Abstract
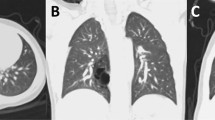
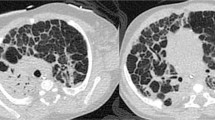
Congenital lung malformations (CLMs) are rare developmental anomalies of the lung, including congenital pulmonary airway malformations (CPAM), bronchopulmonary sequestration, congenital lobar overinflation, bronchogenic cyst and isolated congenital bronchial atresia. CLMs occur in 4 out of 10,000 live births. Postnatal presentation ranges from an asymptomatic infant to respiratory failure. CLMs are typically diagnosed with antenatal ultrasonography and confirmed by chest CT angiography in the first few months of life. Although surgical treatment is the gold standard for symptomatic CLMs, a consensus on asymptomatic cases has not been reached. Resection, either thoracoscopically or through thoracotomy, minimizes the risk of local morbidity, including recurrent infections and pneumothorax, and avoids the risk of malignancies that have been associated with CPAM, bronchopulmonary sequestration and bronchogenic cyst. However, some surgeons suggest expectant management as the incidence of adverse outcomes, including malignancy, remains unknown. In either case, a planned follow-up and a proper transition to adult care are needed. The biological mechanisms through which some CLMs may trigger malignant transformation are under investigation. KRAS has already been confirmed to be somatically mutated in CPAM and other genetic susceptibilities linked to tumour development have been explored. By summarizing current progress in CLM diagnosis, management and molecular understanding we hope to highlight open questions that require urgent attention.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Panicek, D. M. et al. The continuum of pulmonary developmental anomalies. Radiographics 7, 747–772 (1987).
Stocker, J. T., Madewell, J. E. & Drake, R. M. Congenital cystic adenomatoid malformation of the lung. Classification and morphologic spectrum. Hum. Pathol. 8, 155–171 (1977).
Alshamiri, K. M. & Abbod, H. B. Congenital cystic adenomatoid malformation. Int. J. Pediatr. Adolesc. Med. 4, 159–160 (2017).
Gupta, K. et al. Revisiting the histopathologic spectrum of congenital pulmonary developmental disorders. Fetal Pediatr. Pathol. 31, 74–86 (2012).
Annunziata, F. et al. Congenital lung malformations: unresolved issues and unanswered questions. Front. Pediatr. 7, 239 (2019).
Laberge, J. M. et al. Outcome of the prenatally diagnosed congenital cystic adenomatoid lung malformation: a Canadian experience. Fetal Diagn. Ther. 16, 178–186 (2001).
Gornall, A. S., Budd, J. L., Draper, E. S., Konje, J. C. & Kurinczuk, J. J. Congenital cystic adenomatoid malformation: accuracy of prenatal diagnosis, prevalence and outcome in a general population. Prenat. Diagn. 23, 997–1002 (2003).
Stocker, L. J., Wellesley, D. G., Stanton, M. P., Parasuraman, R. & Howe, D. T. The increasing incidence of foetal echogenic congenital lung malformations: an observational study. Prenat. Diagn. 35, 148–153 (2015).
Lau, C. T., Kan, A., Shek, N., Tam, P. & Wong, K. K. Is congenital pulmonary airway malformation really a rare disease? Result of a prospective registry with universal antenatal screening program. Pediatr. Surg. Int. 33, 105–108 (2017). This paper recalculated the incidence of congenital lung malformations.
Thompson, A. J., Sidebotham, E. L., Chetcuti, P. A. J. & Crabbe, D. C. G. Prenatally diagnosed congenital lung malformations — a long-term outcome study. Pediatr. Pulmonol. 53, 1442–1446 (2018).
Sfakianaki, A. K. & Copel, J. A. Congenital cystic lesions of the lung: congenital cystic adenomatoid malformation and bronchopulmonary sequestration. Rev. Obstet. Gynecol. 5, 85–93 (2012).
Zobel, M., Gologorsky, R., Lee, H. & Vu, L. Congenital lung lesions. Semin. Pediatr. Surg. 28, 150821 (2019).
Moorthie, S. et al. Estimating the birth prevalence and pregnancy outcomes of congenital malformations worldwide. J. Community Genet. 9, 387–396 (2018).
Hermelijn, S. M. et al. Associated anomalies in congenital lung abnormalities: a 20-year experience. Neonatology 117, 697–703 (2020).
Kunisaki, S. M. et al. Fetal risk stratification and outcomes in children with prenatally diagnosed lung malformations: results from a multi-institutional research collaborative. Ann. Surg. 276, e622–e630 (2022).
Kersten, C. M. et al. COllaborative Neonatal Network for the first European CPAM Trial (CONNECT): a study protocol for a randomised controlled trial. BMJ Open 13, e071989 (2023).
Hartman, G. E. & Shochat, S. J. Primary pulmonary neoplasms of childhood: a review. Ann. Thorac. Surg. 36, 108–119 (1983).
Nasr, A., Himidan, S., Pastor, A. C., Taylor, G. & Kim, P. C. Is congenital cystic adenomatoid malformation a premalignant lesion for pleuropulmonary blastoma? J. Pediatr. Surg. 45, 1086–1089 (2010).
Casagrande, A. & Pederiva, F. Association between congenital lung malformations and lung tumors in children and adults: a systematic review. J. Thorac. Oncol. 11, 1837–1845 (2016). This systematic review collected, to our knowledge, for the first time all the paediatric and adult cases of congenital lung malformations associated with lung tumours.
Walsh, S., Wood, A. E. & Greally, P. Pleuropulmonary blastoma type I following resection of incidentally found congenital lobar emphysema. Ir. Med. J. 102, 230 (2009).
Bogers, A. J., Hazebroek, F. W., Molenaar, J. & Bos, E. Surgical treatment of congenital bronchopulmonary disease in children. Eur. J. Cardiothorac. Surg. 7, 117–120 (1993).
Korol, E. The correlation of carcinoma and congenital cystic emphysema of the lungs; report of ten cases. Dis. Chest 23, 403–411 (1953).
Brcic, L. et al. Pleuropulmonary blastoma type I might arise in congenital pulmonary airway malformation type 4 by acquiring a Dicer 1 mutation. Virchows Arch. 477, 375–382 (2020).
Messinger, Y. H. et al. Pleuropulmonary blastoma: a report on 350 central pathology-confirmed pleuropulmonary blastoma cases by the International Pleuropulmonary Blastoma Registry. Cancer 121, 276–285 (2015).
Rossi, G. et al. MUC5AC, cytokeratin 20 and HER2 expression and K-RAS mutations within mucinogenic growth in congenital pulmonary airway malformations. Histopathology 60, 1133–1143 (2012).
Nelson, N. D. et al. Defining the spatial landscape of KRAS mutated congenital pulmonary airway malformations: a distinct entity with a spectrum of histopathologic features. Mod. Pathol. 35, 1870–1881 (2022).
Hermelijn, S. M. et al. Early KRAS oncogenic driver mutations in nonmucinous tissue of congenital pulmonary airway malformations as an indicator of potential malignant behavior. Hum. Pathol. 103, 95–106 (2020).
Summers, R. J., Shehata, B. M., Bleacher, J. C., Stockwell, C. & Rapkin, L. Mucinous adenocarcinoma of the lung in association with congenital pulmonary airway malformation. J. Pediatr. Surg. 45, 2256–2259 (2010).
Cass, D. L. et al. Increased cell proliferation and decreased apoptosis characterize congenital cystic adenomatoid malformation of the lung. J. Pediatr. Surg. 33, 1043–1046 (1998).
Hsu, J. S. et al. Cancer gene mutations in congenital pulmonary airway malformation patients.ERJ Open Res. 5, 00196-2018 (2019).
Patrizi, S., Pederiva, F. & d’Adamo, A. P. Whole-genome methylation study of congenital lung malformations in children. Front. Oncol. 11, 689833 (2021). This study described, to our knowledge, for the first time methylation anomalies in congenital lung malformations in children.
Luo, J. et al. PITX2 enhances progression of lung adenocarcinoma by transcriptionally regulating WNT3A and activating Wnt/β-catenin signaling pathway. Cancer Cell Int. 19, 96 (2019).
Goldstein, B., Trivedi, M. & Speth, R. C. Alterations in gene expression of components of the renin-angiotensin system and its related enzymes in lung cancer. Lung Cancer Int. 2017, 6914976 (2017).
Kunisaki, S. M. Narrative review of congenital lung lesions. Transl. Pediatr. 10, 1418–1431 (2021).
Taylor, B., Rice, A., Nicholson, A. G., Hind, M. & Dean, C. H. Mechanism of lung development in the aetiology of adult congenital pulmonary airway malformations. Thorax 75, 1001–1003 (2020).
Lezmi, G. et al. Congenital cystic adenomatoid malformations of the lung: diagnosis, treatment, pathophysiological hypothesis [French]. Rev. Pneumol. Clin. 69, 190–197 (2013).
Langston, C. New concepts in the pathology of congenital lung malformations. Semin. Pediatr. Surg. 12, 17–37 (2003).
Correia-Pinto, J., Gonzaga, S., Huang, Y. & Rottier, R. Congenital lung lesions — underlying molecular mechanisms. Semin. Pediatr. Surg. 19, 171–179 (2010).
Doktor, F., Antounians, L., Lacher, M. & Zani, A. Congenital lung malformations: dysregulated lung developmental processes and altered signaling pathways. Semin. Pediatr. Surg. 31, 151228 (2022).
Simonet, W. S. et al. Pulmonary malformation in transgenic mice expressing human keratinocyte growth factor in the lung. Proc. Natl Acad. Sci. USA 92, 12461–12465 (1995).
Clark, J. C. et al. FGF-10 disrupts lung morphogenesis and causes pulmonary adenomas in vivo. Am. J. Physiol. Lung Cell Mol. Physiol. 280, L705–L715 (2001).
White, A. C. et al. FGF9 and SHH signaling coordinate lung growth and development through regulation of distinct mesenchymal domains. Development 133, 1507–1517 (2006).
Warburton, D. et al. The molecular basis of lung morphogenesis. Mech. Dev. 92, 55–81 (2000).
Leibel, S. L., McVicar, R. N., Winquist, A. M., Niles, W. D. & Snyder, E. Y. Generation of complete multi-cell type lung organoids from human embryonic and patient-specific induced pluripotent stem cells for infectious disease modeling and therapeutics validation. Curr. Protoc. Stem Cell Biol. 54, e118 (2020).
Gonzaga, S. et al. Cystic adenomatoid malformations are induced by localized FGF10 overexpression in fetal rat lung. Am. J. Respir. Cell Mol. Biol. 39, 346–355 (2008).
Wang, X. et al. Elevated Kruppel-like factor 5 expression in spatiotemporal mouse lungs is similar to human congenital cystic adenomatoid malformation of the lungs. J. Int. Med. Res. 46, 2856–2865 (2018).
Guseh, J. S. et al. Notch signaling promotes airway mucous metaplasia and inhibits alveolar development. Development 136, 1751–1759 (2009).
Kim, J. H. et al. Lack of epithelial PPARγ causes cystic adenomatoid malformations in mouse fetal lung. Biochem. Biophys. Res. Commun. 491, 271–276 (2017).
Stocker, J. T. Congenital pulmonary airway malformation — a new name for and an expanded classification of congenital cystic adenomatoid malformation of the lung. Histopathology 41, 424–458 (2002).
Pogoriler, J., Swarr, D., Kreiger, P., Adzick, N. S. & Peranteau, W. Congenital cystic lung lesions: redefining the natural distribution of subtypes and assessing the risk of malignancy. Am. J. Surg. Pathol. 43, 47–55 (2019).
Dehner, L. P., Schultz, K. A. P. & Hill, D. A. Congenital pulmonary airway malformations with a reconsideration and current perspective on the stocker classification. Pediatr. Dev. Pathol. 26, 241–249 (2023).
Szafranski, P. et al. Phenotypic expansion of TBX4 mutations to include acinar dysplasia of the lungs. Am. J. Med. Genet. A 170, 2440–2444 (2016).
Vincent, M. et al. Clinical, histopathological, and molecular diagnostics in lethal lung developmental disorders. Am. J. Respir. Crit. Care Med. 200, 1093–1101 (2019).
Imai, Y. & Mark, E. J. Cystic adenomatoid change is common to various forms of cystic lung diseases of children: a clinicopathologic analysis of 10 cases with emphasis on tracing the bronchial tree. Arch. Pathol. Lab. Med. 126, 934–940 (2002).
Kunisaki, S. M. et al. Bronchial atresia: the hidden pathology within a spectrum of prenatally diagnosed lung masses. J. Pediatr. Surg. 41, 61–65 (2006).
Riedlinger, W. F. et al. Bronchial atresia is common to extralobar sequestration, intralobar sequestration, congenital cystic adenomatoid malformation, and lobar emphysema. Pediatr. Dev. Pathol. 9, 361–373 (2006).
Swarr, D. T. et al. Novel molecular and phenotypic insights into congenital lung malformations. Am. J. Respir. Crit. Care Med. 197, 1328–1339 (2018).
Dehner, L. P. et al. Type I pleuropulmonary blastoma versus congenital pulmonary airway malformation type IV. Neonatology 111, 76 (2017).
MacSweeney, F. et al. An assessment of the expanded classification of congenital cystic adenomatoid malformations and their relationship to malignant transformation. Am. J. Surg. Pathol. 27, 1139–1146 (2003).
Dehner, L. P. et al. Pleuropulmonary blastoma: evolution of an entity as an entry into a familial tumor predisposition syndrome. Pediatr. Dev. Pathol. 18, 504–511 (2015).
Volpe, M. V., Archavachotikul, K., Bhan, I., Lessin, M. S. & Nielsen, H. C. Association of bronchopulmonary sequestration with expression of the homeobox protein Hoxb-5. J. Pediatr. Surg. 35, 1817–1819 (2000).
Gabelloni, M., Faggioni, L., Accogli, S., Aringhieri, G. & Neri, E. Pulmonary sequestration: what the radiologist should know. Clin. Imaging 73, 61–72 (2021).
Conran, R. M. & Stocker, J. T. Extralobar sequestration with frequently associated congenital cystic adenomatoid malformation, type 2: report of 50 cases. Pediatr. Dev. Pathol. 2, 454–463 (1999).
Cass, D. L. et al. Cystic lung lesions with systemic arterial blood supply: a hybrid of congenital cystic adenomatoid malformation and bronchopulmonary sequestration. J. Pediatr. Surg. 32, 986–990 (1997).
Alamo, L., Vial, Y., Gengler, C. & Meuli, R. Imaging findings of bronchial atresia in fetuses, neonates and infants. Pediatr. Radiol. 46, 383–390 (2016).
Kravitz, R. M. Congenital malformations of the lung. Pediatr. Clin. North Am. 41, 453–472 (1994).
Ortiz, R. J. et al. Bronchogenic cyst: lessons learned in 20 years of experience at a tertiary pediatric center. J. Pediatr. Surg. https://doi.org/10.1016/j.jpedsurg.2023.06.010 (2023).
Morikawa, N. et al. Congenital bronchial atresia in infants and children. J. Pediatr. Surg. 40, 1822–1826 (2005).
Kunisaki, S. M. et al. Current operative management of congenital lobar emphysema in children: a report from the Midwest Pediatric Surgery Consortium. J. Pediatr. Surg. 54, 1138–1142 (2019).
Tsai, A. Y. et al. Outcomes after postnatal resection of prenatally diagnosed asymptomatic cystic lung lesions. J. Pediatr. Surg. 43, 513–517 (2008).
Wong, A., Vieten, D., Singh, S., Harvey, J. G. & Holland, A. J. Long-term outcome of asymptomatic patients with congenital cystic adenomatoid malformation. Pediatr. Surg. Int. 25, 479–485 (2009).
Lujan, M. et al. Late-onset congenital cystic adenomatoid malformation of the lung. Embryology, clinical symptomatology, diagnostic procedures, therapeutic approach and clinical follow-up. Respiration 69, 148–154 (2002).
Ng, C., Stanwell, J., Burge, D. M. & Stanton, M. P. Conservative management of antenatally diagnosed cystic lung malformations. Arch. Dis. Child. 99, 432–437 (2014).
Criss, C. N. et al. Asymptomatic congenital lung malformations: Is nonoperative management a viable alternative? J. Pediatr. Surg. 53, 1092–1097 (2018).
Adzick, N. S. et al. Fetal cystic adenomatoid malformation: prenatal diagnosis and natural history. J. Pediatr. Surg. 20, 483–488 (1985).
Kunisaki, S. M. et al. Large fetal congenital cystic adenomatoid malformations: growth trends and patient survival. J. Pediatr. Surg. 42, 404–410 (2007).
Macardle, C. A. et al. Surveillance of fetal lung lesions using the congenital pulmonary airway malformation volume ratio: natural history and outcomes. Prenat. Diagn. 36, 282–289 (2016).
Monni, G. et al. Prenatal ultrasound diagnosis of congenital cystic adenomatoid malformation of the lung: a report of 26 cases and review of the literature. Ultrasound Obstet. Gynecol. 16, 159–162 (2000).
Achiron, R., Gindes, L., Zalel, Y., Lipitz, S. & Weisz, B. Three- and four-dimensional ultrasound: new methods for evaluating fetal thoracic anomalies. Ultrasound Obstet. Gynecol. 32, 36–43 (2008).
Priest, J. R., Williams, G. M., Hill, D. A., Dehner, L. P. & Jaffe, A. Pulmonary cysts in early childhood and the risk of malignancy. Pediatr. Pulmonol. 44, 14–30 (2009).
Downard, C. D. et al. Treatment of congenital pulmonary airway malformations: a systematic review from the APSA outcomes and evidence based practice committee. Pediatr. Surg. Int. 33, 939–953 (2017).
Perlman, S. et al. The added value of f-TAPSE in the surveillance of pregnancies complicated by fetal and placental tumors. Prenat. Diagn. 37, 788–792 (2017).
Girsen, A. I. et al. Prediction of neonatal respiratory distress in pregnancies complicated by fetal lung masses. Prenat. Diagn. 37, 266–272 (2017).
Crombleholme, T. M. et al. Cystic adenomatoid malformation volume ratio predicts outcome in prenatally diagnosed cystic adenomatoid malformation of the lung. J. Pediatr. Surg. 37, 331–338 (2002).
David, M., Lamas-Pinheiro, R. & Henriques-Coelho, T. Prenatal and postnatal management of congenital pulmonary airway malformation. Neonatology 110, 101–115 (2016).
Kane, S. C., Ancona, E., Reidy, K. L. & Palma-Dias, R. The utility of the congenital pulmonary airway malformation-volume ratio in the assessment of fetal echogenic lung lesions: a systematic review. Fetal Diagn. Ther. 47, 171–181 (2020).
Delacourt, C. et al. Predicting the risk of respiratory distress in newborns with congenital pulmonary malformations.Eur. Respir. J. 59, 2100949 (2022).
Gerall, C. et al. Prenatal ultrasound- and MRI-based imaging predictors of respiratory symptoms at birth for congenital lung malformations. J. Pediatr. Surg. 58, 420–426 (2023).
Peters, N. C. J. et al. Prediction of postnatal outcome in fetuses with congenital lung malformation: 2-year follow-up study. Ultrasound Obstet. Gynecol. 58, 428–438 (2021).
Ehrenberg-Buchner, S. et al. Fetal lung lesions: can we start to breathe easier? Am. J. Obstet. Gynecol. 208, 151.e1-7 (2013).
Ruchonnet-Metrailler, I. et al. Neonatal outcomes of prenatally diagnosed congenital pulmonary malformations. Pediatrics 133, e1285-91 (2014).
Mon, R. A. et al. Diagnostic accuracy of imaging studies in congenital lung malformations. Arch. Dis. Child. Fetal Neonatal Ed. 104, F372–F377 (2019).
Newman, B. Magnetic resonance imaging for congenital lung malformations. Pediatr. Radiol. 52, 312–322 (2022).
Wong, K. K. Y., Flake, A. W., Tibboel, D., Rottier, R. J. & Tam, P. K. H. Congenital pulmonary airway malformation: advances and controversies. Lancet Child Adolesc. Health 2, 290–297 (2018). This paper highlighted the open controversies on the management of congenital lung malformations that are still unresolved.
Tivnan, P., Winant, A. J., Epelman, M. & Lee, E. Y. Pediatric congenital lung malformations: imaging guidelines and recommendations. Radiol. Clin. North Am. 60, 41–54 (2022).
Style, C. C. et al. Accuracy of prenatal and postnatal imaging for management of congenital lung malformations. J. Pediatr. Surg. 55, 844–847 (2020).
Narayan, R. R. et al. Predicting pathology from imaging in children undergoing resection of congenital lung lesions. J. Surg. Res. 236, 68–73 (2019).
Cheeney, S. H. E., Maloney, E. & Iyer, R. S. Safety considerations related to intravenous contrast agents in pediatric imaging. Pediatr. Radiol. https://doi.org/10.1007/s00247-022-05470-z (2022).
Hermelijn, S. M. et al. A clinical guideline for structured assessment of CT-imaging in congenital lung abnormalities. Paediatr. Respir. Rev. 37, 80–88 (2021).
Kim, W. S. et al. Congenital cystic adenomatoid malformation of the lung: CT-pathologic correlation. Am. J. Roentgenol. 168, 47–53 (1997).
Parikh, D. H. & Rasiah, S. V. Congenital lung lesions: postnatal management and outcome. Semin. Pediatr. Surg. 24, 160–167 (2015).
Calvert, J. K. & Lakhoo, K. Antenatally suspected congenital cystic adenomatoid malformation of the lung: postnatal investigation and timing of surgery. J. Pediatr. Surg. 42, 411–414 (2007).
Sauvat, F., Michel, J. L., Benachi, A., Emond, S. & Revillon, Y. Management of asymptomatic neonatal cystic adenomatoid malformations. J. Pediatr. Surg. 38, 548–552 (2003).
El-Ali, A. M., Strubel, N. A. & Lala, S. V. Congenital lung lesions: a radiographic pattern approach. Pediatr. Radiol. 52, 622–636 (2022).
Merli, L. et al. Congenital lung malformations: a novel application for lung ultrasound? J. Ultrasound 24, 349–353 (2021).
Quercia, M., Panza, R., Calderoni, G., Di Mauro, A. & Laforgia, N. Lung ultrasound: a new tool in the management of congenital lung malformation. Am. J. Perinatol. 36, S99–S105 (2019).
Kellenberger, C. J. et al. Structural and perfusion magnetic resonance imaging of congenital lung malformations. Pediatr. Radiol. 50, 1083–1094 (2020).
Ciet, P. & Litmanovich, D. E. MR safety issues particular to women. Magn. Reson. Imaging Clin. N. Am. 23, 59–67 (2015).
Elders, B. et al. Congenital lung abnormalities on magnetic resonance imaging: the CLAM study. Eur. Radiol. https://doi.org/10.1007/s00330-023-09458-7 (2023).
Fowler, D. J. & Gould, S. J. The pathology of congenital lung lesions. Semin. Pediatr. Surg. 24, 176–182 (2015).
Desai, S. et al. Secondary vascular changes in pulmonary sequestrations. Histopathology 57, 121–127 (2010).
Mukhtar, S. & Trovela, D. A. V. Congenital Lobar Emphysema (StatPearls Publishing, 2022).
Schuster, S. R., Harris, G. B., Williams, A., Kirkpatrick, J. & Reid, L. Bronchial atresia: a recognizable entity in the pediatric age group. J. Pediatr. Surg. 13, 682–689 (1978).
Peranteau, W. H. et al. Effect of maternal betamethasone administration on prenatal congenital cystic adenomatoid malformation growth and fetal survival. Fetal Diagn. Ther. 22, 365–371 (2007).
Muntean, A. et al. The long-term outcome following thoraco-amniotic shunting for congenital lung malformations. J. Pediatr. Surg. 58, 213–217 (2023).
Rosenblat, O. et al. In-utero treatment of prenatal thoracic abnormalities by thoraco-amniotic shunts, short and long term neuro developmental outcome: a single center experience. J. Pediatr. Surg. 57, 364–368 (2022).
Morris, L. M., Lim, F. Y., Livingston, J. C., Polzin, W. J. & Crombleholme, T. M. High-risk fetal congenital pulmonary airway malformations have a variable response to steroids. J. Pediatr. Surg. 44, 60–65 (2009).
Kunisaki, S. M. & Jennings, R. W. Fetal surgery. J. Intensive Care Med. 23, 33–51 (2008).
Bratu, I. et al. The multiple facets of pulmonary sequestration. J. Pediatr. Surg. 36, 784–790 (2001).
da Silva, O. P., Ramanan, R., Romano, W., Bocking, A. & Evans, M. Nonimmune hydrops fetalis, pulmonary sequestration, and favorable neonatal outcome. Obstet. Gynecol. 88, 681–683 (1996).
Litwinska, M. et al. Management options for fetal bronchopulmonary sequestration. J. Clin. Med. 11, 1724 (2022).
Mallmann, M. R. et al. Bronchopulmonary sequestration with massive pleural effusion: pleuroamniotic shunting vs intrafetal vascular laser ablation. Ultrasound Obstet. Gynecol. 44, 441–446 (2014).
Rothenberg, S. S. First decade’s experience with thoracoscopic lobectomy in infants and children. J. Pediatr. Surg. 43, 40–44 (2008).
Rothenberg, S. S. Thoracoscopic lobectomy in infants and children. J. Laparoendosc. Adv. Surg. Tech. A 31, 1157–1161 (2021). This paper comprehensively describes the technique of thoracoscopic lobectomy as well as the preoperative and postoperative care.
Rothenberg, S. S. et al. Two decades of experience with thoracoscopic lobectomy in infants and children: standardizing techniques for advanced thoracoscopic surgery. J. Laparoendosc. Adv. Surg. Tech. A 25, 423–428 (2015).
Cano, I., Anton-Pacheco, J. L., Garcia, A. & Rothenberg, S. Video-assisted thoracoscopic lobectomy in infants. Eur. J. Cardiothorac. Surg. 29, 997–1000 (2006).
Bonnard, A. Thoracoscopic lobectomy for congenital pulmonary airway malformation: where are we in 2019? Eur. J. Pediatr. Surg. 30, 146–149 (2020).
Rothenberg, S. S. et al. Thoracoscopic lobectomy in infants less than 10 kg with prenatally diagnosed cystic lung disease. J. Laparoendosc. Adv. Surg. Tech. A 21, 181–184 (2011).
Lawal, T. A., Gosemann, J. H., Kuebler, J. F., Gluer, S. & Ure, B. M. Thoracoscopy versus thoracotomy improves midterm musculoskeletal status and cosmesis in infants and children. Ann. Thorac. Surg. 87, 224–228 (2009).
Adams, S. et al. Does thoracoscopy have advantages over open surgery for asymptomatic congenital lung malformations? An analysis of 1626 resections. J. Pediatr. Surg. 52, 247–251 (2017).
Laberge, J. M., Puligandla, P. & Flageole, H. Asymptomatic congenital lung malformations. Semin. Pediatr. Surg. 14, 16–33 (2005).
Kapralik, J., Wayne, C., Chan, E. & Nasr, A. Surgical versus conservative management of congenital pulmonary airway malformation in children: a systematic review and meta-analysis. J. Pediatr. Surg. 51, 508–512 (2016).
Duron, V. et al. Asymptomatic congenital lung malformations: timing of resection does not affect adverse surgical outcomes. Front. Pediatr. 8, 35 (2020).
Esposito, C. et al. Thoracoscopic management of pediatric patients with congenital lung malformations: results of a European Multicenter Survey. J. Laparoendosc. Adv. Surg. Tech. A 31, 355–362 (2021).
Engall, N., Sethuraman, C., Wilkinson, D. J., Lansdale, N. & Peters, R. T. Does timing of resection influence the presence of inflammation within congenital lung malformations? Eur. J. Pediatr. Surg. 33, 81–84 (2023).
Elhattab, A. et al. Thoracoscopic surgery for congenital lung malformations: does previous infection really matter? J. Pediatr. Surg. 56, 1982–1987 (2021).
Garrett-Cox, R., MacKinlay, G., Munro, F. & Aslam, A. Early experience of pediatric thoracoscopic lobectomy in the UK. J. Laparoendosc. Adv. Surg. Tech. A 18, 457–459 (2008).
Mei-Zahav, M., Konen, O., Manson, D. & Langer, J. C. Is congenital lobar emphysema a surgical disease? J. Pediatr. Surg. 41, 1058–1061 (2006).
Aziz, D. et al. Perinatally diagnosed asymptomatic congenital cystic adenomatoid malformation: to resect or not? J. Pediatr. Surg. 39, 329–334 (2004).
Chetcuti, P. A. & Crabbe, D. C. CAM lungs: the conservative approach. Arch. Dis. Child. Fetal Neonatal Ed. 91, F463–F464 (2006).
Hall, N. J., Chiu, P. P. & Langer, J. C. Morbidity after elective resection of prenatally diagnosed asymptomatic congenital pulmonary airway malformations. Pediatr. Pulmonol. 51, 525–530 (2016).
Aspirot, A. et al. A contemporary evaluation of surgical outcome in neonates and infants undergoing lung resection. J. Pediatr. Surg. 43, 508–512 (2008).
Rahman, N. & Lakhoo, K. Comparison between open and thoracoscopic resection of congenital lung lesions. J. Pediatr. Surg. 44, 333–336 (2009).
Bunduki, V. et al. Prognostic factors associated with congenital cystic adenomatoid malformation of the lung. Prenat. Diagn. 20, 459–464 (2000).
Robson, V. K., Shieh, H. F., Wilson, J. M. & Buchmiller, T. L. Non-operative management of extralobar pulmonary sequestration: a safe alternative to resection? Pediatr. Surg. Int. 36, 325–331 (2020).
Cook, J., Chitty, L. S., De Coppi, P., Ashworth, M. & Wallis, C. The natural history of prenatally diagnosed congenital cystic lung lesions: long-term follow-up of 119 cases. Arch. Dis. Child. 102, 798–803 (2017).
Karlsson, M., Conner, P., Ehren, H., Bitkover, C. & Burgos, C. M. The natural history of prenatally diagnosed congenital pulmonary airway malformations and bronchopulmonary sequestrations. J. Pediatr. Surg. 57, 282–287 (2022).
Dossche, L. W. J. et al. Long-term neurodevelopment in children with resected congenital lung abnormalities. Eur. J. Pediatr. https://doi.org/10.1007/s00431-023-05054-5 (2023).
Duarte, J. C., Ferreira, P. G., Alfaro, T. M., Carvalho, L. & Ferreira, A. J. Cystic adenomatoid pulmonary malformation in adults: a retrospective study in a tertiary university hospital. Rev. Port. Pneumol. 23, 109–110 (2017).
Gorospe, L. et al. Cystic adenomatoid malformation of the lung in adult patients: clinicoradiological features and management. Clin. Imaging 40, 517–522 (2016).
Hamanaka, R., Yagasaki, H., Kohno, M., Masuda, R. & Iwazaki, M. Congenital cystic adenomatoid malformation in adults: report of a case presenting with a recurrent pneumothorax and a literature review of 60 cases. Respir. Med. Case Rep. 26, 328–332 (2019).
Polaczek, M. et al. Clinical presentation and characteristics of 25 adult cases of pulmonary sequestration. J. Thorac. Dis. 9, 762–767 (2017).
Berrington de Gonzalez, A., Pasqual, E. & Veiga, L. Epidemiological studies of CT scans and cancer risk: the state of the science.Br. J. Radiol. 94, 20210471 (2021).
Eber, E. Adult outcome of congenital lower respiratory tract malformations. Swiss Med. Wkly 136, 233–240 (2006).
Davenport, M. & Eber, E. Long term respiratory outcomes of congenital thoracic malformations. Semin. Fetal Neonatal Med. 17, 99–104 (2012).
Hall, N. J. & Stanton, M. P. Long-term outcomes of congenital lung malformations. Semin. Pediatr. Surg. 26, 311–316 (2017).
Spoel, M. et al. Lung function of infants with congenital lung lesions in the first year of life. Neonatology 103, 60–66 (2013).
Hijkoop, A. et al. Lung function, exercise tolerance, and physical growth of children with congenital lung malformations at 8 years of age. Pediatr. Pulmonol. 54, 1326–1334 (2019).
Calzolari, F. et al. Outcome of infants operated on for congenital pulmonary malformations. Pediatr. Pulmonol. 51, 1367–1372 (2016).
Markel, M. et al. Congenital lung malformation patients experience respiratory infections after resection: a population-based cohort study. J. Pediatr. Surg. 57, 829–832 (2022).
Barikbin, P. et al. Postnatal lung function in congenital cystic adenomatoid malformation of the lung. Ann. Thorac. Surg. 99, 1164–1169 (2015).
Huang, J. X., Hong, S. M., Hong, J. J., Chen, Q. & Cao, H. Medium-term pulmonary function test after thoracoscopic lobectomy and segmentectomy for congenital lung malformation: a comparative study with normal control. Front. Pediatr. 9, 755328 (2021).
Dincel, A. et al. Long-term respiratory outcomes of post-op congenital lung malformations. Pediatr. Int. 63, 704–709 (2021).
Tocchioni, F. et al. Long-term lung function in children following lobectomy for congenital lung malformation. J. Pediatr. Surg. 52, 1891–1897 (2017).
Willers, C. et al. School-age structural and functional MRI and lung function in children following lung resection for congenital lung malformation in infancy. Pediatr. Radiol. 52, 1255–1265 (2022).
Lau, C. T., Wong, K. K. Y. & Tam, P. Medium term pulmonary function test after thoracoscopic lobectomy for congenital pulmonary airway malformation: a comparative study with normal control. J. Laparoendosc. Adv. Surg. Tech. A 28, 595–598 (2018).
Albanese, C. T. & Rothenberg, S. S. Experience with 144 consecutive pediatric thoracoscopic lobectomies. J. Laparoendosc. Adv. Surg. Tech. A 17, 339–341 (2007).
Lam, F. K. F., Lau, C. T., Yu, M. O. & Wong, K. K. Y. Comparison of thoracoscopy vs. thoracotomy on musculoskeletal outcomes of children with congenital pulmonary airway malformation (CPAM). J. Pediatr. Surg. 56, 1732–1736 (2021).
Sadeghi, A. H. et al. Virtual reality and artificial intelligence for 3-dimensional planning of lung segmentectomies. JTCVS Tech. 7, 309–321 (2021).
Bakhuis, W. et al. Preoperative visualization of congenital lung abnormalities: hybridizing artificial intelligence and virtual reality.Eur. J. Cardiothorac. Surg. 63, ezad014 (2022).
Sumner, T. E., Phelps, C. R. 2nd, Crowe, J. E., Poolos, S. P. & Shaffner, L. D. Pulmonary blastoma in a child. Am. J. Roentgenol. 133, 147–148 (1979).
Papagiannopoulos, K. A., Sheppard, M., Bush, A. P. & Goldstraw, P. Pleuropulmonary blastoma: is prophylactic resection of congenital lung cysts effective? Ann. Thorac. Surg. 72, 604–605 (2001).
Veronesi, G. et al. Report on first international workshop on robotic surgery in thoracic oncology. Front. Oncol. 6, 214 (2016).
Ballouhey, Q. et al. A comparison of robotic surgery in children weighing above and below 15.0 kg: size does not affect surgery success. Surg. Endosc. 29, 2643–2650 (2015). This paper gives an outlook on the application of robotic surgery in patients with congenital lung malformations.
Durand, M. et al. Robotic lobectomy in children with severe bronchiectasis: a worthwhile new technology. J. Pediatr. Surg. 56, 1606–1610 (2021).
Ballouhey, Q. et al. Assessment of paediatric thoracic robotic surgery. Interact. Cardiovasc. Thorac. Surg. 20, 300–303 (2015).
Meehan, J. J., Phearman, L. & Sandler, A. Robotic pulmonary resections in children: series report and introduction of a new robotic instrument. J. Laparoendosc. Adv. Surg. Tech. A 18, 293–295 (2008).
Herriges, M. & Morrisey, E. E. Lung development: orchestrating the generation and regeneration of a complex organ. Development 141, 502–513 (2014).
Leblanc, C. et al. Congenital pulmonary airway malformations: state-of-the-art review for pediatrician’s use. Eur. J. Pediatr. 176, 1559–1571 (2017).
Mullassery, D. & Smith, N. P. Lung development. Semin. Pediatr. Surg. 24, 152–155 (2015).
Morrisey, E. E. & Hogan, B. L. Preparing for the first breath: genetic and cellular mechanisms in lung development. Dev. Cell 18, 8–23 (2010).
Prince, L. S. FGF10 and human lung disease across the life spectrum. Front. Genet. 9, 517 (2018).
Bernstein, E. et al. Dicer is essential for mouse development. Nat. Genet. 35, 215–217 (2003).
Harris, K. S., Zhang, Z., McManus, M. T., Harfe, B. D. & Sun, X. Dicer function is essential for lung epithelium morphogenesis. Proc. Natl Acad. Sci. USA 103, 2208–2213 (2006).
Yuan, T., Volckaert, T., Chanda, D., Thannickal, V. J. & De Langhe, S. P. Fgf10 signaling in lung development, homeostasis, disease, and repair after injury. Front. Genet. 9, 418 (2018).
Yu, J. et al. Induced pluripotent stem cell lines derived from human somatic cells. Science 318, 1917–1920 (2007).
Danopoulos, S. et al. Discordant roles for FGF ligands in lung branching morphogenesis between human and mouse. J. Pathol. 247, 254–265 (2019).
Otto-Verberne, C. J., Ten Have-Opbroek, A. A., Balkema, J. J. & Franken, C. Detection of the type II cell or its precursor before week 20 of human gestation, using antibodies against surfactant-associated proteins. Anat. Embryol. 178, 29–39 (1988).
Liggins, G. C. The role of cortisol in preparing the fetus for birth. Reprod. Fertil. Dev. 6, 141–150 (1994).
Jobe, A. H. & Ikegami, M. Lung development and function in preterm infants in the surfactant treatment era. Annu. Rev. Physiol. 62, 825–846 (2000).
Author information
Authors and Affiliations
Contributions
Introduction (F.P.); Epidemiology (F.P. and J.M.S.); Mechanism/pathophysiology (K.K.Y.W., A.P.D. and F.P.); Diagnosis, screening and prevention (R.A., P.C., F.P. and J.v.d.T.); Management (N.H., J.M.S., S.S.R. and F.P.); Quality of life (H.I.); Outlook (F.P.). All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Disease Primers thanks M. Davenport, A. W. Flake, S. Kunisaki, G. B. Mychaliska and N. Usui for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Acinar dysplasia
-
A rare malformation characterized by growth arrest of the lower respiratory tract and complete absence of gas-exchanging units, resulting in critical respiratory insufficiency at birth.
- Acinar-like tissue
-
A tissue composed of polarized epithelial cells rich in rough endoplasmic reticulum and characterized by an abundance of secretory zymogen granules.
- Channels of Lambert
-
Microscopic collateral airways between the distal bronchiolar tree and adjacent alveoli.
- Congenital anomalies
-
Structural or functional anomalies occurring during intrauterine life and affecting an estimated 6% of global live births (WHO definition).
- Congenital diaphragmatic hernia
-
A defect in the diaphragm causing the herniation of abdominal contents into the thoracic cavity, resulting in lung hypoplasia and altered pulmonary vascular development.
- Epithelial–mesenchymal interaction
-
A series of programmed, sequential and reciprocal communications between the epithelium and the mesenchyme, with its heterotypic cell population, that result in the differentiation of one or both cell populations.
- EXIT-to-resection
-
In the EXIT-to-resection procedure, a hysterotomy is performed to exteriorize the fetal head and torso enabling orotracheal intubation and placement of peripheral IV; the lung malformation can be resected while the fetus is still on placental support34.
- Foregut duplication cysts
-
Benign developmental anomalies that contain foregut derivatives.
- Hydrops
-
Abnormal interstitial fluid collection in two or more compartments of the fetal body.
- Lung compliance
-
A measure of the expansion of the lung.
- Mediastinal shift
-
The deviation of mediastinal structures towards one side of the chest cavity.
- Oesophageal duplication
-
Separate masses along or in continuity with the native oesophagus.
- Polyhydramnios
-
A condition that occurs when too much amniotic fluid builds up during pregnancy.
- Pores of Kohn
-
Small communications between adjacent pulmonary alveoli that provide a collateral pathway for aeration.
- Thoraco-amniotic shunt
-
A shunt that drains fluid from the lung into the amniotic sac to treat pleural effusion, for example, in congenital pulmonary airway malformations.
- Tidal volumes
-
The amount of air that moves in or out of the lungs with each respiratory cycle.
- Tricuspid annular plane systole excursion
-
A scoring system used with non-invasive Doppler echocardiography to determine right ventricular function.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pederiva, F., Rothenberg, S.S., Hall, N. et al. Congenital lung malformations. Nat Rev Dis Primers 9, 60 (2023). https://doi.org/10.1038/s41572-023-00470-1
Accepted:
Published:
DOI: https://doi.org/10.1038/s41572-023-00470-1
This article is cited by
-
Kongenitale Lungenfehlbildungen
Die Radiologie (2024)