Abstract
This Review focuses on the changing epidemiology of infections among patients with end-stage renal disease who are undergoing dialysis. In particular, bloodstream infections related to vascular access in patients undergoing hemodialysis, and peritonitis in patients undergoing peritoneal dialysis, are highlighted. Gram-positive (staphylococcal and enterococcal) bloodstream infections and Gram-negative peritonitis (especially extended-spectrum β-lactamase-producing organisms) contribute substantially to excess health-care use owing to infection caused by dialysis access. Although the management of peritoneal-dialysis-related peritonitis has been hampered by a dearth of randomized, controlled studies, epidemiological data have provided useful information. To overcome the problem of differing methods used to monitor infections within various dialysis centers, uniform reporting systems for vascular-access-related infection and peritoneal-dialysis-related peritonitis, as recommended by the Centers for Disease Control and Prevention and the International Society for Peritoneal Dialysis, respectively, are discussed. Infections unrelated to the port of entry for dialysis are also examined, namely hepatitis and respiratory infection. To address the disease burden, we examine the infection-related mortality as well as the implications for subsequent cardiovascular mortality.
Key Points
-
Gram-positive (staphylococcal and enterococcal) bloodstream infections and Gram-negative peritonitis (especially extended-spectrum β-lactamase-producing organisms) contribute substantially to excess health-care use owing to infection caused by dialysis access
-
Standard empiric protocols for the treatment of infection in dialysis settings should be replaced by a regime tailored to the local circumstances, the individual organism and its antibiotic resistance pattern
-
The prevalence of hepatitis C remains significantly higher in patients on hemodialysis than in those undergoing peritoneal dialysis; increased duration of dialysis therapy is associated with increased risk of seroconversion
-
Inadequate antibody titers after vaccination against hepatitis B virus are a consistent and strong predictor of hepatitis B seroconversion
-
Patients undergoing hemodialysis seem to be more susceptible to infections, such as pneumonia, than those on peritoneal dialysis; vaccination against influenza mitigates the increased mortality in patients on hemodialysis
-
Infection seems to contribute to the cardiovascular disease burden in patients on dialysis
Similar content being viewed by others
Introduction
Infection remains one of the most common causes of morbidity and mortality, as well as hospitalization, in patients receiving dialysis. According to the results of a study conducted in a sample of 332,442 incident patients on dialysis in the USA with end-stage renal disease (ESRD), the cumulative annual incidence of infection-related hospitalization was 26% for children and 31% for adults.1 The burden of infection-related mortality among patients with ESRD is best illustrated by a comparative analysis of data from the United States Renal Data System (USRDS), in which the annual mortality rate secondary to sepsis was 100–300-fold higher in patients on dialysis treatment than in the general population.2
Accumulating evidence points to a growing burden of infection among patients on dialysis. The risk of infection varies with the characteristics of the patients who are selected for dialysis. Increased access to dialysis has led to less-stringent selection of patients, as characterized by an increasing proportion of elderly patients, those with diabetes, and frail individuals with complex coexisting conditions. In addition, the trend towards advancing age among patients receiving dialysis is expected to confer an increased susceptibility to infection; older age has repeatedly proven to be an independent risk factor for infection in dialysis populations.3,4 In a USRDS study involving an incident dialysis cohort of 119,858 patients, one-half of those aged 65 years or older had at least one infection-related hospitalization during a median follow-up of nearly 2 years.4 Of interest, while hospitalization rates in dialysis populations have stabilized since 1993, the relative contribution of infection-related hospitalization has increased by nearly 26% from 1993 to 2007.5,6 The high burden of infectious complications in this population clearly merits special attention. Although no randomized, controlled trials have focused on mitigating infectious complications in dialysis populations, compelling reasons exist to examine the data on epidemiology in this setting. Results from observational studies can provide insights for managing and preventing infection in patients on dialysis.
This Review describes the epidemiology and clinical characteristics of infection in patients receiving hemodialysis and peritoneal dialysis. The source of infection in patients treated with dialysis is also highlighted, and can be broadly categorized as either access-related or access-unrelated.
Access-related infections
Hemodialysis
Access remains the Achilles heel of dialysis treatment, especially with regard to vascular access for hemodialysis. Despite an apparent decline in the overall rate of vascular-access-related hospitalization owing to infection, as observed in the USRDS data, the rate is still approximately twice as high as it was a decade ago.5
The clinical significance of bloodstream infection in patients receiving hemodialysis is well recognized. According to a population-based study on the epidemiology of severe bloodstream infection, patients on maintenance hemodialysis had the highest risk of developing a severe bloodstream infection resulting in admission to the intensive care unit (relative risk 208.7, 95% CI 142.9–296.3).7 The incidence of vascular-access-related bloodstream infection varies between medical facilities and can be influenced by the percentage of patients who receive dialysis via a central venous catheter (CVC).8 Several types of vascular access used in hemodialysis, listed in order of increasing risk of infection, are as follows: arteriovenous fistulas created from the patient's own blood vessels; arteriovenous grafts constructed from synthetic materials; tunneled CVCs; and nontunneled CVCs.8
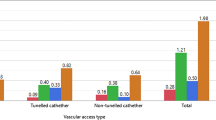
Since the tracking of access-related infection is now recommended as a clinical performance indicator and parameter for continuous monitoring, a clear and universally agreed parameter for reporting infection is needed. For surveillance and benchmarking purposes, current guidelines from the Centers for Disease Control and Prevention (CDC) suggest that dialysis units should report their vascular-access-related infection rates as the number of such events per 100 patient-months on dialysis.9,10 This dialysis event rate should preferably be calculated for the different types of vascular access, in addition to the overall event rate. This parameter (events per 100 patient-months on dialysis) is gaining acceptance for monitoring infections, although the more traditional parameter reporting infection rates per 1,000 catheter-days has been in place for many years. The two parameters differ in terms of deriving the denominator data. Reporting the infection rate per 1,000 catheter-days mandates the number of patients with catheters to be counted each day and is therefore more commonly used in hospital-based studies of bloodstream infection. In the case of outpatient dialysis centers, the patient population is much more stable in terms of numbers, hence the denominator is derived from the dialysis population in the first week of each month. For example, a center treating 56, 52, and 59 patients with hemodialysis during the first week of three successive months would have a total of 167 patient-months for the 3-month period. The rate of vascular-access-related bloodstream infections is then calculated by dividing the total number of events by the total number of patient-months, and multiplying the result by 100. This method allows calculation of relatively accurate rates while greatly reducing the burden of collecting denominator data.11 Depending on local practices and the diagnostic criteria used, the incidence of vascular-access-related bloodstream infections in patients on dialysis ranges from 0.6 to 3.5 episodes per 100 patient-months (Table 1).12,13,14,15,16,17
Staphylococcus aureus is the most common microorganism implicated in vascular-access-related bloodstream infections (27.7–50.0%), followed by coagulase-negative staphylococci. As the leading pathogen causing bloodstream infection among patients on hemodialysis, S. aureus has remained dominant in the epidemiology literature.18 S. aureus infection has also been associated with high mortality, morbidity and use of health-care resources; for example, if a patient receiving hemodialysis develops an S. aureus bloodstream infection, the average length of hospitalization is over 50 days.19 Furthermore, a high incidence of secondary complications, including infective endocarditis, osteomyelitis, septic arthritis, epidural abscess, and infection of intravascular devices, has been associated with S. aureus bloodstream infection (Table 2).19,20,21,22,23
A pressing need remains for both nephrologists and the infection control community to examine the progressive spread of meticillin-resistant S. aureus (MRSA). Given the likelihood of repeated hospitalization and surgery, the requirement for vascular access and frequent puncture of the vascular access site, patients receiving hemodialysis are particularly vulnerable to the development of MRSA carrier status and infection. Overall, the incidence of invasive MRSA infection among patients on hemodialysis is 100-fold higher than for the general population (45.2 events per 1,000 patients on dialysis versus 0.2–0.4 events per 1,000 patients in the general population).24 Of note, the adverse consequences of MRSA infection seem to be exaggerated in the dialysis population. A study of 143 patients undergoing hemodialysis reported that MRSA bloodstream infection, when compared to infection with meticillin-susceptible strains of S. aureus, was associated with higher infection-related mortality (OR 5.4), increased length of hospital stay and increased hospital costs.25 However, in a population-based study, mortality rates associated with MRSA bacteremia and meticillin-sensitive S. aureus bacteremia were similar after adjustment for major confounding variables.26 In another study of 504 hospitalized patients with S. aureus bacteremia (188 of whom had MRSA bloodstream infections), the mortality risk ratio associated with MRSA bacteremia, versus meticillin-sensitive strains, was only 1.68 (however, the study population under investigation was not exclusively comprised of patients on dialysis, and this factor could underlie the disparity in mortality data observed between this and other studies).27
An analysis published in 2011 concluded that MRSA nasal carriage in patients receiving hemodialysis is associated with an increased risk of both all-cause mortality (2.46-fold increased risk) and infection-related mortality (4.99-fold increased risk).28 However, studies evaluating the relationship between MRSA nasal carriage or infection, and adverse outcomes among patients undergoing hemodialysis, have not established a causal relationship.28 Thus, we cannot exclude the possibility that MRSA carrier status is a surrogate marker for increased morbidity in patients on hemodialysis, as the sickest patients are most prone to frequent hospitalization and contact with MRSA (80% of MRSA infections in patients on dialysis are acquired within the health-care setting).24
At the same time, patterns in the epidemiology of S. aureus infection and in the susceptibility of this organism to treatment with vancomycin have been changing. In essence, a steady increase has been evident in the minimum inhibitory concentration (MIC) for vancomycin (a phenomenon sometimes referred to as the MIC creep),18,29,30 owing to the emergence of vancomycin-intermediate S. aureus (MIC 4–8 μg/ml) and vancomycin-resistant S. aureus (MIC ≥16 μg/ml). Even among the vancomycin-susceptible staphylococci, subpopulation strains with a MIC of 1–2 μg/ml can be present. This change in antibiotic susceptibility has practical implications for the clinical care of patients who require dialysis because S. aureus infections are now more resistant to treatment and require increasingly aggressive empirical vancomycin dosing.30,31 To address the growing number of reports of vancomycin treatment failure and heteroresistance (that is, the presence of mixed populations of drug-sensitive and drug-resistant organisms in a single clinical isolate, in proportions higher than expected from background mutation alone) in S. aureus isolates, the MIC considered to represent vancomycin susceptibility has decreased from ≤4 μg/ml to ≤2 μg/ml since 2006. At the same time, a new target trough vancomycin level of 15–20 μg/ml was proposed.31
The changing epidemiology of enterococcal infections in patients on hemodialysis deserves attention. Enterococci are currently the second to third most common organisms responsible for bacteremia in these patients (Table 1). The two major organisms are Enterococcus fecalis and Enterococcus faecium. Previously, clinicians had little interest in identifying enterococci to the species level, but this situation changed after the detection of an increase in enterococci other than E. fecalis (primarily E. faecium) that had unusually high levels of ampicillin resistance, high levels of gentamicin resistance, and increasing levels of vancomycin resistance. According to the results of an analysis of surveillance data on 24,179 nosocomial bloodstream infections occurring in 49 US hospitals between 1995 and 2002, the estimated incidence of vancomycin resistance in E. faecium isolates was 60%, versus 2% in E. fecalis isolates.32 A study from 2008 showed a worsening trend of antibiotic resistance; 80% of E. faecium isolates and 6.9% of E. fecalis isolates collected between 2006 and 2007 were vancomycin-resistant.33 Selective pressure for enterococcal vancomycin resistance in hemodialysis units arises from antimicrobial use (in particular, vancomycin and cephalosporin agents) as well as frequent and prolonged hospitalization. Development of vancomycin resistance is problematic and leads to limited treatment options because it often occurs in enterococcal strains that are already resistant to ampicillin. Curbing the spread of vancomycin resistance among enterococci in hospital outbreaks has now become a primary concern for hemodialysis units.34 Patients receiving hemodialysis who are infected with vancomycin-resistant enterococci should be isolated during hospitalization and treatment, as mandated by the CDC guidelines, although data from high-quality studies are not available to support this recommendation.
Preventive strategies to reduce CVC-related bloodstream infection have been comprehensively reviewed previously in this journal.35 Mupirocin ointment seems to be effective in reducing the risk of CVC-related bacteremia, according to a Cochrane database systematic review, and povidone ointment, polysporin ointment and topical honey have shown promising results that warrant further investigation in randomized, controlled trials.36 Of interest, a new approach to prevent CVC-related bacteremia involves the use of antibiotic lock solutions (also referred to as antimicrobial catheter lock solutions) containing an antimicrobial agent, such as gentamicin, in conjunction with an anticoagulant.35,37 These solutions are instilled into the CVC lumen at the end of each dialysis session to prevent biofilm formation.35,37 Although the prophylactic use of antibiotic lock solutions for the purpose of preventing infection has not been recommended in the Kidney Disease: Outcomes Quality Initiative8 or CDC38 guidelines, the preponderance of available data from randomized, controlled studies suggest a reduction in CVC-related bacteremia with this technique. Four meta-analyses have demonstrated that use of intraluminal antibiotic lock solutions reduces the rate of CVC-related bacteremia by 56–87% (Table 3).39,40,41,42 However, the risk of developing bacterial resistance remains a subject of ongoing debate, because of the relatively short follow-up period of most published studies. An observational study published in 2010 investigating the use of prophylactic gentamicin as the antibiotic component in catheter lock solutions found an emerging risk of gentamicin-resistant, Gram-positive infections (primarily owing to Staphylococcus and Enterococcus species).43 One trend of concern is that major complications, including four deaths and four cases of endocarditis, were associated with the 24 episodes of gentamicin-resistant CVC-related bacteremia reported in this study.43
Thus, the use of catheter lock solutions that do not include an antibiotic component should probably be explored as they would reduce the likelihood of antibiotic resistance. To date, the results from trials investigating trisodium citrate catheter lock solutions have been mixed.44,45 In addition, promising results from a multicenter, randomized, controlled trial published in 2011 showed a significant decrease in the rate of CVC-related bacteremia (from 4.1 to 1.2 episodes per 100 patient-months) after once-weekly use of recombinant tissue plasminogen activator as a catheter lock solution.46 The cost of such approaches is, however, a key issue, because health-care providers might not be willing to pay for expensive preventive tools.
Peritoneal dialysis
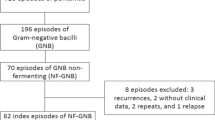
Large-scale observational studies have enabled valid conclusions to be drawn regarding the epidemiology of access-related infection in patients undergoing peritoneal dialysis. Most of these data are from single-center studies,47,48 but multicenter studies are emerging, especially from the Australian and New Zealand Dialysis and Transplant (ANZDATA) registry.49,50 Rapid changes in the epidemiology and outcomes of peritonitis in patients on peritoneal dialysis have been reflected by the large number of revisions or updates of the International Society for Peritoneal Dialysis (ISPD) guidelines over the past two decades.51,52,53,54,55
Continuous monitoring of the peritoneal-dialysis-related infection rate, as with CVC-related bloodstream infection among patients receiving hemodialysis, is recommended and should be undertaken at least annually for every peritoneal dialysis program.55 In addition, the infection rate associated with specific organisms should be calculated and compared to that in the literature. The usual way of reporting the peritonitis rate is to calculate the duration of peritoneal dialysis in months, divided by the number of episodes of peritonitis, which is expressed as the interval in months between episodes.55 Alternatively, the peritonitis rate can be determined by calculating the number of infections caused by an organism in a given time period, divided by the duration of dialysis in years (time at risk), which is expressed as episodes per year.54,55 To date, there is no consensus on when calculations for the time at risk should begin; the first day of patient training in the dialysis procedure seems to be preferable to the date of catheter insertion, because the latter might lead to falsely low values in calculations of the peritonitis rate (largely in centers that place the catheter many weeks or even months before the start of training).56 Benchmarking of peritonitis rates in peritoneal dialysis populations has been more widely practiced than that of CVC-related bloodstream infection rates in hemodialysis populations; the maximum acceptable peritonitis infection rate is now recognized to be no more than one episode every 18 months (or 0.67 episodes per year at risk). According to the latest ISPD guidelines, relapsing peritonitis should be counted as a single episode. Moreover, a peritonitis rate of 0.67 per year at risk should be considered acceptable, but not the target rate, as most programs can now achieve a peritonitis rate of 0.36 episodes per year at risk.56
In contradistinction to hemodialysis-related infections, coagulase-negative staphylococci are, in general, more common than S. aureus as the cause of peritoneal-dialysis-related peritonitis. A major reason for this phenomenon is that touch contamination has a key role in causing coagulase-negative staphylococcal peritonitis in patients on peritoneal dialysis. In the two largest studies of coagulase-negative staphylococcal peritonitis, this organism accounted for 11.4–26.0% of all such infections, which were estimated to occur at a rate of 0.064–0.160 episodes per patient-year (Table 4).47,49 Despite an initial decrease in the rates of coagulase-negative staphylococcal peritonitis during the late 1990s (presumably related to introduction of the flush-before-fill technique and disconnect system), the incidence of infection by these microorganisms has since remained static in most dialysis programs. The published data, in general, seem to suggest a relatively favorable outcome in mild cases of coagulase-negative staphylococcal peritonitis, with the reported complete cure rate (defined as complete resolution of peritonitis by antibiotics alone, without relapse or recurrence within 4 weeks of completing therapy55,56) of over 70%.47,49 One study suggested a high prevalence of meticillin-resistant coagulase-negative strains of staphylococci in patients with peritoneal-dialysis-related peritonitis (49.5%), although the treatment outcome remains favorable with the routine use of cefazolin as the first-line antibiotic.47 Infection with meticillin-resistant coagulase-negative strains of staphylococci can sometimes be associated with an increased risk of relapse (ranging from 14.2% to 16.9%),47,49 defined as an episode that occurs within 4 weeks of completing therapy for a prior peritonitis episode with the same organism.55,56 In patients who experience relapse of coagulase-negative staphylococci peritonitis, clinicians should consider the possibility of colonization of the intra-abdominal portion of the catheter with a biofilm, which is best treated by replacing the catheter.
S. aureus is another important Gram-positive bacterial cause of peritonitis. This organism is reported to cause 11.9–14.0% of all peritonitis episodes,48,50 which represents an absolute rate of 0.072–0.080 episodes per patient-year (Table 4). Although S. aureus is a slightly less frequent cause of bacterial peritonitis than is coagulase-negative staphylococci in patients on peritoneal dialysis, S. aureus produces a more severe form of peritonitis. A single-center analysis showed that only 51% of patients with meticillin-sensitive S. aureus peritonitis and 46% with MRSA peritonitis achieved complete resolution of infection without relapse, recurrence of peritonitis, or the need for catheter removal.48 The differences in etiology underlie the varied treatment outcomes between coagulase-negative staphylococcal peritonitis and S. aureus peritonitis. The latter is more often a result of catheter infection than touch contamination, which explains its association with a high rate of relapse (up to 20%).50 In the presence of concomitant catheter-tunnel or exit-site S. aureus infection, catheter removal is, therefore, often advised.55 Although exit-site infection is considered to contribute to recurrence of S. aureus peritonitis, an analysis of data on 245 consecutive patients with this infection demonstrated that an elective change of catheter seemed to be ineffective in preventing subsequent episodes of peritonitis.50 Furthermore, the presence of an exit-site infection was not associated with the response to antibiotic treatment in that study. This finding suggests that factors other than an infected catheter (such as persistent nasal carriage) might influence the likelihood of repeat episodes of S. aureus peritonitis.
An important point to note is that the proportion of peritonitis episodes caused by Gram-negative bacteria has been increasing relative to all peritoneal-dialysis-associated infections, and that the severity of such infections and the strength of their association with poor outcomes are also increasing.57 Although the overall rate of peritonitis has been improving, the most substantial degree of improvement has been observed in rates of Gram-positive peritonitis. Conversely, the incidence of Gram-negative peritonitis has remained constant. This evolution in the epidemiology of infection has been observed over the past two decades. In a review of 546 episodes of peritonitis that occurred from 1991 to 1998, the rate of Gram-positive peritonitis declined significantly from 0.75 to 0.28 episodes per patient-year, whereas the occurrence of Gram-negative peritonitis remained constant at approximately 0.16 episodes per patient-year.58 A similar phenomenon has been observed by the authors of this Review. During the period from 1994 to 2003, data on 1,787 peritonitis episodes demonstrated a decline in coagulase-negative staphylococcal peritonitis from 0.21 to 0.06 episodes per patient-year; this drop occurred in parallel with a reduction in the use of spike sets for peritoneal dialysis.59 A better connection technique, the disconnect system, offers a more effective means than do spike systems of preventing peritonitis owing to contamination. The incidence of Escherichia coli and Klebsiella peritonitis, however, remained static.59
From an epidemiological point of view, Gram-positive and Gram-negative peritonitis should be examined separately because their clinical outcomes are markedly different. Peritonitis episodes caused by Gram-negative organisms are more likely to require hospital admission,60 and to result in catheter loss61,62 and failure of peritoneal dialysis.61 Among all the Gram-negative organisms, the Pseudomonas species is probably the most important cause of severe peritonitis in patients undergoing peritoneal dialysis. Three large retrospective studies have, for instance, confirmed high rates of catheter loss after Pseudomonas peritonitis (Table 4).63,64,65 Before a universal policy of using two antipseudomonal antibiotics was instigated, catheter loss occurred in 61.3% of patients with Pseudomonas peritonitis;63 furthermore, analyses of two large cohorts from 2001 and 2009 (treated after implementation of this policy) still showed a catheter removal rate of around 40%.64,65
A major risk factor for Pseudomonas peritonitis is the presence of a concomitant Pseudomonas exit-site infection.63,64 The presence of exit-site infection, as a surrogate marker of biofilm formation, is strongly predictive of a high relapse rate and antibiotic resistance; use of aggressive therapy, such as early removal of the catheter, is still justified in these patients. According to the findings of another report on 104 episodes of Pseudomonas peritonitis, a higher frequency of antibiotic use was evident within 30 days of infection with Pseudomonas than with nonpseudomonal peritonitis.64 A recent course of antibiotic therapy (within 30 days of the onset of peritonitis) also predicted a significantly lower complete cure rate of Pseudomonas peritonitis (11.6% versus 42.9%, P <0.001); this finding could be explained by the development of resistant bacterial strains.64 Alternatively, this association could represent a surrogate marker of recent peritonitis or exit-site infection. Either way, these findings are in keeping with the current ISPD recommendations for prompt catheter removal if catheter infection is present at or precedes development of peritonitis.55
Another large, heterogenous group of non-Pseudomonas Gram-negative organisms, the Enterobacteriaceae, have become an increasingly recognized cause of serious peritoneal infectious complications; the two most common species, as observed in two large case series, are E. coli (accounting for 32.9–52.9% of episodes), and Klebsiella species (accounting for 20.4–27.1% of episodes).66,67 Although infection with these microorganisms is associated with a better complete cure rate than is Pseudomonas peritonitis (58.1% versus 22.1–32.3%), approximately 40% of the episodes of peritonitis observed did not respond to treatment with a single antibiotic, despite bacterial isolates demonstrating sensitivity to the agent in vitro.66 A further analysis showed a gradual increase in the prevalence of antibiotic resistance to several commonly used antibiotics, including cephalothin and cefuroxime, in E. coli and Klebsiella infections. A slight increase in the prevalence of resistance to netilmicin and gentamicin was also evident.66 The observation that antibiotic use by patients on peritoneal dialysis was associated with the development of enterobacterial resistance to cefotaxime, ceftazidime, and the combination drugs cefoperazone–sulbactam and piperacillin–tazobactam,66 provides strong evidence for the propensity of these Gram-negative bacteria to adapt to antibiotics, mainly by modifying the substrate spectrum of common plasmid-mediated and chromosomal β-lactamases.
With the rising proportion of Gram-negative bacteria that demonstrate resistance to broad-spectrum cephalosporins—a surrogate marker for extended-spectrum β-lactamase (ESBL) production—one would expect a worsening severity of Gram-negative peritonitis. A retrospective study conducted in Spain assessed the medical records of patients who developed E. coli peritonitis before and after 1996 (when the first case of ESBL-producing E. coli was identified). The researchers found that the duration of peritoneal inflammation increased significantly, from 3.1 days to 5.2 days, and that catheter removal rates increased significantly, from 19% to 39%, respectively.68 These results mirror data collected over a period of 10 years from another series of patients who developed E. coli peritonitis, in which treatment failure (temporary or permanent cessation of peritoneal dialysis, or death during peritonitis) and infection-related mortality were significantly higher after 1996, when ESBL-producing E. coli became prevalent.69
Taken together, the findings of these studies indicate an increasing severity of Gram-negative peritonitis. However, most of the data accrued from observational studies support, but do not prove, the efficacy of more aggressive antibiotic treatment, such as extending the duration of antibiotic therapy to 21 days.51 Nevertheless, the emergence of severe forms of Gram-negative peritonitis warrants further investigation to address how we should change the treatment paradigm for this disease entity.
Although the incidence of peritoneal-dialysis-related fungal infection is low numerically, such infections carry the greatest morbidity and mortality of all access-related infections in patients on peritoneal dialysis.51,70 According to two large case series of patients with fungal peritonitis, the most commonly isolated organisms were Candida albicans and other Candida species, which accounted for approximately 70% of all infections.70,71 Catheter removal (together with antifungal therapy) was associated with improved survival in both studies.70,71 An important concern with fungal peritonitis is its association with exceptionally high infection-related mortality (up to 40%).71 In a large, incident dialysis cohort of 21,935 patients included in the ANZDATA registry, peritoneal dialysis was consistently associated with an increased hazard ratio of death from infection compared to hemodialysis, after 6 months of treatment.72 Notably, this association was largely driven by increased rates of death from fungal infections (primarily peritonitis) in patients on peritoneal dialysis.72 The results of this analysis suggest that further attention to preventing fungal peritonitis is much needed. As with Gram-negative peritonitis, the precise risk factors for fungal infection have yet to be established, but recent antibiotic treatment for peritonitis (or any other infection) is strongly suspected to have an important role.70
Infections unrelated to dialysis access
Viral hepatitis
Infectious complications that are associated with the dialysis procedure (but not the dialysis access per se) affect a substantial number of patients. For example, hepatitis B virus (HBV) and hepatitis C virus (HCV) infections have remained a major health issue in dialysis units since the early recognition of patient-to-patient and patient-to-staff transmission of hepatotropic viruses in the 1960s. According to a systematic review of 33 nosocomial HBV outbreaks between 1992 and 2007, hemodialysis units accounted for the highest proportion of outbreaks (30.3%).73
Some patient-specific risk factors for HBV infection coexist in hemodialysis and peritoneal dialysis; patients have an impaired host defense system against viral infections, and they frequently require blood product transfusions. The risk of exposure to viral hepatitis can be further increased in patients on hemodialysis owing to the nature of the dialysis procedure itself. Examples of potential transmission routes include blood contact with contaminated equipment, injection of liquids harboring the hepatitis virus, and exposure of broken skin or mucous membranes to the virus.74 The treatment process in hemodialysis not only creates the opportunity for viral exposure via sharing vials of drugs containing multiple treatment doses but also via shared patient care: for example, blood-contaminated hands or gloves; failure to clean and disinfect dialysis machines, equipment, supplies and environmental surfaces; and preparing and distributing parenteral medications via common mobile medication carts at dialysis stations. Added to these concerns is the failure to identify and segregate patients who are positive for HBV. Nosocomial transmission can also occur when a patient's care is shared between a number of staff, and where hemodialysis machines, equipment and other supplies are shared between HBV-positive and unaffected patients. According to a prospective analysis of data from 1987 to 1990 on 185 patients receiving hemodialysis and 124 patients having continuous ambulatory peritoneal dialysis, the hepatitis B surface antigen seroconversion rate was 0.19 events per patient-year with hemodialysis and 0.01 events per patient-year with continuous ambulatory peritoneal dialysis. Hemodialysis treatment was the only significant risk factor associated with HBV infection.75
By contrast, an observational study conducted from 1997 to 2001, involving 308 hemodialysis facilities worldwide, confirmed that the majority of facilities (78.1%) had a zero hepatitis B seroconversion rate.76 Overall, the seroconversion rate was markedly lower than previously reported, at 0.0078 events per patient-year.76 In fact, the results of further studies suggest a greatly reduced risk of HBV infection in hemodialysis units worldwide (Figure 1).76,77,78 Of note, in an analysis of data from eight national registries in the Asia–Pacific region (where a high prevalence of HBV infection exists), the prevalence of hepatitis B surface antigen seropositivity was generally comparable between peritoneal dialysis and hemodialysis populations.77 These findings, indicating a reduced HBV infection risk in patients undergoing hemodialysis, are likely to be a result of improved infection control measures, as well as screening and vaccination programs.
In addition to this inferential evidence, surveillance data from an observational study show a significantly decreased risk of hepatitis B seroconversion (risk ratio 0.44, P = 0.01) in hemodialysis facilities that report the use of a protocol for managing patients infected with HBV and the routine administration of hepatitis B vaccine.76 These approaches have now been incorporated into practice guidelines from the CDC, which recommend segregation of patients (and their equipment) who are seropositive for hepatitis B surface antigen, and routine HBV screening and vaccination.79 Despite the accumulating evidence describing a substantial decrease in the incidence of HBV infection in patients on dialysis, the protection conferred by hepatitis B vaccination remains suboptimal among patients with chronic kidney disease. The seroconversion rate after intramuscular administration of recombinant hepatitis B vaccine, in general, is in the range of 44–76% among patients on dialysis.80 A particularly important direction for future research might be to explore the best HBV vaccination strategy, with the aim of improving the immune response in patients with chronic kidney disease and further reducing the transmission of this virus in dialysis units. Potential options include the use of hepatitis B vaccination earlier in the course of kidney disease, intradermal administration of the vaccine, use of augmented doses of vaccine, and development of adjuvant vaccines that have the potential for increased immunogenicity.80,81
HCV infection continues to be the most common hepatotropic viral infection in patients on hemodialysis. The hepatitis C seroconversion rate in hemodialysis units ranges from 0.011 to 0.036 per patient-year on hemodialysis,78 and the prevalence of HCV infection in hemodialysis units varies from 2.7% in the UK78 to over 20% in southern areas of Europe (Figure 1). The prevalence of HCV is also consistently higher in patients on hemodialysis than in the corresponding general populations. The varying prevalence of HCV infection between these regions could in part reflect the type of laboratory assay used to identify it,82 but is more likely to be derived from differences in the implementation of infection control measures between both dialysis units and countries.
Several risk factors for HCV infection have been identified in patients on dialysis that provide strong evidence for an association with dialysis center practices and delivery of care. The Dialysis Outcomes and Practice Patterns Study, a prospective observational study involving 308 representative dialysis facilities in France, Germany, Italy, Japan, Spain, the UK and the USA, found that an increase in the proportion of highly trained staff (defined as at least 2 years of formal nursing training) was associated with a significantly decreased prevalence of HCV (OR 0.93 per 10% increase) as well as a trend towards a reduced likelihood of seroconversion (risk ratio 0.92) in a combined model.78 Good evidence suggests that HCV prevalence in the dialysis facility was strongly associated with the risk of seroconversion; for every 10% increase in the prevalence of this infection, the adjusted risk ratio for hepatitis C seroconversion increased by 1.36.78
In contrast to HBV infection, the risk of HCV infection remains significantly higher in patients treated with hemodialysis than in those on peritoneal dialysis (7.9% versus 3.0% in an Asia–Pacific survey).77 To further adjust for the confounding effect of differences in the number of years at risk between the two modalities of dialysis treatment, an analysis of the rate of hepatitis C seroconversion per patient-year on dialysis was performed for patients in Australia and New Zealand over a 10-year period from 1995 to 2005; the incidence of HCV infection was significantly lower in the peritoneal dialysis group than in the hemodialysis group (0.0003 versus 0.001 events per patient-year).77 Consistent with this observation are the findings from a Brazilian study, in which patients on peritoneal dialysis also had a reduced rate of hepatitis C seroconversion compared with those on hemodialysis.75
An important epidemiological difference between HBV and HCV infection is that an increased duration of dialysis therapy is associated only with an increased risk of hepatitis C seroconversion.78,83 However, the lack of effective vaccination (that is, inadequate antibody titers) against HBV is a consistent and strong predictor of hepatitis B seroconversion.76,83 No vaccine for HCV is currently available. Since 2001, therefore, the CDC has recommended initial serological screening for anti-HCV antibodies in patients on long-term hemodialysis upon admission to any unit. Thereafter, anti-HCV antibody screening should be conducted semi-annually, or earlier if an unexplained elevation in alanine transaminase levels occurs, to facilitate the early detection of virus transmission and the implementation of control measures.79 Poor adherence to these CDC recommendations has been repeatedly linked to HCV transmission within hemodialysis units.84,85 A prospective observational study evaluated the transmission of HCV within a hemodialysis unit by means of genetic and phylogenetic analyses.86 Blood-contaminated surfaces (sometimes with detectable levels of HCV RNA) were identified as the source of HCV cross-transmission. More importantly, the study showed that a low ratio of nurses to patients and poor hand hygiene were independent predictors for the presence of hemoglobin on environmental surfaces.86 Systematic investigations of outbreaks of HCV infection found that the most common areas where lapses in infection control practices occurred were the improper handling and preparation of parenteral medication, and inadequate cleaning and disinfection of environmental surfaces between treatment of successive patients.84,85,87 International travel by patients and receiving hemodialysis treatment in developing countries have also been implicated as risk factors for HCV infection.88
With the increasing emphasis on universal infection control measures, the incidence and prevalence of HCV infection among patients on dialysis, in general, seems to be declining, at least in Europe and the USA.89,90,91 In the absence of a vaccine and treatment capable of eradicating the infection, transmission of HCV to patients receiving dialysis can be prevented by adherence to recommended infection control practices. Peritoneal dialysis could potentially offer a more isolated, home-based therapy and lower parenteral exposure risk to HCV than hemodialysis. Home-based hemodialysis therapy might also reduce the risk of cross-transmission of the virus compared to center-based therapy.92
Respiratory infection
Pneumonia is another common cause of hospitalization in patients with ESRD, and rates of this infection are substantially higher in this patient population than in the general population.93 Overall, the mortality rate from pneumonia is 14–16-fold higher in patients on dialysis than in the general population.94 Nonetheless, important gaps exist in our knowledge of the epidemiology of respiratory infection in patients undergoing dialysis, which has received relatively little attention to date.
The risk of pneumonia varies between subgroups of patients on dialysis, according to the limited number of studies available. Rates of hospitalization for pneumonia, on Cox regression analysis, were significantly higher in patients on dialysis who were more than 65 years of age, those with a low BMI (BMI <18.5 kg/m2) and individuals with low serum albumin concentrations (characteristics suggestive of the malnutrition-inflammation complex syndrome), according to administrative data from the USRDS.93 Patients on peritoneal dialysis, however, were excluded from this study. Very few published studies have examined the epidemiology of pneumonia in both the peritoneal dialysis and hemodialysis settings.95,96 Interestingly, in a USRDS study that included an incident dialysis cohort of nearly 300,000 patients, one in five (21%) developed pneumonia within 1 year of starting dialysis, and 42% of these individuals required hospitalization.95 Rates of pneumonia were significantly higher in patients on hemodialysis than in those on peritoneal dialysis (29.0 versus 18.2 events per 100 patient-years, an increase of 59%), implying that individuals on hemodialysis might be more susceptible to this infection.95 After adjustment for differences in measured comorbidity and confounding factors, hemodialysis remained strongly associated with pneumonia, with an adjusted HR of 1.41 versus peritoneal dialysis.95 In contrast to the USRDS data, however, the ANZDATA cohort study found that the risk of fatal pneumonia was not significantly different between patients receiving peritoneal dialysis and those on hemodialysis.72 Reasons for these differing observations between countries remain uncertain.
Several plausible reasons could underlie why patients undergoing hemodialysis might be particularly susceptible to pulmonary infections. Therapy-related factors for this increased risk include transient hypoxemia occurring during the dialysis procedure, as a result of margination of leukocytes in the pulmonary vasculature and carbon dioxide losses. A further risk factor is the practice of hemodialysis in institutional sessions, which is inherently associated with exposure to other patients on hemodialysis and health-care personnel. Another line of reasoning maintains that an increased burden of unmeasured comorbidity in patients receiving hemodialysis might explain their elevated risk of pneumonia.95 Irrespective of the modality of dialysis, patients with ESRD clearly belong to a high-risk group for developing pneumonia (of both bacterial and viral causes). Viral causes of pneumonia deserve particular attention in patients on dialysis. An analysis of data on the influenza A H1N1 virus (swine influenza) pandemic, for instance, confirmed a 10-fold higher mortality rate as well as a higher hospitalization rate in patients on dialysis versus the general population (34% versus 6–7%, respectively).97 Likewise, severe acute respiratory syndrome is also associated with a longer duration in hospital and a more aggressive clinical course in patients treated with dialysis.98,99
An obvious implication of the increased viral-pneumonia-related mortality in dialysis populations is the improved benefit of influenza vaccination. Analysis of the USRDS data has confirmed that influenza vaccination in patients on dialysis is associated with a statistically significant decrease in the risk of death and hospitalization for any cause; this finding was most consistent among patients treated with hemodialysis.100
Cardiovascular disease
Cardiovascular morbidity and mortality have always been major concerns for nephrologists managing patients on dialysis, and it has been shown that reduced residual renal function, inflammation, valvular calcification and left ventricular hypertrophy are predictors of cardiovascular mortality in patients on peritoneal dialysis.101 The interaction between infection and cardiovascular disease, however, seems to be a new concern.
An interesting finding from the USRDS analysis was a significant decrease in cardiovascular-event-related mortality associated with influenza vaccination, in addition to reductions in all-cause mortality, influenza and/or pneumonia-related mortality.100 These findings mirror observations made in another USRDS study, in which pneumonia in patients on dialysis was strongly associated with subsequent cardiovascular events (adjusted HR 3.02, 95% CI 2.89–3.16), within 6 months of pneumonia.95 Although the mechanisms linking infection, chronic inflammation and cardiovascular disease have been elusive, this phenomenon of infection being a harbinger of future cardiovascular events and death has been repeatedly investigated and confirmed in observational and epidemiological studies.102,103 In a historical cohort study of 393,451 patients on hemodialysis or peritoneal dialysis, septicemia was identified as a precursor to the development of cardiovascular events and death.102 Septicemia was associated with the development of myocardial infarction, congestive heart failure, stroke and peripheral vascular disease, and the adjusted risk ratio of these events remained approximately double that expected for up to 5 years after the initial infection.102 These observations have been confirmed in another prospective study—the Dialysis Morbidity and Mortality Wave 2 study—in which septicemia or bacteremia were associated with a nearly twofold increase in the risk of myocardial infarction or stroke.103 Whether infection can be considered a risk factor for atherogenesis and cardiovascular disease, however, remains unclear. Interest in the role of endotoxemia is growing; even low-grade endotoxemia was a strong risk factor for the development of atherosclerosis in an epidemiological study,104 presumably owing to activation of innate and adaptive immune mechanisms. Of note is the potential impact of circulating endotoxins on survival in patients undergoing peritoneal dialysis or hemodialysis.105,106
Conclusions
Existing epidemiological data suggest that infection in dialysis populations is associated with a marked increase in the use of health-care resources, as well as excess morbidity and mortality.107 Despite the potential limitations of observational and epidemiological studies, they have provided important information about the changing nature of infections in patients on dialysis, and on the implications for clinical management of these individuals. For instance, patients undergoing peritoneal dialysis or hemodialysis have a notably increased risk of infection, particularly peritonitis in the former group and catheter-related bloodstream infection in the latter group. Moreover, infection in patients on either form of dialysis is also associated with an increased risk of subsequent cardiovascular events; this increase in risk is only partially explained by underlying conditions, such as frailty. Thus, the presence of infection in a patient on dialysis has a substantial effect on cardiovascular mortality and morbidity, and should influence decisions regarding the use of therapies intended to minimize that risk. Further research is needed to translate these findings on the epidemiology of infection in patients on dialysis into effective preventive strategies.
Review criteria
The MEDLINE, PubMed, Ovid and CINAHL databases and the Cochrane Database of Systematic Reviews were searched for literature published from 1995 to 2011. The search terms used were “dialysis”, “infection”, “hemodialysis”, “bacteremia”, “peritoneal dialysis”, “peritonitis”, “central venous catheter”, “catheters”, “hepatitis” and “epidemiology”. Other keywords related to microbiology were also used, including “Staphylococcus”, “Enterococcus” and “Pseudomonas”. Bibliographies of relevant studies identified in the search and key reviews were searched for additional publications.
References
Chavers, B. M., Solid, C. A., Gilbertson, D. T. & Collins, A. J. Infection-related hospitalization rates in pediatric versus adult patients with end-stage renal disease in the United States. J. Am. Soc. Nephrol. 18, 952–959 (2007).
Sarnak, M. J. & Jaber, B. L. Mortality caused by sepsis in patients with end-stage renal disease compared with the general population. Kidney Int. 58, 1758–1764 (2000).
Powe, N. R., Jaar, B., Furth, S. L., Hermann, J. & Briggs, W. Septicemia in dialysis patients: incidence, risk factors, and prognosis. Kidney Int. 55, 1081–1090 (1999).
Dalrymple, L. S. et al. Infection-related hospitalizations in older patients with ESRD. Am. J. Kidney Dis. 56, 522–530 (2010).
United States Renal Data System. 2009 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States [online], (2009).
Dalrymple, L. S. & Go, A. S. Epidemiology of acute infections among patients with chronic kidney disease. Clin. J. Am. Soc. Nephrol. 3, 1487–1493 (2008).
Laupland, K. B. et al. Severe bloodstream infections: a population-based assessment. Crit. Care Med. 32, 992–997 (2004).
Vascular Access 2006 Work Group. Clinical practice guidelines for vascular access. Am. J. Kidney Dis. 48 (Suppl. 1), S176–S247 (2006).
Tokars, J. I. Description of a new surveillance system for bloodstream and vascular access infections in outpatient hemodialysis centers. Semin. Dial. 13, 97–100 (2000).
Centers for Disease Control and Prevention. Dialysis Event [online], (2011).
Lok, C. E. & Mokrzycki, M. H. Prevention and management of catheter-related infection in hemodialysis patients. Kidney Int. 79, 587–598 (2011).
Hoen, B., Paul-Dauphin, A., Hestin, D. & Kessler, M. EPIBACDIAL: a multicenter prospective study of risk factors for bacteremia in chronic hemodialysis patients. J. Am. Soc. Nephrol. 9, 869–876 (1998).
Tokars, J. I. A prospective study of vascular access infections at seven outpatient hemodialysis centers. Am. J. Kidney Dis. 37, 1232–1240 (2001).
Taylor, G. et al. Prospective surveillance for primary bloodstream infections occurring in Canadian hemodialysis units. Infect. Control Hosp. Epidemiol. 23, 716–720 (2002).
Dopirak, M. et al. Surveillance of hemodialysis-associated primary bloodstream infections: the experience of ten hospital-based centers. Infect. Control Hosp. Epidemiol. 23, 721–724 (2002).
Gilad, J. et al. Surveillance of chronic haemodialysis-associated infections in southern Israel. Clin. Microbiol. Infect. 11, 547–552 (2005).
Lafrance, J. P. et al. Vascular access-related bloodstream infections in First Nations, community and teaching Canadian dialysis units, and other center-level predictors. Nephron Clin. Pract. 114, c204–c212 (2010).
Vandecasteele, S. J., Boelaert, J. R. & De Vriese, A. S. Staphylococcus aureus infections in hemodialysis: what a nephrologist should know. Clin. J. Am. Soc. Nephrol. 4, 1388–1400 (2009).
Greiner, W. et al. Clinical outcome and costs of nosocomial and community-acquired Staphylococcus aureus bloodstream infection in haemodialysis patients. Clin. Microbiol. Infect. 13, 264–268 (2007).
Marr, K. A. et al. Incidence and outcome of Staphylococcus aureus bacteremia in hemodialysis patients. Kidney Int. 54, 1684–1689 (1998).
Engemann, J. J. et al. Clinical outcomes and costs due to Staphylococcus aureus bacteremia among patients receiving long-term hemodialysis. Infect. Control Hosp. Epidemiol. 26, 534–539 (2005).
Inrig, J. K. et al. Relationship between clinical outcomes and vascular access type among hemodialysis patients with Staphylococcus aureus bacteremia. Clin. J. Am. Soc. Nephrol. 1, 518–524 (2006).
Troidle, L., Eisen, T., Pacelli, L. & Finkelstein, F. Complications associated with the development of bacteremia with Staphylococcus aureus. Hemodial. Int. 11, 72–75 (2007).
Centers for Disease Control and Prevention. Invasive methicillin-resistant Staphylococcus aureus infections among dialysis patients—United States, 2005. MMWR Morb. Mortal. Wkly Rep. 56, 197–199 (2007).
Reed, S. D. et al. Costs and outcomes among hemodialysis-dependent patients with methicillin-resistant or methicillin-susceptible Staphylococcus aureus bacteremia. Infect. Control Hosp. Epidemiol. 26, 175–183 (2005).
Harbarth, S., Rutschmann, O., Sudre, P. & Pittet, D. Impact of methicillin resistance on the outcome of patients with bacteremia caused by Staphylococcus aureus. Arch. Intern. Med. 158, 182–189 (1998).
Selvey, L. A., Whitby, M. & Johnson, B. Nosocomial methicillin-resistant Staphylococcus aureus bacteremia: is it any worse than nosocomial methicillin-sensitive Staphylococcus aureus bacteremia? Infect. Control Hosp. Epidemiol. 21, 645–648 (2000).
Lai, C. F. et al. Nasal carriage of methicillin-resistant Staphylococcus aureus is associated with higher all-cause mortality in hemodialysis patients. Clin. J. Am. Soc. Nephrol. 6, 167–174 (2011).
Boucher, H. W. & Sakoulas, G. Perspectives on daptomycin resistance, with emphasis on resistance in Staphylococcus aureus. Clin. Infect. Dis. 45, 601–608 (2007).
Vandecasteele, S. J. & De Vriese, A. S. Recent changes in vancomycin use in renal failure. Kidney Int. 77, 760–764 (2010).
Hidayat, L. K., Hsu, D. I., Quist, R., Shriner, K. A. & Wong-Beringer, A. High-dose vancomycin therapy for methicillin-resistant Staphylococcus aureus infections: efficacy and toxicity. Arch. Intern. Med. 166, 2138–2144 (2006).
Wisplinghoff, H. et al. Nosocomial bloodstream infections in US hospitals: analysis of 24,179 cases from a prospective nationwide surveillance study. Clin. Infect. Dis. 39, 309–317 (2004).
Hidron, A. I. et al. NHSN annual update: antimicrobial-resistant pathogens associated with healthcare-associated infections: annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006–2007 Infect. Control Hosp. Epidemiol. 29, 996–1011 (2008).
Servais, A. et al. Rapid curbing of a vancomycin-resistant Enterococcus faecium outbreak in a nephrology department. Clin. J. Am. Soc. Nephrol. 4, 1559–1564 (2009).
Betjes, M. G. Prevention of catheter-related bloodstream infection in patients on hemodialysis. Nat. Rev. Nephrol. 7, 257–265 (2011).
McCann, M. & Moore, Z. E. Interventions for preventing infectious complications in haemodialysis patients with central venous catheters. Cochrane Database of Systematic Reviews, Issue 1. Art. No.: CD006894. http://dx.doi.org/10.1002/14651858.CD006894.pub2 (2010).
Chow, K. M. et al. Antibiotic lock solutions for the prevention of catheter-related bacteraemia in haemodialysis patients. Hong Kong Med. J. 16, 269–274 (2010).
O'Grady, N. P. et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recomm. Rep. 51, 1–29 (2002).
James, M. T. et al. Meta-analysis: antibiotics for prophylaxis against hemodialysis catheter-related infections. Ann. Intern. Med. 148, 596–605 (2008).
Yahav, D. et al. Antimicrobial lock solutions for the prevention of infections associated with intravascular catheters in patients undergoing hemodialysis: systematic review and meta-analysis of randomized, controlled trials. Clin. Infect. Dis. 47, 83–93 (2008).
Jaffer, Y., Selby, N. M., Taal, M. W., Fluck, R. J. & McIntyre, C. W. A meta-analysis of hemodialysis catheter locking solutions in the prevention of catheter-related infection. Am. J. Kidney Dis. 51, 233–241 (2008).
Labriola, L., Crott, R. & Jadoul, M. Preventing haemodialysis catheter-related bacteraemia with an antimicrobial lock solution: a meta-analysis of prospective randomized trials. Nephrol. Dial. Transplant. 23, 1666–1672 (2008).
Landry, D. L. et al. Emergence of gentamicin-resistant bacteremia in hemodialysis patients receiving gentamicin lock catheter prophylaxis. Clin. J. Am. Soc. Nephrol. 5, 1799–1804 (2010).
Weijmer, M. C. et al. Randomized, clinical trial comparison of trisodium citrate 30% and heparin as catheter-locking solution in hemodialysis patients. J. Am. Soc. Nephrol. 16, 2769–2777 (2005).
Power, A. et al. Sodium citrate versus heparin catheter locks for cuffed central venous catheters: a single-center randomized controlled trial. Am. J. Kidney Dis. 53, 1034–1041 (2009).
Hemmelgarn, B. R. et al. Prevention of dialysis catheter malfunction with recombinant tissue plasminogen activator. N. Engl. J. Med. 364, 303–312 (2011).
Szeto, C. C. et al. Coagulase negative staphylococcal peritonitis in peritoneal dialysis patients: review of 232 consecutive cases. Clin. J. Am. Soc. Nephrol. 3, 91–97 (2008).
Szeto, C. C. et al. Staphylococcus aureus peritonitis complicates peritoneal dialysis: review of 245 consecutive cases. Clin. J. Am. Soc. Nephrol. 2, 245–251 (2007).
Fahim, M. et al. Coagulase-negative staphylococcal peritonitis in Australian peritoneal dialysis patients: predictors, treatment and outcomes in 936 cases. Nephrol. Dial. Transplant. 25, 3386–3392 (2010).
Govindarajulu, S. et al. Staphylococcus aureus peritonitis in Australian peritoneal dialysis patients: predictors, treatment, and outcomes in 503 cases. Perit. Dial. Int. 30, 311–319 (2010).
Keane, W. F. et al. Peritoneal dialysis-related peritonitis treatment recommendations. 1993 update. The Ad Hoc Advisory Committee on Peritonitis Management. International Society for Peritoneal Dialysis. Perit. Dial. Int. 13, 14–28 (1993).
Keane, W. F. et al. Peritoneal dialysis-related peritonitis treatment recommendations: 1996 update. Perit. Dial. Int. 16, 557–573 (1996).
Keane, W. F. et al. Adult peritoneal dialysis-related peritonitis treatment recommendations: 2000 update. Perit. Dial. Int. 20, 396–411 (2000).
Piraino, B. et al. Peritoneal dialysis-related infections recommendations: 2005 update. Perit. Dial. Int. 25, 107–131 (2005).
Li, P. K. et al. Peritoneal dialysis-related infections recommendations: 2010 update. Perit. Dial. Int. 30, 393–423 (2010).
Piraino, B. et al. ISPD position statement on reducing the risks of peritoneal dialysis-related infections. Perit. Dial. Int. http://dx.doi.org/10.3747/pdi.2011.00057.
Szeto, C. C. & Chow, K. M. Gram-negative peritonitis—the Achilles heel of peritoneal dialysis? Perit. Dial. Int. 27 (Suppl. 2), S267–S271 (2007).
Zelenitsky, S. et al. Analysis of microbiological trends in peritoneal dialysis-related peritonitis from 1991 to 1998. Am. J. Kidney Dis. 36, 1009–1013 (2000).
Szeto, C. C. et al. Change in bacterial aetiology of peritoneal dialysis-related peritonitis over 10 years: experience from a centre in South-East Asia. Clin. Microbiol. Infect. 11, 837–839 (2005).
Troidle, L., Gorban-Brennan, N., Kliger, A. & Finkelstein, F. Differing outcomes of Gram-positive and Gram-negative peritonitis. Am. J. Kidney Dis. 32, 623–628 (1998).
Bunke, C. M., Brier, M. E. & Golper, T. A. Outcomes of single organism peritonitis in peritoneal dialysis: Gram negatives versus Gram positives in the Network 9 Peritonitis Study. Kidney Int. 52, 524–529 (1997).
Choi, P. et al. Peritoneal dialysis catheter removal for acute peritonitis: a retrospective analysis of factors associated with catheter removal and prolonged postoperative hospitalization. Am. J. Kidney Dis. 43, 103–111 (2004).
Bunke, M., Brier, M. E. & Golper, T. A. Pseudomonas peritonitis in peritoneal dialysis patients: the Network #9 Peritonitis Study. Am. J. Kidney Dis. 25, 769–774 (1995).
Szeto, C. C. et al. Clinical course of peritonitis due to Pseudomonas species complicating peritoneal dialysis: a review of 104 cases. Kidney Int. 59, 2309–2315 (2001).
Siva, B. et al. Pseudomonas peritonitis in Australia: predictors, treatment, and outcomes in 191 cases. Clin. J. Am. Soc. Nephrol. 4, 957–964 (2009).
Szeto, C. C. et al. Enterobacteriaceae peritonitis complicating peritoneal dialysis: a review of 210 consecutive cases. Kidney Int. 69, 1245–1252 (2006).
Jarvis, E. M. et al. Predictors, treatment, and outcomes of non-Pseudomonas Gram-negative peritonitis. Kidney Int. 78, 408–414 (2010).
Valdés-Sotomayor, J. et al. Increased severity of Escherichia coli peritonitis in peritoneal dialysis patients independent of changes in in vitro antimicrobial susceptibility testing. Perit. Dial. Int. 23, 450–455 (2003).
Yip, T. et al. Risk factors and outcomes of extended-spectrum β-lactamase-producing E. coli peritonitis in CAPD patients. Perit. Dial. Int. 26, 191–197 (2006).
Miles, R. et al. Predictors and outcomes of fungal peritonitis in peritoneal dialysis patients. Kidney Int. 76, 622–628 (2009).
Wang, A. Y. et al. Factors predicting outcome of fungal peritonitis in peritoneal dialysis: analysis of a 9-year experience of fungal peritonitis in a single center. Am. J. Kidney Dis. 36, 1183–1192 (2000).
Johnson, D. W. et al. Associations of dialysis modality and infectious mortality in incident dialysis patients in Australia and New Zealand. Am. J. Kidney Dis. 53, 290–297 (2009).
Lanini, S. et al. Patient to patient transmission of hepatitis B virus: a systematic review of reports on outbreaks between 1992 and 2007. BMC Med. 7, 15 (2009).
Edey, M., Barraclough, K. & Johnson, D. W. Review article: hepatitis B and dialysis. Nephrology (Carlton) 15, 137–145 (2010).
Cendoroglo Neto, M. et al. Incidence of and risk factors for hepatitis B virus and hepatitis C virus infection among haemodialysis and CAPD patients: evidence for environmental transmission. Nephrol. Dial. Transplant. 10, 240–246 (1995).
Burdick, R. A. et al. Patterns of hepatitis B prevalence and seroconversion in hemodialysis units from three continents: the DOPPS. Kidney Int. 63, 2222–2229 (2003).
Johnson, D. W. et al. Frequencies of hepatitis B and C infections among haemodialysis and peritoneal dialysis patients in Asia-Pacific countries: analysis of registry data. Nephrol. Dial. Transplant. 24, 1598–1603 (2009).
Fissell, R. B. et al. Patterns of hepatitis C prevalence and seroconversion in hemodialysis units from three continents: the DOPPS. Kidney Int. 65, 2335–2342 (2004).
[No authors listed] Recommendations for preventing transmission of infections among chronic hemodialysis patients. MMWR Recomm. Rep. 50, 1–43 (2001).
Chow, K. M. et al. Extra-high-dose hepatitis B vaccination does not confer longer serological protection in peritoneal dialysis patients: a randomized controlled trial. Nephrol. Dial. Transplant. 25, 2303–2309 (2010).
Barraclough, K. A. & Playford, E. G. Hepatitis B virus infection in hemodialysis populations: progress toward prevention. Kidney Int. 77, 177–180 (2010).
Kidney Disease: Improving Global Outcomes (KDIGO). KDIGO clinical practice guideline for the prevention, diagnosis, evaluation, and treatment of hepatitis C in chronic kidney disease. Kidney Int. Suppl. 109, S1–S99 (2008).
Grzegorzewska, A. E., Kaczmarek-Leki, V., Młot-Michalska, M. & Niepolski, L. Seroconversion rate to positivity for antibodies against core antigen of hepatitis B virus and duration of renal replacement therapy. Nephrol. Dial. Transplant. 26, 970–976 (2011).
Centers for Disease Control and Prevention. Hepatitis C virus transmission at an outpatient hemodialysis unit—New York, 2001–2008. MMWR Morb. Mortal. Wkly Rep. 58, 189–194 (2009).
Thompson, N. D. et al. Hepatitis C virus transmission in hemodialysis units: importance of infection control practices and aseptic technique. Infect. Control Hosp. Epidemiol. 30, 900–903 (2009).
Girou, E. et al. Determinant roles of environmental contamination and noncompliance with standard precautions in the risk of hepatitis C virus transmission in a hemodialysis unit. Clin. Infect. Dis. 47, 627–633 (2008).
Patel, P. R., Thompson, N. D., Kallen, A. J. & Arduino, M. J. Epidemiology, surveillance, and prevention of hepatitis C virus infections in hemodialysis patients. Am. J. Kidney Dis. 56, 371–378 (2010).
Bhattacharya, S. et al. Holiday haemodialysis and imported hepatitis C virus infection: a series of sixteen cases in two large haemodialysis units. J. Clin. Virol. 45, 296–299 (2009).
Tokars, J. I., Miller, E. R., Alter, M. J. & Arduino, M. J. National surveillance of dialysis-associated diseases in the United States, 1997. Semin. Dial. 13, 75–85 (2000).
Finelli, L., Miller, J. T., Tokars, J. I., Alter, M. J. & Arduino, M. J. National surveillance of dialysis-associated diseases in the United States, 2002. Semin. Dial. 18, 52–61 (2005).
Sauné K. et al. Decreased prevalence and incidence of HCV markers in haemodialysis units: a multicentric French survey. Nephrol. Dial. Transplant. 26, 2309–2316 (2011).
Li, P. K. et al. Increasing home based dialysis therapies to tackle dialysis burden around the world: a position statement on dialysis economics from the 2nd Congress of the International Society for Hemodialysis. Nephrology (Carlton) 16, 53–56 (2011).
Slinin, Y., Foley, R. N. & Collins, A. J. Clinical epidemiology of pneumonia in hemodialysis patients: the USRDS waves 1, 3, and 4 study. Kidney Int. 70, 1135–1141 (2006).
Sarnak, M. J. & Jaber, B. L. Pulmonary infectious mortality among patients with end-stage renal disease. Chest 120, 1883–1887 (2001).
Guo, H., Liu, J., Collins, A. J. & Foley, R. N. Pneumonia in incident dialysis patients—the United States Renal Data System. Nephrol. Dial. Transplant. 23, 680–686 (2008).
Aslam, N., Bernardini, J., Fried, L., Burr, R. & Piraino, B. Comparison of infectious complications between incident hemodialysis and peritoneal dialysis patients. Clin. J. Am. Soc. Nephrol. 1, 1226–1233 (2006).
Marcelli, D., Marelli, C. & Richards, N. Influenza A(H1N1)v pandemic in the dialysis population: first wave results from an international survey. Nephrol. Dial. Transplant. 24, 3566–3572 (2009).
Kwan, B. C. et al. Severe acute respiratory syndrome in dialysis patients. J. Am. Soc. Nephrol. 15, 1883–1888 (2004).
Wong, P. N. et al. Clinical presentation and outcome of severe acute respiratory syndrome in dialysis patients. Am. J. Kidney Dis. 42, 1075–1081 (2003).
Gilbertson, D. T. et al. Influenza vaccine delivery and effectiveness in end-stage renal disease. Kidney Int. 63, 738–743 (2003).
Li, P. K. & Chow, K. M. The clinical and epidemiological aspects of vascular mortality in chronic peritoneal dialysis patients. Perit. Dial. Int. 25 (Suppl. 3), S80–S83 (2005).
Foley, R. N., Guo, H., Snyder, J. J., Gilbertson, D. T. & Collins, A. J. Septicemia in the United States dialysis population, 1991 to 1999. J. Am. Soc. Nephrol. 15, 1038–1045 (2004).
Ishani, A., Collins, A. J., Herzog, C. A. & Foley, R. N. Septicemia, access and cardiovascular disease in dialysis patients: the USRDS Wave 2 study. Kidney Int. 68, 311–318 (2005).
Wiedermann, C. J. et al. Association of endotoxemia with carotid atherosclerosis and cardiovascular disease: prospective results from the Bruneck Study. J. Am. Coll. Cardiol. 34, 1975–1981 (1999).
Szeto, C. C. et al. Endotoxemia is related to systemic inflammation and atherosclerosis in peritoneal dialysis patients. Clin. J. Am. Soc. Nephrol. 3, 431–436 (2008).
McIntyre, C. W. et al. Circulating endotoxemia: a novel factor in systemic inflammation and cardiovascular disease in chronic kidney disease. Clin. J. Am. Soc. Nephrol. 6, 133–141 (2011).
Li, P. K., Leung, C. B. & Szeto, C. C. in Handbook of Dialysis Therapy 4th edn Ch. 42 (eds Nissenson, A. R. & Fine, R. N.) 396–413 (Elsevier, Oxford, 2008).
Acknowledgements
The authors' research work is supported in part by the Richard Yu Chinese University of Hong Kong Peritoneal Dialysis Research Fund.
Author information
Authors and Affiliations
Contributions
P. K. Li and K. M. Chow contributed equally to discussion of content for the article, researching data to include in the manuscript, writing, and reviewing and editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
P. K. Li declares that he has acted as a consultant and as Principal Investigator on clinical trials conducted for Baxter. K. M. Chow declares no competing interests.
Rights and permissions
About this article
Cite this article
Li, PT., Chow, K. Infectious complications in dialysis—epidemiology and outcomes. Nat Rev Nephrol 8, 77–88 (2012). https://doi.org/10.1038/nrneph.2011.194
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2011.194
This article is cited by
-
Short-term outcomes of colorectal cancer surgery in patients with dialysis: a systematic review and meta-analysis
Langenbeck's Archives of Surgery (2023)
-
Invasive aspergillosis in the patient with focal segmental glomerulosclerosis initiating hemodialysis: a case report and mini-review
Renal Replacement Therapy (2022)
-
Aortic arch calcification affects causes of death in patients on hemodialysis: a retrospective cohort study
Renal Replacement Therapy (2022)
-
Critical peritonitis secondary to gastrointestinal mucormycosis in a peritoneal dialysis patient: a case report
CEN Case Reports (2022)
-
Semi-Implantable Bioelectronics
Nano-Micro Letters (2022)