Abstract
Study design
Retrospective chart review.
Objectives
The primary aim was to identify the number of patients requiring vasopressors beyond the first week of cervical spinal cord injury (SCI). Secondary objectives were to note the type, duration and doses of vasopressors and any association between prolonged vasopressors use and outcome.
Setting
Neurosurgical intensive care of a tertiary trauma care centre.
Methods
After Ethical approval we retrospectively collected the data of patients of isolated cervical SCI admitted to neurosurgical intensive care from January to December 2017. Vasopressor requirement for sepsis or cardiac arrest was excluded.
Results
Out of 80 patients analysed, 54 (67.5%) received vasopressors. The prolonged requirement of vasopressors was observed in 77.7%. Our preferred agent was dopamine (64.8%). We found out that longer requirement (in days) of high dose of dopamine was associated with higher survival (p = 0.03).
Conclusion
Our results describe a significant portion of cervical SCI patients need ongoing vasopressor to maintain a mean arterial pressure >65 mm of Hg beyond first week. We observed patients who required longer duration of high dose dopamine had a higher chance of survival suggesting some unknown mechanism of high dose of dopamine. This is first such observation, further studies are needed to substantiate.
Similar content being viewed by others
Introduction
Acute traumatic cervical spinal cord injury (SCI) imparts a huge economic and social burden on a country [1]. Regardless of advancements in perioperative and intensive care management the functional outcome continues to remain poor in such patients with many patients need prolonged hospital stay and neurorehabilitaion [2]. The principles of management are early stabilisation and prevention of secondary insult to spinal cord [3]. Intensive blood pressure management targeting a mean arterial pressure (MAP) of 85–90 mm of Hg is aimed during the first week of the injury and 65 mm Hg thereafter to maintain adequate spinal cord perfusion is often the mainstay of management [4, 5]. In such patients after the acute phase of injury, hypotension is often observed and can be either orthostatic hypotension or resting hypotension [6]. The hypotension is attributed to various causes such as sympathetic nervous system dysfunction, low plasma catecholamine levels, impaired baroreceptors function, spinal and/or neurogenic shock, cardiovascular deconditioning, hyponatremia and low plasma volume, poor muscular pumping activity [7, 8]. The management of chronic hypotension in these patients is indeed challenging and often need continual low dose of intravenous vasopressors to maintain a MAP of 65 mm of Hg or above [7]. Such patients often require either pharmacological or non-pharmacological methods to treat the chronic hypotension [9]. Majority of the instances the vasoconstrictor agent started in the acute phase is continued beyond the first week and gradually weaned over time. However no studies in literature explored the use of long term vasopressors in such patients after the initial week of intensive therapy. This is first such investigation that explores the use of prolong use of vasopressors in these patients. We conducted the analysis with the primary aim of this study was to identify the number of patients requiring vasopressors beyond the first week of cervical SCI. Secondary objectives were to note the type, duration and doses of vasopressors for such kind of the patients beyond the first week of injury and to find out the association between prolonged usage of vasopressors and outcome. Our exploratory objectives were (1) presence of spinal cord signal changes in magnetic resonance imaging (MRI) and its effect outcome; (2) possibility of incentive spirometry and outcome; (3) weaning from mechanical ventilation and outcome.
Methodology
After Institute Ethical Committee approval we collected the data of patients of acute traumatic cervical spinal injury admitted to neurosurgical intensive care unit (ICU) from January to December 2017. Patients with associated head injury, admission 7 days after injury and those treated elsewhere before were excluded. Patients were managed as per the standard ICU protocol. All the patients were monitored with prompt correction of fluid deficits and anaemia before starting vasopressors in the ICU. All the data of the patient were kept confidential. Data was collected from electronic medical records, patient admission, operation theatre records, ICU records and discharge sheets. American Spinal Injury Association Impairment Scale (AIS) [10] and level of cervical SCI was recorded from the databases. Radiological data were recorded from the electronic records. Data regarding the type, duration and dose of vasopressors were noted from the nursing records till the patients discharged from the hospital or death. Initiation of vasopressors as a management for septic shock or post resuscitation from cardiac arrest was excluded from analysis. We also acquired the data of incentive spirometry and weaning from mechanical ventilation from the nursing records.
We defined requirement of vasopressors therapy 7 days and beyond as prolonged vasopressor requirement. We classified doses of dopamine as low (<5 mcg/kg/min), medium (5–10 mcg/kg/min) and high (>10 mcg/kg/min) [11]. Similarly we also have defined the dose of noradrenaline as low (0.05–0.5 mcg/kg/min) and high (0.5–2 mcg/kg/min) [12]. The level of cervical SCI as classified as high (C1–C4) for first to fourth cervical vertebra and low (C5–C7) for fifth to seventh cervical vertebrae [13]. AIS was dichotomised into complete (category A) and incomplete (category B, C, D, E) [10]. Also we have classified the AIS to severe cervical injury (AIS A and B) and mild cervical injury (AIS C, D, E) group [14]. We have reviewed the MRI database to determine the cord signal changes. We followed the patients till the time of discharge or death. We labelled all in-hospital mortality as non-survivors, while others who were discharged were considered as survivors.
All the statistical analyses were done using STATA 12.0 (Stata Corp, College Station, TX). Data were expressed as medians with range for nonparametric data and in percentages for binary variables. We have used Kruskal–Wallis test to compare patient level characteristics in vasopressor groups. Mann–Whitney U test was applied to look into differences between variables in survivor and non-survivor group. The Pearson’s chi square test and Fisher exact tests were used for categorical data as appropriate. A P value less than 0.05 was considered significant.
Results
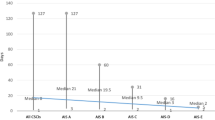
Medical records of 100 patients of isolated acute cervical SCI admitted to the neurosurgical ICU reviewed. Twenty patients were excluded due to various reasons (Fig. 1). Finally a total of 80 patients with a median age of 40 years were analysed (Fig. 1). Out of the 80 patients, 69 (86.25%) were male (Table 1). Fifty-four patients (67.5%) received vasopressors to maintain a target MAP of 85–90 mm of Hg. We noticed that 42 patients (77.7%) needed prolonged vasopressors to maintain a MAP > 65 mm of Hg. The median duration of prolonged vasopressor therapy was 13 (7–86) days. We have used dopamine, noradrenaline or combination as vasopressors. Majority of our patients 35 out of 54 (64.8%) received dopamine and in 29 patients required prolonged dopamine. The patient level characteristics in vasopressor groups were described in Table 2. While the analysis of AIS revealed the patients of category A required longer duration of low and medium doses of dopamine (P = 0.02 and P = 0.01). AIS category A was significantly associated with prolonged vasopressors requirement (P = 0.001) (Fig. 2). We observed severe cervical injury group (AIS A, B combined) and complete cervical injury (AIS A) required prolong vasopressor as compared to mild injury group (P = 0.001 and P = 0.005) (Table 3). However we did not find any such association between duration of dopamine use in various doses to the level of cervical injury.
a Distribution of American Spinal Injury Association Impairment Scale (AIS) categories in survivors and non-survivors. b Patients receiving longer and shorter vasopressor therapy in different American Spinal Injury Association Impairment Scale (AIS). c Graphical representation of survivors and non-survivors receiving long and short term vasopressor therapy in AIS-A category of patients.
Sixty seven patients out of 80 patients (83.7%) survived at the time of discharge. We found that mortality was high in severe cervical injury (AIS A, B combined) as compared to mild cervical injury group (P = 0.01). The main cause of death amongst non-survivors were sepsis, multiorgan dysfunction and circulatory arrest. We observed out of the 42 patients who needed long term vasopressors 31 patients (73.8%) survived (P = 0.09). Many patients received a variable period of dopamine infusion at different doses as mentioned above. In total 10 patients (8 survived) received high dose of dopamine in the prolonged vasopressor group. When we analysed the use of dopamine, we found out that survivors received a longer duration (in days) of high dose of dopamine (p = 0.03) (Table 4). The median duration of high dose dopamine usage was 4 (1–10) days in survivor group as compared to 1 (0–1) day in non-survivor group (Table 4).
Many patients (64 out of 67 patients) in the survivor group were successfully weaned off mechanical ventilation. Similarly many patients in the survivor group were able to perform incentive spirometry. (53 out of 67 patients) (Table 5). However presence of spinal cord signal changes in MRI did not affect the outcome (Table 5).
Discussion
In our study we found out that a significant proportion of cervical SCI patients require prolong course of vasopressor to treat the ongoing hypotension (MAP < 65 mm Hg). In one study authors report the prevalence of persistent resting hypotension was 38% in paraplegic patients after SCI [6]. In our study we did not determine the cause of the persistent hypotension. Form our study it is evident that 64.8% of patients received dopamine. In a similar study dopamine was used as first choice of vasopressor in 60.3% of patients requiring vasopressors [15]. In our practice we prefer dopamine as compare to noradrenaline as majority of the patients manifest neurogenic shock with sinus bradycardia and hypotension in the acute phase. The AANS/CNS Joint Committee guidelines state to maintain a MAP goal of 85–90 mm but do not make a specific recommendation regarding the type of vasopressor [16]. The Consortium for Spinal Cord Medicine suggests use of dopamine or norepinephrine for cervical or high thoracic regions [17].
A recent systematic review analysed the use of dopamine, noradrenaline and phenyleprine for SCI, suggested use of noradrenaline and phenylephrine as more complications observed in the dopamine usage [5]. Majority of the complications were ST segment elevation, atrial fibrillation, and ventricular tachycardia [5, 15]. In our practice we found no such adverse events related to dopamine use, although our study did not probe into the adverse effects related to vasopressor use.
We also found that severe cervical injury group (AIS A and B) and complete cervical injury (AIS A) patients needed prolonged vassopressor therapy. Previous such studies support our findings as episodic hypotension was observed more in severe cervical injury group and at least half of them needed vasopressors. However in their observation such episodes of hypotension were not seen beyond 14 days of SCI [14].
Evidences point that hypotension with neurological injury results in poorer outcomes [11]. Multiple studies have proven that intensive blood pressure management in the acute phase in SCI patients is associated with better outcome [5, 18]. This analysis where we targeted the subacute and chronic phase of cervical SCI reveals 31 out of 42 survivors received prolonged vasopressors, but the result was not statistically significant.
In this analysis we have observed that the patients in the survivor group received longer duration of high dose of dopamine administration (>10 mcg/kg/min) as compared to non-survivors. This might be due to the fact that, dopamine in high doses acts on alpha receptors which can cause peripheral vasoconstriction [19]. In our analysis only 10 patients required longer duration of high dose of dopamine.
We did not find any association of cervical injury level to the use of prolonged vasopressor. In a previously done study authors found no significant difference in the frequency of neurogenic shock by injury level, but patients with a higher injury level had a significantly greater requirement for a cardiovascular intervention compared with patients with lower injuries [20]. In this study the authors classified high and low cervical injury level as C1–C5 and C6–C7 respectively.
One of our exploratory outcomes is the effect of presence of spinal cord signal changes in MRI on outcome, which revealed no significant association with outcome. Studies in the past have similar results where presence of cord oedema, cord haemorrhage had no effect on neurological functional recovery [21]. We have observed majority of the patients in the survivor group could perform incentive spirometry and thus weaning from mechanical ventilation was observed in many patients in the survivor group.
The study has the following limitations. Firstly, the retrospective design of the study makes it vulnerable to attrition of data leading to small samples size and the findings of which cannot be generalised unless large scale prospective studies are conducted. Due to the retrospective nature of the design, we have not acquired data on blood pressure readings; which can be considered as a limitation. We did not analyse the noradrenaline dose as the use of noradrenaline was much less as compared to the use of dopamine and the data regarding the dose of noradrenaline was not available during several occasions.
Conclusion
A significant portion of cervical SCI patients need an ongoing vasopressors to maintain a modest MAP beyond first week. We observed patients who received longer duration of high dose dopamine had a higher chance of survival suggesting some unknown mechanism of high dose of dopamine. This is first such observation, and we think that further studies are needed to substantiate.
References
Singh A, Tetreault L, Kalsi-Ryan S, Nouri A, Fehlings MG. Global prevalence and incidence of traumatic spinal cord injury. Clin Epidemiol. 2014;6:309–31.
Fielingsdorf K, Dunn RN. Cervical spine injury outcome-a review of 101 cases treated in a tertiary referral unit. S Afr Med J. 2007;97:203–7.
Ploumis A, Yadlapalli N, Fehlings MG, Kwon BK, Vaccaro AR. A systematic review of the evidence supporting a role for vasopressor support in acute SCI. Spinal Cord. 2010;48:356–62.
Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE, et al. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery. 2013;60:82–91.
Saadeh YS, Smith BW, Joseph JR, Jaffer SY, Buckingham MJ, Oppenlander ME, et al. The impact of blood pressure management after spinal cord injury: a systematic review of the literature. Neurosurg Focus. 2017;43:E20.
Ashta KK, Kumar R. Prevalence of resting bradycardia, resting hypotension and orthostatic hypotension in chronic spinal cord injury patients. Int J Adv Med. 2017;4:1319–122.
Claydon VE, Steeves JD. Orthostatic hypertension following spinal cord injury: understanding clinical pathophysiology. Spinal Cord. 2006;44:341–35.
Grigorean VT, Sandu AM, Popescu M, Iacobini MA, Stoian R, Neascu C, et al. Cardiac dysfunctions following spinal cord injury. J Med Life. 2009;2:133–45.
Krassioukov A, Eng JJ, Warburton DE, Teasell R. Spinal Cord Injury Rehabilitation Evidence Research Team. A systematic review of the management of orthostatic hypotension after spinal cord injury. Arch Phys Med Rehabil. 2009;90:876–85.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46.
King JE. What is “renal dose” dopamine? Nursing 2004;34:26.
Bassi E, Park M, Azevedo LC. Therapeutic strategies for high-dose vasopressor-dependent shock. Crit Care Res Pr. 2013;2013:654708.
Shao J, Zhu W, Chen X, Jia L, Song D, Zhou X, et al. Factors associated with early mortality after cervical spinal cord injury. J Spinal Cord Med. 2011;34:555–562.
Lehmann KG, Lane JG, Piepmeier JM, Batsford WP. Cardiovascular abnormalities accompanying acute spinal cord injury in humans: incidence, time course and severity. J Am Coll Cardiol. 1987;10:46–52.
Inoue T, Manley GT, Patel N, Whetstone WD. Medical and surgical management after spinal cord injury: vasopressor usage, early surgerys, and complications. J Neurotrauma. 2014;31:284–91.
Walters BC, Hadley MN, Hurlbert RJ, Aarabi B, Dhall SS, Gelb DE, et al. American Association of Neurological Surgeons; Congress of Neurological Surgeons. Guidelines for the management of acute cervical spine and spinal cord injuries: 2013 update. Neurosurgery. 2013;60:82–91.
Consortium for Spinal Cord Medicine. Early acute management in adults with spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2008;31:403–479.
Catapano JS, John Hawryluk GW, Whetstone W, Saigal R, Ferguson A, Talbott J, et al. Higher Mean Arterial Pressure Values Correlate with Neurologic Improvement in Patients with Initially Complete Spinal Cord Injuries. World Neurosurg. 2016;96:72–9.
Glick DB: The Autonomic Nervous System. In miller RD, editor. Miller’s Anesthesia, ed 8. Philadelphia: Elsevier; 2015. p. 367.
Bilello JF, Davis JW, Cunningham MA, Groom TF, Lemaster D, Sue LP. Cervicalspinal cord injury and the need for cardiovascular intervention. Arch Surg. 2003;138:1127–9.
Kurpad S, Martin AR, Tetreault LA, Fischer DJ, Skelly AC, Mikulis D, et al. Impact of Baseline Magnetic Resonance Imaging on Neurologic, Functional, and Safety Outcomes in Patients With Acute Traumatic Spinal Cord Injury. Glob Spine J 2017;7:151S–174S.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mishra, R.K., Goyal, K., Bindra, A. et al. An investigation to the prolonged requirement (>7 days) of vasopressors in cervical spinal cord injury patients—a retrospective analysis. Spinal Cord Ser Cases 7, 96 (2021). https://doi.org/10.1038/s41394-021-00459-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00459-6