Abstract
Although several studies have investigated the associations of neck circumference (NC) with arterial blood pressures (BPs) and hypertension, no such studies have been conducted among Northern Chinese population. Between April and June 2015, a total of 2631 subjects aged ≥35 years old were recruited from Northeastern China. NC and arterial BPs were measured by trained personnel. Generalized linear and logistic regression analyses were applied to examine the associations of NC with arterial BPs and hypertension risk. The optimal cut-off points of NC for predicting hypertension were assessed by the receiver operating characteristic analysis. We found that NC was significantly associated with arterial BPs and hypertension risk in the Northeastern Chinese adults, even after adjusting for many covariates including body mass index, waist circumference or waist-to-hip ratio. The optimal cut-off values for NC to predict hypertension differed with sex, age, and body mass index. Our study suggests that NC may play an independent role in predicting hypertension beyond the classical anthropometric indices, and that it could be used as a valuable anthropometric measurement for routine assessment in primary care clinics and future epidemiological studies.
Similar content being viewed by others
Introduction
Hypertension is a leading risk factor for many disorders including coronary heart disease and stroke, and contributes to approximately 12.8% of annual deaths worldwide1. The causes of hypertension are complex and are correlated with numerous environmental and genetic factors. Among them, adiposity is a well-documented modifiable risk factor. Body mass index (BMI), waist circumference (WC) and waist-to-hip (WHR) are the most used anthropometric indices to reflect the total body adiposity or visceral adiposity, and to predict hypertension risk2,3,4. However, several recent studies reported that the regional deposition of fat, especially in the upper body segment, is more pathogenic than total body adiposity and visceral abdominal fat5, 6.
Neck circumference (NC), a simple, cheap, time-saving and practical anthropometric parameter, has been used as a surrogate measure for the upper body subcutaneous adipose tissue distribution. In the past decade, accumulating evidence showed that NC was independently associated with metabolic syndrome7, 8, obstructive sleep apnea syndrome8, and cardiovascular diseases9,10,11,12,13,14. However, only a few studies have investigated the relationships of NC with arterial blood pressures (BPs) and hypertension9, 12, 14, and the results were often inconsistent. In a systematic literature review, we found 3 human epidemiological studies on NC and arterial BPs or hypertension in Chinese population. Specifically, Zhou et al. investigated the relationships of NC with cardio-metabolic syndrome risk in 4201 middle-aged Chinese southerners, and found that NC had significant associations with arterial BPs and hypertension12. Similarly, a more recent study conducted in 1943 Central Chinese reported that the positive predictive of NC for discriminating hypertension were 77.58% in males and 71.36% in females13. However, another study on 1709 adults from central China, showed that NC was not associated with systolic blood pressure (SBP) and the association with diastolic blood pressure (DBP) was very weak14.
In China, the distribution of hypertension and obesity prevalence rates show a large geographical imbalance and people living in north areas usually have higher prevalence of the two disorders than the southerners, presumably due to differences in environmental exposure, dietary patterns, life habits, and genetic backgrounds15,16,17. However, the 3 prior studies mentioned above were all performed in Southern and Central China, and, to the best of our knowledge, no such study had been performed in people living in northern China. In addition, several prior studies conducted in other countries have applied receiver operating characteristic (ROC) analysis to assess the accuracy of NC as diagnostic tests for hypertension18,19,20 and indicated that NC may be a valuable anthropometric parameter to predict hypertension risk. However, no study to date has explored the optimal cut-offs of NC in discriminating hypertension in Chinese adults.
Therefore, we conducted a large community-based cross-sectional study in Northeastern China to explore (1) the potential relationships of NC with arterial BPs and hypertension; (2) the optimal cut-points of NC for predicting hypertension risk.
Results
Participant characteristics
Figure 1 shows the sampling procedure of this study. A total of 2631 participants were included with a mean age of 59.78 ± 10.66 years. The demographic, clinical, lifestyle and anthropometric characteristics of the survey participants, overall and stratified by gender, are summarized in Table 1. The average NC was 35.40 ± 4.41 cm, and the overall prevalence of hypertension was 42.38%. Compared with females, males manifested significantly higher NC, BMI, WC, hip circumference (HC), WHR, SBP, DBP, triglycerides (TG), and lower total cholesterol (TC), low-density lipoprotein (LDL-C) and high-density lipoprotein (HDL-C) levels, and were more likely to be smokers, drinkers, and have higher education levels (all p < 0.05).
Relationships of NC with arterial BPs
Firstly, we performed univariate linear regression analysis to explore the associations of the conventional predisposing factors with arterial BPs. As shown in Table S1, the p values for age, gender, fasting blood glucose (FBG), salt consumption, family history of hypertension, smoking and drinking status, physical activity and history of hypertension were less than 0.2. Thus, these variables were included in the final multivariate regression model. Further, we made additional adjustments for BMI, WC and WHR one by one due to close collinearity between them. For all subjects, NC was significantly associated with increased SBP and DBP levels in all the 5 models. For females, after further adjustments for BMI (model 3) or WC (model 4), the effect sizes were attenuated but still significant. For males, NC was associated with SBP in all the 5 models. However, for DBP, its association with NC became insignificant after additional adjustments for BMI or WC (Table 2).
Relationship of NC with hypertension risk
We also performed univariate and multivariate logistic regression models to estimate the relationships of NC levels with hypertension risk (Table S2 and Table 3), and found that NC was significantly associated with hypertension risk in all the 5 models. Stratified analyses by gender also revealed a significant association in both males and females (All p < 0.05).
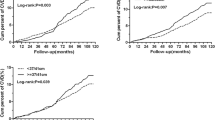
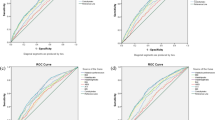
Subsequently, we used the areas under the ROC curves (AUCs) to evaluate the predictive values of NC for hypertension susceptibility (Table 4). The AUCs of NC were 0.577 and 0.583 for the risk of hypertension in females and males, respectively. NC of 32.75 cm for females and 35.75 cm for males were optimal cut-off points of combined sensitivity and specificity in identifying hypertension. Considering there are different NC levels in various age and BMI groups, we also assessed the optimal cut-offs of NC for hypertension by age groups and BMI categories. For age groups, ROC analysis showed that the AUCs for NC and hypertension was highest in 35–44 age group (0.619), and followed by 45–64 (0.584) and ≥65 age groups (0.573). The corresponding best cut-offs for determining hypertension was 38.50 cm, 32.25 cm and 34.25 cm, respectively. For BMI categories, the ROC cut-off values were observed at 31.55 cm (AUC: 0.559) for normal weight, 32.40 cm (AUC: 0.551) for overweight, and 33.30 cm (AUC: 33.30) for obesity.
Furthermore, we assessed the associations between NC categories based on cut-off values and the risk of hypertension by gender (Table 5). Therefore, NC < 32.75 cm and <35.75 cm were the references in females and males, respectively. The results showed that in models fully adjusted for all the covariates and BMI, WC or WHR (models 3, 4 and 5), NC was significantly correlated with hypertension risk in both females and males.
Discussion
In this study, we found that NC was associated with arterial BPs and hypertension risk in the Northeast urban Chinese adults, even after adjusting for many covariates including BMI, WC or WHR. In addition, we estimated the optimal cut-off value for NC to predict hypertension, and found that the values differed with gender, age and BMI.
NC with arterial BPs and hypertension
In recent years, a growing number of studies have been performed to estimate the associations of NC with arterial BPs and hypertension. For instance, in a longitudinal cohort study of 431 Israeli individuals, Ben-Noun et al. reported that NC was strongly associated with SBP and DBP levels21. In a cross-sectional study of 4201 Chinese adults, Zhou and colleagues found that NC had positive correlation with SBP, DBP and hypertension12. Additionally, Lee et al. compared the predictive power of anthropometric indices for hypertension in a Korean population, and found that NC was a valuable index in distinguishing hypertension and normotension19. Consistent with these prior findings, our current study found that NC was significantly associated with both arterial BPs and hypertension.
Due to the close link of NC with BMI and WC, several previous studies found that after further adjustments of BMI or WC, the associations of NC with arterial BPs and hypertension became insignificant9, 18. For example, in the Framingham Heart Study in 3307 participants, Preis et al. found that NC were related with SBP and DBP levels and hypertension risk in both males and females after adjusting for several potential covariates. However, after further adjustments for BMI, NC was positively related to DBP in males only9. Likewise, in a cross-sectional study of Caucasion population, Assyov et al. observed that NC was associated with hypertension in univariate analysis. However, when adjusted for WC and age, the association lost its statistical significance in females18. Contrary with these studies, our study showed that the significance of the associations of NC with arterial BPs and hypertension were not changed after additional adjustments for BMI or WC, although the magnitudes of the associations were slightly attenuated. The inconsistencies between those prior studies and ours may be caused by differences in genetic backgrounds, dietary habits, adjustment factors, and the effects of other confounding factors.
Optimal cut-off points of NC on hypertension risk
We further used the ROC analysis to determine the predictive validity of NC and evaluated optimal cut-off values for identifying hypertension, and found that a NC of more than 32.75 cm in females and 35.75 cm in males is suitable for assessing the likelihood of hypertension. In a systematic MEDLINE search, we found 4 relevant human epidemiological studies on the accuracy of NC as diagnostic test for hypertension. A study of 255 Caucasian adults found that the cut-off values of NC for the prediction of hypertension in females and males were 35 cm and 38 cm, respectively, which were relatively greater than those observed in our analysis18. Additionally, Zhou et al. reported that NC was a valuable index for discriminating hypertension in Chinese adults (AUCs were 0.635 and 0.659 for males and females, respectively)12, which further corroborated by the subsequent studies among Korean population (AUCs were 0.617 and 0.645 for males and females respectively)19 and American children (AUCs were 0.75 and 0.72 for boys and girls, respectively)20. In our study, the AUCs for males and females were 0.583 (95% CI = 0.546–0.621) and 0.577 (95% CI = 0.550–0.604), respectively, which were relatively lower than those observed in the previous studies. However, in the current study we observed that both the discriminative values in distinguishing hypertension were statistically significant (All p values < 0.001). Additionally, applying binary logistic regression analyses, we explored the association of NC with hypertension risk based on the calculated cut-off values of ROC analysis, and observed that participants with NC above cut-off values had an approximately 1.70-fold increased risk of hypertension than those with NC below cut-off values. In sum, although there exists heterogeneity in the diagnostic value of NC in discriminating hypertension among different populations, evidence from our and those previous studies consistently support that NC is a valuable index for discriminating hypertension.
Because of the links of age and BMI with NC, we further assessed the optima cut-offs of NC by age and BMI groups, and found that the cut-off values were relatively higher in the younger and those with higher BMI. To our knowledge, this is the first study to determine the age- and BMI-specific predictive validity of NC in identifying hypertension, thus it is difficult to directly compare our results with other findings. Future studies with large sample size and longitudinal design is needed to validate our findings.
Potential mechanisms
The precise mechanisms underlying the relationships of NC with arterial BPs and hypertension are not fully understood. Several investigators have proposed that upper-body subcutaneous fat might affect the arterial BPs and the development of hypertension via releasing large amounts of systemic free fatty acid, which may induce insulin resistance, vascular injury, provoke endothelia cell dysfunction, and increase oxidative stress and very-low-density lipoprotein cholesterol production22,23,24,25,26. Additionally, NC is an important predictor of obstructive sleep apnea syndrome. Obstructive sleep apnea syndrome can cause hypertension by increasing sympathetic activity, which influences vascular resistance and cardiac output27, as well as the potential for fluid retention28, 29. Thus, the association of NC with arterial BPs and hypertension may also be mediated by its relationship with the severity of sleep-disordered breathing.
Limitations and strengths
In interpreting the findings of the current study, three main limitations should be acknowledged. Firstly, the cross-sectional nature of the present study may limit the interpretation of causality of associations between NC and arterial BPs and hypertension. Secondly, self-reported information such as smoking and drinking status, and physical activity might have caused recall biases. In addition, we used questionnaire method to evaluate salt intake, which might have caused underestimation of actual salt intake30,31,32. Thirdly, NC is a proxy for upper-body subcutaneous fat, we did not perform radiographic measures to directly quantify the depot of fat. Despite these caveats, our study still has several advantages. First, to the best of our knowledge, it explored the associations of NC with arterial BPs and hypertension risk for the first time in the Northern Chinese adults, and reported the optimal sex-, age-, and BMI-specific NC cut-off points in the population. Second, all participants were of Han nationality and from the same district, which reduce the selective bias and improve the validity of statistical analysis.
Conclusion
In conclusion, this is the first study to explore the relationship between NC and BPs in Northern Chinese. Our findings suggest that NC may play an independent role in predicting hypertension beyond the classical anthropometric indices including WC, BMI, and WHR, and that the optimal cut-offs of NC for distinguishing hypertension differs with sex, age and BMI. The measurement of NC is inexpensive and easier to obtain, thus it could be used as an important measure to consider for routine assessment in primary care clinics and other health care settings as well as for large-scale epidemiological studies on obesity-related diseases. However, considering the limitations of our study, further large prospective population-based studies and mechanistic studies are still needed to validate our finding, and to explain how NC contributes to the elevated arterial BPs and the development of hypertension.
Methods
Study participants and inclusion criteria
The cross-sectional study was conducted in Shenhe district between April and June 2015. The district locates in the center of Shenyang city and consists of 14 blocks. A total of over one million people reside in this district, of whom 73.00% are registered residents. A 3-stage sampling method was applied to select participants in this study. In the first stage, we selected all the 14 blocks of the district, and from each of these, 8 communities were randomly identified. In the second stage, we selected 25 households from each of the residence community using systematic sampling. In the third stage, one participant, aged ≥35 years old and lived in the district for at least 2 years, was selected from each household without replacement. The sampling frame resulted in the selection of 2800 potential participants, of whom 2761 individuals agreed to participant in the investigation and filled out the questionnaire, yielding a response rate of 98.61%. All of the participants are registered residents of the district. Inclusion criteria included: (1) without thyroid diseases, neck masses and deformity, malignant diseases, and secondary hypertension; (2) without pregnancy, lactation and weight control; (3) Han nationality. Finally, a total of 2631 individuals met these criteria and were included in the present analysis. The study was in accordance with the World Medical Association Declaration of Helsinki-Ethical Principles for Medical Research Involving Human Subjects and was approved by the Ethics Committee of China Medical University. A written informed consent form was obtained from all participants after they had been informed of the objectives, benefits and confidentiality of personal information.
Anthropometric measures
The anthropometric indices were measured using standard techniques and equipments with the subjects in light clothing after an overnight fast. BMI was calculated as weight in kilograms divided by the square of height in meters (kg/m2). NC was measured at the level of the laryngeal prominence using a flexible tape, with the subjects in the standing position and the head held erect and eyes facing forward. WC was measured at the level of the midpoint between the lower rib margin and the iliac crest. HC was measured at the level of maximal protrusion of the gluteal muscles. WHR was calculated as WC divided by HC.
BPs measurements and definition
Based on the standardized procedural guidelines33, 34, BPs were measured using a standard mercury-column sphygmomanometer after 15 minutes of rest in the sitting position. At the first examination, BPs were measured in both right arm and left arm. When there is a consistent inter-arm difference, the arm with the higher pressure was used. The average of 3 consecutive measurements to the nearest 2 mmHg in the one selected arm was recorded. Participants were advised not to drink alcohol, tea or coffee, smoke and to take exercise for at least 30 minutes before measuring BPs. Essential hypertension was defined as an average SBP ≥ 140 mmHg and/or an average DBP ≥ 90 mmHg, and/or currently receiving treatment for hypertension with antihypertensive medicine.
Data collection
All participants underwent a self-administered questionnaire delivered by a face-to-face interview. The questionnaire had two parts: the first section elicited baseline information of demographic characteristic; the second section elicited information on tobacco use, alcohol consumption, salt consumption, and physical activity as well as other health-related information. Smoking and drinking status were categorized as current-, former- and non-smoking or drinking, which were detailed in our previous paper35. Physical activity levels were categorized as high (≥3 days of vigorous-intensity activity achieving ≥1500 metabolic equivalent of energy (MET)-minutes/week, or ≥7 days of any combination of walking, moderate- or vigorous intensity activities achieving ≥3000 MET-minutes/week), moderate (not meeting the criteria for the “high” category and ≥3 days of vigorous-intensity activity of at least 20 minutes/day or ≥5 days of moderate-intensity activity or walking of at least 30 minutes/day or ≥5 days of any combination of walking, moderate- or vigorous intensity activities achieving ≥600 MET-minutes/week), and low (not meeting any of the above mentioned criteria) categories36.
All participants were asked for permission to collect a blood sample after an overnight fast of >8 hours. The concentrations of TC, TG, HDL-C, LDL-C, and FBG in samples were determined using a Mindray Autoanalyzer (BS 380 type; Mindray Ltd.; Shenzhen, China) in local community health service centers as well as environment and non-communicable diseases research centers, China Medical University. All assays were performed according to the manufacturer’s instructions.
Statistical analysis
As human body shape differs according to gender, the data for females and males were treated separately. All of the continuous variables were tested for normality by Shapiro-Wilks W test before Student’s t-test, and those non-normally distributed variables were log-transformed to reach normality and variance homogeneity. Differences in the distribution of baseline characteristics between males and females were tested using student’s t-test for continuous variables (age, BMI, WC, HC, NC, WHR, SBP, DBP, FBG, TG, TC, LDL-C, HDL-C and salt consumption) and chi-square test for categorical variables (family history of hypertension, education levels, smoking and drinking status and physical activity). Generalized linear regression models were used to examine the associations of NC with SBP and DBP. Univariate and multivariate logistic regression models were used to assess the association between NC and hypertension risk. We performed univariate regression analysis to evaluate the potential risk factors of arterial BPs and hypertension, and those with p < 0.2 in the univariate analysis were included in the multivariate model. Additionally, to avoid the problem of multi-collinearity, BMI and WC were included in the models as categorical variables, because multicollinearity between categorical variables was thought to be not as strong as that between continuous variables37. Normal weight was defined as a BMI < 24, overweight was defined as 24 ≤ BMI < 28, and obesity was defined as a BMI ≥ 2838. Abdominal obesity was defined based on WC (WC ≥ 85 cm for males and ≥80 cm for females). Therefore, model 1 included only NC. In model 2, we adjusted for age, FBG, salt consumption, smoking and drinking status, physical activity and family history of hypertension. In model 3, we adjusted for the covariates in model 2 as well as BMI categories. In model 4, we adjusted for the covariates in model 2 as well as WC categories. In model 5, we adjusted for the covariates in model 2 as well as WHR. Subsequently, ROC analysis was performed to assess the accuracy of NC as diagnostic test for hypertension, and determine optimal sex, age and BMI-specific cut-offs of NC for predicting hypertension. Logistic regression models were also used to assess the associations of NC (per unit increases of NC) and NC categories (≥cut off value versus < cut-off value) with hypertension risk. All statistical analyses were performed using SPSS software (version 17.0; SPSS Inc,. Chicago, IL, USA). A two tailed p value < 0.05 was taken as statistically significant.
References
Lawes, C. M., Vander, H. S. & Rodgers, A. International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet 371, 1513–1518 (2008).
Siani, A. et al. The relationship of waist circumference to blood pressure: the Olivetti Heart Study. Am. J. Hypertens. 15, 780–786 (2002).
Dyer, A. R. et al. Ten-year incidence of elevated blood pressure and its predictors: the CARDIA study. Coronary Artery Risk Development in (Young) Adults. J. Hum. Hypertens. 13, 13–21 (1999).
Kannel, W. B., Brand, N., Skinner, J. J., Dawber, T. R. & McNamara, P. M. The relation of adiposity to blood pressure and development of hypertension. The Framingham study. Ann. Intern. Med. 67, 48–59 (1967).
Fox, C. S. et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116, 39–48 (2007).
Freedman, D. S. & Rimm, A. A. The relation of body fat distribution, as assessed by six girth measurements, to diabetes mellitus in women. Am. J. Public Health 79, 715–720 (1989).
Hoebel, S., Malan, L. & de Ridder, J. H. Determining cut-off values for neck circumference as a measure of the metabolic syndrome amongst a South African cohort: the SABPA study. Endocrine 42, 335–342 (2012).
Onat, A. et al. Neck circumference as a measure of central obesity: associations with metabolic syndrome and obstructive sleep apnea syndrome beyond waist circumference. Clin. Nutr. 28, 46–51 (2009).
Preis, S. R. et al. Neck circumference as a novel measure of cardiometabolic risk: the Framingham Heart Study. J. Clin. Endocrinol Metab. 95, 3701–3710 (2010).
Kurtoglu, S., Hatipoglu, N., Mazicioglu, M. M. & Kondolot, M. Neck circumference as a novel parameter to determine metabolic risk factors in obese children. Eur. J. Clin. Invest. 42, 623–630 (2012).
Androutsos, O. et al. Neck circumference: a useful screening tool of cardiovascular risk in children. Pediatr. Obes. 7, 187–195 (2012).
Zhou, J. Y. et al. Neck circumference as an independent predictive contributor to cardio-metabolic syndrome. Cardiovasc. Diabetol. 12, 76 (2013).
Luo, Y. Q. et al. Neck circumference as an effective measure for identifying cardiometabolic syndrome: a comparison with waist circumference. Endocrine 55, 822–830 (2017).
Liang, J. et al. Neck circumference and prehypertension: the cardiometabolic risk in Chinese study. J. Hypertens. 33, 275–278 (2015).
Yang, B. et al. Associations of MTHFR C677T and MTRR A66G gene polymorphisms with metabolic syndrome: a case-control study in Northern China. Int. J. Mol. Sci. 15, 21687–702 (2014).
The World Bank. Toward a healthy and harmonious life in China: Stemming the rising tide of non-communicable disease. Available online: http://www.worldbank,org/en/news/2011/07/26/toward-health-harmonious-life-china-stemming-rising-tide-of-non-communicable-diseases (accessed on 21 July 2016).
Yang, B. et al. Geograpgical and ethnic distribution of MTHFR gene polymorphisms and their associations with diseases among Chinese population. Clin. Genet. doi:10.1111/cge.12929 (2016).
Assyov, Y., Gateva, A., Tsakova, A. & Kamenov, Z. A comparison of the clinical usefulness of neck circumference and waist circumference in individuals with severe obesity. Endocr. Res. 1–9 (2016).
Lee, B. J. & Kim, J. Y. A comparison of the predictive power of anthropometric indices for hypertension and hypotension risk. PloS One 9, e84897 (2014).
Nafiu, O. O., Zepeda, A., Curcio, C. & Prasad, Y. Association of neck circumference and obesity status with elevated blood pressure in children. J. Hum. Hypertens. 28, 263–268 (2014).
Ben-Noun, L. L. & Laor, A. Relationship between changes in neck circumference and changes in blood pressure. Am. J. Hypertens. 17, 409–414 (2004).
Koutsari, C., Snozek, C. L. & Jensen, M. D. Plasma NEFA storage in adipose tissue in the postprandial state: sex-related and regional differences. Diabetologia 51, 2041–2048 (2008).
Kissebah, A. H., Alfarsi, S., Adams, P. W. & Wynn, V. Role of insulin resistance in adipose tissue and liver in the pathogenesis of endogenous hypertriglyceridaemia in man. Diabetologia 12, 563–571 (1976).
Piro, S. et al. Direct apoptotic effects of free fatty acids on human endothelial cells. Nutr. Metab. Cardiovasc. Dis. 18, 96–104 (2008).
Stojiljkovic, M. P. et al. Increasing plasma fatty acids elevates F2-isoprostanes in humans: implications for the cardiovascular risk factor cluster. J. Hypertens. 20, 1215–1221 (2002).
Santosa, S. & Jensen, M. D. Why are we shaped differently, and why does it matter? Am. J. Physiol. Endocrinol. Metab. 295, E531–E535 (2008).
Calhoun, D. A. Obstructive sleep apnea and hypertension. Curr. Hypertens. Rep. 12, 189–195 (2010).
Nieto, F. J. et al. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 283, 1829–1836 (2000).
Apaydin, M., Ayik, S. O., Akhan, G., Peker, S. & Uluc, E. Carotid intima-media thickness increase in patients with habitual simple snoring and obstructive sleep apnea syndrome is associated with metabolic syndrome. J. Clin. Ultrasound 41, 290–296 (2013).
Kawano, Y. et al. Report of the working group for dietary salt reduction of the Japanese society of hypertension: (2) assessment of salt intake in the management of hypertension. Hypertens. Res. 30, 887–893 (2007).
Kaneko, S. et al. Estimation of salt intake using a questionnaire. J. Health Human Ecol. 59, 113–122 (1993).
Qin, Y. et al. Salt intake, knowledge of salt intake, and blood pressure control in Chinese hypertensive patients. J. Am. Soc. Hypertens. 8, 909–914 (2014).
Kirkendall, W. M., Feinleib, M., Freis, E. D. & Mark, A. L. Recommendations for human blood pressure determination by sphygmomanometers. Subcommittee of the AHA Postgraduate Education Committee. Hypertension 3, 510A–519A (1981).
Pickering, T. G. et al. Recommendations for blood pressure measurement in humans and experimental animals: part 1: blood pressure measurement in humans: a statement for professionals from the Subcommittee of Professional and Public Education of the American Heart Association Council on High Blood Pressure Research. Circulation 111, 697–716 (2005).
Fan, S. et al. Interactions of Methylenetetrahydrofolate Reductase C677T Polymorphism with Environmental Factors on Hypertension Susceptibility. Int. J. Environ. Res. Public Health 13, pii: E601. 10.3390/ijerph 13060601 (2016).
Wu, F. et al. Common risk factors for chronic non-communicable diseases among older adults in China, Ghana, Mexico, India, Russia and South Africa: the study on global AGEing and adult health (SAGE) wave 1. BMC Public Health 15, 88 (2015).
Zhou, Z., Hu, D. & Chen, J. Association between obesity indices and blood pressure or hypertension: which index is the best? Public Health Nutr 12, 1061–1071 (2009).
Fan, S. J. et al. Are MTHFR C677T and MTRR A66G Polymorphisms Associated with Overweight/Obesity Risk? From a Case-Control to a Meta-Analysis of 30,327 Subjects. Int. J. Mol. Sci. 16, 11849–11863 (2015).
Acknowledgements
The authors gratefully acknowledge the assistance and cooperation of the faculty and staff of Shenhe Center for Disease Control and Prevention, and thank all of the participants in our study. We also thank Prarthana Nair in China Medical University for her elaborative reviewing of this manuscript and useful suggestions on language use. This study was supported by a grand from the Educational Department of Liaoning Province (No. 20131015900).
Author information
Authors and Affiliations
Contributions
S.F., B.Y. and G.S. conceived and designed the experiments. S.F., B.Y., X.Z., J.H., P.M. and L.Y. performed the experiments. S.F. and B.Y. analyzed the data. Q.Z. contributed reagents/materials/analysis tools. S.F., and B.Y. wrote the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fan, S., Yang, B., Zhi, X. et al. Neck circumference associated with arterial blood pressures and hypertension: A cross-sectional community-based study in northern Han Chinese. Sci Rep 7, 2620 (2017). https://doi.org/10.1038/s41598-017-02879-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-02879-7
This article is cited by
-
Evaluation of the appropriate predictive contributor and diagnostic threshold for the cardio-metabolic syndrome in Chinese Uyghur adults
BMC Public Health (2019)
-
Neck circumference as an indicator of elevated blood pressure independent from body composition: implications from the China nation health survey (CNHS)
BMC Cardiovascular Disorders (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.