Abstract
The aim of this review was to discuss frequently encountered themes such as cataract surgery in presence of age-related macular degeneration (AMD), dementia, Immediate Sequential Bilateral Cataract Surgery (ISBCS), discussing non-standard intraocular lens (IOL) options during consultation in the National Health Services (NHS) and the choice of the biometric formulae based on axial length. Individual groups of authors worked independently on each topic. We found that cataract surgery does improve visual acuity in AMD patients but the need for cataract surgery should be individualised. In patients with dementia, cataract surgery should be considered ‘sooner rather than later’ as progression may prevent individuals presenting for surgery. This should be planned after discussion of patients’ best interests with any carers; multifocal IOLs are not proven to be the best option in these patients. ISBCS gives comparable outcomes to delayed sequential surgeries with a low risk of bilateral endophthalmitis and it can be cost-saving and efficient. Patients are entitled to know all suitable IOL options that can improve their quality of life. Deliberately withholding this information or pressuring patients to choose a non-standard IOL is inappropriate. However, one should be mindful of the not spending inappropriate amounts of time discussing these in the NHS setting which may affect care of other NHS patients. Evidence suggests Hoffer Q, Haigis, Hill-RBF and Kane formulae for shorter eyes; Barrett Universal II (BU II), Holladay II, Haigis and Kane formulae for longer eyes and BU II, Hill-RBF and Kane formulae for medium axial length eyes.
摘要
本文旨在探讨在合并年龄相关性黄斑变性 (age-related macular degeneration, AMD)、 痴呆进行白内障手术以及即刻连续性双侧白内障手术(Immediate Sequential Bilateral Cataract Surgery, ISBCS)时存在的一些问题, 讨论在国家医疗服务制度 (National Health Services, NHS) 和基于生物轴向长度公式计算眼内人工晶体的选择。每组作者针对每个话题进行独立工作。我们发现, 白内障手术确实能提高AMD患者的视力, 但是否需要行白内障手术应因人而异。对于痴呆患者, 白内障手术应该被认为“更早而不是晚”, 因为病情进展可能会妨碍患者接受手术。这应在与医疗人员讨论病人的最大利益后进行安排和计划;尚未证明多焦IOLs是这些患者的最佳选择。与延迟连续手术相比, ISBCS双侧眼内炎的风险较低, 并且其成本更低及高效。患者有权获知所有可以改善其生活质量的合适的IOL选择方面的信息, 故意隐瞒这些信息或强迫患者选择非标准IOL是不妥的。然而, 在NHS系统中人们应该注意不要花过多的时间讨论这些, 因为这可能会影响NHS其他患者的护理。证据表明Hoffer Q、Haigis、Hill-RBF和Kane公式适用于眼轴较短的眼;较长眼轴的眼使用Barrett Universal II (BU II)、Holladay II、Haigis和Kane公式, 中等眼轴的眼使用BU II、Hill-RBF和Kane公式。
Similar content being viewed by others
Introduction
Cataract surgery is the commonest surgery performed in the National Health Services (NHS) in the United Kingdom. The protocols for preassessment and the criteria for listing the patients vary from region to region and from one Care Commissioning Group (CCG) to other. It is also predicted that the workload of cataract surgery is going to increase over the coming decade. As the demand increases the need to streamline and standardise the delivery of cataract surgery also increases.
A typical cataract surgery patient pathway consists of a detailed preoperative assessment with a nurse and a doctor for consenting followed by intraocular lens (IOL) power selection on the day of the surgery from the available biometry before they are seen for a postoperative follow up in the NHS clinics and/or by the community optometrists for glasses. There are some recurring and frequently encountered situations during a typical cataract patient pathway in the United Kingdom which can have more than one valid opinion on management and are subject to the surgeon’s experience/perception with these situations. Some of these issues encountered during the preoperative assessment and consenting process include co-existing macular degeneration, dementia, immediate sequential bilateral cataract surgeries (ISBCS) and discussion on the non-standard IOL options during NHS consultations. Prior to surgery surgeons may have differing opinions on the choice of IOL power calculation formulas based on the axial length. Literature in the field of biometric formulae is evolving rapidly with the advent of newer generation formulae.
In this review individual groups of authors discuss some of these frequently encountered themes such as cataract surgery in the presence of age-related macular degeneration, dementia, eligibility of ISBCS, discussing non-standard IOL options during NHS consultation and updates on the newer biometric formulae based on axial length.
Cataract surgery in patients with age-related macular degeneration
Advanced age-related macular degeneration (AMD) and cataract are common causes of visual impairment affecting the elderly across the world [1]. The chronology of these conditions has been a matter of controversy. Whilst macular pathology due to AMD may be first visualised only after cataract surgery, these conditions usually co-exist in various severity levels. Phototoxicity and dysfunction of inflammatory cascade have been implicated in the aetiopathogenesis of both disorders, but questions remain with regards to how cataract surgery and AMD are interlinked [2,3,4,5,6]. Although cataract surgery is effective in improving visual acuity and quality of life in most patients, ocular morbidities such as AMD are predictors of poor visual outcomes [7].
Various studies have evaluated the effects of cataract surgery on early AMD, advanced AMD and neovascular AMD. A recent Cochrane review could not draw reliable conclusions on whether cataract surgery was beneficial or harmful in patients with dry AMD after 1 year. The review concluded that cataract surgery provides short term (6 months) improvement in visual acuity (VA) in eyes with AMD compared with no surgery and it is unclear whether timing of surgery has any effect on long-term outcomes [8]. The Age-related Eye Disease Study (AREDS) report 27 showed significant visual gains after cataract surgery across all AMD severity groups [5]. The mean gain of VA in AREDS cohort was 6 letters in the mild AMD group, 4 letters in the moderate AMD and 2 letters in the advanced AMD group. A more recent AREDS2 study found results similar to report 27 and concluded improved visual outcomes in eyes with AMD after cataract surgery [9]. Another review highlighting the effect of cataract surgery on AMD progression concluded that cataract removal results in improved visual acuity, no significant AMD progression and better quality of life [10].
There is conflicting evidence regarding the timing of surgery and VA outcomes in eyes with neovascular AMD (nAMD). In the AREDS study, VA gains were less in the nAMD eyes compared to early AMD groups. In a retrospective analysis of ANCHOR (Anti-VEGF antibody for treatment of predominantly Classic choroidal Neovascularization in AMD) and MARINA (Minimally Classic/occult Trial of the Anti-VEGF antibody Ranibizumab in the treatment of Neovascular AMD) trials noted a 2 line improvement from pre-operative VA at 3 months following surgery [3]. Kessel et al. and Lee et al. reported a mean improvement of 7 letters and 15 letters respectively in nAMD eyes, 6 months after surgery [6, 11]. However, 7% of patients in the Lee study lost almost 3 lines following surgery. The Fight Retinal Blindness! (FRB!) Project also reported loss of VA in eyes that were operated within 6 months of initiating intravitreal therapy, however a mean gain of 2 lines were recorded 12 months after surgery in the same cohort [12]. In addition, increased risks of post-operative complications such as posterior capsule rupture and endophthalmitis have been noted in eyes with nAMD on intravitreal therapy undergoing cataract surgery [13, 14].
Reactivation of existing neovascular membrane secondary to iatrogenic inflammation has also been reported [15]. The longer the eye with neovascular complex is quiescent before cataract surgery, the less likely it is to activate [6]. The Fight Retinal Blindness Project reported that the proportion of visits at which the CNV lesion was graded as active was similar before and after the cataract operation in the nAMD group. However, relatively greater CNV activity was observed in eyes with nAMD that underwent cataract surgery than not and the authors related this finding to probable pro-inflammatory cytokine release following cataract surgery [12]. There seems to be an advantage of having a pre-operative exudation free period prior to cataract surgery or anti VEGF injections may be given at the time of cataract surgery to improve VA outcomes [6, 16]. The course of nAMD and frequency of intravitreal injections required are not influenced by undergoing cataract operation [11, 12].
Limited data is available on the result of cataract operation in eyes with disciform scars secondary to nAMD. Yorgun et al. studied the effect of cataract surgery on 23 eyes with disciform scars and compared them with 36 control eyes. The duration of stable period of disease and mean number of anti-VEGF injections received prior to stable period were similar in both groups [17]. A definite improvement in visual acuity was observed following cataract removal in eyes with disciform scars but this improvement was not sustained in the long-term.
To conclude, cataract surgery improves visual acuity across all grades of AMD severity at least in the short-term. There is minimal evidence to support worsening of AMD following cataract removal. It is preferable to delay cataract surgery by 6 months or more from the date of initiation of anti-VEGF and when the neovascular complex has been quiescent. However, the timing of surgery needs to be individualized for each patient after considering the macula status and assessing the patient’s needs.
Cataract surgery in patients with dementia
People living with dementia cite loss of personal autonomy as one of their major fears of the disease process and loss of vision is a significant part of this process [18]. Poor vision is also a significant contributor to falls with subsequent associated morbidity and mortality in this cohort of patients [19]. Visual morbidity in people living with dementia can be attributed to diseases of the eye, the dementia itself or concurrent other pathologies such as stroke. Dementia is usually categorised by the underlying pathology of which Alzheimer’s disease, vascular dementia or a combination of both account for 80% with rarer causes such as Lewy Body disease, dementia associated with Parkinson’s, traumatic brain injury and posterior cortical atrophy accounting for the remainder [20].
There are 3 main areas of note in the provision of cataract surgery in people living with dementia:
-
Why are people living with dementia having less cataract surgery than their peers?
-
Should they be offered general anaesthesia with immediate sequential bilateral cataract surgery (ISBCS)?
-
Would they benefit from multifocal implants?
People living with dementia have reduced levels of cataract surgery
In the UK we perform ~400,000 cataract surgery procedures annually and the majority of these are performed in the >65 age group [21]. Dementia is present in 7.1% of the >65 age group rising to 25% in the >85 age group [22].
The PrOVIDe study sponsored by NIHR demonstrated that 32.5% of people living with dementia had binocular visual acuity worse than 6/12 [23]. Over 50% of the correctable visual morbidity in this study was due to refractive error and wearing the correct spectacles would improve the vision to better than 6/12. Of the remainder, 48% of people whose vision could not be improved by new glasses had unoperated cataracts. As the population ages the number of people living with dementia who also have cataracts is only going to increase and become a more important part of our surgical workload. The question then arises as to why people with dementia have such a large amount of uncorrected visual morbidity? It is proposed that this is due to multiple issues such as failure of the individual to report their symptoms, failure of carers to signpost their disability, failure of eye care professionals to identify the visual morbidity or to attribute this to the dementia rather than the visual pathway [23].
People with dementia attending a cataract service present some unique dilemmas which will require modification of our pathways. Their ability to convey their symptoms may well not correlate well with their level of morbidity and their abilities to do so may fluctuate from day to day due to the presence of dementia. This requires flexibility from the entire team of eye care practitioners managing the consultation from providing extended consultations, quiet spaces in the waiting areas and clinical acumen in the decision as to whether to offer cataract surgery.
Should people living with Dementia have general anaesthesia and/or ISBCS?
There have been anecdotal reports that patients have worse dementia after general anaesthesia, and this has sometimes led to people with dementia being denied cataract surgery if they are unable to tolerate local anaesthesia. Post-operative cognitive dysfunction (POCD) has been reported to occur in up to 25% of surgical procedures [24]. However, these studies have been in cardiac surgery. The causes of POCD in cardiac surgery are multifactorial and the use of cardiopulmonary bypass has often been cited as the major contributor to the problem. However, evidence is accumulating that off-pump cardiac surgery produces a similar effect on neuropsychological performance to that with the use of cardiopulmonary bypass [25].
POCD has recently been analysed in non-cardiac surgery [26]. This study demonstrated in cataract surgery the incidence is similar between general and local anaesthesia and not as high as in invasive cardiac surgery. Any occurrences of POCD in cataract surgery are usually attributable to age >85 years rather than dementia. For this reason, we should now not refuse general anaesthesia for people living with dementia requiring cataract surgery due to the risks of POCD and the possibility of POCD explained in the consent process with the patient, their carers and the anaesthetic team looking after them. However, there are risks of general anaesthesia in this demographic of patients and if there is bilateral cataract, ISBCS reduces these risks by eliminating the need for a second anaesthetic. Recently National Institute of Clinical Excellence (NICE) and the Royal College of Ophthalmologists have recommended that “ISBCS” should be considered for people who are at low risk of operative and postoperative complications [27, 28]. However, it is important that the potential benefits and harms of ISBCS are fully discussed with patients and their carers pre-operatively. It therefore seems good practice in the author’s (PGU) opinion that when general anaesthesia is required for cataract surgery in people living with dementia that ISBCS should be considered and discussed with the patient and their carers. This also indicated the advantage of early cataract surgery in people living with dementia as it can be undertaken with LA which removes the risks of GA in more advanced disease.
Should we offer multifocal implants to people living with dementia?
Problems with wearing glasses is one of the major reasons for visual morbidity for people living with dementia [23]. This is due to multiple factors including: incorrect spectacle prescription, confusing distance and reading glasses or inability to cooperate with spectacle wearing. Cataract surgery presents an ideal opportunity to correct this by eliminating refractive error. The majority of clinicians aim for emmetropia following surgery with reading spectacles for near tasks. In people with severe dementia i.e., housebound, it is the author’s (PGU) current practice to offer mild myopia (−1D) as near tasks without spectacles such as feeding are predominant and due to the lack of walking, the risk of falls is lower.
Multifocal implants could be utilised to eliminate entirely the need for spectacles. At present there are no published studies we are aware of to determine the risks and benefits in this cohort of patients. There are some publications which could aid in the decision process as to whether to offer multifocal implants. Multifocality relies on neuroadaption to provide clear simultaneous distance and near vision. Functional MRI studies have demonstrated the plasticity required in higher cortical visual areas during the neuroadaption phase after multifocal implantation [29]. People with dementia demonstrate loss of function in these areas of the visual pathway and surrounding areas notably the increased prevalence of eye movement disorders such as phorias [30]. Also, multifocal implants are relatively contraindicated in patients with retinal pathology such as diabetic retinopathy and age-related macular degeneration and there is evidence that the dementia process involves the neural structures in the retina and affects retinal and visual performance [31]. It seem that for these reasons that in the author’s opinion (PGU) the benefits of using a multifocal IOL in people with dementia are unknown and the possible side effects outweigh these potential benefits during the lifetime of the person concerned and may not be used until definitive studies show their safety.
Immediate sequential bilateral cataract surgery
Immediate sequential bilateral cataract surgery (ISBCS) has become more common with surveys in 2018/2019 indicating 67% of ophthalmic surgeons across Europe [32] and 86% in the US [33] practice ISBCS. However, incorporating ISBCS is subject to debate [34,35,36], particularly with regards to occurrence of bilateral sight-threatening complications. This mini-review highlights benefits and potential disadvantages of ISBCS.
Clinical outcomes
Three randomized controlled trials (RCT) have compared ISBCS and delayed sequential bilateral cataract surgery (DSBCS) [37,38,39]. The largest [39] comprising 1614 eyes, found no differences in visual acuity or complications between the two groups at 30 days or self-perceived visual function at 1 year. Similar findings were reported in an RCT of 504 patients [38], with patient satisfaction, complication rates and refractive outcomes being similar at 1 month and in a smaller RCT in 96 patients [37] with similar visual function in both groups at 4 months. As expected, a meta-analysis of these RCTs [40] found no differences in visual or refractive outcomes between ISBCS and DSBCS, with poor quality of evidence. Similar equality of outcomes was demonstrated in a second meta-analysis [41], which found both approaches improved patients’ quality of life (QOL) and visual acuity. With regards to non-randomized studies, an investigation in 220 patients [42] found visual acuities, stereopsis and contrast sensitivity to be comparable, although at 4 months self-perceived visual function remained higher with ISBCS. Similarly, a non-randomized prospective study of 84 patients reported no differences in clinical outcomes [43], as did a retrospective comparative study of 3561 ISBCS and 13 711 DSBCS cases [44]. It seems likely therefore that although further high quality RCTs are indicated, clinical outcomes are similar for ISBCS and DSBCS.
Quality of life
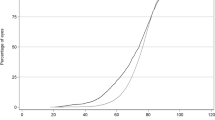
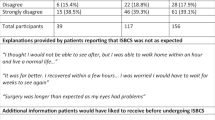
It is known that in DSBCS, cataract surgery on the second eye has a positive impact on QOL [37, 45,46,47,48,49], with one RCT of 208 patients who had expedited second eye cataract surgery compared to routine waiting times, reporting better QOL scores in the expedited group [49]. Indeed, in one RCT comparing ISBCS versus DSBCS [37], it was documented, that DSBCS patients while waiting for their second eye cataract surgery had significantly poorer contrast sensitivity, greater difficulties with performing daily activities and lower QOL scores compared to ISBCS patients. Interestingly, in a prospective observational questionnaire study of DSBCS, 45% of patients reported their second eye operation, which took place within 6 months of the first, to be more painful or of longer duration, compared to 13.5% reporting this to be the case in their first eye [45]. It appears that delay in second eye CS can impact patient satisfaction, offering some advantages to ISBCS, although further studies are required to elucidate this.
Refractive outcomes
Survey studies of US and European ophthalmologists found that the risk of implanting the incorrect IOL resulting in bilateral refractive surprise is one reason why some ophthalmologists do not perform ISBCS [32, 33]. Modern biometry hardware and IOL power calculation formulae enable a high degree of accuracy with regards to targeting post-operative refractive outcomes, with a Royal College of Ophthalmologist (RCOphth) audit of 8943 eyes finding that post-operative refraction was within 1 dioptre (D) and 0.5D of the target refraction in 89% and 62% of cases, respectively [46]. The use of the first eye refraction to guide selection of IOL in the second eye is controversial. Jabbour et al. [50] and Landers and Goggins [51] in studies suggested that each eye of an individual patient should be considered independently. Conversely, a large patient cohort study (n = 2129) found that applying a 50% correction factor to second eyes of patients improved refractive outcomes [52], which was similar to findings reported by Covert et al. [53]. With regards to comparative studies, the refractive outcomes of patients undergoing ISBCS appear to be comparable to patients undergoing DSBCS. In the RCT by Sarikkola et al. [38], refraction was within ±1.00D of the target spherical equivalent (SE) in 91.0% in the ISBCS group and 90.3% in the DSBCS group, while in a recent retrospective review of 1235 patients undergoing ISBCS, 92.05% of eyes were within ±0.5D of the target post-operative refraction [54]. It seems that with accurate biometric assessment and appropriate patient selection a high degree of refractive targeting in ISBCS can be achieved, although further comparative studies are indicated.
Endophthalmitis
Post-operative CS endophthalmitis is a devastating sight-threatening complication. The widespread use of intracameral antibiotics in CS has reduced this risk, with a reported rate of 0.029% in a cohort of 464,996 cases [55,56,57]. To date, there have been five reported cases of bilateral endophthalmitis following ISBCS [55, 58,59,60,61]. A review of the first four cases [55, 58,59,60] by Arshinoff [62] found each case to breach aseptic protocol, whereas limited information was available in the most recent case [61]. In the three RCTs comparing ISBCS and DSBCS [37,38,39] there were no reported cases of either unilateral or bilateral endophthalmitis in either group and none of toxic anterior segment syndrome. Similarly, in a cohort of 95,606 ISBCS cases, Arshinoff and Bastianelli [63] reported no cases of bilateral endophthalmitis and neither did Ganesh et al. [54] in a cohort of 1235 patients. Interestingly, in a recent study of 2687 cases (5374 eyes) undergoing DSBSC, where the second eye CS was performed within 5 days of the first eye surgery, there were five cases of unilateral endophthalmitis [63], with in each case the affected eyes being the first and occurring after CS of the second eye. It appears that with the use of intra-operative intracameral antibiotics and adherence to rigid aseptic protocol bilateral endophthalmitis following ISBCS in very rare, although vigilance and thorough analysis of further reported cases is essential.
Cost-effectiveness
Published evidence indicates that ISBCS is more cost effective than DSBCS in terms of medical facility costs and for patients themselves. In a non-randomized cohort study, ISBCS patients were found to have significantly less distance and travel times, fewer hospital visits and less time for visual recovery compared to the DSBCS [43]. A cost-analysis study by Lundstrom et al. [64] found DSBCS to be 14% more expensive than ISBCS, while a further cost-effectiveness analysis study found that compared to DSBCS, the cost-effectiveness of ISBCS was calculated to be $1431 per QALY gained [65]. O’Brien et al. [66] and Leiva et al. [67] found lower average hospital costs in patients undergoing ISBCS compared to DSBCS. However, lower physician imbursement rates for ISBCS, which include an automatic discounting by medical insurance companies of second eye surgery in ISBCS, can negatively impact the income of ophthalmologists in the private sector, with a cost analysis study in the US estimating a net loss of $19,900 to $91,700 (base case) when transitioning to ISBCS from DSCBS [68]. This negative financial impact of ISBCS in the private sector (and in some public health care settings) is likely to be acting as a deterrent for its utilization negating any potential cost-efficiency advantages to both patients and medical facilities and needs further investigation with adequate second eye remuneration.
Surgical productivity
With increasing population growth, population age, patient expectations and rates of chronic disease associated with cataracts, the demand for cataract surgery is escalating [69]. To meet this need, the efficient use of the operating room (OR) is essential. A recent Time and Motion study (TMS) of cataract surgery in the NHS indicated that adjusting workload and staff numbers and tasks could potentially double surgical productivity [70]. A follow-up study by the same authors re-modelled their TMS data as hypothetical ISBCS cases [71] and postulated that by reducing patient preparation and transfer time in the OR with ISBCS, an average 16% reduction in the time taken for 2 cataract surgery was possible, allowing for increased case numbers to be undertaken per operating list. Clinical real-world studies based on such models are indicated but the routine introduction of ISBCS into the public health sector has potential to improve the productivity of cataract surgery.
Case selection
The current RCOphth national guidelines advises that ISBCS can be considered in suitable cases, with appropriate counselling of patients [72]. Pre-defined protocols to select ISBCS cases are essential, with suggested ideal patient groups including vulnerable adults, patients reliant on hospital transport, and working patients who require faster visual rehabilitation [35, 36, 73]. Selecting technically straightforward and not high risk cases is advised in order to reduce both intra- and post-operative risks and ensure good clinical outcomes [36, 73]. Senior grade surgeons are generally better placed to perform more efficient ISBCS surgery and reduce the risk of complications [73]. In fact in a recent study by Aaronson et al. [74] paper, the authors clearly show that even with improvements in surgical teaching complication rates are consistently lower with senior surgeons. This is, of course, not to say that with proper supervision and training that complication rates in trainee surgeons cannot be minimized but this is not the subject of the current review.
Based on current evidence, ISBCS is a viable alternative to DSBCS. The clinical and refractive outcomes appear to be comparable, with a very low risk of post-operative bilateral endophthalmitis. The associated hospital and patient-related costs are lower in ISBCS, and it may offer efficiencies in surgical productivity. The meticulous selection and preparation of appropriate cases for ISBCS is essential in minimizing risks and ensuring positive clinical outcomes.
The ethical dilemma of discussing non-standards intraocular lenses within the National Health Service setting
In the vast majority of cases with visually significant cataract, a standard monofocal IOL will suffice for them and give them the visual rehabilitation they desire. As part of our standard clinical practice, we need to manage their expectations and give patients a realistic understanding of their likely visual outcome. Part of that outcome is the necessity to wear spectacles postoperatively and the visual quality they will achieve with and without correction. To obtain true informed consent, the patient needs to understand the nature of their likely post-operative vision so they can weigh the risks against the potential benefits. As emphasis on patient choice within the NHS grows it is recognised that patients are entitled to choose freely between NHS and private treatment. There has been much debate concerning the ethical and legal implications of blurring the boundaries between NHS and private care.
The benefits of removing a visually significant cataract and replacing it with a monofocal IOL are clear, but there are other non-standard IOLs available which can correct astigmatism and give some degree of spectacle independence. In the post Montgomery [75] era we have refocussed on patient autonomy and the need for patients to be given all available information to make informed choices for their care. The paternalistic approach of deciding what is best for our patients and making assumptions regarding what is and is not important for them has been rightly consigned to history. We can no longer decide unilaterally that a patient will or will not desire some degree of spectacle independence or removal of their astigmatism so they can have clear unaided vision for distance.
There are only a limited number of NHS trust in the UK who are allowed to offer the choice of toric monofocal IOLs for the patients who meet the local Trust’s eligibility criteria. Until non-standard IOLs such as toric and multifocal IOLs are routinely available across the NHS we are faced with an ethical dilemma regarding whether we should broach the subject of these IOLs with patients when we are aware that they may be only available on a private basis. It is our responsibility to ensure that we inform the patient fully about the choices of IOLs based on their visual demand, but we must not act like a salesperson and try to persuade the patient to have a private procedure in order to utilise IOLs that may not be available on the NHS. These scenarios can be fraught with a significant conflict of interests and as physicians we should guard against this in the patient’s best interests. There have been numerous complaints regarding this issue but so far none have yet reached the courts.
General recommendations can be outlined below:
-
1.
We must establish ourselves that the potential IOL we seek to discuss with a patient is indeed in their best interest. There is evidence to support the use of toric IOLs to reduce post-operative astigmatism [76,77,78] however this only refers to the benefit in being less spectacle dependant for a specific distance (usually far vision). Whether this is desirable for the patient should be elucidated from questioning about visual needs. The argument for multifocal IOLs is less clear [79] as there can be significant detriment which is not the case with a successful toric IOL. Multifocals can cause reduction in contrast sensitivity, light energy loss and dysphotopsia which can be extremely troubling for some patients and this may influence the surgeon’s perception on the suitability of multifocal IOLs for their patients.
-
2.
Deliberately withholding information about a procedure (and in this case an IOL) which may improve a specific patient’s quality of life is unethical, however, vision is an emotive issue and patients may garner, intentionally or unintentionally, the perception that if they pay out money for a “premium” IOL they will achieve premium vision which is not always the case. We must ensure that patients are not pressured in any way into pursuing private care and are clear that paying for a procedure with premium IOL does not necessarily mean a “better” IOL. Using terms such as “premium” IOLs can be misleading and should be avoided when talking to patients. Guidance from the British Medical Association [80] is clear: “If treatment is only available privately, patients should be told that upfront. Patients are generally aware of the availability of private treatment and so the option is always open to them to enquire, but where there is a new treatment available that is not provided on the NHS, patients cannot be expected to know about it. Therefore, it is appropriate to provide balanced and factual information about the treatment, although this needs careful handling to ensure the patient or the family do not feel pressure to choose the private option.”
-
3.
It would be inappropriate to spend significant time within the NHS setting discussing private options as that would compromise the care of other NHS patients however if a patient asks a direct question regarding private options, they should be furnished with the appropriate facts so they can consider the options before them. Exactly how this is done should be carefully managed to avoid allegations of trying to coerce patients into private care or wasting NHS time promoting private practice. In many cases the patients themselves may initiate the conversation regarding private care and if that is the case it should be clearly documented. NHS Employers have published a code of conduct for private practice [81] which states:
“2.9 In the course of their NHS duties and responsibilities consultants should not initiate discussions about providing private services for NHS patients, nor should they ask other NHS staff to initiate such discussions on their behalf.
2.10 Where an NHS patient seeks information about the availability of, or waiting times for, NHS and/or private services, consultants should ensure that any information provided by them, is accurate and up-to-date and conforms with any local guidelines.”
-
4.
If a clinician believes that the patient would benefit from an alternative treatment not available on the NHS it is reasonable to inform the patient of this option and encourage them to explore it further if they wish through private means. In practise, as a part of partnership approach, this means trying to determine the patients’ needs using clinical acumen but without making judgements or assumptions. For example, if a patient has a keratometric astigmatism of 1D then it may be possible to address this quite easily with appropriate incision position or a limbal relaxing incision. If a similar patient has 3D of keratometric astigmatism, then the likelihood is that they will be left with visually significant residual astigmatism and therefore a brief discussion regarding the benefits of toric IOLs is ethically appropriate.
-
5.
The ethical position regarding multifocal IOLs is less clear cut. On the face of it achieving spectacle independence for all distances is desirable for most patients however current technology does not deliver this without some compromises. The NICE guidance [28] states that we should not offer multifocal intraocular lenses for people having cataract surgery but does not elaborate on the reasoning for this conclusion. It is up to the surgeon to use their clinical judgement based on individual patients wishes and circumstances when considering whether to raise such issues with patients.
-
6.
It is inappropriate to deny patient’s choice and surgeons should not make decisions based on perceived willingness or affordability to decide whether to mention other treatment options. Decisions about what information to provide to a patient must be guided by the needs and preferences of the individual. If a treatment is considered to be clinically appropriate, then whether or not the treatment is funded by the NHS should not be the deciding factor in whether the treatment is recommended to the patient. The GMCs Guidance on consent [82] states that you should discuss “…any treatments that you believe have greater potential benefit for the patient than those you or your organisation can offer”. Furthermore, it clearly states that you should not make assumptions about the information, “a-a patient might want or need, b-the clinical or other factors a patient might consider significant, or c-a patient’s level of knowledge or understanding of what is proposed.”
-
7.
We must provide patients with enough information to make an informed choice. If there is a genuine belief that a patient would benefit from a different intervention such as a toric or multifocal IOL then that should be mentioned to them so they can make an informed choice as to whether to explore the option further or discount it. Extreme care must be taken not to pressurise a patient into non-NHS care. Similarly, spending NHS time and resources on discussions on private care are inappropriate. Documentation should be clear as to what was discussed and the fact that the patient was given appropriate information but asked to investigate their options further outside the NHS clinic if they are interested.
Despite all our precautions we will inevitably be faced with patients who complain because they were not offered a specific lens option whereas others who do proceed with a non-NHS lens with a less than ideal outcome will complain that they were pressured into their private care. This is often because busy surgeons may not consciously be aware of how their well-intentioned guidance on options outside the NHS may be perceived by certain patients, and on the other hand they may forget to explain these options especially when there may be very little time to discuss all options in many busy clinical settings. Only through strict adherence to guidance, appropriate documentation, and engaging with the patient can we protect ourselves and our patients.
Choice of intraocular lens calculation formulas for short, long and medium axial length
Intraocular lens calculation methods have evolved significantly with development of the newer generation of formulae. According to the guideline of The Royal College of Ophthalmologists published in 2010, postoperative refraction outcomes within ±1.00D of the target refraction in 85% of cases is achievable [72]. With improved accuracy of IOL power calculation formulae this benchmark is likely to change since more recent studies have published promising outcomes with up to 77.9% of eyes within ±0.50D and 96.6% of eyes within ±1.00D of refractive prediction [83].
The 1st and 2nd generation formulae are no longer recommended, and their inferiority is already established for short and long eyes [72, 84, 85]. Third generation formulae, such as Holladay 1, Hoffer Q, and SRK-T attempt to predict the estimated lens position (ELP) using axial length (AL), corneal curvature (K), and A constant as variables. The inability to accurately predict pseudophakic anterior chamber depth (ACD) and hence post-operative ELP remains a major obstacle to accurate calculation in some of these formulae [86]. It has been shown that errors in the prediction of post-operative ACD might account for up to 20 to 42% of the total refractive prediction error of an IOL calculation formula [87, 88]. A recent study demonstrated that ACD changes following phacoemulsification were not consistent in different axial lengths. Pseudophakic ACD enhancement is more remarkable in the eyes with short AL and shallow AC compared to the eyes with long AL and deep AC [89]. Therefore, accurate prediction of pseudophakic ACD is essential for an accurate IOL power calculation. The 4th and 5th generation formulae take into account ACD and more biometric parameters to predict the IOL power with greater accuracy [90]. Haigis, Holladay 2, Barrett Universal II, Hill-RBF, Olsen and Kane formulae are examples of the 4th and 5th generation formulae.
As the latest guidelines published by the RCOphth was a decade ago, it is vital to have an update on the accuracy of newer formulae based on the axial length of the eye. The updates on the accuracy of the IOL calculation formulae in predicting IOL power in eyes with different axial lengths are discussed below.
Short eyes
In the literature short eyes are referred to the eyes with AL less than 22 mm [90,91,92,93,94,95,96]. To highlight the importance of accurate post-operative refractive prediction it should be mentioned that patients of this group tend to have lens extraction earlier in life for the risk of angle closure glaucoma or refractive purposes. In fact, clear lens extraction with IOL insertion is becoming the refractive procedure of choice in patients with high hyperopia [97] as phakic IOL and laser refractive surgery are relatively contraindicated in this group due to endothelial cell loss in the first and high risk of regression [98, 99] and pseudokeratectasia [97] in the latter. Nevertheless, the short eyes pose the highest challenge in terms of refractive outcome. In actual fact, the prediction error increases with increasing hyperopia [96]. As higher IOL powers are needed for emmetropia in eyes with shorter axial length, any inaccuracy in the ELP has an exaggerated effect [96]. Moreover, the IOLs with optical power above +30D are less likely to be available in +0.50D increments compared to the IOLs below +30D of power [94]. And finally, their post-operative ACD tends to be significantly different from the pre-operative ACD as mentioned above [89], signifying the importance of accurate ACD measurement in this group.
The commonly used SRK-T formula predicts postoperative ACD as a function of corneal curvature and axial length, together with the IOL A-constant [97]. However, Hoffer Q formula relies on personalized ACD, AL, and K for the estimation of post-operative ELP [95]. Hence, Hoffer Q has been proved more accurate than the SRK-T formula in short eyes according to some studies [100,101,102]. Haigis formula, on the other hand, calculates the ELP using measurements of ACD and AL. Thus, the accuracy of the Hoffer Q and Haigis formulae in eyes with short AL may differ according to the ACD, even in presence of same Ks and AL [95]. Some studies found no statistically significant difference between these formulae [92, 96, 101]. However, other studies found Haigis having significantly smaller mean absolute error (MAE) compared to Hoffer Q, Holladay 1 and SRK-T in short eyes [93, 97]. Using this formula, 72% and 93% of eyes achieved refractive outcome within ±0.50D and ±1.00D of target refraction respectively [93]. Eom et al. [95] in 2013 assessed the accuracy of Haigis and Hoffer Q in 75 patients with short eyes. They did not find a significant difference between these formulae in eyes with ACD >2.40 mm. However, Haigis proved more accurate in eyes with ACD <2.40 mm. This emphasises the important role of ACD in IOL power calculation.
With evolution of the 4th and 5th generation formulae more comparative studies were conducted to assess the accuracy of these formulae in short eyes.
Barrett Universal II (BU II) includes lens thickness (LT) and white-to-white (WTW) measurements in addition to AL, Ks and ACD to calculate the IOL power. In comparison with SRK-T, SRK II and Olsen it showed more accurate refractive prediction in 53 short eyes [84]. It also showed the least number of refractive surprise (refractive outcome beyond ±1.00D) when compared with Holladay II, SRK-T, Hoffer Q, and Hill-RBF in a study with small sample size of 21 [103]. However, Gokce et al. found no significant difference between Hoffer Q, Holladay I and II, Olsen, Haigis, and Barrett Universal II formulae among 67 short eyes and Connell and Kane found no superiority between Kane, Olsen, Hill-RBF, Holladay I and II, SRK-T, Hoffer Q, Haigis and Barrett Universal II formulae among 46 eyes with short AL [83, 104].
Kane formula was introduced in 2018. In addition to AL, Ks and ACD it uses patient’s gender, central corneal thickness (CCT) and LT to calculate the IOL power. Darcey et al. reported superiority of this formula in accurate prediction of IOL power in 766 hyperopic eyes compared to Hill RBF, BU II, Haigis, SRK-T, Holladay 2, Hoffer Q and Olsen [105]. More recently another study on 182 eyes with extreme hyperopia and IOL power ≥ +30D reported that Kane formula had statistically significant lower MAE compared to Hill-RBF, Holladay I and II, Haigis, BU II, SRK/T Hoffer Q and Olsen formulae [106].
In summary, various studies have demonstrated suitability of Haigis and Hoffer Q formulae in IOL calculation in short eyes. Newer formulae like Hill-RBF, Holladay 2, and BU II have demonstrated as accurate in other studies and Kane formula has reported better outcome compared to all previous formulae (Table 1). Further cohort studies from various centres would be required to establish the accuracy of these new formulae in short eyes.
Long eyes
High myopia is associated with increased incidence of cataract [107], possibly due to the proinflammatory internal microenvironment in the high myopic eye [108]. Additionally, similar to hyperopic eyes, clear lens exchange or cataract surgery could be performed as refractive procedure in these eyes. Nonetheless, these eyes are also prone to refractive error, in particular undesired hyperopia [109], following phacoemulsification. Axial myopia has been defined as AL > 24.5 mm [83, 103, 110, 111], >25mm [112], >25.5mm [113] and AL > 26mm [83, 105, 108, 114]. Similar to hyperopia the error rate of refraction prediction increases in extreme AL [108, 111].
The main sources of errors include:
-
Axial length measurement: due to commonly present staphyloma partial coherence interferometry (PCI) biometry provides a more accurate measurement of AL compared to ultrasound method [102, 115].
-
Prediction of effective lens position (due to broken down correlation between the anatomical parameters like AL, K readings and post-operative ACD changes) [85, 110].
-
The formula employed to calculate the IOL power: Haigis identified the use of plus-power IOL constants for both positive-dioptre IOLs and negative-dioptre IOLs as a source of hyperopic refractive error [116]. At present, optimized IOL constants are calculated separately for the positive-dioptre and negative-dioptre ranges within the framework of ULIB (User Group for Laser Interference Biometry) and studies have suggested that using the ULIB constants yields mean numerical errors that are lower than those with the optical constants [109]. With ULIB-optimised constants, the Haigis formula has produced accurate results [94].
The BU‐II formula has shown great results in long eyes [113, 117]. The Hill-RBF method uses adaptive learning from a large dataset to predict refractive outcomes [83]. This formula employs pattern recognition and data interpolation to derive the IOL power. Olsen formula, on the other hand, uses exact ray tracing technique and thick‐lens considerations for IOL power calculation and a C constant that indicates the final position of IOL [84]. The Holladay 2 formula has also been updated to include a new axial length adjustment [83]. In addition to AL, Ks, and ACD, this formula uses other parameters, such as WTW and LT, in an attempt to better predict the final ELP.
Various studies have compared the accuracy of the 3rd and 4th generation formula in long eyes and a few recent studies have included the 5th generation formulae in their reports.
Abulafia et al. in 2015 did not find any significant difference in MAE between SRK-T, Hoffer Q, Haigis, BU II, Holladay 2 and Olsen in less myopic eyes (IOL power ≥6D). However, BU II, Haigis and Holladay I did better in more myopic eyes with IOL power < 6D [109]. The inaccuracy of Hoffer Q and SRK-T formulae in IOL power calculation in eyes with AL > 26 mm was reported in several studies [83, 108, 111, 114]. Wan et al. achieved good outcomes with BU II and Hill RBF formulae [114]. The percentage of eyes within ±0.25D, ± 0.50D and ±1.00D of the target refraction using Hill-RBF formula was 59.84%, 86.61% and 96.85% respectively in this study [114]. Connell and Kane also found accurate results with BU II, Hill-RBF, Haigis, Holladay 2, Olsen and Kane with no significant differences in their MAE in long eyes [83]. Holladay 2, Hill RBF and BU II were reported equally accurate in eyes with AL > 25 mm [112] and Roberts et al. reported similar outcome with Hill RBF, BU II, Holladay 2, SRKT and Hoffer Q in eyes longer than 24.5 mm but less refractive surprise with BU II [103]. BU II has been demonstrated to be significantly more accurate formula in eyes with AL ≥ 26 mm, AL > 25 mm and AL > 24.5 mm compared to Holladay, Haigis, SRK-T, Hoffer Q, Olsen, Hill-RBF [105, 106, 111, 113, 117], and in comparison, with Olsen, SRK-T and SRK II in eyes with AL > 24.5 mm [84]. The percentage of the eyes within ±0.5D and ±1.00D using BU II formula was respectively 79.56% and 97.24% in Zhang et al. [108] report and 71.07% and 97.97% in Kuthirummal et al. [84]. article, both studies from Asia. Another study in 2017 reported superiority of BU II in medium long eyes (24.5≥AL > 26). They found no statistically significant difference in MAE between BU II, Hill RBF and SRK-T in long eyes [118]. Darcey et al published a report with a large sample size, of which 637 eyes had long AL (≥26 mm). They found Kane formula the most accurate, followed by Barrett U II. In their report Holladay I and Hoffer Q formulae were detected as the least accurate formulae in long eyes [105].
In summary, the 4th and 5th generation formulae appear more accurate than the older generation formulae in myopic eyes. BU II has proved superior to Hoffer Q, SRK-T, Holladay 1,2, Haigis and Olsen in IOL calculation in eyes with high myopia in some studies [83, 105, 108, 111, 113, 114, 117] and comparable with Hill-RBF, Haigis, Kane, Holladay 2, and Olsen in some other studies [83, 111, 112] and inferior to Kane formula in one study [105]. While BU II has proved to have the lowest reported MAE in various studies, it seems that one can also depend on Hill-RBF, Holladay 2 and Haigis (with optimised constant) in myopic eyes (Table 1). More studies are required to establish the accuracy of newer formulae like Kane in long eyes.
Medium eyes
Medium eyes are defined as eyes with axial length ranging from 22 to 24.5 mm in some studies and from 22 to 26 mm in other studies, with additional definition of “medium long” for eyes with AL between 24.5 and 26 mm. Medium eyes comprise the largest scale studies among published papers, making more powerful studies with more reliable outcomes.
Narvaez et al. found Equal accuracy between 3rd generation formulae i.e., Hoffer Q, Holladay and SRK-T in eyes with AL of 22-24.5 mm and 24.5 to 26 mm among 600 patients in 2006 [119]. BU II was found to have significantly lower MAE and highest percentage of eyes within 0.25D, 0.50D and 1.00D in comparison with Holladay 1, 2, SRK-T and Haigis, in medium and medium long eyes [117] and in comparison with SRK-T and SRK II in eyes with AL between 22-24.5mm [84]. It also appeared to have the lowest percentage of refractive surprise (outside ± 1.00 D) across the entire AL groups including 289 medium eyes [103]. Moreover, Kane et al. found BU II the most accurate formula in medium long eyes (AL between 24.5 and 26 mm) followed by Hill RBF [118]. This formula appeared comparable to Olsen [84] and Hill RBF and Holladay [112] in 762 eyes with AL of 22-25 mm. BU II and Hill RBF respectively achieved 42.8 and 43% within 0.25D and 76.4% and 77.6% within 0.50D. The accuracy of Kane formula has been measured against existing formulae in two large scale studies. It was found to be the most accurate formula with the lowest MAE (P < 0.01) compared to SRK-T, Hoffer Q, Hill RBF, Holladay 1,2, Olsen, and BU II among over 700 patients in Australia [83] and 9000 patients in a UK based study [105].
In summary, the newer formulae have demonstrated increased precision in recent studies. Based on published data BU II, Kane and Hill RBF formulae may safely be used to achieve predictable refractive outcome in eyes with medium axial length undergoing cataract surgery (Table 1).
Table 2 describes the summary of recommended formulae for various axial lengths.
Conclusions
In summary, the current evidence on the controversies and dilemmas for cataract surgery in the United Kingdom includes:
-
1.
The cataract surgery improves visual acuity across all grades of AMD severity; however, it should be delayed until a reasonable quiescent period following stopping of anti-VEGF therapy. There is no strong evidence to support worsening of AMD following cataract surgery.
-
2.
Flexibility in assessment of patients with dementia presenting to a cataract service is recommended as their ability to present or express their symptoms may fluctuate or may be not present. The decision for the surgery should be taken in conjunction with next of kin and carers after establishing best interest for these patients on an individual basis. When general anaesthesia is required for cataract surgery in people living with dementia, ISBCS could be considered and discussed with the patient and their carers. Multifocality relies on neuroadaption to provide clear simultaneous distance and near vision which is governed by higher cortical visual areas. People with dementia demonstrate loss of function in these areas of the visual pathway and there is evidence that the dementia process involves the neural structures in the retina and affects retinal and visual performance and therefore multifocal IOLs may not be the best choice for these patients with dementia.
-
3.
Based on current evidence, ISBCS is a viable alternative to DSBCS as the benefits of ISBCS (including comparable clinical and refractive outcomes, reduced hospital costs, improved surgical efficiency and single patient visit for surgery, preassessment and follow-up) outweigh the low risk of post-operative bilateral endophthalmitis. However, meticulous selection and preparation of appropriate cases is essential.
-
4.
When discussing non-standard IOLs in the NHS setting it is important to ascertain that the potential IOL we seek to discuss with a patient is indeed in their best interest, avoid deliberate withholding of information about an IOL which may improve a specific patient’s quality of life and be mindful of the inappropriate time spent in the NHS settings discussing private options which could compromise the care of other NHS patients. It is important for the surgeon not to inappropriately deny patient’s choice and decisions should be taken in partnership with the patients after providing enough information to the patient to make an informed choice.
-
5.
Based on the existing literature, for shorter eyes (AL < 22 mm) Hoffer Q, Haigis, Hill-RBF and Kane formulae are recommended whereas for long eyes (AL > 26 mm) BU II, Holladay 2, Haigis (with optimised constant) and Kane formulae produce better outcomes. For medium eyes with AL of >22 mm but <26 mm, BU II, Hill- RBF and Kane formulae are recommended.
References
Liu IY, White L, LaCroix AZ. The association of age-related macular degeneration and lens opacities in the aged. Am J Public Health. 1989;79:765–9.
Chew EY, Sperduto RD, Milton RC, Clemons TE, Gensler GR, Bressler SB, et al. 3rd. Risk of advanced age-related macular degeneration after cataract surgery in the Age-Related Eye Disease Study: AREDS report 25. Ophthalmology. 2009;116:297–303.
Rosenfeld PJ, Shapiro H, Ehrlich JS, Wong P. Cataract surgery in ranibizumab-treated patients with neovascular age-related macular degeneration from the phase 3 ANCHOR and MARINA trials. Am J Ophthalmol. 2011;152:793–8.
Saraf SS, Ryu CL, Ober MD. The effects of cataract surgery on patients with wet macular degeneration. Am J Ophthalmol. 2015;160:487–92.e1.
Forooghian F, Agrón E, Clemons TE, Ferris FL 3rd, Chew EY. Visual acuity outcomes after cataract surgery in patients with age-related macular degeneration: age-related eye disease study report no. 27. Ophthalmology. 2009;116:2093–100.
Lee TG, Kim JH, Chang YS, Kim CG, Kim JW. Factors influencing the exudation recurrence after cataract surgery in patients previously treated with anti-vascular endothelial growth factor for exudative age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2014;252:1573–9.
Schein OD, Steinberg EP, Cassard SD, Tielsch JM, Javitt JC, Sommer A. Predictors of outcome in patients who underwent cataract surgery. Ophthalmology. 1995;102:817–23.
Casparis H, Lindsley K, Kuo IC, Sikder S, Bressler NM. Surgery for cataracts in people with age-related macular degeneration. Cochrane Database Syst Rev. 2017;2:Cd006757.
Huynh N, Nicholson BP, Agrón E, et al. Visual acuity after cataract surgery in patients with age-related macular degeneration: age-related eye disease study 2 report number 5. Ophthalmology. 2014;121:1229–36.
Ehmann DS, Ho AC. Cataract surgery and age-related macular degeneration. Curr Opin Ophthalmol. 2017;28:58–62.
Kessel L, Koefoed Theil P, Lykke Sorensen T, Munch IC. Cataract surgery in patients with neovascular age-related macular degeneration. Acta Ophthalmol. 2016;94:755–60.
Daien V, Nguyen V, Morlet N, et al. Outcomes and predictive factors after cataract surgery in patients with neovascular age-related macular degeneration. the fight retinal blindness! project. Am J Ophthalmol. 2018;190:50–7.
Shalchi Z, Okada M, Whiting C, Hamilton R. Risk of posterior capsule rupture during cataract surgery in eyes with previous intravitreal injections. Am J Ophthalmol. 2017;177:77–80.
Hahn P, Yashkin AP, Sloan FA. Effect of prior Anti-VEGF injections on the risk of retained lens fragments and endophthalmitis after cataract surgery in the elderly. Ophthalmology. 2016;123:309–15.
Cugati S, Mitchell P, Rochtchina E, Tan AG, Smith W, Wang JJ. Cataract surgery and the 10-year incidence of age-related maculopathy: the Blue Mountains Eye Study. Ophthalmology. 2006;113:2020–5.
Furino C, Ferrara A, Cardascia N, et al. Combined cataract extraction and intravitreal bevacizumab in eyes with choroidal neovascularization resulting from age-related macular degeneration. J Cataract Refract Surg. 2009;35:1518–22.
Arıkan Yorgun M, Toklu Y, Kar ME, Çakmak BH. Effect of cataract surgery in patients with neovascular age-related macular degeneration: further evidence from disciform scars. Int Ophthalmol. 2018;38:459–67.
Bjorklof GH, Helvik AS, Ibsen TL, Telenius EW, Grov EK, Eriksen S. Balancing the struggle to live with dementia: a systematic meta-synthesis of coping. BMC Geriatr. 2019;19:295.
Campbell AJ, Sanderson G, Robertson MC. Poor vision and falls. BMJ. 2010;340:c2456.
Lobo A, Launer LJ, Fratiglioni L, et al. Prevalence of dementia and major subtypes in Europe: A collaborative study of population-based cohorts. Neurologic Diseases in the Elderly Research Group. Neurology. 2000;54:S4–9. 11 Suppl 5
https://www.rcophth.ac.uk/wp-content/uploads/2015/10/RCOphth-The-Way-Forward-Cataract-300117.pdf.
Prince MKM, Guerchet M, McCrone P, Prina M, Comas-Herrera A; Wittenberg R, et al. Dementia UK: Second Edition – Overview: Alzheimer’s Society; 2014.
Bowen M, Edgar DF, Hancock B, Haque S, Shah R, Buchanan S, et al. The Prevalence of Visual Impairment in People with Dementia (the PrOVIDe study): a cross-sectional study of people aged 60–89 years with dementia and qualitative exploration of individual, carer and professional perspectives. Southampton (UK): NIHR Journals Library; 2016. https://doi.org/10.3310/hsdr04210106.
Bryson GL, Wyand A. Evidence-based clinical update: general anesthesia and the risk of delirium and postoperative cognitive dysfunction. Can J Anaesth. 2006;53:669–77.
Jensen BO, Hughes P, Rasmussen LS, Pedersen PU, Steinbruchel DA. Cognitive outcomes in elderly high-risk patients after off-pump versus conventional coronary artery bypass grafting: a randomized trial. Circulation. 2006;113:2790–5.
Newman S, Stygall J, Hirani S, Shaefi S, Maze M. Postoperative cognitive dysfunction after noncardiac surgery: a systematic review. Anesthesiology. 2007;106:572–90.
https://www.rcophth.ac.uk/wp-content/uploads/2015/12/Cataract-Commissioning-Guide-January-2018.pdf.
Rosa AM, Miranda AC, Patricio MM, et al. Functional magnetic resonance imaging to assess neuroadaptation to multifocal intraocular lenses. J Cataract Refract Surg. 2017;43:1287–96.
Antoniades CA, Kennard C. Ocular motor abnormalities in neurodegenerative disorders. Eye (Lond). 2015;29:200–7.
Javaid FZ, Brenton J, Guo L, Cordeiro MF. Visual and ocular manifestations of Alzheimer’s disease and their use as biomarkers for diagnosis and progression. Front Neurol. 2016;7:55
Mills EC, Zarei-Ghanavati M, Liu CSC. Immediate sequential bilateral cataract surgery: The rationale, implementation, and beliefs of ophthalmic surgeons across Europe. J Cataract Refract Surg. 2019;45:1725–31.
Amsden LB, Shorstein NH, Fevrier H, Liu L, Carolan J, Herrinton LJ. Immediate sequential bilateral cataract surgery: surgeon preferences and concerns. Can J Ophthalmol. 2018;53:337–41.
Henderson BA, Schneider J. Same-day cataract surgery should not be the standard of care for patients with bilateral visually significant cataract. Surv Ophthalmol. 2012;57:580–3.
Li O, Kapetanakis V, Claoue C. Simultaneous bilateral endophthalmitis after immediate sequential bilateral cataract surgery: what’s the risk of functional blindness? Am J Ophthalmol. 2014;157:749–51 e1.
Smith GT, Liu CS. Is it time for a new attitude to “simultaneous” bilateral cataract surgery? Br J Ophthalmol. 2001;85:1489–96.
Lundstrom M, Albrecht S, Nilsson M, Astrom B. Benefit to patients of bilateral same-day cataract extraction: Randomized clinical study. J Cataract Refract Surg. 2006;32:826–30.
Sarikkola AU, Uusitalo RJ, Hellstedt T, Ess SL, Leivo T, Kivela T. Simultaneous bilateral versus sequential bilateral cataract surgery: Helsinki Simultaneous Bilateral Cataract Surgery Study Report 1. J Cataract Refract Surg. 2011;37:992–1002.
Serrano-Aguilar P, Ramallo-Farina Y, Cabrera-Hernandez JM, et al. Immediately sequential versus delayed sequential bilateral cataract surgery: safety and effectiveness. J Cataract Refract Surg. 2012;38:1734–42.
Kessel L, Andresen J, Erngaard D, Flesner P, Tendal B, Hjortdal J. Immediate sequential bilateral cataract surgery: a systematic review and meta-analysis. J Ophthalmol. 2015;2015:912481.
Malvankar-Mehta MS, Chen YN, Patel S, Leung AP, Merchea MM, Hodge WG. Immediate versus delayed sequential bilateral cataract surgery: a systematic review and meta-analysis. PLoS One. 2015;10:e0131857.
Nassiri N, Nassiri N, Sadeghi Yarandi SH, Rahnavardi M. Immediate vs delayed sequential cataract surgery: a comparative study. Eye. 2009;23:89–95.
Rush SW, Gerald AE, Smith JC, Rush JA, Rush RB. Prospective analysis of outcomes and economic factors of same-day bilateral cataract surgery in the United States. J Cataract Refract Surg. 2015;41:732–9.
Herrinton LJ, Liu L, Alexeeff S, Carolan J, Shorstein NH. Immediate sequential vs. delayed sequential bilateral cataract surgery: retrospective comparison of postoperative visual outcomes. Ophthalmology. 2017;124:1126–35.
Adatia FA, Munro M, Jivraj I, Ajani A, Braga-Mele R. Documenting the subjective patient experience of first versus second cataract surgery. J Cataract Refract Surg. 2015;41:116–21.
Brogan K, Diaper CJM, Rotchford AP. Cataract surgery refractive outcomes: representative standards in a National Health Service setting. Br J Ophthalmol. 2019;103:539–43.
Gothwal VK, Wright TA, Lamoureux EL, Khadka J, McAlinden C, Pesudovs K. Improvements in visual ability with first-eye, second-eye, and bilateral cataract surgery measured with the visual symptoms and quality of life questionnaire. J Cataract Refract Surg. 2011;37:1208–16.
Hodge W, Horsley T, Albiani D, et al. The consequences of waiting for cataract surgery: a systematic review. CMAJ. 2007;176:1285–90.
Laidlaw DA, Harrad RA, Hopper CD, et al. Randomised trial of effectiveness of second eye cataract surgery. Lancet. 1998;352:925–9.
Jabbour J, Irwig L, Macaskill P, Hennessy MP. Intraocular lens power in bilateral cataract surgery: whether adjusting for error of predicted refraction in the first eye improves prediction in the second eye. J Cataract Refract Surg. 2006;32:2091–7.
Landers J, Goggin M. An inter-eye comparison of refractive outcomes following cataract surgery. J Refract Surg. 2010;26:197–200.
Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL. First eye prediction error improves second eye refractive outcome results in 2129 patients after bilateral sequential cataract surgery. Ophthalmology. 2011;118:1701–9.
Covert DJ, Henry CR, Koenig SB. Intraocular lens power selection in the second eye of patients undergoing bilateral, sequential cataract extraction. Ophthalmology. 2010;117:49–54.
Ganesh S, Brar S, Sreenath R. Immediate sequential bilateral cataract surgery: A 5-year retrospective analysis of 2470 eyes from a tertiary care eye center in South India. Indian J Ophthalmol. 2017;65:358–64.
Benezra D, Chirambo MC. Bilateral versus unilateral cataract extraction: advantages and complications. Br J Ophthalmol. 1978;62:770–3.
Endophthalmitis Study Group ESoC, Refractive S. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg. 2007;33:978–88.
Friling E, Lundstrom M, Stenevi U, Montan P. Six-year incidence of endophthalmitis after cataract surgery: Swedish national study. J Cataract Refract Surg. 2013;39:15–21.
Kashkouli MB, Salimi S, Aghaee H, Naseripour M. Bilateral Pseudomonas aeruginosa endophthalmitis following bilateral simultaneous cataract surgery. Indian J Ophthalmol. 2007;55:374–5.
Ozdek SC, Onaran Z, Gurelik G, Konuk O, Tekinsen A, Hasanreisoglu B. Bilateral endophthalmitis after simultaneous bilateral cataract surgery. J Cataract Refract Surg. 2005;31:1261–2.
Puvanachandra N, Humphry RC. Bilateral endophthalmitis after bilateral sequential phacoemulsification. J Cataract Refract Surg. 2008;34:1036–7.
Mota SH. Pseudomonas aeruginosa-induced bilateral endophthalmitis after bilateral simultaneous cataract surgery: case report. Arq Bras Oftalmol. 2018;81:339–40.
Arshinoff S. Bilateral endophthalmitis after simultaneous bilateral cataract surgery. J Cataract Refract Surg. 2008;34:2006–8. author reply 8
Arshinoff SA, Bastianelli PA. Incidence of postoperative endophthalmitis after immediate sequential bilateral cataract surgery. J Cataract Refract Surg. 2011;37:2105–14.
Lundstrom M, Albrecht S, Roos P. Immediate versus delayed sequential bilateral cataract surgery: an analysis of costs and patient value. Acta Ophthalmol. 2009;87:33–8.
Malvankar-Mehta MS, Filek R, Iqbal M, et al. Immediately sequential bilateral cataract surgery: a cost-effective procedure. Can J Ophthalmol. 2013;48:482–8.
O’Brien JJ, Gonder J, Botz C, Chow KY, Arshinoff SA. Immediately sequential bilateral cataract surgery versus delayed sequential bilateral cataract surgery: potential hospital cost savings. Can J Ophthalmol. 2010;45:596–601.
Leivo T, Sarikkola AU, Uusitalo RJ, Hellstedt T, Ess SL, Kivela T. Simultaneous bilateral cataract surgery: economic analysis; Helsinki Simultaneous Bilateral Cataract Surgery Study Report 2. J Cataract Refract Surg. 2011;37:1003–8.
Neel ST. A cost and policy analysis comparing immediate sequential cataract surgery and delayed sequential cataract surgery from the physician perspective in the United States. JAMA Ophthalmol. 2014;132:1359–62.
Roberts HW, Myerscough J, Borsci S, Ni M, O’Brart DPS. Time and motion studies of National Health Service cataract theatre lists to determine strategies to improve efficiency. Br J Ophthalmol. 2018;102:1259–67.
O’Brart DP, Roberts H, Naderi K, Gormley J. Economic modelling of immediately sequential bilateral cataract surgery (ISBCS) in the National Health Service based on possible improvements in surgical efficiency. BMJ Open Ophthalmol. 2020;5:e000426.
Cataract surgery guidelines by The Royal College of Ophthalmologists. https://www.rcophth.ac.uk/wp-content/uploads/2014/12/2010-SCI-069-Cataract-Surgery-Guidelines-2010-SEPTEMBER-2010-1.pdf.
Grzybowski A, Krzyzanowska-Berkowska P. Immediate sequential bilateral cataract surgery: who might benefit from the procedure? J Cataract Refract Surg. 2013;39:1119–20.
Aaronson A, Viljanen A, Kanclerz P, Grzybowski A, Tuuminen R. Cataract complications study: an analysis of adverse effects among 14,520 eyes in relation to surgical experience. Ann Transl Med. 2020;8:1541 https://doi.org/10.21037/atm-20-845
https://www.supremecourt.uk/cases/docs/uksc-2013-0136-judgment.pdf. (accessed August 2020.
Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016;123:275–86.
Lake JC, Victor G, Clare G, Porfirio GJ, Kernohan A, Evans JR. Toric intraocular lens versus limbal relaxing incisions for corneal astigmatism after phacoemulsification. Cochrane Database Syst Rev. 2019;12:CD012801.
Nanavaty MA, Bedi KK, Ali S, Holmes M, Rajak S. Toric intraocular lenses versus peripheral corneal relaxing incisions for astigmatism between 0.75 and 2.5 diopters during cataract surgery. Am J Ophthalmol. 2017;180:165–77.
de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016;12:CD003169.
The interface between NHS and private treatment: a practical guide for doctors in England, Wales and Northern Ireland. https://www.derbyshirelmc.org.uk/theinterfacebetweennhsandprivatetreatmentapracticalguidefordoctorsinenglandwalesandnorthernireland.
https://www.nhsemployers.org/~/media/Employers/Documents/Pay%20and%20reward/DH_085195.pdf.
https://www.gmc-uk.org/static/documents/content/Consent_-_English_0617.pdf. General Medical Council.
Connell BJ, Kane JX. Comparison of the Kane formula with existing formulas for intraocular lens power selection. BMJ Open Ophthalmol. 2019;4:e000251.
Kuthirummal N, Vanathi M, Mukhija R, et al. Evaluation of Barrett universal II formula for intraocular lens power calculation in Asian Indian population. Indian J Ophthalmol. 2020;68:59–64.
Petermeier K, Gekeler F, Messias A, Spitzer MS, Haigis W, Szurman P. Intraocular lens power calculation and optimized constants for highly myopic eyes. J Cataract Refract Surg. 2009;35:1575–81.
Gokce SE, Montes De Oca I, Cooke DL, Wang L, Koch DD, Al-Mohtaseb Z. Accuracy of 8 intraocular lens calculation formulas in relation to anterior chamber depth in patients with normal axial lengths. J Cataract Refract Surg. 2018;44:362–8.
Holladay JT, Gills JP, Leidlein J, Cherchio M. Achieving emmetropia in extremely short eyes with two piggyback posterior chamber intraocular lenses. Ophthalmology. 1996;103:1118–23.
Lee AC, Qazi MA, Pepose JS. Biometry and intraocular lens power calculation. Curr Opin Ophthalmol. 2008;19:13–7.
Ning X, Yang Y, Yan H, Zhang J. Anterior chamber depth—a predictor of refractive outcomes after age-related cataract surgery. BMC Ophthalmol. 2019;19:134.
Doshi D, Limdi P, Parekh N, Gohil N. A comparative study to assess the predictability of different IOL power calculation formulas in eyes of short and long axial length. J Clin Diagn Res. 2017;11:NC01–NC4.
Wang Q, Jiang W, Lin T, Wu X, Lin H, Chen W. Meta-analysis of accuracy of intraocular lens power calculation formulas in short eyes. Clin Exp Ophthalmol. 2018;46:356–63.
Roh YR, Lee SM, Han YK, Kim MK, Wee WR, Lee JH. Intraocular lens power calculation using IOLMaster and various formulas in short eyes. Korean J Ophthalmol. 2011;25:151–5.
Moschos MM, Chatziralli IP, Koutsandrea C. Intraocular lens power calculation in eyes with short axial length. Indian J Ophthalmol. 2014;62:692–4.
Hoffer KJ, Savini G. IOL power calculation in short and long eyes. Asia Pac J Ophthalmol (Philos). 2017;6:330–1.
Eom Y, Kang SY, Song JS, Kim YY, Kim HM. Comparison of Hoffer Q and Haigis formulae for intraocular lens power calculation according to the anterior chamber depth in short eyes. Am J Ophthalmol. 2014;157:818–24 e2.
Day AC, Cooper D, Burr J, et al. Clear lens extraction for the management of primary angle closure glaucoma: surgical technique and refractive outcomes in the EAGLE cohort. Br J Ophthalmol. 2018;102:1658–62.
MacLaren RE, Natkunarajah M, Riaz Y, Bourne RR, Restori M, Allan BD. Biometry and formula accuracy with intraocular lenses used for cataract surgery in extreme hyperopia. Am J Ophthalmol. 2007;143:920–31.
Naderi M, Sabour S, Khodakarim S, Daneshgar F. Studying the factors related to refractive error regression after PRK surgery. BMC Ophthalmol. 2018;18:198.
Frings A, Druchkiv V, Pose L, Linke SJ, Steinberg J, Katz T. Analysis of excimer laser treatment outcomes and corresponding angle kappa in hyperopic astigmatism. J Cataract Refract Surg. 2019;45:952–8.
Gavin EA, Hammond CJ. Intraocular lens power calculation in short eyes. Eye. 2008;22:935–8.
Carifi G, Aiello F, Zygoura V, Kopsachilis N, Maurino V. Accuracy of the refractive prediction determined by multiple currently available intraocular lens power calculation formulas in small eyes. Am J Ophthalmol. 2015;159:577–83.
Aristodemou P, Knox Cartwright NE, Sparrow JM, Johnston RL. Formula choice: Hoffer Q, Holladay 1, or SRK/T and refractive outcomes in 8108 eyes after cataract surgery with biometry by partial coherence interferometry. J Cataract Refract Surg. 2011;37:63–71.
Roberts TV, Hodge C, Sutton G, Lawless M. contributors to the Vision Eye Institute IOLor. Comparison of Hill-radial basis function, Barrett Universal and current third generation formulas for the calculation of intraocular lens power during cataract surgery. Clin Exp Ophthalmol. 2018;46:240–6.
Gokce SE, Zeiter JH, Weikert MP, Koch DD, Hill W, Wang L. Intraocular lens power calculations in short eyes using 7 formulas. J Cataract Refract Surg. 2017;43:892–7.
Darcy K, Gunn D, Tavassoli S, Sparrow J, Kane JX. Assessment of the accuracy of new and updated intraocular lens power calculation formulas in 10 930 eyes from the UK National Health Service. J Cataract Refract Surg. 2020;46:2–7.
Kane JX, Melles RB. Intraocular lens formula comparison in axial hyperopia with a high-power intraocular lens of 30 or more diopter. J Cataract Refract Surg. 2020;46:1236–39.
Kanthan GL, Mitchell P, Rochtchina E, Cumming RG, Wang JJ. Myopia and the long-term incidence of cataract and cataract surgery: the Blue Mountains Eye Study. Clin Exp Ophthalmol. 2014;42:347–53.
Zhang Y, Liang XY, Liu S, Lee JW, Bhaskar S, Lam DS. Accuracy of intraocular lens power calculation formulas for highly myopic eyes. J Ophthalmol. 2016;2016:1917268.
Abulafia A, Barrett GD, Rotenberg M, et al. Intraocular lens power calculation for eyes with an axial length greater than 26.0 mm: comparison of formulas and methods. J Cataract Refract Surg. 2015;41:548–56.
Wang Q, Jiang W, Lin T, et al. Accuracy of intraocular lens power calculation formulas in long eyes: a systematic review and meta-analysis. Clin Exp Ophthalmol. 2018;46:738–49.
Zhou D, Sun Z, Deng G. Accuracy of the refractive prediction determined by intraocular lens power calculation formulas in high myopia. Indian J Ophthalmol. 2019;67:484–9.
Tang KS, Tran EM, Chen AJ, Rivera DR, Rivera JJ, Greenberg PB. Accuracy of biometric formulae for intraocular lens power calculation in a teaching hospital. Int J Ophthalmol. 2020;13:61–5.
Melles RB, Holladay JT, Chang WJ. Accuracy of intraocular lens calculation formulas. Ophthalmology. 2018;125:169–78.
Wan KH, Lam TCH, Yu MCY, Chan TCY. Accuracy and precision of intraocular lens calculations using the new hill-RBF version 2.0 in eyes with high axial myopia. Am J Ophthalmol. 2019;205:66–73.
Rose LT, Moshegov CN. Comparison of the Zeiss IOLMaster and applanation A-scan ultrasound: biometry for intraocular lens calculation. Clin Exp Ophthalmol. 2003;31:121–4.
Haigis W. Intraocular lens calculation in extreme myopia. J Cataract Refract Surg. 2009;35:906–11.
Kane JX, Van Heerden A, Atik A, Petsoglou C. Intraocular lens power formula accuracy: comparison of 7 formulas. J Cataract Refract Surg. 2016;42:1490–500.
Kane JX, Van Heerden A, Atik A, Petsoglou C. Accuracy of 3 new methods for intraocular lens power selection. J Cataract Refract Surg. 2017;43:333–9.
Narvaez J, Zimmerman G, Stulting RD, Chang DH. Accuracy of intraocular lens power prediction using the Hoffer Q, Holladay 1, Holladay 2, and SRK/T formulas. J Cataract Refract Surg. 2006;32:2050–3.
Funding
There was no funding attached to this work. Independent group of authors worked on different topics of this review without any funding support.
Author information
Authors and Affiliations
Contributions
SC, SS: contributed to the section of “Age-related macular degeneration and cataract”. PU: contributed to the section of “Dementia and cataract”. KN, DO: contributed to the section of “Immediate Simultaneous Bilateral Cataract Surgery”. AA: contributed to the section of “The ethical dilemma of discussing non-standard intraocular lenses within the National Health Service setting”. ZA, MAN: contributed to the section of “Intraocular lens calculation formulas for short, long and medium axial length eyes”
Corresponding author
Ethics declarations
Conflict of interest
SC, SS, PGU, KN, AA, ZA: No conflict of interests to disclose. DO: Non-commercial research grants with Rayner Ltd., Alcon Inc. and Avedro Inc. Consultant to Zeiss and Sparca Inc. MAN: Research grants from Alcon Laboratories, USA; European Society of Cataract & Refractive Surgery; Johnson & Johnson, USA; NuVision Biotherapies, UK; Rayner Intraocular lenses, UK. Lecture fees from Alcon Laboratories, USA & Bausch & Lomb, USA. Consultant to Hoya. Travel grant from Alcon Laboratories, USA & Bausch & Lomb, USA.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chandra, S., Sivaprasad, S., Ursell, P.G. et al. Recurring themes during cataract assessment and surgery. Eye 35, 2482–2498 (2021). https://doi.org/10.1038/s41433-021-01548-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01548-4