Abstract
Background:
Vasopressin is a systemic vasoconstrictor. Its pulmonary vasodilatory effect is controversial, and limited data are available on its use in neonates with pulmonary hypertension. Hypothesizing that the vasopressin-induced pulmonary vasodilation is developmentally regulated, we evaluated its pulmonary and systemic arterial response in newborn and adult rats.
Methods:
Vessels were mounted on a wire myograph, and the vasopressin-induced changes in vasomotor tone measured. The vessel- and age-dependent differences in vasopressin V1a and V2 receptors’ expression were evaluated by western blotting.
Results:
Vasopressin induced a dose-dependent increase in mesenteric arterial tone at both ages, but of greater magnitude in adult vessels (P < 0.01). At lower concentrations, vasopressin induced pulmonary vasodilation in adult vessels and vasoconstriction in newborn arteries. The adult vasopressin-induced pulmonary vasodilation was inhibited by ibuprofen, suggesting that the response is prostaglandin mediated. Pulmonary tissue V1a receptor protein expression was higher in adult, when compared with newborn arteries (P < 0.01). The adult vessels V1a expression predominated in the pulmonary arteries, and V2 was only detected in mesenteric arteries.
Conclusion:
The vasopressin-induced pulmonary vasodilation is absent in newborn rats likely due to the lower tissue V1a expression early in life. These animal data challenge the therapeutic use of vasopressin in neonatal pulmonary hypertension.
Similar content being viewed by others
Main
Vasopressin, also known as 8-arginine-vasopressin or anti-diuretic hormone, is of a neurohypophysial origin and has an important neurotransmitter role on the control of circadian rhythm, thermoregulation, and adrenocorticotropic hormone release (1). Aside from these central effects, vasopressin acts in a circulation-specific manner to modulate vascular tone. It induces systemic vasoconstriction, and this effect led to its therapeutic use in clinical conditions where reduced systemic vascular resistance is a concern, such as septic shock (1,2). Yet, vasopressin has also been shown to reduce pulmonary vascular resistance in human and animals (3,4,5,6) leading to its use in the treatment of pulmonary arterial hypertension in adults (3,4). A recent review of the available clinical literature did not find sufficient evidence to recommend vasopressin as a pulmonary vasodilator in adults (7).
Persistent pulmonary hypertension syndrome of the newborn (PPHN) is a clinical condition associated with high morbidity and mortality (8). Inhaled nitric oxide remains the preferred therapeutic strategy to treat infants with the PPHN syndrome given its preferential vasodilatory effect on the pulmonary vasculature (8). Yet, a number of pharmacological agents are also commonly utilized in the treatment of this disorder (8). In spite of limited data to justify its clinical use as a pulmonary vasodilator, vasopressin has been employed in the treatment of infants with PPHN syndrome (9).
Aside from the paucity of data in support of the therapeutic use of vasopressin in the infants with pulmonary hypertension, there is reason to dispute the claim of this drug having a pulmonary vasodilatory effect early in life. In rats, the tissue vasopressin receptors’ mRNA expression is developmentally regulated, and the V1a subunit potentially involved in its vasodilatory response is not present in newborn lungs (10).
Therefore, the purpose of the present study was to conduct an in vitro comparative evaluation of the effect of vasopressin on the pulmonary and systemic vascular tone of newborn and adult rats. We hypothesized that vasopressin does not have a pulmonary vasodilatory effect in the newborn.
Results
Vasopressin Effect on Mesenteric and Pulmonary Arterial Vasomotor Tone
We first evaluated the vasopressin dose response in adult mesenteric and pulmonary arteries without any agonist-induced prestimulation. Vasopressin induced contraction of mesenteric arterial smooth muscle but had no effect on the pulmonary arteries ( Figure 1 ).
Vasopressin effect in adult pulmonary and mesenteric arteries without agonist-induced tone. Non-precontracted adult pulmonary (n = 4) and mesenteric arteries (n = 4) response to vasopressin. Open circles indicate pulmonary artery; solid circles indicate mesenteric artery. *P < 0.05 by one-way ANOVA with repeated measures and Fisher’s least-square difference multiple-comparison test.
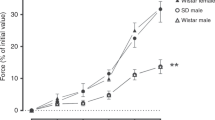
To further evaluate the potential relaxant effect of vasopressin, all subsequent dose–response measurements were obtained in vessels precontracted with the previously determined EC75 U46619 concentration. In mesenteric arteries, vasopressin induced a dose-dependent increase in smooth muscle contraction that was maximal for both ages at 6 × 10−9 mol/l ( Figure 2a ). In contrast, the vasopressin effect on the pulmonary arterial vasomotor tone was age dependent ( Figure 2b ). Whereas an incremental dose-dependent relaxation was observed in the adult arteries, vasopressin induced a dual response in the newborn pulmonary vessels. In the latter, vasopressin stimulation led to pulmonary arterial muscle contraction that was maximal at 3 × 10−9 mol/l, and vasorelaxation was only observed at the highest tested concentration (6 × 10−7 mol/l).
Vasopressin induced vasomotor tone changes in newborn and adult pulmonary and mesenteric arteries. Vasopressin dose response in thromboxane A2 analog (U46619) precontracted (EC75 concentration) (a) newborn and adult mesenteric (n = 4 each) and (b) newborn and adult pulmonary arteries (newborn, n = 6; adult, n = 8). The vasopressin-induced changes are expressed as percentage of precontraction force values. Positive values indicate vasopressin-induced contraction, and negative values indicate vasorelaxation. Open circles indicate newborn; solid circles indicate adult. **P< 0.01 vs. respective initial 10−12 mol/l values by two-way ANOVA and Tukey–Kramer multiple-comparison test.
Since tachyphylaxis has been reported in vasopressin-stimulated vessels in vitro, we evaluated the mesenteric and pulmonary arterial response to a single high concentration of the drug (6 × 10−7 mol/l). The vasopressin response to the single dose was similar to the one observed following multiple incremental concentrations. In mesenteric arteries, only muscle contraction was observed at both ages, whereas in the pulmonary tissue, vasorelaxation was seen in adult vessels and the opposite in the newborn arteries ( Figure 3 ).
Vasopressin single-dose effect on newborn and adult pulmonary and mesenteric arterial tone. Single concentration (6 × 10−7 mol/l) of vasopressin induced force in (a) newborn and adult mesenteric (newborn, n = 3; adult, n = 4) and (b) newborn and adult pulmonary arteries (newborn, n = 4; adult, n = 4) precontracted with thromboxane A2 analog (U46619 (EC75 concentration). Vasopressin-induced response is expressed as percentage change from U46619-induced force, and negative values indicate relaxation. **P < 0.01 vs. newborn values by unpaired Student’s t-test.
Mechanism Accounting for the Vasopressin-Induced Pulmonary Vasorelaxation
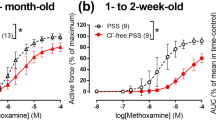
We further proceeded to investigate the mechanism involved in the vasopressin-induced relaxation of adult pulmonary arteries. Two main pathways have been suggested as being involved in the regulation of vasopressin-induced vasodilation: endothelium-dependent nitric oxide synthase–derived nitric oxide and vasodilating prostaglandins (11,12). As such, we evaluated the impact of inhibitors of both pathways on the vasopressin-induced pulmonary vasodilatory response. The cyclooxygenase inhibitor ibuprofen, but not the nitric oxide synthase blocker Nω-nitro-L-arginine methyl ester hydrochloride, significantly (P < 0.01) inhibited the vasopressin-induced pulmonary vasorelaxation ( Figure 4 ). In the presence of ibuprofen, vasopressin induced pulmonary vasorelaxation at concentrations 3 × 10−7 and 6 × 10−7 mol/l, yet of a lesser magnitude when compared with untreated control vessels.
Vasopressin pulmonary vasodilatory effect and cyclooxygenase/nitric oxide synthase inhibition. Vasopressin dose response in thromboxane A2 analog (U46619) precontracted (EC75 concentration) adult pulmonary arteries in the absence (control; n = 8) and presence of either the cyclooxygenase inhibitor ibuprofen (10−4 mol/l; n = 4) or the nitric oxide synthase blocker l-NAME (10−4 mol/l; n = 4). Positive values indicate vasopressin-induced contraction, and negative values indicate vasorelaxation. Open circles indicate control; solid circles indicate l-NAME; solid triangles indicate ibuprofen. **P < 0.01 relates to ibuprofen data significantly different when compared with control vessels at the same vasopressin concentrations by two-way ANOVA and Tukey–Kramer multiple-comparison test.
A comparative evaluation of the pulmonary and mesenteric artery vasopressin V1a and V2 receptors’ expression was conducted. As shown in Figure 5 , pulmonary and mesenteric expression of the V1a receptor is tissue and age dependent. Whereas a higher V1a receptor expression was documented in adult, when compared with newborn pulmonary arterial tissue, the opposite age-dependent pattern was observed in mesenteric vessels ( Figure 5a , b ). When the endothelial and smooth muscle cell–specific expression of the V1a receptor was evaluated ( Figure 5c – f ), no age-dependent changes were observed in muscle cells, whereas the endothelial receptor expression pattern mirrored the whole tissue data. We further comparatively quantified the adult pulmonary and mesenteric arterial tissue V1a expression and observed that the former has a higher (P = 0.02) V1a receptor expression when compared with mesenteric vessels (V1a/glyceraldehyde 3-phosphate dehydrogenase of 1.9 ± 0.4 arbitrary units (n = 4) vs. 0.5 ± 0.2 arbitrary units (n = 4), respectively).
Pulmonary and mesenteric tissue, endothelial, and smooth muscle cell vasopressin V1a receptor protein expression. Newborn and adult rat third to fourth generation (a) pulmonary (n = 4 each) and (b) mesenteric arterial tissue (n = 4 each), as well as their respective (c,d) primary endothelial (n = 4 each) and (d,f) smooth muscle cells (n = 3 each). Vasopressin V1a receptor was determined by western blotting and normalized to the tissue and cell glyceraldehyde 3-phosphate dehydrogenase (GAPDH) content. **P < 0.01 vs. adult values by unpaired Student’s t-test. Representative western blots are illustrated.
Finally, we quantified the vasopressin V2 receptor protein expression in newborn and adult pulmonary and mesenteric arterial rat tissue ( Figure 6 ). In pulmonary vessels, V2 receptor expression was undetectable with the commercially available antibody used (panel a), whereas its expression in mesenteric vessels was significantly higher in adult, when compared with newborn tissue (panel b; P < 0.05).
Pulmonary and mesenteric arteries vasopressin V2 receptor protein expression. Newborn and adult rat third to fourth generation (a) pulmonary (n = 3 each) and (b) mesenteric arterial tissue (n = 3 each). Vasopressin V2 receptor was determined by western blotting and normalized to the tissue and cell glyceraldehyde 3-phosphate dehydrogenase (GAPDH) content. Adult rat kidney tissue was used as a positive control. *P < 0.05 vs. newborn values by unpaired Student’s t-test. Representative western blots are illustrated.
Discussion
Vasopressin is a powerful systemic vasoconstrictor commonly utilized clinically to reverse shock unresponsive to other vasopressors (2). On the basis of its potential pulmonary vasodilator effect, this drug has been increasingly employed in the treatment of pulmonary hypertension in adults (1) and infants with the PPHN syndrome (9).
In the present study, we evaluated the age- and circulation-specific effects of vasopressin on the newborn and adult rat vascular tone. In adult rats, in vitro exposure to vasopressin led to a significant increase in mesenteric arterial tone and dose-dependent pulmonary arterial vasorelaxation. In contrast, vasopressin stimulation of newborn rat vascular tissue resulted in increased pulmonary vasomotor tone at low doses and pulmonary vasorelaxation only at the maximal tested concentration (6 × 10−7 mol/l). The observed vasopressin-induced increase in mesenteric vasomotor tone, although of lesser magnitude in newborn arteries, was present at both tested ages.
The pulmonary vasodilatory effect of vasopressin in adult animals is species dependent. It is present in dogs (13), absent in rabbits (14), and in guinea pigs, only documented in pulmonary veins (15). To some extent, this species-related differences in vasopressin response are secondary to the experimental conditions under which the vessels were tested. In published reports where vasopressin failed to induce pulmonary arterial vasodilation, the drug effect was evaluated in vessels lacking basal vasomotor tone (14,15). Vasopressin has also been reported to vasorelax systemic vessels such as the human forearm vasculature (16) and cerebral vessels of distinct adult animal species (17).
Precontracted pulmonary arteries of adult rodents exhibit vasodilation in response to vasopressin (18,19), whereas vasoconstriction in response to a very high drug concentration (10−5 mol/l) was reported in unstimulated mouse pulmonary vessels (20). In the present study, we did not observe any vasopressin-induced vasomotor effect in adult rat pulmonary arteries lacking basal agonist-stimulated tone, even when exposed to concentrations as high as 6 × 10−7 mol/l.
Vasopressin acts on three receptors: V1a, V1b, and V2 (21). The V1a receptor is present in vascular tissue endothelial and smooth muscle cells and considered responsible for the vasopressin-induced vasoconstriction and vasodilation (13,21). V2 is the main vasopressin receptor isotype in renal parenchymal tissue (22), while its expression in rat lung is controversial (23). The V1b (or V3) is expressed in the anterior pituitary gland and involved in adrenocorticotropic hormone secretion (24).
In the present study, we confirmed that in rats, V1a receptor expression is present in both pulmonary and mesenteric arterial tissue endothelial and smooth muscle cells but exhibiting a circulation- and age-specific distinct pattern. Comparing adult rat vascular tissue, we showed that V1a expression is higher in pulmonary, as opposed to mesenteric, arteries.
We were unable to detect significant V2 receptor expression in pulmonary arterial tissue at both tested ages. In the present study, mesenteric arterial V2 receptor expression was found to be age dependent and highest in adult, as compared with newborn tissue. Together, these data suggest that V1a is responsible for pulmonary arterial vasorelaxation, whereas the V2 receptor modulates the vasopressin constrictor response that is predominant in mesenteric vessels, when compared with pulmonary arteries.
The present data strongly suggest that the age-related dependency of the vasopressin-induced pulmonary vasorelaxation is caused by the significantly lower expression of vasopressin V1a receptor in newborn, as compared with adult lung vascular endothelial cells. A previous report showing evidence for V1a receptor mRNA expression in adult, but not newborn rat lungs (10), further supports this conclusion. In keeping with the present evidence, vasopressin administration (20 mIU/kg/min) to newborn goats induced a significant increase in pulmonary vascular resistance (25). Together, these data strongly suggest that in newborn animals, vasopressin has no pulmonary vasodilatory effect.
The mechanism by which vasopressin induces pulmonary vasodilation in adult animals is controversial. The presence of an intact endothelium is required for vasopressin to induce pulmonary vasorelaxation (13). Endothelium-derived nitric oxide (6,26) has been incriminated as the mediator of vasopressin-induced pulmonary vasodilation. Yet vasopressin stimulation did not alter nitric oxide generation in rat aorta (27). In rat (28) and canine (29) systemic arteries, cyclooxygenase inhibition potentiates the vasopressin-induced vasoconstriction suggesting that prostaglandins are involved in the vasopressin regulation of vasomotor tone. Sai et al. (5) observed that while the adult canine pulmonary arterial vasodilation to vasopressin was nitric oxide dependent, prostacyclin was involved in the drug-induced pulmonary vein relaxation.
In the present study, the cyclooxygenase inhibitor ibuprofen, but not the nitric oxide synthase blocker l-NAME, suppressed the vasopressin-induced pulmonary vasorelaxation at lower drug concentrations. In fact, in the presence of ibuprofen, vasopressin enhanced pulmonary vasomotor tone, suggesting that it unmasked a direct effect of this drug on the vessels’ smooth muscle contractile potential. Finally, there is evidence that prostaglandins regulate the vasomotor tone of certain vascular beds through the V2 receptor. Medina et al. (30) documented that the V2 receptor agonist desmopressin caused endothelium-dependent relaxation in human renal arteries, and this vasodilatory effect was inhibited by indomethacin. Since in the present study we were unable to document V2 receptor expression in lung vascular tissue, it is unlikely that the vasopressin-induced pulmonary vasodilation in rats is modulated via this receptor.
Clinical studies in adult subjects have not consistently shown an effect of vasopressin on the pulmonary vasculature (3). Similarly, little is known about the vasopressin effect on the newborn pulmonary vasomotor tone with its pulmonary vasodilatory therapeutic effect in infants mostly appearing as clinical case reports. Scheurer et al. (4) described two neonates who showed elevated pulmonary arterial pressure following surgical correction of their anomalous pulmonary veins. Both infants were treated with nitric oxide, and one of them with the phosphodiesterase 3 inhibitor milrinone prior to the addition of vasopressin, making it difficult to confirm the vasopressin pulmonary vasodilatory effect (4). Stathopoulos et al. (31). recently reported on the effect of a long-acting analog of vasopressin (terlipressin). The drug was shown to improve the patient’s systemic arterial pressure and reduce the echocardiographic estimate of elevated pulmonary arterial pressure in a newborn with congenital diaphragmatic hernia (31). Given such limited evidence for its potential pulmonary vasodilatory effect, it is rather surprising that a significant number of neonatologists acknowledge its therapeutic use in the PPHN syndrome (9).
Finally, the extent to which the in vitro vasopressin concentrations utilized in the present study reflect in vivo therapeutic serum levels in humans deserves further comments. The physiological serum vasopressin levels in adult human subjects is 2.22 pg/ml (32). In adult dogs, a basal plasma vasopressin level of 2.3 ± 0.4 pg/ml was reported that increased to 280 ± 23 pg/ml following vasopressin infusion (7.6 ng/kg/min) (33). In newborn sheep, the physiological vasopressin levels have been reported to be in the range of 7.0 pg/ml (34). In the present study, we evaluated in vitro vasopressin concentrations ranging from 1.1 to 660,000 pg/ml (10−12 to 6 × 10−7 mol/l). The adult pulmonary arteries only exhibited significant vasorelaxation at vasopressin concentrations ≥3,300 pg/ml. Thus, to the extent that the adult rat pulmonary arteries evaluated in vitro reflect the in vivo conditions, vasopressin concentrations higher than commonly utilized clinically are required to induce significant pulmonary vasodilation.
In summary, whereas vasopressin has a significant systemic vasoconstrictor effect in newborn and adult rats, the pulmonary vasodilatory response of this drug is age dependent. The reduced expression of V1a receptors in the pulmonary arterial tissue of the newborn, as compared with adult rat, likely accounts for the lack of vasopressin-induced pulmonary vasodilation early in life. These animal data, together with the limited clinical evidence in support of vasopressin having a significant pulmonary vasodilatory effect early in life, raise concerns about its therapeutic use in infants with the PPHN syndrome. Further studies attempting to validate the present animal data in newborn and adult human tissue are warranted.
Materials and Methods
Animals
All procedures were conducted according to criteria established by the Canadian Council on Animal Care and were approved by the Animal Care Committees of The Hospital for Sick Children Research Institutes.
Newborn (2–7 d of age) and adult (>60 d of age) Sprague-Dawley rats were studied. The animals were killed with an overdose of pentobarbital sodium (50 mg/kg i.p.; BHD, Toronto, Ontario, Canada), and the lungs, as well as mesenteric bed, were quickly removed and maintained on an ice bed for further dissections.
Near-resistance (third to fourth generations) intrapulmonary and mesenteric arteries were isolated and mounted on a wire myograph (Danish Myo Technology A/S, Aarhus, Denmark). The vessels were bathed in Krebs–Henseleit buffer (NaCl, 115 mmol/l; NaHCO3, 25 mmol/l; NaHPO4, 1.38 mmol/l; KCl, 2.51 mmol/l; MgSO4–7 H2O, 2.46 mmol/l; CaCl2, 1.91 mmol/l; and dextrose, 5.56 mmol/l) bubbled with air/6% CO2 and maintained at 37 °C.
Organ Bath Study
The functional evaluation of pulmonary and mesenteric arteries has been previously described (35). Briefly, lung intralobar pulmonary or mesenteric artery ring segments (average diameter: 80–100 µm and length = 2 mm) were dissected free and mounted on a wire myograph. Isometric changes were digitized and recorded online (Myodaq; Danish Myo Technology A/S). After 1 h of equilibration, the optimal vessel resting tension was determined by repeated stimulation with 128 mmol/l KCl until maximum active tension was reached. All subsequent force measurements were obtained at optimal resting tension.
The vascular muscle precontraction was induced with the predetermined effective concentration to induce 75% of maximal contraction (EC75) with the thromboxane A2-mimetic U46619 (Cayman Chemical, Ann Arbor, MI). The newborn and adult U46619 EC75 concentrations were 4 × 10−7 and 2 × 10−7 mol/l for the pulmonary arteries and 6 × 10−7 and 4 × 10−8 mol/l for the mesenteric vessels, respectively. The vasopressin (Pharmaceutical Partners of Canada, Richmond Hill, Ontario, Canada)–induced changes in newborn and adult pulmonary and mesenteric vascular tone were determined.
Western Blotting
Primary endothelial and smooth muscle cells retrieved from intrapulmonary and mesenteric arteries, as well as the whole tissue extracts, were utilized to measure vasopressin V1a and V2 receptors’ expression.
For vascular endothelial cells’ isolation, the tissue digested with 1 mg/ml of collagenase type II (Sigma-Aldrich, Oakville, Ontario, Canada) for 2 h at 37 °C. The digest was then passed through 70 μm cell strainer to remove tissue fragments, pelleted by centrifugation at 200g for 10 min and resuspended with 2% fetal bovine serum (Gibco, Burlington, Canada) in phosphate-buffered solution containing 5µl biotinylated rat antimouse CD31 antibody (BD PharMingen, San Diego, CA). After incubation on ice for 1 h, the endothelial cells were immobilized with streptavidin magnetic beads (New England Biolabs, Ipswich, MA) on ice. The endothelial cells were then placed on the EasySep magnet (Stemcell technologies, Vancouver, British Columbia, Canada) for 5 min, and unbound cells were removed. Bound endothelial cells were lysed in 10 mmol/l Tris–HCl (pH 7.4) lysis buffer containing 1% Triton X-100 and protease/phosphatase inhibitors (Roche Diagnostics Canada, Laval, Quebec, Canada) and centrifuged at 13000g for 30 min.
For smooth muscle isolation, the arteries were digested with 1 mg/ml collagenase type II for 2 h, pelleted at 200g for 10 min, and washed with growth medium composed of Dulbecco’s modified essential medium (Wisent, Montreal, Quebec, Canada) supplemented with 10% fetal bovine serum (Wisent) and 2.5% penicillin/streptomycin/fungizone. The pellet was resuspended in growth medium and incubated at 37 °C, 5% CO2 with 90% humidity followed by media changes at 24 h and every 4 d until confluence. Cells were utilized at passage 2.
For the whole tissue protein extraction, the pulmonary and mesenteric arteries were lysed in 10 mmol/l Tris–HCl (pH 7.4) lysis buffer containing 1% Triton X-100 and protease/phosphatase inhibitors (Roche Diagnostics Canada, Laval, Quebec, Canada) and centrifuged at 13,000g for 30 min. Equal amounts of lysate proteins in Laemmli buffer were separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis and immunoblotted, as previously described using the following antibodies: rabbit vasopressin V1a (AVPV1a) and V2 (AVPV2A) (Alpha Diagnostic, San Antonio, TX), mouse GAPDH (Sigma-Aldrich), antimouse IgG peroxidase conjugated (Sigma-Aldrich) and antirabbit IgG horseradish peroxidase conjugated (Cell Signaling Technology, Danvers, MA). Detection was performed with the enhanced chemiluminescence reagent (Perkin Elmer, Shelton, CT). Band intensities were quantified using ImageJ (National Institutes of Health, Bethesda, MD) and expressed relative to GAPDH.
Statistical Analysis
Data were evaluated by one or two-way ANOVA with multiple comparisons obtained by the Tukey–Kramer test. On comparing only two groups, Student’s t-test was employed. Statistical significance was accepted at P < 0.05. All statistical analyses were performed with the Number Cruncher Statistical System (NCSS, Kaysville, UT). Data are presented as means ± SEM.
Statement of Financial Support
This study was supported by grants from the Canadian Institutes of Health Research (MOP 93710 to J.B.). M.E. was supported by a grant in aid from the Takatsuki General Hospital (Japan).
Disclosure
The authors have no financial ties to the products evaluated in this study or potential/perceived conflicts of interest.
References
Sharman A, Low J . Vasopressin and its role in critical care. Cont Educ Anaesth Crit Care Pain 2008; 8:134–7.
Tayama E, Ueda T, Shojima T, et al. Arginine vasopressin is an ideal drug after cardiac surgery for the management of low systemic vascular resistant hypotension concomitant with pulmonary hypertension. Interact Cardiovasc Thorac Surg 2007;6:715–9.
Smith AM, Elliot CM, Kiely DG, Channer KS . The role of vasopressin in cardiorespiratory arrest and pulmonary hypertension. QJM 2006;99:127–33.
Scheurer MA, Bradley SM, Atz AM . Vasopressin to attenuate pulmonary hypertension and improve systemic blood pressure after correction of obstructed total anomalous pulmonary venous return. J Thorac Cardiovasc Surg 2005;129:464–6.
Sai Y, Okamura T, Amakata Y, Toda N . Comparison of responses of canine pulmonary artery and vein to angiotensin II, bradykinin and vasopressin. Eur J Pharmacol 1995;282:235–41.
Eichinger MR, Walker BR . Enhanced pulmonary arterial dilation to arginine vasopressin in chronically hypoxic rats. Am J Physiol 1994;267(6 Pt 2):H2413–9.
Price LC, Wort SJ, Finney SJ, Marino PS, Brett SJ . Pulmonary vascular and right ventricular dysfunction in adult critical care: current and emerging options for management: a systematic literature review. Crit Care 2010;14:R169.
Steinhorn RH . Pharmacotherapy for pulmonary hypertension. Pediatr Clin North Am 2012;59:1129–46.
Shivananda S, Ahliwahlia L, Kluckow M, Luc J, Jankov R, McNamara P . Variation in the management of persistent pulmonary hypertension of the newborn: a survey of physicians in Canada, Australia, and New Zealand. Am J Perinatol 2012;29:519–26.
Hirasawa A, Hashimoto K, Tsujimoto G . Distribution and developmental change of vasopressin V1A and V2 receptor mRNA in rats. Eur J Pharmacol 1994;267:71–5.
Aoyagi T, Koshimizu TA, Tanoue A . Vasopressin regulation of blood pressure and volume: findings from V1a receptor-deficient mice. Kidney Int 2009;76:1035–9.
Okamura T, Ayajiki K, Fujioka H, Toda N . Mechanisms underlying arginine vasopressin-induced relaxation in monkey isolated coronary arteries. J Hypertens 1999;17:673–8.
Evora PR, Pearson PJ, Schaff HV . Arginine vasopressin induces endothelium-dependent vasodilatation of the pulmonary artery. V1-receptor-mediated production of nitric oxide. Chest 1993;103:1241–5.
García-Villalón AL, Garcia JL, Fernández N, Monge L, Gómez B, Diéguez G . Regional differences in the arterial response to vasopressin: role of endothelial nitric oxide. Br J Pharmacol 1996;118:1848–54.
Rieg AD, Rossaint R, Uhlig S, Martin C . Cardiovascular agents affect the tone of pulmonary arteries and veins in precision-cut lung slices. PLoS ONE 2011;6:e29698.
Tagawa T, Imaizumi T, Endo T, et al. Vasodilatory effect of arginine vasopressin is mediated by nitric oxide in human forearm vessels. J Clin Invest 1993;92:1483–90.
Cosentino F, Sill JC, Katusic ZS . Endothelial L-arginine pathway and relaxations to vasopressin in canine basilar artery. Am J Physiol 1993;264(2 Pt 2):H413–8.
Walker BR, Haynes J Jr, Wang HL, Voelkel NF . Vasopressin-induced pulmonary vasodilation in rats. Am J Physiol 1989;257(2 Pt 2):H415–22.
Jin HK, Yang RH, Chen YF, Thornton RM, Jackson RM, Oparil S . Hemodynamic effects of arginine vasopressin in rats adapted to chronic hypoxia. J Appl Physiol 1989;66:151–60.
Xu M, Platoshyn O, Makino A, et al. Characterization of agonist-induced vasoconstriction in mouse pulmonary artery. Am J Physiol Heart Circ Physiol 2008;294:H220–8.
Koshimizu TA, Nakamura K, Egashira N, Hiroyama M, Nonoguchi H, Tanoue A . Vasopressin V1a and V1b receptors: from molecules to physiological systems. Physiol Rev 2012;92:1813–64.
Bankir L, Bichet DG, Bouby N . Vasopressin V2 receptors, ENaC, and sodium reabsorption: a risk factor for hypertension? Am J Physiol Renal Physiol 2010;299:F917–28.
Fay MJ, Du J, Yu X, North WG . Evidence for expression of vasopressin V2 receptor mRNA in human lung. Peptides 1996;17:477–81.
Roberts EM, Pope GR, Newson MJ, Lolait SJ, O’Carroll AM . The vasopressin V1b receptor modulates plasma corticosterone responses to dehydration-induced stress. J Neuroendocrinol 2011;23:12–9.
Sakamoto H, Takenoshita M, Asakura Y, Ibara S, Ikenoue T . Comparison of circulatory effects between arginine vasopressin (AVP) and dopamine in conscious newborn goats. J Vet Med Sci 1996;58:511–4.
Resta TC, Walker BR . Chronic hypoxia selectively augments endothelium-dependent pulmonary arterial vasodilation. Am J Physiol 1996;270(3 Pt 2):H888–96.
Millette E, Lamontagne D . Endothelium-dependent and NO-mediated desensitization to vasopressin in rat aorta. Br J Pharmacol 1996;119:899–904.
Walker BR . Prostaglandin modulation of the vascular effects of vasopressin in the conscious rat. Proc Soc Exp Biol Med 1985;180:258–63.
Onoue H, Nakamura N, Toda N . Endothelium-dependent and -independent responses to vasodilators of isolated dog cerebral arteries. Stroke 1988;19:1388–94.
Medina P, Segarra G, Vila JM, Chuan P, Domenech C, Lluch S . V2-receptor-mediated relaxation of human renal arteries in response to desmopressin. Am J Hypertens 1999;12(2 Pt 1):188–93.
Stathopoulos L, Nicaise C, Michel F, et al. Terlipressin as rescue therapy for refractory pulmonary hypertension in a neonate with a congenital diaphragmatic hernia. J Pediatr Surg 2011;46:e19–21.
Cintra Ede A, Maciel JA Jr, Araújo S, et al. Vasopressin serum levels in patients with severe brain lesions and in brain-dead patients. Arq Neuropsiquiatr 2004;62(2A):226–32.
Nyhan DP, Geller HS, Goll HM, Murray PA . Pulmonary vasoactive effects of exogenous and endogenous AVP in conscious dogs. Am J Physiol 1986;251(5 Pt 2):H1009–16.
Miao DC, Velaphi SC, Roy T, Despain K, Rosenfeld CR . Metabolism and synthesis of arginine vasopressin in conscious newborn sheep. Am J Physiol Endocrinol Metab 2008;295:E672–7.
Enomoto M, Gosal K, Cubells E, et al. Sex-dependent changes in the pulmonary vasoconstriction potential of newborn rats following short-term oxygen exposure. Pediatr Res 2012;72:468–78.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Enomoto, M., Pan, J., Shifrin, Y. et al. Age dependency of vasopressin pulmonary vasodilatory effect in rats. Pediatr Res 75, 315–321 (2014). https://doi.org/10.1038/pr.2013.221
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2013.221
This article is cited by
-
Hydrogen peroxide promotes gastric motility in the newborn rat
Pediatric Research (2018)