Abstract
Purpose
To describe clinical characteristics and visual outcomes of non-traumatic open globe injuries.
Setting
A level 1 trauma centre in a large urban medical centre.
Design
Retrospective study.
Methods
Charts of non-traumatic open globe patients admitted to MHH-TMC from 1/2010 to 3/2015 were reviewed for demographics, cause, clinical characteristics, visual acuity (VA) and enucleation.
Results
Thirty eyes were included: 15 (50%) were males with a mean age of 47 (±28) years. All presented with zone 1 injury. Twenty-five (83%) had a perforated corneal ulcer. Presenting VA was count fingers (n = 3, 10%) to NLP (n = 6, 20%). Twenty-four (80%) involved infection, 5 (17%) congenital, 3 (10%) chemical burn and 2 (7%) neurotrophic. Conjunctival injection (n = 22, 77%), corneal opacification (n = 20, 71%) and relative afferent pupillary defect (n = 9, 44%) were common. After treatment, 23 (88%) were worse than 6/60 (20/200), 9 (35%) were NLP and 8 (27%) required enucleation.
Conclusions
Often non-traumatic open globe injuries are zone 1 and due to perforated infectious ulcers. Compared to previously reported traumatic injuries, these have higher rates of enucleation (27% vs 8%) and poorer final VA (88% vs 68% worse than 6/60 20/200).
Similar content being viewed by others
Introduction
Open globe injuries describe full-thickness wounds through the cornea or sclera [1, 2]. Open globe injuries and their sequelae are a significant cause of monocular vision loss and morbidity [1]. Open globes can be traumatic in nature (e.g. penetrating, projectile, blunt force trauma) or non-traumatic (e.g. infectious corneal ulcers, burns). Non-traumatic injuries may not result in immediate open globes but may be more insidious in nature. The epidemiology and characteristics of different types of traumatic open globes and the visual prognosticators of zones of injuries have been well established in the literature [3,4,5,6].
However, in literature describing open globes, often excluded are non-traumatic causes of full-thickness wounds of the globe, such as perforations from corneal ulcers, inflammatory processes or chemical burns [3,4,5]. Lekskul et al. [7] investigated non-traumatic causes of corneal perforations secondary to corneal diseases and infections; however, the study contained no patients with previous open globes, endophthalmitis, chemical burns, neurotrophic or congenital etiologies. To our knowledge, there are no studies evaluating all presenting non-traumatic causes of open globes.
Our aim is to characterize causes and predispositions of non-traumatic open globes, their presentation and visual outcome. Through this process, better understanding of causes and prognosticators may be ascertained, and possible prevention strategies may be conceived.
Methods
Study design
This is a retrospective review of patients with non-traumatic open globes who presented to the Robert Cizik Eye Clinic of the Ruiz Department of Ophthalmology and Visual Science at the McGovern Medical School at The University of Texas Health Science Center at Houston (UTHealth) and/or to Memorial Hermann Hospital Texas Medical Center from January 2010 through March 2015. Institutional Review Board approval was obtained from The University of Texas Health Science Center Committee for the Protection of Human Subjects. All research adhered to the tenets of the Declaration of Helsinki and was HIPAA compliant.
Participants
A chart review of patients of all ages was undertaken. Patients were identified by the following ICD-9/ICD-10 codes: perforated corneal ulcer (370.06/H16.07), 871.0: ocular laceration and rupture with or without prolapse of intraocular tissue or exposure of intraocular tissue (871.0 & 871.1/S05.3 & S052), rupture of eye with partial loss of intraocular tissue (871.2), unspecified laceration of eye (871.4), unspecified open wound of eyeball (871.9/S05.9) and burn with resulting rupture and destruction of eyeball (940.5/T26.2). We defined, and included, non-traumatic injuries as those that do not involve mechanical trauma causing immediate perforating or penetrating injury. Charts with traumatic aetiologies were excluded. Furthermore, those without a consultation exam and medical or surgical repair performed by the ophthalmology service were also excluded. Selected patients received a full visual exam, including of the posterior pole, per standard of care. If both eyes were eligible, one eye was randomly selected.
Data collection
Participant demographics (age, sex and race/ethnicity) and open globe characteristics including cause of injury, type of injury, zone of injury and visual acuity (VA) at presentation were obtained. The cause of injury was classified as infection, congenital, chemical burn, neurotrophic, other/unknown or a combination. Zone of injury was divided into three zones according to the following criteria: Zone 1: cornea and limbus, Zone 2: anterior 5 mm of sclera posterior to the limbus, Zone 3: posterior sclera greater than 5 mm from the limbus [1, 2]. Clinical examination findings at presentation, including relative afferent pupil defects (RAPD), chemosis, sub-conjunctival haemorrhage, abnormal pupil or iris shape, hyphema, conjunctival injection, corneal opacifications, discharge, hypopyon and culture, were recorded. Postoperative data collected included patient follow-up, duration of follow-up, and whether the injured eye required enucleation or evisceration. The VA at the last follow-up was collected as the final VA.
Data analysis
VA change from presentation to the final visit was classified into improved, remained same, remained no light perception (NLP) and worse outcome. The data were summarized by mean (±standard deviation) for continuous variables or frequency (percentage) for discrete variables. Fisher exact test was performed to identify the prognostic factors that associated with VA outcome.
A P value < 0.05 was considered as statistically significant. All statistics were computed using SAS for Windows 9.4 (SAS Inc., Cary, NC).
Results
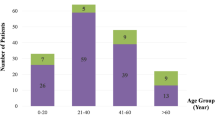
Demographics
Thirty (30) patients who had non-trauma-related open globe were included in this study. Fifteen (50%) were males with an average age of 47 (±28, range 1–90) years old. Of 26 patients with reported race/ethnicity, 8 (31%) were white, 6 (23%) black, 9 (35%) Hispanic and 3 (12%) Asian. Nine (30%) eyes had no history of ocular diseases. The 21 (70%) eyes with a history of one or more ocular diseases included: 12 corneal diseases (including Axenfelds syndrome), 5 previous ocular trauma, 4 glaucoma and 4 cataracts. Fourteen eyes (47%) had previously undergone ocular surgeries (Supplementary Table 1).
Outcomes
Table 1 contains the outcome of each patient, including whether enucleation was necessary, VA at the final visit, duration of follow-up and VA change from presentation to the final visit. Of the 30 eyes, 4 (13%) were primary enucleated. Of 23 (77%) eyes with follow-up, the average follow-up period was 4.4 months (±3.3). In addition to four primary enucleations, four eyes (13%) underwent secondary enucleation during the follow-up period, resulting in a total of eight (27%) enucleated eyes. The final VA was unknown in four eyes, with three due to loss of follow-up and one unable to be evaluated due to mental status. The final VA of the remaining 26 eyes was 4 (15%) with VA 6/60 (20/200) to 6/90 (20/300), 4 (15%) were count fingers (CF), 9 (35%) were hand motion (HM) to light perception (LP), and 35% (9/26) were NLP. Compared to initial presentation, 10 (38%) patients improved, 6 (23%) remained stable, 6 (23%) remained NLP and 4 (15%) had worse outcomes.
Presentation and clinical characteristics
All 30 (100%) patients presented with zone 1 injuries and 25 (83%) open globes were due to a perforated corneal ulcer with or without uveal prolapse. At presentation, no eyes had vision better than count fingers: 3 CF (10%), 6 HM (20%), 15 LP (50%), and 6 NLP (20%). Twenty (67%) of non-traumatic open globes were caused by infection exclusively (Fig. 1). Other causes included five (17%) with congenital predispositions, three (10%) with chemical burns, two (7%) from neurotrophic pathologies, and one (3%) that was unknown (Fig. 2). Congenital problems included keratoconus, congenital corneal hypaesthesia, congenital glaucoma, Axenfelds Syndrome, and Fuch’s dystrophy. One of the two eyes with neurotrophic pathology also had congenital predisposition. Three eyes had a combination of congenial and infectious causes, while one eye had a combination of chemical and infectious cause of open globe.
Figure 3 describes the common presenting signs (>10%) in these patients, who most frequently presented with abnormal pupil (14/17, 82%), followed by conjunctival injection (22/30, 77%) and corneal opacification (20/28, 71%). High incidence of corneal opacification often made examination of other clinical characteristics difficult. Of the 22 patients who were able to be assessed for a relative afferent pupil defect (RAPD), 9 (44%) of them had a RAPD. Discharge (7/30, 23%), chemosis (4/30, 13%) and hypopyon (3/27, 11%) occurred at substantially lower rates. One patient had 85% conjunctivalization of cornea; thus, the intraocular examination was not able to be performed. Incidences of sub-conjunctival haemorrhage and hyphema were rare (<10%).
Fifteen of 20 cultured eyes (75%) had an identifiable organism. Two (13%) were fungal and the rest 13 (87%) were bacterial. Of the 13 positive bacterial cultures, 62% (8/13) were Gram-negative rods, 31% (4/13) were Gram-positive cocci, and 8% (1/13) were unknown with unavailable outside hospital records.
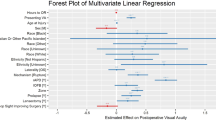
Prognostic factors
VA outcomes
VA outcomes for each ocular sign are summarized in Fig. 3. Eyes presenting with RAPD (P = 0.001) and chemosis (P = 0.047) had worse VA outcomes. Of the eight eyes with RAPD and follow-up, none (0%) had improved VA (P = 0.001): three (38%) eyes remained the same, four (50%) eyes remained NLP, and one (12%) eye worsened. VA improved in 8 of 10 (80%) eyes without a RAPD (Fig. 3). Of four chemotic eyes with known final VA, one (25%) eye remained the same VA, three (75%) eyes remained NLP, and no eyes improved or worsen. However, of 22 eyes without chemosis, 10 (45%) eyes improved, 5 (23%) eyes remained the same, 3 (14%) eyes remained NLP, and 4 (18%) eyes worsened (P = 0.047).
There were only 3 (10%) eyes with hypopyon in our cases. However, it should be noted that all 3 (100%) remained NLP. Due to insufficient statistical power, it did not reach the significance level (P = 0.095) as a prognostic factor for VA change, but it did portend an unfavourable prognosis.
VA outcome was different between eyes without culture and eyes with culture (P = 0.015). Of eight eyes without culture, none (0%) had VA improvement, two (25%) remained stable, three (38%) remained NLP, and three (38%) worsened. For 18 eyes with culture, 10 (56%) had VA improvement and 4 (22%) had worse VA outcomes. While there were no differences in VA outcome among bacterial, fungal infection and negative culture results (P = 0.71), VA improvement was observed in 46% (6/13) of bacterial infection patients and 50% (1/2) of fungal infections. Further stratification of the bacterial infections by Gram stain status, only 25% (1/4) of Gram positive improved while 50% (4/8) of Gram-negative infectious improved and all of patients with the final VA equal to better than 6/90 (20/300) in this study were Gram negative.
Enucleation
There were no baseline ocular signs associated with outcome of enucleation except presence of RAPD (P = 0.017). Four (44%) of 9 RAPD eyes underwent enucleation and none (0%) of 13 non-RAPD eyes underwent enucleation.
Six (60%) of 10 eyes who did not undergo culture either had primary (n = 2) or secondary enucleation (n = 4), while only 2 of 20 (10%) eyes who underwent culture were enucleated primarily (P = 0.007).
Discussion
Open globe injuries have long been known to be true ocular emergencies with poor visual prognosis. However, further differentiating between traumatic and non-traumatic open globes is important in prognosticating outcomes. Epidemiologically, we found non-traumatic open globes had no gender predilection but were more commonly seen in those with previous ocular disease or surgery. Clinical characteristics are also essential to the ophthalmologist in initial evaluation and understanding prognosis of open globes. Within our cohort of non-traumatic globes, we found patients with a RAPD, chemosis, or hypopyon portended a worse prognosis. The presence of these signs can assist the clinician in weighing the risks and benefits of treatment options.
Our series of non-traumatic open globe injuries consisted entirely of zone 1 injuries, with none of our patients presenting with a VA better than CF, a majority LP or NLP (70%). By contrast, Parver et al. [4], using the National Eye Trauma Registry, examined all traumatic open globe injuries from 1985 to 1991, and found that 37.8% of open globes from traumatic causes at presentation had a VA of CF or better, and 14.2% had a VA of 6/12 (20/40) or better. Sahin Atik et al. [8] and Rao et al. [9] also showed a lower prevalence of zone 1 injuries among all open globes compared to our non-traumatic globe cohort, reporting that approximately 50% of open globe injuries occurred in zone 1 [8, 9]. Examining the final VA of open globes with zone 1 injuries, Sahin Atik found that 68% of zone 1 injuries had a final VA of greater than 6/60 (20/200). Pieramici et al. [10] found that 48% of zone 1 injuries had a final VA of 6/12 (20/40) or better, 25% had a final VA of between 6/12 (20/40) and 6/240 (20/800), 20% had a vision worse than 6/240 (20/800), and 7% required enucleation. Our cohort had distinctly worse outcomes, as none of our patients had a final VA better than 6/60 (20/200) and 31% (8/26) required enucleation (primary or secondary).
This difference in outcomes is likely multi-faceted. In studies that examine zones of injury for traumatic open globes, the final VA has a progressively worse prognosis with successive zone of injury due to posterior segment involvement causing irreparable damage. The structural anatomy of the eye can be restored, but damage to the nerve layer is irreversible [11]. A majority of the injuries in these eyes are secondary to purely traumatic forces (projectiles, impalements) in which the injury would only be relegated to the point of impact or perforation. In contrast, the causes for non-traumatic open globe injuries are not simply confined to the location of the defect. An infective bacterial or fungal keratitis that leads to a perforated corneal ulcer may likely have seeded further into the eye. Surgical intervention alone may not salvage vision, and medical intervention may be too late to halt the infectious and inflammatory damage [12]. In corneal ulcers secondary to chemical burns, more than just the cornea can be affected. Alkali substances can penetrate the eye, causing ciliary body and trabecular meshwork damage leading to acute IOP rise and permanent glaucomatous damage. These substances may also cause limbal ischaemia leading to stem cell deficiency and damage to the conjunctiva causing scarring and dryness [13].
Another facet of the poor visual prognosis in our patient cohort may be related to their ocular comorbidities. Seventy percent (70%) of our patients had a pre-existing ocular disease, and 47% of our patients had undergone previous ocular surgeries (e.g. cataract extraction, penetrating keratoplasty). Prior ocular trauma or prior ocular surgery weakens the natural integrity of the eye. These potentially led to poorer outcomes from one of three mechanisms: (1) greater susceptibility to infections, (2) limited ceiling for improvement, or (3) VA may have already been partially compromised.
It is worth noting that while traumatic open globes tend to occur in males at higher rates [4], we found that non-traumatic open globes were just as likely to occur in females as males. This difference could be attributed to how causes of traumatic open globes are more frequently associated with occupational hazards in men [14], while non-traumatic globes have no such associations.
This study also evaluated the various presenting clinical signs of non-traumatic open globes for prognostic value (Supplementary Table 2 and Fig. 3). An abnormal pupil, corneal opacification, and injection were the most common findings. RAPD tended to prognosticate a poorer outcome with either worse VA outcomes or the need for enucleation and none showed improvement. Similarly, Rahman et al. [15] investigated all causes of open globes and found that not only was RAPD significantly associated with poor visual outcomes but that 48% of all open globes with a RAPD proceeded to enucleation. As in our study, globes without a RAPD did not result in enucleation. While RAPD is a non-specific sign, its presence in non-traumatic open globes may signify permanent, irreparable injury and a poor visual prognosis.
While only three (10%) hypopyon were seen in our cases, all required enucleation or remained NLP. Chemosis was also infrequently seen (13%), but similarly carried a worse visual prognosis. While hypopyon and chemosis are not discussed in great detail in the literature, we found that both portended a poor visual prognosis in our patients.
A large proportion of our cases required infectious work-up and their stratification was important in considering microbial aetiologies of open globes. Besides the study done by Lekskul et al., no other studies have looked at infectious causes of open globes. Lekskul found that 15% of their non-traumatic open globes were secondary to bacterial keratitis, with half of those having improved final VA and half having worsening VA; 8% were due to fungal keratitis, with none of their cases showing improvement.
No large-scale studies have looked at infectious causes of open globes; therefore, we extrapolated comparable information from previous studies that examined microbial keratitis. Geographical regions play a major part in the type of infectious keratitis. Shah et al. [16] showed a positive correlation (r = 0.83) between the developmental status of the country and the incidence of bacterial corneal ulcers. As our study took place in the United States, a developed nation, the cohort of open globes due to infectious causes showed a similar trend at 87% and 13% for bacterial and fungal, respectively. Furthermore, Shah found that 64% of culture positive bacterial keratitis in North America were Gram positive, while 36% were Gram negative. In contrast, our cohort had a higher proportion of Gram negative at 62% (8/13) compared to Gram positive at 31% (4/13). It is possible that Gram-negative infections progress more quickly to perforated ulcers, although no studies currently exist that compare progression to perforation of Gram-positive versus Gram-negative bacterial keratitis. Alternatively, previous studies on microbial keratitis have included trauma as a primary cause, which more often result in Gram-positive infectious aetiology. Keay et al. [17] showed that 29% of their traumatic cases resulted in Gram-positive infection while only 5% were due to Gram-negative bacteria. Further studies are needed to understand the prevalence of Gram-negative bacteria causing non-traumatic open globes.
Our study’s exclusion of traumatic cases may account for the relatively few microbial cases secondary to fungal organisms. Wong et al. [18] showed that fungal keratitis was 2.69 more likely to be associated with trauma than all bacterial keratitis was.
We examined the effect of microbial species on VA outcomes in our study. No open globe with positive fungal culture achieved a VA better than CF, though none had worsened VA once treated. In contrast, in bacterial infections half had better VA, and a third had worsened VA. The best potential for recovery was seen among Gram-negative causes. Finally, a statistically significant association was found between VA acuity and eyes that underwent culture. We hypothesize that this is due to better tailored treatment for these eyes.
In conclusion, we examine the gap in the literature of open globes secondary to non-traumatic causes, as our study shows they have extremely poor outcomes with higher proportion of NLP and enucleations. Zone 1 was always the site of the injury, infectious aetiologies found to be the primary cause, and predilection for those with prior ocular surgery and disease was seen. Male gender did not increase risk. Infectious aetiologies in our study showed a lower incidence of fungal keratitis and a higher rate of Gram-negative infections, which may be explained by the exclusion of traumatic injury. Chemical burns and infections (as well as the other aetiologies) may contribute to greater concurrent ocular morbidity beyond the point of perforation, unlike traumatic aetiologies. RAPD was an important predictor of poor visual outcome or enucleation, and while not significant, hypopyon and chemosis were seen only in eyes with worse outcomes.
To further delve into outcomes of non-traumatic globes and potential interventions, several other factors remain to be thoroughly studied—use and comparison of therapeutic interventions, aggressiveness of intervention, and medical versus surgical routes of treatment.
A limit of this study stems from its retrospective nature with limited follow-up. Furthermore, we entered the care of several patients in media res, which prevented us from having a full picture on a few patients, particularly the cultures of ongoing infections and their underlying aetiologies. While posterior pole findings were outside the scope of this study, injury to the posterior pole is often secondary to the aetiology of the non-traumatic injury or sequelae to it (e.g. infection causing perforation and affecting the back of the eye) and may be the subject of further investigations.
Another limitation of this study was the sample size of patients. These types of open globes are very rare, and while this study represents a relatively large cohort, it is still small in absolute terms, limiting the degree of analysis possible. The stratification of patients by different causes or presenting symptoms was limited to descriptive statistics.
Despite these limitations, this study importantly contributes to the literature by examining outcomes and prognosis of non-traumatic open globes.
Summary
What is known about this topic
-
Characteristics of traumatic open globes have been thoroughly studied, with demographics, zone of injury, mechanism, and prognosis well known.
-
There is no existing literature that currently characterizes non-traumatic open globe injuries, which is important in efforts to better understand prognosis and treat disease.
What this study adds
-
Non-traumatic open globe injuries do not have the same predilection for males, although they occur more frequently in those with prior ocular disease.
-
Injury is most often to the cornea and limbus and involves infection, with RAPD predicting poor final visual outcome.
-
Overall, non-traumatic causes of open globes demonstrated extremely poor visual outcomes.
References
Kuhn F, Morris R, Witherspoon CD. Birmingham Eye Trauma Terminology (BETT): terminology and classification of mechanical eye injuries. Ophthalmol Clin North Am. 2002;15:139–43.
Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Ophthalmology. 1996;103:240–3.
Mansouri M, Faghihi H, Hajizadeh F, Rasoulinejad S, Rajabi M, Tabatabaey A. et al. Epidemiology of open-globe injuries in Iran: analysis of 2,340 cases in 5 years (Report No. 1). Retina. 2009;29:1141–9.
Parver LM, Dannenberg AL, Blacklow B, Fowler CJ, Brechner RJ, Tielsch JM. Characteristics and causes of penetrating eye injuries reported to the National Eye Trauma System Registry, 1985-9. Public Health Rep. 1993;108:625–32.
Casson RJ, Walker JC, Newland HS. Four-year review of open eye injuries at the Royal Adelaide Hospital. Clin Exp Ophthalmol. 2002;30:15–18.
Fujikawa A, Mohamed YH, Kinoshita H, Matsumoto M, Uematsu M, Tsuiki E, et al. Visual outcomes and prognostic factors in open-globe injuries. BMC Ophthalmol. 2018;18:138.
Lekskul M, Fracht HU, Cohen EJ, Rapuano CJ, Laibson PR. Nontraumatic corneal perforation. Cornea. 2000;19:313–9.
Sahin Atik S, Ugurlu S, Egrilmez ED. Open globe injury: demographic and clinical features. J Craniofac Surg. 2018;29:628–31.
Rao L, Ninan A, Rao K. Descriptive study on ocular survival, visual outcome and prognostic factors in open globe injuries. Indian J Ophthalmol. 2010;58:321.
Pieramici DJ, MacCumber MW, Humayun MU, Marsh MJ, de Juan E. Open-globe Injury. Ophthalmology. 1996;103:1798–803.
Yalcin Tök O, Tok L, Eraslan E, Ozkaya D, Ornek F, Bardak Y. Prognostic factors influencing final visual acuity in open globe injuries. J Trauma. 2011;71:1794–1800.
Kent C. Winning the battle against corneal ulcers. Rev Ophthalmol. 2013. https://www.reviewofophthalmology.com/article/winning-the-battle-against-corneal-ulcers-42796. Accessed June 27, 2019.
Singh P, Tyagi M, Kumar Y, Gupta KK, Sharma PD. Ocular chemical injuries and their management. Oman J Ophthalmol. 2013;6:83–6.
Koo L, Kapadia MK, Singh RP, Sheridan R, Hatton M. Gender differences in etiology and outcome of open globe injuries. J Trauma. 2005;59:175–8.
Rahman I, Maino A, Devadason D, Leatherbarrow B. Open globe injuries: factors predictive of poor outcome. Eye. 2006;20:1336–41.
Shah A, Sachdev A, Coggon D, Hossain P. Geographic variations in microbial keratitis: an analysis of the peer-reviewed literature. Br J Ophthalmol. 2011;95:762–7.
Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K, et al. Microbial keratitis. Ophthalmology. 2006;113:109–16.
Wong TY, Ng TP, Fong KS, Tan DT. Risk factors and clinical outcomes between fungal and bacterial keratitis: a comparative study. CLAO J. 1997;23:275–81.
Funding
This work was supported in part by National Eye Institution Vision Core Grant P30EY028102 and Research to Prevent Blindness. Funding sources were not involved in collection, analysis or collection of data, or writing of this manuscript.
Author information
Authors and Affiliations
Contributions
AWG collected data and wrote first drafts of the manuscript. ELC contributed to the conception and review of the article. JZF, MLP, AZC, KR, and ELC edited subsequent drafts and revisions. AZC additionally contributed to data analysis. All authors contributed to manuscript revision, read, and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Gross, A.W., Fan, J.Z., Pfeiffer, M.L. et al. Non-traumatic open globe injuries: presenting characteristics and visual outcomes. Eye 36, 2323–2327 (2022). https://doi.org/10.1038/s41433-021-01869-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01869-4