Abstract
Extensive evidence supports the hypothesis that deficits in inhibitory GABA transmission in the prefrontal cortex (PFC) may drive pathophysiological changes underlying symptoms of schizophrenia that are not currently treated by available medications, including cognitive and social impairments. Recently, the mGlu1 subtype of metabotropic glutamate (mGlu) receptor has been implicated as a novel target to restore GABAergic transmission in the PFC. A recent study reported that activation of mGlu1 increases inhibitory transmission in the PFC through excitation of somatostatin-expressing GABAergic interneurons, implicating mGlu1 PAMs as a potential treatment strategy for schizophrenia. Here, we leveraged positive allosteric modulators (PAMs) of mGlu1 to examine whether mGlu1 activation might reverse physiological effects and behavioral deficits induced by MK-801, an NMDA receptor antagonist commonly used to model cortical deficits observed in schizophrenia patients. Using ex vivo whole-cell patch-clamp electrophysiology, we found that MK-801 decreased the frequency of spontaneous inhibitory postsynaptic currents onto layer V pyramidal cells of the PFC and this cortical disinhibition was reversed by mGlu1 activation. Furthermore, acute MK-801 treatment selectively induced inhibitory deficits onto layer V pyramidal cells that project to the basolateral amygdala, but not to the nucleus accumbens, and these deficits were restored by selective mGlu1 activation. Importantly, the mGlu1 PAM VU6004909 effectively reversed deficits in sociability and social novelty preference in a three-chamber assay and improved novel objection recognition following MK-801 treatment. Together, these findings provide compelling evidence that mGlu1 PAMs could serve as a novel approach to reduce social and cognitive deficits associated with schizophrenia by enhancing inhibitory transmission in the PFC, thus providing an exciting improvement over current antipsychotic medication.
Similar content being viewed by others
Introduction
Schizophrenia is a chronic brain disease that involves three primary symptom clusters: positive, negative, and cognitive impairment [1]. Current antipsychotic medications show efficacy in treating the positive symptoms of the disease; however, they do not mitigate negative symptoms and cognitive deficits [2, 3]. Therefore, intense ongoing efforts aim to delineate the cellular and molecular mechanisms underlying these symptom clusters to develop novel, improved therapeutics to treat individuals with schizophrenia. The prefrontal cortex (PFC) plays a critical role in orchestrating complex behavioral functions known to be disrupted in individuals with schizophrenia, including many cognitive processes and social behavior [4, 5]. A key regulator of these behavioral outputs within the PFC is the γ-aminobutyric acid (GABA) system [5, 6]. Based on many studies demonstrating that reduced GABAergic transmission in the PFC is associated with decreased sociability and impaired cognition [5, 7, 8], it has long been hypothesized that loss of GABAergic transmission in the PFC may drive pathophysiological changes underlying behavioral deficits in schizophrenia patients [9]. In support of this hypothesis, reduced PFC mRNA and protein levels of glutamic acid decarboxylase 67 (GAD67), the enzyme responsible for synthesis of GABA from glutamate precursor for GABA, is one of the most consistent pathophysiological findings in postmortem brain tissue from patients with schizophrenia [10,11,12]. Furthermore, enhancing GABA signaling and normalizing the balance between inhibition and excitation (I/E balance) in the PFC improves cognition and social interaction [13, 14]. Thus, restoring cortical inhibition represents a promising strategy to address unmet clinical needs for people living with schizophrenia.
The mGlu1 receptor subtype of metabotropic glutamate mGlu receptors has recently been implicated as a critical regulator of inhibitory signaling in the PFC [14]. Highly expressed on GABAergic interneurons of the PFC [14,15,16,17], activation of the mGlu1 receptor enhances feedforward inhibition onto glutamatergic pyramidal neurons in acute PFC slices [18]. A recent study by Maksymetz et al. showed that mGlu1 augments somatostatin-expressing interneuron (SST-IN) output in the prelimbic (PL) PFC, resulting in increased inhibition [14]. Leveraging novel positive allosteric modulators (PAMs) selective for mGlu1, we found that activation of mGlu1 shifts I/E balance toward inhibition in the PL-PFC and reverses deficits in working memory via actions on SST interneurons. Together, these findings strongly suggest that mGlu1 is an important regulator of PFC inhibition and a promising target for treating symptoms of schizophrenia that are not alleviated by current medications. However, the potential efficacy of mGlu1 PAMs in reversing deficits in inhibitory transmission and reversing additional PFC-dependent behavioral deficits in NMDAR hypofunction models, such as social behavior and other forms of cognition, has yet to be determined.
Multiple studies suggest that N-methyl-d-aspartate receptor (NMDAR) hypofunction may play a key role in pathophysiology of schizophrenia and that this is due in part to disruption of PFC GABAergic transmission, which leads to behavioral impairments associated with the disease. The NMDAR hypofunction hypothesis of schizophrenia is largely based on observations that NMDAR antagonists, such as phencyclidine (PCP) and dizocilpine (MK-801), elicit behavioral abnormalities reminiscent of all three classes of schizophrenia-related symptomology (positive, negative, and cognitive) [19]. Of the non-competitive NMDAR antagonists, MK-801 displays high specificity and affinity for NMDARs and produces behavioral effects related to schizophrenia across multiple species [20]. Extensive preclinical literature demonstrates the ability of acute MK-801 administration to induce deficits in social interaction and a multitude of cognitive processes including working memory, attention, and recognition memory [14, 21, 22]. Importantly, MK-801 disrupts cortical networks and the function of PFC GABA interneurons. For instance, systemic injection of MK-801 decreases the firing of GABAergic interneurons and disinhibits pyramidal cells in the mPFC, suggesting that the primary target of MK-801 is the GABAergic neurons [23]. Therefore, administration of MK-801 is commonly used to model cortical inhibitory deficits and associated behavioral deficits relevant to schizophrenia. In the present study, we use an NMDAR antagonist model of cortical disinhibition in mice to test our central hypothesis that selective activation of mGlu1 will reverse deficits in PL-PFC inhibitory transmission and social and cognitive deficits. Using this approach, we evaluated the efficacy of an mGlu1 PAM in reversing social and non-social cognitive deficits associated with schizophrenia. The findings from this study provide important insights into the synaptic mechanism by which mGlu1 regulates inhibitory transmission in the PFC and excitatory outputs to brain regions central to social behavior and cognition.
Materials and methods
Animal use
Adult (>8-week-old) male and female C57BL/6J mice (Cat No. 000664; RRID: IMSR_JAX:000664) were obtained from Jackson Laboratories (Bar Harbor, ME, USA). Experiments were performed in group-housed mice (5/cage) on a 12 h light cycle (lights on at 6:00 a.m.) and given access to food/water ad libitum in accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals. All experimental protocols were approved by the Vanderbilt Institutional Animal Care and Use Committee. Mice were injected either vehicle (0.9% saline) or MK-801 (0.18 mg/kg, i.p) 24 h prior to all electrophysiology or behavioral studies.
Compounds
DHPG ((S)-3,5-dihydroxyphenylglycine) was purchased from Hello-Bio Inc. (Princeton, NJ, USA). MTEP hydrochloride and MK-801 maleate were purchased from Tocris Bioscience (Minneapolis, MN, USA). As previously described, VU6004909 was synthesized in-house [24, 25]. Stock solutions were prepared in deionized water for DHPG and MTEP, 0.9% saline for MK-801, and 10% Tween-80 for VU6004909.
Electrophysiology
Whole-cell recordings were performed as previously described [14, 26]. Briefly, mice were anesthetized with 5% isoflurane and the brain was rapidly removed and mounted to the cutting stage of a vibratome. Coronal sections containing the medial PFC (mPFC) were prepared at 300 μm in ice-cold NMDG-HEPES artificial cerebrospinal fluid (aCSF) containing (in mM: 92 NMDG, 2.5 KCl, 1.25 NaH2PO4, 30 NaHCO3, 20 HEPES, 25 glucose, 2 thiourea, 5 Na-ascorbate, 3 Na-pyruvate, 0.5 CaCl2·2H2O, and 10 MgSO4·7H2O, pH 7.3–7.4 with HCl). Slices were then transferred to 32 °C NMDG-HEPES solution for 10 min and then were transferred to a holding chamber containing aCSF (in mM: 126 NaCl, 2.5 KCl, 1.25 Na2PO4, 26 NaHCO3, 10 glucose, 2 CaCl2, 1 MgSO4, supplemented with 500 μM sodium ascorbate) at room temperature for a minimum of 1 h prior to acquisition of recordings. Slices were submerged in the recording chamber (Warner Instruments, CT, USA) and perfused with aCSF maintained at 31 ± 1 °C using an in-line heater (Warner Instruments, CT, USA) at a rate of 2 mL/min. Whole-cell patch-clamp recordings were performed in the prelimbic PFC from visually identified layer V pyramidal neurons. Cells were excluded from analysis if access resistance changed more than 25% throughout the recording period. To record spontaneous inhibitory postsynaptic currents (sIPSCs) and within-cell sIPSCs:sEPSCs ratios, pipets were filled with a Cesium-based internal solution (in mM: 140 CsMeSO3, 5NaCl, 10 HEPES, 0.2 EGTA, 2 MgATP, 0.2 NaGTP, 5 QX-314). sEPSCs and sIPSCs were recorded at −70 mV and +10 mV, respectively (adjusted for the liquid junction potential). Bath application of 50 μM picrotoxin was used to confirm that sIPSCs were GABAA mediated while sEPSCs were confirmed by bath application of 20 μM CNQX and 50 μM D-AP5. To generate within-cell sIPSC:EPSC ratios, baseline sEPSCs were recorded for 2 min at −70 mV, then voltage holding was elevated to +10 mV for recording of sIPSCs and in response to compound application.
Three-chamber test
Social interaction test
The three-chamber test was used to assay sociability and preference for social novelty as demonstrated previously [27]. Briefly, the mouse was placed in the middle chamber of the three-chamber apparatus and allowed to explore freely for 5 min. After 5 min of habituation, identical small metal wire cups were placed in the left and right chambers and the dividers were lifted. An unfamiliar adult C57BL/6 J male (Stranger 1) was placed inside one of the wire cups. Location of the stranger mouse and the empty wire cage was counterbalanced between sessions. The test subject was returned to the apparatus and was allowed to move freely throughout all three chambers of the apparatus for 10 min. Time spent exploring the empty cup and stranger mouse was analyzed as described previously using AnyMaze software and the social interaction index was calculated as (time spent exploring stranger mouse)/[(time spent exploring empty cup) + (total spent exploring stranger mouse)].
Preference for social novelty test
Immediately following the social interaction test (phase 2), a 10 min testing phase occurred to test preference for social novelty. The original stranger mouse (stranger 1) remained in its wire cage on one side of the apparatus. A new unfamiliar mouse (stranger 2) was placed in the wire cage on the opposite side, which was previously empty during the sociability test. Interaction times were calculated as described previously using AnyMaze software and the social novelty recognition index was calculated as (time spent exploring novel mouse)/[(time spent exploring familiar mouse) + (total spent exploring novel mouse)].
Novel object recognition
Short-term recognition memory was measured using the novel object recognition assay (NOR) as reported previously [28]. Briefly, mice were habituated in an empty arena consisting of a dark-colored Plexiglas box (32 × 32 × 40 cm) for 10 min. Approximately 24 h later, the mice were injected with vehicle (10% Tween-80) or VU6004909 (i.p.; 60 mg/kg) and placed back into their home cage for 30 min. Mice were then placed back into the NOR arena containing 2 identical objects for 10 min. Following the exposure period, mice were placed back into their home cages for 1 h. The mice were then returned to the arena in which one of the previously exposed (familiar) objects was replaced by a novel object. The mice were video recorded for 10 min while they explored the objects. Time spent exploring each object was analyzed using AnyMaze software and the novelty recognition index was calculated as (time spent exploring novel object)/[(time spent exploring familiar object) + (total spent exploring novel object)].
Data analysis
Data are presented as mean ± standard error (SEM). The sample size of mice in each experiment is denoted by “N” and cells/slices by “n”. Statistical analyses were performed using GraphPad Prism (CA). A paired/unpaired two-tailed Student’s t-test, one/two-way ANOVA, or repeated measures two-way ANOVA with Bonferroni’s post-test were used where appropriate. Results of statistical analyses are presented in the “Results” section.
Results
mGlu1 activation reverses MK-801-induced deficits in spontaneous inhibitory transmission onto PL-PFC pyramidal cells
To determine the role of mGlu1 in regulating cortical inhibitory signaling, we leveraged an NMDAR hypofunction model to elicit physiological and behavioral deficits associated with schizophrenia. Antagonizing NMDARs with pharmacological agents such as MK-801 precipitates symptoms in individuals with schizophrenia and induces schizophrenia-like symptoms including cognitive deficits in healthy individuals [29]. Furthermore, administration of the NMDAR antagonist MK-801 in rodents increases mPFC pyramidal neuron firing while decreasing the activity of PV- and SST-INs [23] and increases PFC brain activity as measured by fMRI studies [14]. Therefore, we used MK-801 as a pharmacological tool to model schizophrenia-like functional deficits in inhibitory transmission and directly test the hypothesis that selective activation of mGlu1 reverses deficits in inhibitory transmission onto prelimbic (PL)-PFC pyramidal cells.
First, mice were injected with MK-801 (0.18 mg/kg, i.p.) or saline, and then, whole-cell patch-clamp electrophysiology experiments in acute brain slices were performed 24 h later to measure spontaneous inhibitory and excitatory postsynaptic currents (sIPSC/sEPSCs) onto layer V pyramidal cells (Fig. 1A). We found that acute MK-801 treatment significantly reduced sIPSC frequency onto layer V pyramidal cells (6.46 ± 0.41 Hz) compared to saline-treated mice (11.13 ± 0.69 Hz) (Fig. 1A, B, p < 0.0001, Student’s t-test). The amplitude of sIPSCs onto layer V pyramidal cells in mice treated with MK-801 (39.51 ± 3.14 pA) was not significantly different compared to saline-treated mice (40.27 ± 3.21 pA) (Fig. 1C, p = 0.87, Student’s t-test). Additionally, the rise and decay time of sIPSCs did not differ between saline- and MK-801-treated mice (Supplementary Fig. 1). Next, we evaluated the frequency and amplitude of sEPSCs onto layer V pyramidal cells in mice pretreated with saline or MK-801 (Fig. 1D, E). We found that the sEPSC frequency of mice treated with MK-801 (16.83 ± 1.62 Hz) was not significantly different compared to saline-treated mice (15.96 ± 1.36 Hz) (Fig. 1D, p = 0.69, Student’s t-test). The amplitude of sEPSCs onto layer V pyramidal cells did not differ between saline (−20.78 ± 2.24 pA) and MK-801-treated mice (−21.24 ± 2.34 pA) (Fig. 1E, p = 0.89, Student’s t-test). Lastly, we compared the ratio of sIPSC to sEPSC frequency within the same pyramidal neurons. MK-801 treatment significantly decreased the inhibitory/excitatory (I/E) ratio (0.53 ± 0.09) compared to saline-treated mice (1.20 ± 0.14) (Fig. 1F, p = 0.0005, Student’s t-test), suggesting that acute MK-801 administration induces deficits in inhibitory signaling in the PL-PFC relevant to those associated with schizophrenia.
A Representative trace of voltage-clamp recording of layer V pyramidal cell 24 h following a single injection of MK-801 (0.18 mg/kg, i.p.) (middle) or saline (top) and following bath application of DHPG (30 µM) and MTEP (3 µM). Scale bar, 2.5 s. B MK-801 decreases sIPSC frequency compared to mice treated with saline (n/N = 4 to 6/5 cells/mice per group, ***p < 0.0001 versus saline, Student’s t-test). C MK-801 does not alter sIPSC amplitude compared to saline-treated mice (n/N = 4–6/5 cells/mice per group, p = 0.87, Student’s t-test). D, E sEPSC frequency nor amplitude are significantly different in MK-801 treated mice compared to saline-treated mice (3 to 4/4 cells/mice per group, p > 0.05 versus saline, Student’s t-test). F I/E ratio is significantly reduced in MK-801 treated mice compared to saline-treated mice (n/N = 3 to 4/4 cells/mice per group, p = 0.0005 versus saline, Student’s t-test). G Bath application of DHPG (30 μM) and MTEP (3 μM) significantly increases sIPSC frequency in both saline and MK-801 treated mice (n/N = 4–6/4 cells/mice per group, p < 0.0001 versus aCSF vehicle, two-way ANOVA, Bonferroni’s post-test). Bath application of the mGlu1 NAM, VU0469650 (3 μM), reverses the effects of DHPG and MTEP on sIPSC frequency in saline- and MK-801-treated mice (n/N = 2 to 3/3 cells/mice per group, p > 0.05 versus aCSF vehicle, two-way ANOVA, Bonferroni’s post-test). Open circle; female subjects. Filled circle; male subjects.
Based on evidence that selective activation of mGlu1 receptors increases output from SST-INs onto layer V pyramidal cells of the PFC [14], we further hypothesized that activation of mGlu1 would reverse deficits in sIPSC frequency and restore I/E balance in the PL-PFC of mice treated with MK-801. To this end, we bath applied the group I mGlu receptor agonist DHPG (30 µM) in the constant presence of the mGlu5 negative allosteric modulator (NAM) MTEP (3 µM) while recording sIPSCs onto PL-PFC layer V pyramidal cells from mice treated with MK-801 or saline (Fig. 1G). A two-way ANOVA revealed significant main effects of group, (F(1,97) = 4.71, p = 0.03; drug application, F(2,97) = 135.70, p < 0.0001) and interaction (F(2,97) = 5.89, p = 0.004) (Fig. 1G). Bonferroni post hoc analysis showed that DHPG and MTEP application significantly increased sIPSC frequency in both saline- (20.02 ± 1.26 Hz) and MK-801-treated mice (19.90 ± 0.72 Hz) compared to respective sIPSC frequencies in the presence of aCSF alone (saline: 11.13 ± 0.69; MK-801: 6.46 ± 0.41 Hz) (Fig. 1G, p < 0.0001, two-way ANOVA, Bonferroni’s post-test). Importantly, bath application of DHPG and MTEP in the presence of mGlu1 NAM VU0469650 (3 μM) blocked the effect of DHPG/MTEP application resulting in sIPSC frequencies in saline (8.51 ± 0.96 Hz) and MK-801 treated mice (8.09 ± 0.94Hz) comparable to those observed in the presence of aCSF alone (Fig. 1G, p > 0.05, two-way ANOVA, Bonferroni’s post-test). Furthermore, bath application of the mGlu1 PAM VU6004909 (10 µM) in the presence of a sub-effective concentration of DHPG (3 µM) and MTEP (3 µM) potentiates sIPSC frequency onto Layer V pyramidal cells in both saline and MK-801-treated mice (Supplementary Fig. 2). Importantly, VU6004909 application mitigates MK-801-induced deficits in sIPSC frequency compared to saline-treated mice. Together, these findings support the hypothesis that selective mGlu1 activation reverses deficits induced by MK-801 treatment on inhibitory signaling and restores I/E balance in the PL-PFC.
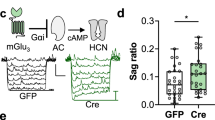
Acute MK-801 treatment induces inhibitory deficits onto PFC-BLA, but not PFC-NAc, projecting layer V pyramidal cells that are reversed by mGlu1 activation
PL-PFC pyramidal cells project to numerous brain regions, such as the nucleus accumbens (NAc) and basolateral amygdala (BLA), and their excitatory drive contributes to many complex behavioral outputs, including social interaction and cognition [30,31,32]. We were interested in understanding whether the effects of MK-801 on inhibitory signaling onto layer V pyramidal cells were expressed differentially across distinct projection populations. To address this question, we infused a retrograde AAV vector encoding a GFP tag into the NAc or BLA of mice and performed whole-cell recordings measuring sEPSCs and sIPSCs onto each of these subpopulations of layer V pyramidal cells 24 h following treatment with MK-801 or saline (Fig. 2). A two-way ANOVA revealed a significant main effect of group (F(1,56) = 8.10, p = 0.006) and interaction (F(1,56) = 35.59, p < 0.0001) (Fig. 2B). Bonferroni post hoc analysis showed that acute MK-801 treatment significantly reduced sIPSC frequency onto layer V pyramidal cells projecting to the BLA (6.08 ± 0.87 Hz) compared to saline-treated mice (14.43 ± 1.14 Hz) (Fig. 2B, p < 0.0001, two-way ANOVA, Bonferroni’s post-test). However, MK-801 treatment did not alter sIPSC frequency onto pyramidal cells projecting to the NAc (12.36 ± 0.92 Hz) compared to saline treatment (9.41 ± 0.76 Hz) (Fig. 2B, p = 0.18). Further, a two-way ANOVA revealed a significant main effect of projection (F(1,56) = 5.02, p = 0.03, and interaction, F(1,56) = 6.45, p = 0.01) (Fig. 2C). Bonferroni post hoc analysis showed that acute MK-801 treatment significantly reduced the amplitude of sIPSCs onto layer V pyramidal cells projecting to the BLA (13.53 ± 1.47 pA) compared to saline-treated mice (21.05 ± 1.64 pA) (Fig. 2C, p = 0.03). However, MK-801 treatment did not alter the amplitude of sIPSCs onto pyramidal cells projecting to the NAc (21.89 ± 2.44 pA) compared to saline-treated mice (20.52 ± 1.34 pA) (Fig. 2C, p > 0.99). The frequency and amplitude of sEPSCs onto BLA- or NAc-projecting pyramidal cells was not significantly different compared to saline-treated mice (Fig. 2D, E, p > 0.99, two-way ANOVA, Bonferroni post-test).
A Schematic depicting the approach for viral-mediated expression of GFP in NAc or BLA-projecting layer V pyramidal cells of the PL-PFC. A retrograde virus promoting the expression of a GFP tag was delivered to the NAc (bottom left) or BLA (bottom right) of male and female mice. Electrophysiology recordings were gathered from GFP-expressing layer V pyramidal cells of the PL-PFC (right). PL, prelimbic; IL, infralimbic. Scale bars, 1 μm. B MK-801 did not alter sIPSC frequency onto pyramidal cells projecting to the NAc (green bars) compared to saline-treated mice (n/N = 4 to 5/4 cells/mice per group, p = 0.18, two-way ANOVA, Bonferroni’s post-test). MK-801 treatment significantly reduced sIPSC frequency onto layer V pyramidal cells projecting to the BLA (purple bars) compared to saline-treated mice (n/N = 3–4/4 cells/mice per group, p < 0.0001 versus saline, two-way ANOVA, Bonferroni’s post-test). C MK-801 treatment decreased the amplitude of sIPSCs onto layer V pyramidal cells projecting to the BLA compared to saline-treated mice (n/N = 3–4/4 cells/mice per group, p = 0.03) but was not altered by MK-801 in NAc-projecting cells (n/N = 4–5/4 cells/mice per group, p > 0.99). D, E MK-801 treatment did not alter the frequency and amplitude of sEPSCs onto BLA- or NAc-projecting pyramidal cells compared to saline-treated mice (n/N = 3–5/3 cells/mice per group, p > 0.99, two-way ANOVA, Bonferroni post-test). F The I/E ratio of BLA-projecting cells was significantly reduced in MK-801 treated mice compared to saline-treated mice (n/N = 3–5/4 cells/mice per group, p = 0.0001). However, the I/E ratio of NAc-projecting cells was not altered by MK-801 treatment compared to saline-treated mice (n/N = 3–4/3 cells/mice per group, p > 0.99). G Bath application of DHPG in the presence of MTEP increased sIPSC frequency onto PFC-BLA (n/N = 2–4/4 cells/mice per group, p < 0.05, two-way ANOVA, Bonferroni’s post-test). Open circle; female subjects. Filled circle; male subjects.
We next determined if MK-801 treatment differentially affected I/E ratios of PFC-NAc or PFC-BLA-projecting cells (Fig. 2F). A two-way ANOVA revealed significant main effects of group (F(1,44) = 14.57, p = 0.0004; projection, F(1,44) = 6.80, p = 0.01), and interaction (F(1,44) = 6.60, p = 0.01) (Fig. 2F). Bonferroni post hoc analysis revealed that MK-801 treatment significantly decreased the I/E ratio of BLA-projecting cells (0.45 ± 0.06) compared to saline-treated mice (1.13 ± 0.08) (Fig. 2F, p = 0.0001), but the I/E ratio of NAc-projecting cells was not altered by MK-801 treatment compared to saline-treated mice (1.00 ± 0.12 vs. 1.13 ± 0.17, respectively) (Fig. 2F, p > 0.99).
To determine if selective mGlu1 activation reversed deficits in inhibitory signaling onto PL-PFC pyramidal cells projecting to the BLA, we bath applied DHPG (30 µM) in the constant presence of MTEP (3 µM) onto slices from mice treated with MK-801 or saline (Fig. 2G). For PFC-BLA projections, a two-way ANOVA revealed significant main effects of group (F(1,40) = 95.55, p < 0.0001) and drug application (F(1,40) = 20.19, p < 0.0001) (Fig. 2G). Bonferroni post hoc analysis showed that DHPG and MTEP application significantly increased sIPSC frequency onto PFC-BLA pyramidal cells in both saline- (27.46 ± 1.24 Hz) and MK-801-treated mice (22.34 ± 2.63 Hz) compared to respective sIPSC frequencies in the presence of aCSF alone (saline: 14.42 ± 1.14; MK-801: 6.08 ± 0.87 Hz) (Fig. 2G, p < 0.05, two-way ANOVA, Bonferroni’s post-test). Together, these results suggest that acute MK-801 administration may induce selective deficits in inhibitory signaling onto layer V pyramidal cells projecting from the PL-PFC to the BLA, but not the NAc, that are reversible by selective activation of mGlu1.
MK-801 induced impairments in sociability and social novelty preference are rescued by mGlu1 PAM VU6004909
A multitude of studies have demonstrated the ability of acute MK-801 administration to induce deficits in social behaviors, including social approach, recognition, and novelty preference [22, 33,34,35]. Additionally, PFC I/E balance has been shown to be a critical determinant of social behavior [5, 7], leading us to hypothesize that activation of mGlu1 receptors would restore deficits in social behavior induced by MK-801. Thus, we evaluated the behavioral efficacy of the mGlu1 PAM VU6004909 on sociability and social novelty preference following acute administration of MK-801 (0.18 mg/kg; i.p.) or saline (Fig. 3) using the three-chambered social approach task [36]. Twenty-four hours following MK-801 (0.18 mg/kg; i.p.) or saline injection, mice were administered VU6004909 (40 mg/kg; i.p.) or vehicle and then were tested in the three-chamber assay 30 min later. Interaction times (Fig. 3C, F) were calculated, and social interaction and novelty indexes were reported (Fig. 3B, E). In the first phase of the three-chambered social approach task, sociability is measured as interaction of the subject mouse in the chamber containing the novel target mouse as opposed to the chamber containing the empty cup (Fig. 3A). A two-way ANOVA revealed a significant main effect of group (F(1,90) = 5.29, p = 0.02) and interaction (F(1,90) = 6.05, p = 0.02)(Fig. 3B). Bonferroni post hoc analysis showed that MK-801 pretreated mice displayed a significantly lower social interaction index (0.52 ± 0.05) compared to control saline-treated mice (0.71 ± 0.02), indicating a deficit in sociability (Fig. 3B, p = 0.001, two-way ANOVA, Bonferroni’s post-test). Pretreatment of MK-801-treated mice with VU6004909 significantly increased social interaction index values compared to MK-801/vehicle-treated mice (0.67 ± .04 vs. 0.52 ± 0.05, respectively) (p = 0.04). Pretreatment of saline-treated mice with VU6004909 did not significantly alter the level of social interaction compared to saline/vehicle-treated control mice (0.67 ± 0.04 vs. 0.71 ± 0.02) (p > 0.99).
A Schematic of the 3-chamber apparatus used to assess social interaction. Twenty-four hours following MK-801 (0.18 mg/kg; i.p.) or saline injection, mice were administered VU6004909 (40 mg/kg; i.p.) or vehicle and then were tested in the three-chamber assay 30 min later. Sociability is measured as interaction of the subject mouse in the chamber containing the novel target mouse as opposed to the chamber containing the empty cup. B Social interaction indexes for mice treated with MK-801 or saline followed by administration of VU6004909 (40 mg/kg; i.p.) or vehicle (10% Tween-80). Mice treated with MK-801 displayed a significantly lower social interaction index compared to control saline-treated mice. VU6004909 administration in saline-treated mice did not significantly alter the level of social interaction compared to saline/vehicle-treated control mice (p > 0.99, two-way ANOVA, Bonferroni’s post-test). Pretreatment of MK-801 treated mice with VU6004909 resulted in levels of social interaction comparable to saline-treated mice (N = 18–32 mice/group, p = 0.001). C Raw interaction times with the empty cup and social stimulus. MK-801 treatment reduced interaction time with the social stimulus compared to saline-treated mice. Mice treated with MK-801 interacted with the empty cup and social stimulus for comparable amounts of time, demonstrating impaired social interaction. This deficit was mitigated by pretreatment with VU6004909 (N = 18-32 mice/group, p < 0.0001, two-way ANOVA, Bonferroni’s post-test). D Schematic of social novelty preference test phase which was measured as interaction of the subject mouse in the chamber containing the novel target mouse as opposed to the chamber containing a familiar mouse. E Novelty preference indexes were lower in MK-801 treated mice compared to saline-treated mice (N = 18–32 mice/group, p = 0.01, two-way ANOVA, Bonferroni’s post-test). VU6004909 administration in saline-treated mice did not significantly alter the level of social novelty preference compared to saline/vehicle-treated control mice (p > 0.99). Pretreatment of MK-801 treated mice with VU6004909 resulted in social novelty preference levels comparable to control saline-treated mice (p > 0.99). F Raw interaction times with the familiar and novel social stimuli. Saline-treated mice showed increased interaction with the novel social stimulus compared to the familiar social stimulus; however, MK-801 treated mice interacted with each social stimulus for a comparable amount of time. Saline and MK-801 treated mice showed increased interaction time with the novel social stimulus following VU6004909 administration (N = 18–32 mice/group, p > 0.99, two-way ANOVA, Bonferroni’s post-test). Open circle; female subjects. Filled circle; male subjects.
In the second phase of the three-chambered social approach task, social novelty preference is measured as interaction of the subject mouse in the chamber containing the novel target mouse as opposed to the chamber containing a familiar mouse (Fig. 3D). A two-way ANOVA revealed a significant main effect of treatment (F(1,89) = 4.33, p = 0.04) and interaction (F(1,89) = 4.39, p = 0.04)(Fig. 3E). Bonferroni post hoc analysis showed that MK-801 pretreated mice displayed a significantly lower novelty preference index (0.47 ± 0.02) compared to control saline-treated mice (0.58 ± 0.02), indicating a deficit in social novelty preference (Fig. 3E, p = 0.01, two-way ANOVA, Bonferroni’s post-test). Pretreatment of MK-801-treated mice with VU6004909 significantly increased social novelty preference levels compared to MK-801/vehicle-treated mice (0.59 ± 0.04 vs. 0.58 ± 0.02, respectively) (p = 0.02). Pretreatment of saline-treated mice with VU6004909 did not significantly alter the level of social novelty preference compared to saline/vehicle-treated control mice (0.58 ± 0.04 vs. 0.58 ± 0.02) (p > 0.99). Together, these findings suggest that the mGlu1 PAM VU6004909 effectively reverses MK-801 induced deficits in sociability and social novelty preference.
mGlu1 PAM VU6004909 improves novel object recognition following MK-801 treatment
It has previously been shown that NMDAR antagonism induces a wide array of cognitive deficits in mice, including novel object recognition (NOR) [21, 33, 37]. Thus, we sought to determine the efficacy of the mGlu1 PAM VU6004909 on NOR following administration of MK-801 (0.18 mg/kg; i.p.) or saline (Fig. 4A). Twenty-four hours following MK-801 or saline pretreatment, mice were administered VU6004909 (40 mg/kg; i.p.) or vehicle 30 min prior to NOR testing. A novelty recognition index (Fig. 4B) was calculated from interaction times with familiar and novel objects (Fig. 4C). A two-way ANOVA revealed a significant main effect of group (F(1,65) = 16.73, p = 0.0001) and interaction (F(1,65) = 5.58, p = 0.02) (Fig. 4B). Bonferroni post hoc analysis showed that mice treated with MK-801 displayed a significantly lower recognition index (−0.02 ± 0.12) compared to control saline-treated mice (0.62 ± 0.08), indicating a deficit in recognition memory (Fig. 4B, p = 0.0002, two-way ANOVA, Bonferroni’s post-test). Recognition index levels were improved by pretreatment with the mGlu1 PAM VU6004909 in MK-801-treated mice (0.34 ± 0.11) to levels comparable to recognition index levels observed with vehicle pretreatment in saline mice (0.62 ± 0.08) (p > 0.99). Pretreatment of saline-treated mice with VU6004909 did not significantly alter the level of recognition memory compared to vehicle administration in saline-treated mice (VU’4909: 0.51 ± 0.08 vs. Veh: 0.62 ± 0.08) (p > 0.99). Additionally, recognition index values were not significantly different between saline (0.51 ± 0.08) or MK-801 (0.34 ± 0.11) mice following VU6004909 treatment (p > 0.99). Total distance traveled during the NOR task did not differ between any groups (Supplementary Fig. 3). Together, these findings suggest that MK-801 induces deficits in NOR which can be reversed by mGlu1 PAM VU6004909 treatment.
A The NOR assay was used to assess short-term recognition memory as measured by the amount of time a mouse spent interacting with one familiar and one novel object. B Novelty preference index of mice treated with MK-801 or saline followed by administration of VU6004909 (40 mg/kg; i.p.) or vehicle (10% Tween-80). Mice treated with MK-801 displayed a significantly lower recognition index compared to control saline-treated mice (N = 16–19 mice/group, p = 0.0002 versus saline/vehicle, two-way ANOVA, Bonferroni’s post-test). Pretreatment with VU6004909 in MK-801 treated mice resulted in recognition index levels comparable to saline-treated mice following administration with either vehicle or VU6004909 (p > 0.99). C Raw interaction times with the novel or familiar objects. Saline-treated mice interacted with the novel object for a greater duration of time compared to the familiar object following pretreatment with vehicle or VU6004909 (N = 16–19 mice/group, p < 0.05 versus familiar object, two-way ANOVA, Bonferroni’s post-test). However, mice treated with MK-801 interacted with the novel and familiar objects for comparable amounts of time (p > 0.99). MK-801 treated mice displayed a trend toward lower interaction time with the familiar object compared to the novel object, suggesting that VU6004909 may improve deficits in NOR elicited by MK-801. Open circle; female subjects. Filled circle; male subjects.
Discussion
In this study, we show for the first time that selective activation of mGlu1 reverses cortical disinhibition and behavioral deficits induced by NMDAR antagonism. Specifically, mGlu1 activation restored inhibitory signaling onto pyramidal cells of the PL-PFC, including BLA-projecting cells which displayed notable disinhibition following NMDAR antagonism. In line with these findings, we found that mGlu1 PAMs elicit potent prosocial and procognitive effects, mitigating NMDAR antagonist-induced behavioral impairments. The present findings not only highlight the potential utility of mGlu1 PAMs in improving cognition and social impairment for the treatment of schizophrenia but also provide important insights into mGlu1 receptor-mediated mechanisms underlying physiological and behavioral processes relevant to schizophrenia.
The balance between inhibitory and excitatory signaling in the PFC is known to be a critical determinant of many complex behavioral outputs, including social behavior and cognition. Notably, I/E imbalance is a hallmark of numerous neuropsychiatric diseases, including schizophrenia. NMDA antagonist models have been widely used in rodents to recapitulate physiological and behavioral impairments associated with schizophrenia [19], including disrupted I/E balance [38, 39]. The majority of these studies have focused on the acute effects of a single dose of NMDA antagonists, such as MK-801 or ketamine subsequently following administration. Despite many studies investigating the short-term effects of MK-801 administration (0–2 h post-administration), there is evidence that a single dose of MK-801 is able to produce behavioral deficits persisting as long as 24 h. For instance, administration of MK-801 (0.03–0.6 mg/kg) produced significant deficits in memory retention that persisted 24 h later in spatial or cued water maze as well as passive avoidance tasks in mice [40, 41]. These findings suggest that MK-801 may elicit cognitive and behavioral deficits for an extended period following administration; however, the persistent physiological consequences of 24 h following MK-801 administration that may drive these behavioral and cognitive deficits are currently unknown. Based on these observations, we hypothesized that MK-801 administration may induce persistent deficits in cortical I/E balance after 24 h. In the present study, we show that acute treatment with MK-801 reduces inhibitory transmission onto layer V pyramidal cells within the PL-PFC. Importantly, these deficits are effectively reversed by selective activation of mGlu1. I/E balance within the PFC depends upon the intricate interplay between glutamatergic excitatory neurons and a variety of subtypes of GABAergic inhibitory INs, including SST-INs, PV-INs and vasoactive intestinal peptide-expressing interneurons (VIP-INs) [42]. Recently, we reported that mGlu1 activation enhances inhibitory neurotransmission in the PL-PFC largely via actions on SST-INs [14]. Therefore, we postulate that impaired inhibitory transmission in the PFC following MK-801 treatment is likely driven by a reduction in SST-IN output, and activation of mGlu1 reverses these deficits by selectively enhancing SST-IN activity. In support of this notion, systemic MK-801 administration in rodents increases pyramidal neuron firing and suppresses SST-IN activity in the PFC [23, 43]. Based on their morphology and firing patterns, SST-INs can be further categorized into Martinotti and non-Martinotti cells [42]. Although it is possible that a combination of these cell-types could contribute to our observed effects of MK-801 on pyramidal cell inhibition, non-Martinotti cells may be a critical population engaged due to their constitutive activation via NMDARs. Furthermore, SST-INs have been shown to directly inhibit excitatory pyramidal cells as well as PV-INs [44]. Therefore, we cannot rule out the contribution of PV-INs in the effects of mGlu1 activation on cortical disinhibition induced by MK-801. Studies using mice deficient in NMDAR-subunit GluN1 in PV-INs have shown blunted induction of MK-801 behavioral effects [45, 46], providing evidence that MK-801 may elicit direct effects on PV-INs. However, previous studies demonstrate that the NMDAR contribution to excitatory transmission onto SST-INs is stronger compared to PV-INs [47,48,49]. Together, this suggests that SST-INs may be more susceptible to NMDA receptor antagonism and are the primary cellular mechanism underlying mGlu1-mediated restoration of I/E balance in the PFC. Nonetheless, future studies will be critical for empirically evaluating the role of PV-INs as well as vasoactive intestinal peptide-expressing interneurons (VIP-INs) in NMDAR antagonist models of cortical disinhibition and reversal of inhibitory deficits by mGlu1 activation.
Ample preclinical and clinical evidence supports a critical role of the PFC I/E balance in the regulation of social behavior. Here, we found that an mGlu1 PAM effectively reversed MK-801-induced deficits in social interaction and preference for social novelty using the three-chamber assay. Based on recent evidence that selective activation of mGlu1 receptors enhances cortical inhibitory signaling through actions on PFC SST-INs [14], the prosocial effects of mGlu1 PAMs likely occur through restoration of cortical inhibition driven by SST-INs. Evidence demonstrating that heightened PFC pyramidal excitation can reduce social interaction in mice as measured by the three-chamber test [50] supports this notion. Recently, it was also reported that synchronized activation of PFC SST-INs selectively induces social discrimination [51]. Furthermore, impaired SST-IN excitability has been directly linked to social interaction and social novelty preference deficits in mice [52]. SST-INs can influence pyramidal cell activity directly or inhibit PV-INs, resulting in perisomatic inhibition of pyramidal neurons [53]. Thus, the ability of mGlu1 PAMs to promote social behavior could be driven by their direct effects on SST-INs to increase inhibition of pyramidal neurons but could also rely on SST-IN mediated inhibition of PV + cell activity. Future interrogation is necessary to directly determine the cell type-specific mechanisms driving the prosocial efficacy of mGlu1 PAMs.
Excitatory projections from the PFC to brain regions such as the BLA and NAc orchestrate distinct aspects of social behavior. For example, a recent study using optogenetic and chemogenetic approaches has demonstrated that activation of BLA-projecting cells from the PL-PFC impairs social behavior in mice [54]. Although the BLA contains distinct subsets of neurons known to encode positive or negative valence [55, 56], there is substantial evidence that PL-PFC to BLA circuit is particularly critical to encoding negative valence. For instance, PL-PFC cells projecting to the BLA are robustly activated following foot shock [54]. Thus, we propose that disinhibition of this circuit via NMDA antagonism could produce a negative emotional state that promotes social avoidance and diminished social preference that could be reversed via mGlu1 receptor-driven enhancement of inhibitory signaling in the PFC. In line with this notion, we found that MK-801 produced deficits in inhibitory signaling onto cells projecting from the PL-PFC to the BLA but not those projecting to the NAc. Additionally, selective activation of mGlu1 reversed MK-801-induced deficits in inhibitory signaling onto PFC-BLA pyramidal cells which paralleled the ability of an mGlu1 PAM to effectively reverse deficits in social behavior induced by MK-801 treatment. Together, these results provide compelling evidence that mGlu1-mediated enhancement of PFC inhibitory tone represents a novel mechanism to balance excitatory signaling in the BLA and restore social behavior.
In addition to PFC-BLA projections, many studies highlight the importance of projections from PL-PFC to the NAc in encoding social information. One study showed that activation of NAc-projecting PL-PFC neurons significantly reduced preference for a social target [57]. Similarly, we found that selective activation of mGlu1 increased inhibition onto this subset of cells in both saline- and MK-801-treated mice (Supplementary Fig. 4). Thus, it is possible that mGlu1-mediated dampening of excitatory drive into the NAc, in addition to normalization of hyperexcitable inputs into the BLA following MK-801 treatment, may also contribute to the ability of mGlu1 PAMs to promote social behavior. Inhibition of PFC-BLA circuits may reduce negative emotional states that reduce social interaction, while reducing excitation of PFC-NAc circuits may promote social learning. Furthermore, corticostriatal and corticoamygdalar circuits are known to regulate distinct aspects of social behavior. Based on this evidence, it is possible that mGlu1 PAMs may promote social behavior by normalizing multiple processes that govern social behavior. However, future studies are needed to delineate the circuit-specific contributions of mGlu1 receptors in various facets of social behavior, including social learning, memory, and emotional contributions involved in sociability, and provide additional insights to the prosocial effects of mGlu1 PAMs.
Because cortical inhibition is critical to many forms of cognition, including recognition of novel and salient stimuli and short-term memory [58,59,60], it is possible that mGlu1 receptor-mediated enhancement of cortical inhibition with mGlu1 PAMs may elicit procognitive effects in assays of non-social cognition. In concordance with a wealth of existing literature [28, 33, 61,62,63,64], we found that NMDAR antagonism produces robust deficits in both social and non-social forms of recognition memory. Specifically, administration of an mGlu1 PAM partially restored deficits in NOR elicited by MK-801 treatment. These findings agree with existing literature highlighting a role of mGlu1 receptors in non-social recognition memory. For example, it has previously been reported that recognition memory is impaired in mGlu1 knockout mice [65]. However, this effect was only present in measures of long-term, but not short-term, recognition memory. Here, we primarily engaged short-term recognition memory as NOR was measured following a 1 h delay period, providing divergent evidence that activation of mGlu1 may also enhance short-term, non-social recognition memory. Future studies are required to determine if mGlu1 PAMs also enhance long-term recognition memory. In addition, questions remain regarding the efficacy of mGlu1 PAMs in additional forms of cognition and the distinct mechanisms by which mGlu1 receptor activation selectively reverses social and non-social deficits.
The current findings provide critical physiological and behavioral evidence in support of the hypothesis that mGlu1 PAMs enhance social and cognitive function by increasing cortical inhibition. Based on recent compelling evidence that mGlu1 receptors regulate cortical inhibition via actions on SST-INs of the PL-PFC [14], it is likely that the prosocial and cognitive-enhancing properties of mGlu1 PAMs reported in the present study occur via actions on SST-INs. Despite this strong evidence, it is also plausible that the actions of mGlu1 PAMs on additional populations of mGlu1 receptors may also contribute to the cognitive and social enhancing effects of these agents. For example, studies using mGlu1–/– mice have demonstrated a critical role of mGlu1 in promoting hippocampal LTP which correlates with deficits in context-specific learning. Moreover, impaired hippocampal synaptic plasticity has also been implicated as a critical mechanism driving NMDAR antagonist-induced deficits in NOR as local administration of the competitive NMDAR antagonist DL-2-amino-5-phosphonovaleric acid (APV), which impairs recognition of novel objects, selectively blocked LTP into the dorsal hippocampus of rats [66]. These findings suggest that the actions of mGlu1 PAMs on hippocampal mGlu1 receptor populations may also contribute to their procognitive efficacy. Additional studies could further determine the respective contributions of extracortical mGlu1 receptor populations in the procognitive efficacy of mGlu1 PAMs.
The present study provides novel evidence for the prosocial and cognitive-enhancing profiles of mGlu1 PAMs and argues that mGlu1 receptors play a critical role in regulating cortical inhibition that is essential to various forms of social and non-social behavioral and cognitive processes. Future studies investigating the efficacy of mGlu1 PAMs in improving other behavioral and cognitive deficits will provide critical information about the therapeutic potential of these agents for the treatment of schizophrenia.
Change history
14 July 2023
The author P. Jeffrey Conn was tagged incorrectly in the HTML version of the original article.
References
Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: overview and treatment options. P T. 2014;39:638–45.
Jablensky A. The diagnostic concept of schizophrenia: its history, evolution, and future prospects. Dialogues Clin Neurosci. 2010;12:271–87.
Stępnicki P, Kondej M, Kaczor AA. Current concepts and treatments of schizophrenia. Molecules. 2018;23:2087.
Szczepanski SM, Knight RT. Insights into human behavior from lesions to the prefrontal cortex. Neuron 2014;83:1002–18.
Bicks LK, Koike H, Akbarian S, Morishita H. Prefrontal cortex and social cognition in mouse and man. Front Psychol. 2015;6:1805.
Ghosal S, Hare B, Duman RS. Prefrontal cortex GABAergic deficits and circuit dysfunction in the pathophysiology and treatment of chronic stress and depression. Curr Opin Behav Sci. 2017;14:1–8.
Paine TA, Swedlow N, Swetschinski L. Decreasing GABA function within the medial prefrontal cortex or basolateral amygdala decreases sociability. Behav Brain Res. 2017;317:542–52.
de Jonge JC, Vinkers CH, Hulshoff Pol HE, Marsman A. GABAergic mechanisms in schizophrenia: Linking Postmortem and in vivo studies. Front Psychiatry. 2017;8:118.
Schoonover KE, Dienel SJ, Lewis DA. Prefrontal cortical alterations of glutamate and GABA neurotransmission in schizophrenia: Insights for rational biomarker development. Biomark Neuropsychiatry. 2020;3:100015.
Hashimoto T, Volk DW, Eggan SM, Mirnics K, Pierri JN, Sun Z, et al. Gene expression deficits in a subclass of GABA neurons in the prefrontal cortex of subjects with schizophrenia. J Neurosci. 2003;23:6315–26.
Thompson M, Weickert CS, Wyatt E, Webster MJ. Decreased glutamic acid decarboxylase(67) mRNA expression in multiple brain areas of patients with schizophrenia and mood disorders. J Psychiatr Res. 2009;43:970–7.
Woo TU, Kim AM, Viscidi E. Disease-specific alterations in glutamatergic neurotransmission on inhibitory interneurons in the prefrontal cortex in schizophrenia. Brain Res. 2008;1218:267–77.
Ferguson BR, Gao WJ. Thalamic control of cognition and social behavior via regulation of gamma-aminobutyric acidergic signaling and excitation/inhibition balance in the medial prefrontal cortex. Biol Psychiatry. 2018;83:657–69.
Maksymetz J, Byun N, Luessen DJ, Li B, Barry R, Gore J, et al. mGlu1 potentiation enhances prelimbic somatostatin interneuron activity to rescue schizophrenia-like physiological and cognitive deficits. Cell Rep. 2022;37:109950.
López-Bendito G, Shigemoto R, Fairén A, Luján R. Differential distribution of group I metabotropic glutamate receptors during rat cortical development. Cereb Cortex. 2002;12:625–38.
Muly EC, Maddox M, Smith Y. Distribution of mGluR1alpha and mGluR5 immunolabeling in primate prefrontal cortex. J Comp Neurol. 2003;467:521–35.
Tasic B, Yao Z, Graybuck LT, Smith KA, Nguyen TN, Bertagnolli D, et al. Shared and distinct transcriptomic cell types across neocortical areas. Nature 2018;563:72–8.
Sun H, Neugebauer V. mGluR1, but not mGluR5, activates feed-forward inhibition in the medial prefrontal cortex to impair decision making. J Neurophysiol. 2011;106:960–73.
Lee G, Zhou Y. NMDAR hypofunction animal models of schizophrenia. Front Mol Neurosci. 2019;12:185.
Nakazawa K, Sapkota K. The origin of NMDA receptor hypofunction in schizophrenia. Pharmacol Ther. 2020;205:107426.
Hoffman KL, Basurto E. Clozapine and glycinamide prevent MK-801-induced deficits in the novel object recognition (NOR) test in the domestic rabbit (Oryctolagus cuniculus). Behav Brain Res. 2014;271:203–11.
Moy SS, Nonneman RJ, Shafer GO, Nikolova VD, Riddick NV, Agster KL, et al. Disruption of social approach by MK-801, amphetamine, and fluoxetine in adolescent C57BL/6J mice. Neurotoxicol Teratol. 2013;36:36–46.
Homayoun H, Moghaddam B. NMDA receptor hypofunction produces opposite effects on prefrontal cortex interneurons and pyramidal neurons. J Neurosci. 2007;27:11496–500.
Garcia-Barrantes PM, Cho HP, Metts AM, Blobaum AL, Niswender CM, Conn PJ, et al. Lead optimization of the VU0486321 series of mGlu(1) PAMs. Part 2: SAR of alternative 3-methyl heterocycles and progress towards an in vivo tool. Bioorg Med Chem Lett. 2016;26:751–56.
Garcia-Barrantes PM, Cho HP, Blobaum AL, Niswender CM, Conn PJ, Lindsley CW. Lead optimization of the VU0486321 series of mGlu1 PAMs. Part 3. Engineering plasma stability by discovery and optimization of isoindolinone analogs. Bioorg Med Chem Lett. 2016;26:1869–72.
Joffe ME, Winder DG, Conn PJ. Contrasting sex-dependent adaptations to synaptic physiology and membrane properties of prefrontal cortex interneuron subtypes in a mouse model of binge drinking. Neuropharmacology. 2020;178:108126.
Nadler JJ, Moy SS, Dold G, Trang D, Simmons N, Perez A, et al. Automated apparatus for quantitation of social approach behaviors in mice. Genes Brain Behav. 2004;3:303–14.
Ghoshal A, Rook JM, Dickerson JW, Roop GN, Morrison RD, Jalan-Sakrikar N, et al. Potentiation of M1 muscarinic receptor reverses plasticity deficits and negative and cognitive symptoms in a schizophrenia mouse model. Neuropsychopharmacology. 2016;41:598–610.
Javitt DC, Zukin SR. Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry. 1991;148:1301–8.
Riga D, Matos MR, Glas A, Smit AB, Spijker S, Van den Oever MC. Optogenetic dissection of medial prefrontal cortex circuitry. Front Syst Neurosci. 2014;8:230.
Xu P, Chen A, Li Y, Xing X, Lu H. Medial prefrontal cortex in neurological diseases. Physiol Genomics. 2019;51:432–42.
Gunaydin LA, Grosenick L, Finkelstein JC, Kauvar IV, Fenno LE, Adhikari A, et al. Natural neural projection dynamics underlying social behavior. Cell. 2014;157:1535–51.
Cieślik P, Radulska A, Pelikant-Małecka I, Płoska A, Kalinowski L, Wierońska JM. Reversal of MK-801-induced disruptions in social interactions and working memory with simultaneous administration of LY487379 and VU152100 in mice. Int J Mol Sci. 2019;20:2781.
Zou H, Zhang C, Xie Q, Zhang M, Shi J, Jin M, et al. Low dose MK-801 reduces social investigation in mice. Pharm Biochem Behav. 2008;90:753–7.
Rung JP, Carlsson A, Rydén Markinhuhta K, Carlsson ML. (+)-MK-801 induced social withdrawal in rats; a model for negative symptoms of schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2005;29:827–32.
Yang M, Silverman JL, Crawley JN. Automated three-chambered social approach task for mice. Curr Protoc Neurosci. 2011;Chapter 8:Unit 8.26.
Nilsson M, Hansson S, Carlsson A, Carlsson ML. Differential effects of the N-methyl-d-aspartate receptor antagonist MK-801 on different stages of object recognition memory in mice. Neuroscience. 2007;149:123–30.
Widman AJ, McMahon LL. Disinhibition of CA1 pyramidal cells by low-dose ketamine and other antagonists with rapid antidepressant efficacy. Proc Natl Acad Sci USA. 2018;115:E3007–E16.
Povysheva NV, Johnson JW. Effects of memantine on the excitation-inhibition balance in prefrontal cortex. Neurobiol Dis. 2016;96:75–83.
Packard MG, Teather LA. Posttraining injections of MK-801 produce a time-dependent impairment of memory in two water maze tasks. Neurobiol Learn Mem. 1997;68:42–50.
Kruk-Slomka M, Biala G. Cannabidiol attenuates MK-801-induced cognitive symptoms of schizophrenia in the passive avoidance test in mice. Molecules. 2021;26:5977.
Tremblay R, Lee S, Rudy B. GABAergic interneurons in the neocortex: from cellular properties to circuits. Neuron. 2016;91:260–92.
Ali F, Gerhard DM, Sweasy K, Pothula S, Pittenger C, Duman RS, et al. Ketamine disinhibits dendrites and enhances calcium signals in prefrontal dendritic spines. Nat Commun. 2020;11:72.
Swanson OK, Maffei A. From hiring to firing: activation of inhibitory neurons and their recruitment in behavior. Front Mol Neurosci. 2019;12:168.
Bygrave AM, Masiulis S, Nicholson E, Berkemann M, Barkus C, Sprengel R, et al. Knockout of NMDA-receptors from parvalbumin interneurons sensitizes to schizophrenia-related deficits induced by MK-801. Transl Psychiatry. 2016;6:e778.
Hudson MR, Sokolenko E, O’Brien TJ, Jones NC. NMDA receptors on parvalbumin-positive interneurons and pyramidal neurons both contribute to MK-801 induced gamma oscillatory disturbances: complex relationships with behaviour. Neurobiol Dis. 2020;134:104625.
McGarry LM, Carter AG. Inhibitory gating of basolateral amygdala inputs to the prefrontal cortex. J Neurosci. 2016;36:9391–406.
Rotaru DC, Yoshino H, Lewis DA, Ermentrout GB, Gonzalez-Burgos G. Glutamate receptor subtypes mediating synaptic activation of prefrontal cortex neurons: relevance for schizophrenia. J Neurosci. 2011;31:142–56.
Wang HX, Gao WJ. Cell type-specific development of NMDA receptors in the interneurons of rat prefrontal cortex. Neuropsychopharmacology. 2009;34:2028–40.
Yizhar O, Fenno LE, Prigge M, Schneider F, Davidson TJ, O’Shea DJ, et al. Neocortical excitation/inhibition balance in information processing and social dysfunction. Nature. 2011;477:171–8.
Scheggia D, Managò F, Maltese F, Bruni S, Nigro M, Dautan D, et al. Somatostatin interneurons in the prefrontal cortex control affective state discrimination in mice. Nat Neurosci. 2020;23:47–60.
Chen D, Wang C, Li M, She X, Yuan Y, Chen H, et al. Loss of Foxg1 Impairs the development of cortical SST-interneurons leading to abnormal emotional and social behaviors. Cereb Cortex. 2019;29:3666–82.
Kubota Y. Untangling GABAergic wiring in the cortical microcircuit. Curr Opin Neurobiol. 2014;26:7–14.
Huang WC, Zucca A, Levy J, Page DT. Social behavior is modulated by valence-encoding mPFC-amygdala sub-circuitry. Cell Rep. 2020;32:107899.
Beyeler A, Namburi P, Glober GF, Simonnet C, Calhoon GG, Conyers GF, et al. Divergent routing of positive and negative information from the amygdala during memory retrieval. Neuron 2016;90:348–61.
Kim J, Pignatelli M, Xu S, Itohara S, Tonegawa S. Antagonistic negative and positive neurons of the basolateral amygdala. Nat Neurosci. 2016;19:1636–46.
Murugan M, Jang HJ, Park M, Miller EM, Cox J, Taliaferro JP, et al. Combined social and spatial coding in a descending projection from the prefrontal cortex. Cell 2017;171:1663–77.e16.
Auger ML, Floresco SB. Prefrontal cortical GABA modulation of spatial reference and working memory. Int J Neuropsychopharmacol. 2014;18:pyu013.
Thanapreedawat P, Kobayashi H, Inui N, Sakamoto K, Kim M, Yoto A, et al. GABA affects novel object recognition memory and working memory in rats. J Nutr Sci Vitaminol. 2013;59:152–7.
Morici JF, Bekinschtein P, Weisstaub NV. Medial prefrontal cortex role in recognition memory in rodents. Behav Brain Res. 2015;292:241–51.
Dogra S, Stansley BJ, Xiang Z, Qian W, Gogliotti RG, Nicoletti F, et al. Activating mGlu 3 metabotropic glutamate receptors rescues schizophrenia-like cognitive deficits through metaplastic adaptations within the hippocampus. Biol Psychiatry. 2021;90:385–98.
Liu X, Li J, Guo C, Wang H, Sun Y, Su YA, et al. Olanzapine reverses MK-801-induced cognitive deficits and region-specific alterations of NMDA receptor subunits. Front Behav Neurosci. 2017;11:260.
Horio M, Fujita Y, Hashimoto K. Therapeutic effects of metabotropic glutamate receptor 5 positive allosteric modulator CDPPB on phencyclidine-induced cognitive deficits in mice. Fundam Clin Pharmacol. 2013;27:483–8.
Griebel G, Pichat P, Boulay D, Naimoli V, Potestio L, Featherstone R, et al. The mGluR2 positive allosteric modulator, SAR218645, improves memory and attention deficits in translational models of cognitive symptoms associated with schizophrenia. Sci Rep. 2016;6:35320.
Kishimoto Y, Fujimichi R, Araishi K, Kawahara S, Kano M, Aiba A, et al. mGluR1 in cerebellar Purkinje cells is required for normal association of temporally contiguous stimuli in classical conditioning. Eur J Neurosci. 2002;16:2416–24.
Baker KB, Kim JJ. Effects of stress and hippocampal NMDA receptor antagonism on recognition memory in rats. Learn Mem. 2002;9:58–65.
Funding
Research was supported by the National Institutes of Health grants MH119673, NS031373, and MH062646 to PJC and MH065215 to DJL. The authors thank the William K. Warren Foundation for endowing the WCNDD. Behavioral experiments were performed using the Vanderbilt University Medical Center Murine Neurobehavior Core and Cell Imaging Shared Resource. The illustrative graphics were created with BioRender.com.
Author information
Authors and Affiliations
Contributions
Conceptualization: DJL; investigation: DJL, IMG, ASF; resources: BJM and CWL; supervision: DJL, DJF, CMN, and PJC; writing–original draft: DJL; writing–review and editing: all authors.
Corresponding authors
Ethics declarations
Competing interests
PJC, CWL, and CMN receive research support from Boehringer Ingelheim and Acadia Pharmaceuticals. CWL also receives support from Ono Pharmaceutical. PJC, CWL, and CMN are inventors on multiple patents for allosteric modulators of metabotropic glutamate receptors. All other authors declare no potential conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Luessen, D.J., Gallinger, I.M., Ferranti, A.S. et al. mGlu1-mediated restoration of prefrontal cortex inhibitory signaling reverses social and cognitive deficits in an NMDA hypofunction model in mice. Neuropsychopharmacol. 47, 1826–1835 (2022). https://doi.org/10.1038/s41386-022-01350-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41386-022-01350-0