 (2014).
Ansell, J. et al. Pharmacology and management of the vitamin K antagonists: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest 133, 160s–198s (2008).
Patel, M. R. et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N. Engl. J. Med. 365, 883–891 (2011).
Hori, M. et al. Rivaroxaban vs. warfarin in Japanese patients with atrial fibrillation - the J-ROCKET AF study. Circ. J. 76, 2104–2111 (2012).
Wong, K. S. et al. Rivaroxaban for stroke prevention in East Asian patients from the ROCKET AF trial. Stroke 45, 1739–1747 (2014).
Chan, P. H. et al. Stroke prevention using dabigatran in elderly Chinese patients with atrial fibrillation. Heart Rhythm 13, 366–373 (2016).
Gorst-Rasmussen, A., Lip, G. Y. & Bjerregaard Larsen, T. Rivaroxaban versus warfarin and dabigatran in atrial fibrillation: comparative effectiveness and safety in Danish routine care. Pharmacoepidemiol. Drug Saf. https://doi.org/10.1002/pds.4034 (2016 [Epub ahead of print]).
Lauffenburger, J. C. et al. Effectiveness and safety of dabigatran and warfarin in real-world US patients with non-valvular atrial fibrillation: a retrospective cohort study. J. Am. Heart Assoc. 4 https://doi.org/10.1161/JAHA.115.001798 (2015).
Yuen, E., Gueorguieva, I., Wise, S., Soon, D. & Aarons, L. Ethnic differences in the population pharmacokinetics and pharmacodynamics of warfarin. J. Pharmacokinet. Pharmacodyn. 37, 3–24 (2010).
Hori, M. et al. Dabigatran versus warfarin: effects on ischemic and hemorrhagic strokes and bleeding in Asians and non-Asians with atrial fibrillation. Stroke 44, 1891–1896 (2013).
Gillott, R. G., Willan, K., Kain, K., Sivananthan, U. M. & Tayebjee, M. H. South Asian ethnicity is associated with a lower prevalence of atrial fibrillation despite greater prevalence of established risk factors: a population-based study in Bradford Metropolitan District. Europace 19, 356–363 (2017).
Chao, T. F. et al. Using the CHA2DS2-VASc score for refining stroke risk stratification in ‘low-risk’ Asian patients with atrial fibrillation. J. Am. Coll. Cardiol. 64, 1658–1665 (2014).
Chao, T. F. et al. Age Threshold for Increased Stroke Risk Among Patients With Atrial Fibrillation: A Nationwide Cohort Study From Taiwan. J. Am. Coll. Cardiol. 66, 1339–1347 (2015).
Chao, T. F. et al. Should atrial fibrillation patients with 1 additional risk factor of the CHA2DS2-VASc score (beyond sex) receive oral anticoagulation? J. Am. Coll. Cardiol. 65, 635–642 (2015).
Shen, A. Y. et al. Racial/Ethnic differences in ischemic stroke rates and the efficacy of warfarin among patients with atrial fibrillation. Stroke 39, 2736–2743 (2008).
Fauchier, L. et al. How to define valvular atrial fibrillation? Arch. Cardiovasc. Dis. 108, 530–539 (2015).
Chao, P. W. et al. Acute appendicitis in patients with end-stage renal disease. J. Gastrointest. Surg. 16, 1940–1946 (2012).
Komenda, P. et al. Secular trends in end-stage renal disease requiring dialysis in Manitoba, Canada: a population-based study. CMAJ open 3, E8–E14 (2015).
Cheng, C. L., Kao, Y. H., Lin, S. J., Lee, C. H. & Lai, M. L. Validation of the National Health Insurance Research Database with ischemic stroke cases in Taiwan. Pharmacoepidemiol. Drug Saf. 20, 236–242 (2011).
Go, A. S. et al. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA 290, 2685–2692 (2003).
Villines, T. C. et al. A comparison of the safety and effectiveness of dabigatran and warfarin in non-valvular atrial fibrillation patients in a large healthcare system. Thromb. Haemost. 114, 1290–1298 (2015).
Lauffenburger, J. C. et al. Factors driving anticoagulant selection in patients with atrial fibrillation in the United States. Am. J. Cardiol. 115, 1095–1101 (2015).
AbuDagga, A. et al. Characteristics affecting oral anticoagulant therapy choice among patients with non-valvular atrial fibrillation: a retrospective claims analysis. BMC Health Serv. Res. 14, 310 (2014).
Singer, D. E. et al. Should patient characteristics influence target anticoagulation intensity for stroke prevention in nonvalvular atrial fibrillation?: the ATRIA study. Circ. Cardiovasc. Qual. Outcomes 2, 297–304 (2009).
Shen, A. Y. et al. Effect of race/ethnicity on the efficacy of warfarin: potential implications for prevention of stroke in patients with atrial fibrillation. CNS Drugs 22, 815–825 (2008).
Laliberte, F. et al. Real-world comparative effectiveness and safety of rivaroxaban and warfarin in nonvalvular atrial fibrillation patients. Curr. Med. Res. Opin. 30, 1317–1325 (2014).
Bauersachs, R. et al. Oral rivaroxaban for symptomatic venous thromboembolism. N. Engl. J. Med. 363, 2499–2510 (2010).
Halperin, J. L. et al. Efficacy and safety of rivaroxaban compared with warfarin among elderly patients with nonvalvular atrial fibrillation in the Rivaroxaban Once Daily, Oral, Direct Factor Xa Inhibition Compared With Vitamin K Antagonism for Prevention of Stroke and Embolism Trial in Atrial Fibrillation (ROCKET AF). Circulation 130, 138–146 (2014).
Lavan, A. H., Gallagher, P. F. & O’Mahony, D. Methods to reduce prescribing errors in elderly patients with multimorbidity. Clin Interv Aging 11, 857–866 (2016).
Lip, G. Y., Nieuwlaat, R., Pisters, R., Lane, D. A. & Crijns, H. J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest 137, 263–272 (2010).
Seeger, J. D. et al. Safety and effectiveness of dabigatran and warfarin in routine care of patients with atrial fibrillation. Thromb. Haemost. 114, 1277–1289 (2015).
Acknowledgements
This study was partially funded by a research grant from the Ministry of Science and Technology in Taiwan (MOST 104-2314-B-002-095). The funder had no role in the study design, data collection and analysis, interpretation of results, publication decisions, or manuscript preparation.
Author information
Authors and Affiliations
Contributions
Study concept and design: All Acquisition, analysis, or interpretation of data: All Drafting of the manuscript: Hsin-Yi Huang Critical revision of the manuscript for important intellectual content: Shin-Yi Lin, Shou-Hisa Cheng, and Chi-Chuan Wang. Statistical analysis: Hsin-Yi Huang Final approval: All Agreement for all aspects to be accountable: All.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, HY., Lin, SY., Cheng, SH. et al. Effectiveness and Safety of Different Rivaroxaban Dosage Regimens in Patients with Non-Valvular Atrial Fibrillation: A Nationwide, Population-Based Cohort Study. Sci Rep 8, 3451 (2018). https://doi.org/10.1038/s41598-018-21884-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-21884-y
This article is cited by
-
Reduced dose direct oral anticoagulants compared with warfarin with high time in therapeutic range in nonvalvular atrial fibrillation
Journal of Thrombosis and Thrombolysis (2023)
-
Cost-Effectiveness of Direct Non-Vitamin K Oral Anticoagulants Versus Vitamin K Antagonists for the Management of Patients with Non-Valvular Atrial Fibrillation Based on Available “Real-World” Evidence: The Italian National Health System Perspective
Clinical Drug Investigation (2021)
-
Safety and effectiveness of rivaroxaban and warfarin in moderate-to-advanced CKD: real world data
Journal of Nephrology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.