Abstract
Background/Objectives
To evaluate the factors influencing final visual outcome after surgical repair of open globe injuries (OGIs) in a rural population using the International Globe and Adnexal Trauma Epidemiology Study (IGATES) online registry.
Subjects/Methods
Retrospective cohort study of patients with OGI. OGIs were identified from the IGATES database at a tertiary referral eye care centre in rural West India over a period of 12 years. Patient demographics, clinical and pre-operative factors affecting final visual outcome was evaluated.
Results
A total of 791 eyes with OGIs were included in data analysis. 11 eyes that were lost to follow-up and 12 eyes with incomplete data were excluded. Most of the patients were male (559, 70.6%) and mean age of all patients was 23.9 years ± 19.4 years. Occupational hazards (including domestic housework) (307, 38.8%) and leisure play (324, 41.0%) were the leading causes of OGI. The most common mechanism of injury was being struck by a wooden stick (250, 31.6%).
Univariate analysis of pre-operative variables showed initial visual acuity (VA), zone of injury, size of wound, structures involved in the injury and presence of infection were significant prognostic factors for worse final visual outcome (p < 0.001). Multivariate analysis showed VA ≤ 3/60 or worse at presentation had statistically significantly higher odds ratio of ending up with worse visual outcomes (p < 0.012).
Conclusions
Males in working age groups suffer from OGIs more frequently, usually from agricultural and pastoral activities. Initial VA, zone 3 injuries, corneoscleral wound, large wound size and presence of post-traumatic infections are significant prognostic factors.
Similar content being viewed by others
Introduction
Open globe injuries (OGIs) are a common cause of permanent visual loss internationally, both in developed and developing countries. Ocular trauma is reported to be one of the most important causes of unilateral vision loss in developing countries and previous epidemiological studies have found that rural populations may have a greater burden of vision impairment or blindness caused by trauma [1, 2]. Risk factors such as male gender, workplace, road accidents, and lower socioeconomic status have been reported [3,4,5,6]. The Birmingham Eye Trauma Terminology (BETTS) [7] defines OGIs as a full thickness injury to the eyeball. They can be secondary to rupture caused by a blunt object or laceration caused by a sharp object, and can be further stratified into penetrating (entrance wound), perforating (entrance and exit wounds) or intraocular foreign body injuries. OGIs are difficult to manage, resulting in successful surgical repair and subsequent visual rehabilitation becoming topics of great significance and challenge.
The International Globe and Adnexal Trauma Epidemiology Study (IGATES) is a collaborative effort of the Asia Pacific Ophthalmic Trauma Society, International Society of Ocular Trauma, Chinese Ocular Trauma Society, and Ocular Trauma Society of India. Limitations and controversies exist with the use of BETTS and ocular trauma score (OTS) [8], which were developed decades ago for the prediction of visual outcomes. The primary aim of IGATES is to develop an updated prognostic classification system for ocular trauma that is in line with updated ocular trauma practice. Data from this current study was collected from rural West India and was derived from the IGATES database. While there have been many epidemiological studies on ocular trauma in rural populations [4, 5, 9, 10], there is a paucity of published studies which look specifically into the prognostic factors affecting final visual outcomes in OGIs. Existing studies which do so have a low sample size and may not be fully representative [11, 12]. This study aims to contribute to existing literature on ocular trauma in rural India and evaluate the risk factors for poor final visual outcomes in OGIs.
Materials (subjects) and methods
This was a retrospective cohort study performed at a tertiary referral eye care centre in rural West India using the IGATES data registry, which includes all OGIs over a 12-year period (from January 2008 to December 2019).
Data recorded included patients’ demographic characteristics, affected eye, mechanism of injury (activity and object), place and circumstances of the injury, duration to primary repair of OGI, initial and final VA, wound characteristics (shape and size of wound), zone of injury, types of wounds (involvement of lid, sclera, cornea or cornea-scleral), presence of infections and total number of surgeries that the patients underwent. Patients who had incomplete data or whom were lost to follow-up were excluded from analysis.
The type and zone of injury were defined according to the classification system of the Ocular Trauma Classification Group [13]. The location of injury was defined as Zone 1 (wound involvement limited to the cornea, including corneoscleral limbus), Zone 2 (wound involving 5 mm of sclera from the corneoscleral limbus), or Zone 3 (wound involving the sclera posterior to the 5 mm from the corneoscleral limbus). Initial and final VA were grouped according to the Snellen chart as no light perception, hand motion (HM) to light perception (LP), counting fingers (CF), 3/60 to 1/60, >6/12 to 6/60, and ≥6/12.
Statistical analysis was carried out using IBM SPSS Statistics (version 27, IBM Corp, New York, USA). Chi-square or Fisher’s Exact Test with p-value estimated using Monte–Carlo simulation was used to analyse the categorical data depending on whether the expected cell value was more than or less than 5. Comparison of statistical differences of continuous data between independent groups was performed by Kruskal–Wallis Test. The unadjusted odds ratio and its 95% confidence interval were obtained by univariate ordinal logistic regression. Additional multivariate analysis (ordinal logistic regression) was conducted to adjust for known prognostic factors and potential confounders.
The study was approved by the local Institutional Ethics Committee (Ophthalmic Mission Trust Ethical Committee) and follows the tenets of the Declaration of Helsinki.
Results
A total of 814 eyes with OGIs were identified, with 791 eyes meeting the inclusion criteria. 11 eyes that were lost to follow-up and 12 eyes with incomplete data were excluded from the analysis.
Demography and clinical data
The demographics and clinical characteristics of the patient population are shown in Table 1a. Most of the patients were males (559, 70.6%) and the mean age of all patients was 23.9 years ± 19.4 years. Most patients were in the age groups of 0–18 years [405 (51.2%)] followed by 19–50 years [291 (36.8%)]. The age group of 19–50 years was statistically significant in predicting poor final VA (Table 1b). The left and right eyes were almost equally affected, with right eye involved in 409 (51.7%) patients and left eye in 382 (48.3%) patients. Most eyes had presenting VA of HM - PL [318 (49.6%)].
The characteristics of the OGIs are seen in Table 2. Of the 791 eyes, majority of the injuries were in Zone 1 [626 (79.1%)]. The rest of the injuries were split relatively equally between Zone 2 [89 (11.3%)] and Zone 3 [76 (9.6%)]. Lid involvement was found in 13 (1.6%) eyes. Most of the wounds were linear in shape [732 (92.6%)] and the mean wound size was 5.9 ± 2.9 mm. 480 (60.7%) eyes had wounds involving only the cornea, 106 (13.4%) eyes involving only the sclera and 205 (25.9%) eyes involving both the cornea and the sclera. Infections consisting of both endophthalmitis and/or infective keratitis developed in 32 eyes (4.0%) and these patients received immediate topical and intravitreal antibiotics therapy. Majority of these eyes had Zone 3 injuries [27 (84.4%)].
Circumstances and mechanism of injury
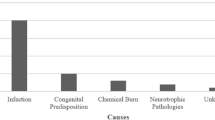
Occupational hazards and leisure play were the leading causes of OGIs in our study, with 307 (38.8%) eyes injured during industrial work and housework, and 324 (41.0%) eyes injured during leisure play. Housework is a broad term which includes all unpaid domestic activities in the form of cooking, cleaning, gardening and gathering food, water or firewood. In the context of a rural Indian population, there is a disproportionately high number of females who are involved in domestic housework due to societal norms. Hence, we decided to include it in our analysis under occupational hazards, which also includes other activities such as industrial and agricultural work. Other activities leading to injury include vehicular injuries (either from accidents or when travelling in unsheltered vehicles), falls, fights and use of explosives. The miscellaneous group constitutes patients in which activities leading to injury were either not well-defined or omitted in the clinical records. The activity leading to injury is shown in Fig. 1a. The most common mechanism of injury was being struck by a wooden stick (250, 31.6%), followed by flying stones (84, 10.6%) and iron wires (61, 7.7%). The miscellaneous group constitutes non-specific mechanisms of injuries, which were not well-defined in the clinical notes. The mechanisms of injury are shown in Fig. 1b.
Surgery
After repair of open globe injury, 646 eyes (81.6%) had VA worse than 6/12. The mean number of surgeries that the patients underwent was 1.8 ± 0.9 and the median duration from time of presentation to surgery was 0.0 days (IQR 1.0–2.0). There was no statistical significance between these two factors and the final VA (Table 1b).
Visual outcomes
Initial VA was found to be statistically significant in predicting final visual outcome (p < 0.001) (Table 1b). As seen in Table 3, on univariate analysis, eyes with VA 3/60 or worse had statistically significant higher odds of ending up with worse visual outcomes. This was also seen in multivariate analysis (Table 4). Univariate analysis showed that the zone of injury was statistically significant in final VA. A Zone 3 injury was 3.71 times (p < 0.001, 95% CI 2.38, 5.76) more likely to result in poor visual outcome on univariate analysis (Table 3) but not on multivariate analysis. The size of the wounds and the structures involved in the injury were statistically significant in relation to the final VA. A larger wound (>6 mm in length) and a cornea-scleral wound were 1.21 times (p < 0.001, 95% CI 1.16, 1.27) and 1.90 times (p < 0.001, 95% CI 1.42, 2.55) more likely to result in poorer visual outcome respectively (Table 3). There was no statistical significance between the shape of the wound and the final VA (Table 1b).
For infected eyes, their visual outcomes were poor, with 10 eyes (31.3%) retaining only HM to LP vision and 10 eyes (31.3%) having no LP vision. The presence of infections had a 3.14 times (p < 0.001, 95% CI 1.64, 5.99) higher likelihood of resulting in poor visual outcome on univariate analysis (Table 3).
Discussion
In India, Ophthalmology services, like most health services, are distributed unequally, with the bulk of services focusing on the urban population [4]. Our tertiary referral centre serves a largely rural population from 3 different districts, receiving more than 60,000 referrals each year, both in the outpatient clinics and emergency department. These districts consist mainly of rural villages whose economies are largely agricultural and pastoral-based [14, 15].
IGATES is split into 2 distinct phases: IGATES-1 consists of a series of retrospective studies to discover key variables, which will then be consolidated into a clinical risk score for validation in IGATES-2, a series of prospective studies. Our recently-published study [6] evaluated some of the clinical factors influencing final visual outcome after surgical repair of OGIs and provided insights into some of the possible variables that can be included in the future clinical risk score. Our eventual goal is to use big data analytics and machine learning to propose a robust model incorporating a wide range of relevant markers to better prognosticate visual outcomes. In this retrospective study, which is part of IGATES-1, we analysed the patient demographics and pre-operative factors affecting final visual outcome following primary repair of 791 OGIs in rural Western India.
The most recent India Population Census [16] stated that there was a higher proportion of males than females in the rural and agricultural workforce. Male preponderance in ocular trauma, which was seen in previous rural population-based studies [4, 5], is consistent with our study findings (70.6%), although it is not statistically significant in the final visual outcome (p = 0.568). The male gender preponderance may reflect the more aggressive characteristics of male behaviour and to a lesser extent, reflect the involvement of men in higher risk working activities. According to existing literature, this trend appears to be similar in developed countries [3, 17,18,19]. In our study, OGIs occurred in all age groups, with a higher prevalence in 0–18 year-olds. The mean age of around 24 years was younger than what was seen in previous studies [19,20,21]. In the same above-mentioned Population Census [16], the younger age groups made up a larger proportion of the population compared to the older age groups. This would mean that more people have to start work at a younger age, and this longer duration of work could potentially predispose them to ocular trauma and OGIs.
The mean duration from initial injury to eventual surgery in our study is much longer than other studies. This abnormally long duration to surgery is unique to our study as health care services are not readily available for the rural population. These patients suffered OGIs and did not seek immediate medical care and were eventually picked up from outreach camps or screening exercises. It is important to note that these patients subsequently had minimal delay in undergoing surgery once their injuries were picked up.
Pre-operative VA was found to be statistically significant on both univariate and multivariate analysis in predicting poor visual outcome. This is consistent with various previous studies [6, 19, 21,22,23,24,25,26]. A decision tree devised by Schmidt et al. [19] showed that initial vision is a key predictor in the open globe outcome prognostic tree and was found to correlate significantly with poorer visual outcomes. Both Rahman et al. [24] and Pieramici et al. [23] described a statistically significant inferior outcome when initial VA was worse than 20/200, with a strong predictor of eventual enucleation. In our study, an initial presenting vision of CF or worse was statistically significant in predicting a poorer final visual outcome. Agrawal et al. [20] however, disagreed on pre-operative VA as a prognostic factor. This discrepancy is possibly due to the exclusion of eyes with endophthalmitis, which would have likely conferred poor initial visual acuity. Another possible explanation could be the difficulty in getting an accurate determination of VA in the emergency department as patients may be in pain and may not be fully cooperative.
Location of wounds and wound characteristics are factors which can affect final visual acuity. In our study, we found that Zone 3 injuries tend to result in poorer visual outcomes and this is statistically significant. This result is consistent with existing literature [18, 20,21,22, 27]. This can be expected clinically because posterior segment injury can cause irreversible damage to the retina and optic nerve, leading to poor visual prognosis even after the structural integrity of the globe has been restored. A larger wound size, as well as a corneoscleral wound, were also found to be statistically significant in resulting in a poorer final visual outcome. These findings are supported in other studies [18, 25, 26, 28]. A larger wound that involves both the cornea and sclera reflects more extensive ocular tissue damage and a higher likelihood of posterior involvement. Cruvinel Isaac et al. [18] found that for each millimetre added to the length of the lesion, there is a 1.28-fold increase in the chance of having a worse prognosis. Rofail et al. [25] found that a laceration larger than 10 mm had a 14.49-fold risk of attaining a final VA of CF or worse compared with lacerations that were 1–5 mm. In our study, the presence of lid lacerations was also associated with poorer visual outcomes in univariate analysis, although this is not seen in multivariate analysis. One possibility for this finding is that the presence of lid lacerations could indicate a more significant traumatic ocular injury that resulted in more extensive concomitant ocular injuries. Lid lacerations or injuries associated with poorer visual outcomes have also been seen in other studies [26, 29].
Post-traumatic endophthalmitis was reported to be 4–8% in OGIs [21, 30, 31]. In our study, the rate of infections (although non-specific to endophthalmitis) was also found to be around 4%, which is consistent with existing literature. The presence of post-traumatic infections was found to be 3.14 times more likely to result in poorer visual outcomes and this was statistically significant. These findings were also seen in other studies [32, 33]. However, one important factor to note was that most of the cases with infections had Zone 3 injuries, which by itself is also a predictor of poor visual outcomes. In our study, the number of surgeries was not statistically significant in predicting final visual outcomes. This was inconsistent with other studies [33,34,35]. A possible explanation for the discrepancy is that the initial management of OGIs in the centre is typically primary closure, even if there were concomitant complications. The patient would then undergo further assessment in an elective setting, followed by subsequent surgeries such as cataract surgery or vitrectomy for vitreous haemorrhage. These would have improved the ocular media and hence improved visual outcomes as well. Finally, a large retrospective case series by Andreoli and Andreoli [36] noted that more than half the OGIs only require initial open globe repair, and even amongst the rest of these patients, most of them only require 1 more additional surgery. This is consistent with our findings, where most patients require 1–2 surgeries after suffering from OGIs.
As previously mentioned, housework is a broad term which includes all unpaid domestic activities in the form of cooking, cleaning, gardening and gathering food, water or firewood. These activities expose subjects to hazards that can predispose them to ocular trauma. Occupational hazards which include both labour work and household chores are the main contributors to OGIs in our study. As mentioned earlier, our centre serves a mostly rural population whose economies are largely agricultural and pastoral-based [14, 15]. Agriculture remains one of the most hazardous occupations with a high prevalence of work-related eye injuries [37,38,39]. In a rural region where agriculture is mostly labour intensive, ocular injuries from vegetation and equipment, such as being hit by wooden sticks, are commonplace. We can hence infer that OGIs are more likely to occur as well. Rearing livestock also has its inherent risks of ocular trauma and subsequent OGI when poked or kicked by the animals. This is particularly unique to a society where pastoral activities contribute to a major part of the economy [16]. In the more developed countries, ocular injuries from animals tend to come from domestic pets such as dogs or from arachnoids and insects during leisure activities like hiking [40]. As most of the studied population stay in rural areas where rearing livestock constitutes a large part of their livelihood, there were 3 animal-related injuries including being poked in the eye by a cow’s horns or a bird’s beak or a direct trauma from a cow’s leg. Vegetative injury such as being hit by flying thorns were also common.
Our study was limited by the absence of any data on the use of eye protection within the population, but we know that the use of protective eyewear amongst agriculture workers is less prevalent [41, 42] and almost non-existent in India. Studies have shown that the use of protective eyewear at work and during sports is invaluable in preventing eye injuries [43, 44]. A recent study by Chatterjee and Agrawal [45] on protective eyewear amongst agricultural workers also showed the effectiveness of eyewear protection, but noted the barriers to eyewear including apathy, cosmesis and discomfort, especially in a hot and humid climate such as India. An additional factor in the indifference towards protective eyewear may be due to the relative illiteracy of the farmers in many of the rural villages [16], who may not have been educated on the use of these eyewear even though there are published standards and guidelines by the Bureau of Indian Standards [46]. A recent report by the Ministry of Labour and Employment of the Government of India [47] has also indicated that despite the various efforts in place to regulate work safety in “unorganised” sectors including agricultural and pastoral work in the studied districts, the implementation of the legislation has been tardy. Involving community health workers to educate workers will help to improve eye protection compliance.
The strength of our study is its large sample size, making it one of the largest retrospective studies reporting on prognostic factors and visual outcomes from OGIs in a rural population. This has allowed us to better understand and compare between a developed and rural population in terms of demographic characteristics and factors affecting final visual outcomes. These results are also an important addition to the IGATES database by providing invaluable data that is derived from a rural population [38,39,40].
The study had some limitations, as it is a retrospective study conducted over a long period of time, where there could be selection bias through convenience sampling. Secondly, a retrospective study design meant that we were unable to calculate the OTS [8] due to missing data. Comparison of OTS with existing literature and IGATES in the future would provide us with additional insights. However, while we do understand that these issues may be better answered with a prospective controlled study, our study still provides an invaluable addition to existing literature, which is lacking for rural Indian populations.
Furthermore, our study has a lack of specific data on anterior and posterior segment complications, such as the presence of relative afferent pupillary defect, hyphaema, vitreous haemorrhage or retinal detachment, which have been shown in many previous studies to be clinically significant in prognosticating final visual outcomes in developed countries [6, 19,20,21, 25]. Whilst these clinical findings are well-established prognostic factors for poor visual outcome, our study provides information on lesser-known clinical findings including various aspects of wound characteristics, such as length and shape.
A possible future solution to limitations in data collection would be the development of a national ophthalmic trauma registry and possible integration into a global registry, which would standardise the data collection of demographic and clinical factors used for descriptive and comparative analysis.
In conclusion, our study has found that amongst the rural population, males in the working age groups suffer OGIs more frequently, usually from agricultural and pastoral activities. Initial VA, zone 3 injuries, corneoscleral wound, large wound size and the presence of post-traumatic infections are significant prognostic factors that can result in poor visual outcomes. While there are legislative guidelines in India on protective eyewear during labour activities, future studies are warranted to assess the indifference and lack of awareness amongst rural workers, which may be a significant barrier towards the uptake of protective eyewear.
Summary
What was known before
-
Males have a higher predisposition towards ocular trauma and open globe injuries (OGIs) in both developing and developed countries—Clinical characteristics from OGIs such as the presenting visual acuity, wound location and characteristics, as well as post-traumatic infections lead to poor visual outcomes.
What this study adds
-
In rural regions where the economy is labour intensive and largely agricultural and pastoral-based, ocular injuries from vegetation, work equipment as well as livestock are commonplace—As far as we know, this study is one of the largest retrospective studies that reports on the prognostic factors and visual outcomes from OGIs in a rural population.
References
Thylefors B. Epidemiological patterns of ocular trauma. Aust N. Z J Ophthalmol. 1992;20:95–8.
Negrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5:143–69.
Dandona L, Dandona R, Srinivas M, John RK, McCarty CA, Rao GN. Ocular trauma in an urban population in southern India: the Andhra Pradesh Eye Disease Study. Clin Exp Ophthalmol. 2000;28:350–6.
Krishnaiah S, Nirmalan PK, Shamanna BR, Srinivas M, Rao GN, Thomas R. Ocular trauma in a rural population of southern India: the Andhra Pradesh Eye Disease Study. Ophthalmology. 2006;113:1159–64.
Nirmalan PK, Katz J, Tielsch JM, Robin AL, Thulasiraj RD, Krishnadas R, et al. Ocular trauma in a rural south Indian population: the Aravind Comprehensive Eye Survey. Ophthalmology. 2004;111:1778–81.
Toh ZH, Agrawal S, Raje D, Hoskin A, Agrawal R, Khandelwal R. International globe and adnexal trauma epidemiology study (IGATES): a report from Central India on visual outcome in open globe injuries and correlation with ocular trauma score. Int Ophthalmol. 2020;40:2797–806.
Kuhn F, Morris R, Witherspoon CD. Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries. Ophthalmol Clin North Am. 2002;15:139–43. v.
Kuhn F, Maisiak R, Mann L, Mester V, Morris R, Witherspoon CD. The Ocular Trauma Score (OTS). Ophthalmol Clin North Am. 2002;15:163–5. vi.
Abraham DI, Vitale SI, West SI, Isseme I. Epidemiology of eye injuries in rural Tanzania. Ophthalmic Epidemiol. 1999;6:85–94.
Khatry SK, Lewis AE, Schein OD, Thapa MD, Pradhan EK, Katz J. The epidemiology of ocular trauma in rural Nepal. Br J Ophthalmol. 2004;88:456–60.
Mackiewicz J, Machowicz-Matejko E, Salaga-Pylak M, Piecyk-Sidor M. Zagorski Z. Work-related, penetrating eye injuries in rural environments. Ann Agric Environ Med. 2005;12:27–9.
Misra S, Nandwani R, Gogri P, Misra N. Clinical profile and visual outcome of ocular injuries in a rural area of western India. Australas Med J. 2013;6:560–4.
Pieramici DJ, Sternberg P Jr, Aaberg TM Sr, Bridges WZ Jr, Capone A Jr, Cardillo JA, et al. A system for classifying mechanical injuries of the eye (globe). The Ocular Trauma Classification Group. Am J Ophthalmol. 1997;123:820–31.
Jhabua DA. District Jhabua: National Informatics Center, Jhabua. 2021. https://jhabua.nic.in/en/.
District Administration B. Official Website of Banswara: Department of Information Technology & Communication. 2021. https://banswara.rajasthan.gov.in/content/raj/banswara/en/home.html#.
Office of the Registrar General & Census Commissioner I. CensusInfo India 2011 Final Population Totals: Ministry of Home Affairs, Government of India. 2020. http://dataforall.org/dashboard/censusinfoindia_pca/.
Wong TY, Tielsch JM. A population-based study on the incidence of severe ocular trauma in Singapore. Am J Ophthalmol. 1999;128:345–51.
Cruvinel Isaac DL, Ghanem VC, Nascimento MA, Torigoe M, Kara-Jose N. Prognostic factors in open globe injuries. Ophthalmologica. 2003;217:431–5.
Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115:202–9.
Agrawal R, Wei HS, Teoh S. Prognostic factors for open globe injuries and correlation of ocular trauma score at a tertiary referral eye care centre in Singapore. Indian J Ophthalmol. 2013;61:502–6.
Yalcin Tok O, Tok L, Eraslan E, Ozkaya D, Ornek F, Bardak Y. Prognostic factors influencing final visual acuity in open globe injuries. J Trauma. 2011;71:1794–800.
Agrawal R, Rao G, Naigaonkar R, Ou X, Desai S. Prognostic factors for vision outcome after surgical repair of open globe injuries. Indian J Ophthalmol. 2011;59:465–70.
Pieramici DJ, Au Eong KG, Sternberg P Jr, Marsh MJ. The prognostic significance of a system for classifying mechanical injuries of the eye (globe) in open-globe injuries. J Trauma. 2003;54:750–4.
Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye. 2006;20:1336–41.
Rofail M, Lee GA, O’Rourke P. Prognostic indicators for open globe injury. Clin Exp Ophthalmol. 2006;34:783–6.
Yucel OE, Demir S, Niyaz L, Sayin O, Gul A, Ariturk N. Clinical characteristics and prognostic factors of scleral rupture due to blunt ocular trauma. Eye. 2016;30:1606–13.
Agrawal R, Wei HS, Teoh S. Predictive factors for final outcome of severely traumatized eyes with no light perception. BMC Ophthalmol. 2012;12:16.
Barr CC. Prognostic factors in corneoscleral lacerations. Arch Ophthalmol. 1983;101:919–24.
Hatton MP, Thakker MM, Ray S. Orbital and adnexal trauma associated with open-globe injuries. Ophthalmic Plast Reconstr Surg. 2002;18:458–61.
Falcao M, Camisa E, Falcao-Reis F. Characteristics of open-globe injuries in northwestern Portugal. Ophthalmologica 2010;224:389–94.
Thompson WS, Rubsamen PE, Flynn HW,Jr., Schiffman J, Cousins SW.Endophthalmitis after penetrating trauma. Risk factors and visual acuity outcomes. Ophthalmology. 1995;102:1696–701.
Al-Mezaine HS, Osman EA, Kangave D, Abu El-Asrar AM. Prognostic factors after repair of open globe injuries. J Trauma. 2010;69:943–7.
Sobaci G, Mutlu FM, Bayer A, Karagul S, Yildirim E. Deadly weapon-related open-globe injuries: outcome assessment by the ocular trauma classification system. Am J Ophthalmol. 2000;129:47–53.
Guven S, Durukan AH, Erdurman C, Kucukevcilioglu M. Prognostic factors for open-globe injuries: variables for poor visual outcome. Eye. 2019;33:392–7.
Pieramici DJ, MacCumber MW, Humayun MU, Marsh MJ, de Juan E,Jr.Open-globe injury. Update on types of injuries and visual results.Ophthalmology. 1996;103:1798–803.
Andreoli MT, Andreoli CM. Surgical rehabilitation of the open globe injury patient. Am J Ophthalmol. 2012;153:856–60.
Forrest KY, Cali JM. Epidemiology of lifetime work-related eye injuries in the U.S. population associated with one or more lost days of work. Ophthalmic Epidemiol. 2009;16:156–62.
Islam SS, Doyle EJ, Velilla A, Martin CJ, Ducatman AM. Epidemiology of compensable work-related ocular injuries and illnesses: incidence and risk factors. J Occup Environ Med. 2000;42:575–81.
Solomon C. Accidental injuries in agriculture in the UK. Occup Med. 2002;52:461–6.
Yardley AM, Hoskin AK, Hanman K, Wan SL, Mackey DA. Animal-inflicted ocular and adnexal injuries in children: a systematic review. Surv Ophthalmol. 2015;60:536–46.
Forst L, Noth IM, Lacey S, Bauer S, Skinner S, Petrea R, et al. Barriers and benefits of protective eyewear use by Latino farm workers. J Agromedicine. 2006;11:11–7.
Saari KM, Aine E. Eye injuries in agriculture. Acta Ophthalmol Suppl. 1984;161:42–51.
Bull N. Mandatory use of eye protection prevents eye injuries in the metal industry. Occup Med. 2007;57:605–6.
Lipscomb HJ. Effectiveness of interventions to prevent work-related eye injuries. Am J Prev Med. 2000;18:27–32. 4 Suppl.
Chatterjee S, Agrawal D. Primary prevention of ocular injury in agricultural workers with safety eyewear. Indian J Ophthalmol. 2017;65:859–64.
Bureau of Indian Standards, The National Standards Body of India: Bureau of Indian Standards, Ministry of Consumer Affairs, Food & Public Distribution, Government of India. https://bis.gov.in/.
Ministry of Labour and Employment Government of India. Report of the Working Group on Occupational Safety and Health for the Twelfth Five Year Plan (2012 to 2017). 2011. Accessed 27 Feb 2021. https://www.ilo.org/global/topics/safety-and-health-at-work/country-profiles/asia/india/WCMS_211795/lang--en/index.htm.
Funding
There is no funding involved in this study. AKH is supported by a National Health and Medical Research Council Dora Lush Postgraduate Research Scholarship and is an employee of Essilor. No other authors have no financial disclosures.
Author information
Authors and Affiliations
Contributions
ZHT was responsible for and contributed towards material preparation, data extraction and analysis, interpreting results, drafting of the initial manuscript and subsequent edits and updating of reference list. SMS and MS were responsible for the study conception, design as well as data collection and extraction. CHC contributed towards data extraction and analysis, creating the tables under the results section and provided feedback on the manuscript. RA and AKH provided guidance throughout data analysis, results interpretation and feedback on the manuscript. All authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Toh, Z.H., Shah, S.M., Chua, C.H. et al. International Globe and Adnexal Trauma Epidemiology Study (IGATES): Visual outcomes in open globe injuries in rural West India. Eye 37, 88–96 (2023). https://doi.org/10.1038/s41433-021-01895-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01895-2