Key Points
-
Antiangiogenic drugs that target vascular endothelial growth factor A (VEGF-A; VEGF) signalling are widely used, either alone or in combination with chemotherapy, to treat various types of cancer
-
Vasculatures in endocrine organs are dependent on the VEGF–VEGF receptor signal transduction pathway for their survival, architecture and function
-
Systemic delivery of anti-VEGF drugs has the potential to adversely affect vasculatures in healthy tissues and organs, including the density and structure of capillary networks in endocrine organs
-
Tumour-derived VEGF can act as a hormone that modulates the structure and function of microvessels in endocrine organs
-
Understanding the mechanisms by which anti-VEGF drugs affect endocrine vasculatures is crucial to minimize the adverse effects associated with their use
Abstract
Systemic administration of antiangiogenic drugs that target components of the vascular endothelial growth factor A (VEGF-A; VEGF) signal transduction pathway has become a viable therapeutic option for patients with various types of cancer. Nevertheless, these drugs can drive alterations in healthy vasculatures, which in turn are associated with adverse effects in healthy tissues. VEGF is crucial for vascular homeostasis and the maintenance of vascular integrity and architecture in endocrine organs. Given these critical physiological functions, systemic delivery of drugs that target VEGF signalling can block VEGF-mediated vascular functions in endocrine organs, such as the thyroid gland, and lead to endocrine dysfunction, including hypothyroidism, adrenal insufficiency and altered insulin sensitivity. This Review discusses emerging evidence from preclinical and clinical studies that contributes to understanding the mechanisms that underlie the vascular changes and subsequent modulations of endocrine function that are induced by targeted inhibition of VEGF signalling. Understanding these mechanisms is crucial for the design of antiangiogenic drugs with minimal associated adverse effects that will enable effective treatment of patients with cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Ferrara, N., Gerber, H. P. & LeCouter, J. The biology of VEGF and its receptors. Nat. Med. 9, 669–676 (2003).
Sato, Y. et al. Properties of two VEGF receptors, Flt-1 and KDR, in signal transduction. Ann. NY Acad. Sci. 902, 201–205 (2000).
Cao, Y. Positive and negative modulation of angiogenesis by VEGFR1 ligands. Sci. Signal. 2, re1 (2009).
Soker, S., Takashima, S., Miao, H. Q., Neufeld, G. & Klagsbrun, M. Neuropilin-1 is expressed by endothelial and tumor cells as an isoform-specific receptor for vascular endothelial growth factor. Cell 92, 735–745 (1998).
Makino, Y. et al. Inhibitory PAS domain protein is a negative regulator of hypoxia-inducible gene expression. Nature 414, 550–554 (2001).
Shweiki, D., Itin, A., Soffer, D. & Keshet, E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature 359, 843–845 (1992).
Fan, L. & Iseki, S. Immunohistochemical localization of vascular endothelial growth factor in the endocrine glands of the rat. Arch. Histol. Cytol. 61, 17–28 (1998).
Shweiki, D., Itin, A., Neufeld, G., Gitay-Goren, H. & Keshet, E. Patterns of expression of vascular endothelial growth factor (VEGF) and VEGF receptors in mice suggest a role in hormonally regulated angiogenesis. J. Clin. Invest. 91, 2235–2243 (1993).
Schlaeppi, J. M. & Wood, J. M. Targeting vascular endothelial growth factor (VEGF) for anti-tumor therapy, by anti-VEGF neutralizing monoclonal antibodies or by VEGF receptor tyrosine-kinase inhibitors. Cancer Metastasis Rev. 18, 473–481 (1999).
Hurwitz, H. et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N. Engl. J.Med. 350, 2335–2342 (2004).
Kubo, H. et al. Blockade of vascular endothelial growth factor receptor-3 signaling inhibits fibroblast growth factor-2-induced lymphangiogenesis in mouse cornea. Proc. Natl Acad. Sci. USA 99, 8868–8873 (2002).
Joukov, V. et al. Proteolytic processing regulates receptor specificity and activity of VEGF-C. EMBO J. 16, 3898–3911 (1997).
Cao, R. et al. Collaborative interplay between FGF-2 and VEGF-C promotes lymphangiogenesis and metastasis. Proc. Natl Acad. Sci. USA 109, 15894–15899 (2012).
Yancopoulos, G. D., Klagsbrun, M. & Folkman, J. Vasculogenesis, angiogenesis, and growth factors: ephrins enter the fray at the border. Cell 93, 661–664 (1998).
Cao, Y. Opinion: emerging mechanisms of tumour lymphangiogenesis and lymphatic metastasis. Nat. Rev. Cancer 5, 735–743 (2005).
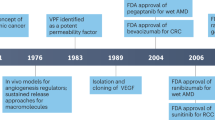
Cao, Y. et al. Forty-year journey of angiogenesis translational research. Sci. Transl. Med. 3, 114rv113 (2011).
Kerbel, R. S. Tumor angiogenesis. N. Engl. J.Med. 358, 2039–2049 (2008).
Cao, Y. & Langer, R. Optimizing the delivery of cancer drugs that block angiogenesis. Sci. Transl. Med. 2, 15ps3 (2010).
[No authors listed] Bevacizumab: more fatal adverse effects. Prescrire Int. 21, 266–267 (2012).
Hamilton, E. P. & Blackwell, K. L. Safety of bevacizumab in patients with metastatic breast cancer. Oncology 80, 314–325 (2011).
Ciombor, K. K., Berlin, J. & Chan, E. Aflibercept. Clin. Cancer Res. 19, 1920–1925 (2013).
Clarke, J. M. & Hurwitz, H. I. Targeted inhibition of VEGF receptor 2: an update on ramucirumab. Expert Opin. Biol. Ther. 13, 1187–1196 (2013).
Tannock, I. F. et al. Aflibercept versus placebo in combination with docetaxel and prednisone for treatment of men with metastatic castration-resistant prostate cancer (VENICE): a phase 3, double-blind randomised trial. Lancet Oncol. 14, 760–768 (2013).
Krupitskaya, Y. & Wakelee, H. A. Ramucirumab, a fully human mAb to the transmembrane signaling tyrosine kinase VEGFR-2 for the potential treatment of cancer. Curr. Opin. Investig. Drugs 10, 597–605 (2009).
Cao, Y. Off-tumor target—beneficial site for antiangiogenic cancer therapy? Nat. Rev. Clin. Oncol. 7, 604–608 (2010).
Palade, G. E., Simionescu, M. & Simionescu, N. Structural aspects of the permeability of the microvascular endothelium. Acta Physiol. Scand. Suppl. 463, 11–32 (1979).
Ballian, N. & Brunicardi, F. C. Islet vasculature as a regulator of endocrine pancreas function. World J. Surg. 31, 705–714 (2007).
Farquhar, M. G., Wissig, S. L. & Palade, G. E. Glomerular permeability I. Ferritin transfer across the normal glomerular capillary wall. J. Exp. Med. 113, 47–66 (1961).
Warner, A. et al. Inappropriate heat dissipation ignites brown fat thermogenesis in mice with a mutant thyroid hormone receptor α1. Proc. Natl Acad. Sci. USA 110, 16241–16246 (2013).
Kolka, C. M. & Bergman, R. N. The barrier within: endothelial transport of hormones. Physiology (Bethesda) 27, 237–247 (2012).
Guney, M. A. et al. Connective tissue growth factor acts within both endothelial cells and β cells to promote proliferation of developing β cells. Proc. Natl Acad. Sci. USA 108, 15242–15247 (2011).
Elfvin, L. G. The ultrastructure of the capillary fenestrae in the adrenal medulla of the rat. J. Ultrastruct. Res. 12, 687–704 (1965).
Møller, M., van Deurs, B. & Westergaard, E. Vascular permeability to proteins and peptides in the mouse pineal gland. Cell Tissue Res. 195, 1–15 (1978).
Lamperti, A. & Mastovich, J. Morphological changes in the hypothalamic arcuate nucleus and median eminence in the golden hamster during the neonatal period. Am. J. Anat. 166, 173–185 (1983).
Simionescu, N., Lupu, F. & Simionescu, M. Rings of membrane sterols surround the openings of vesicles and fenestrae, in capillary endothelium. J. Cell Biol. 97, 1592–1600 (1983).
Hart, T. K. & Pino, R. M. Pseudoislet vascularization. Induction of diaphragm-fenestrated endothelia from the hepatic sinusoids. Lab. Invest. 54, 304–313 (1986).
Esser, S. et al. Vascular endothelial growth factor induces endothelial fenestrations in vitro. J. Cell Biol. 140, 947–959 (1998).
Dvorak, A. M. et al. The vesiculo-vacuolar organelle (VVO): a distinct endothelial cell structure that provides a transcellular pathway for macromolecular extravasation. J. Leukoc. Biol. 59, 100–115 (1996).
Eriksson, A. et al. Small GTP-binding protein Rac is an essential mediator of vascular endothelial growth factor-induced endothelial fenestrations and vascular permeability. Circulation 107, 1532–1538 (2003).
Cao, R. et al. Comparative evaluation of FGF-2-, VEGF-A-, and VEGF-C-induced angiogenesis, lymphangiogenesis, vascular fenestrations, and permeability. Circ. Res. 94, 664–670 (2004).
Yang, Y. et al. Anti-VEGF- and anti-VEGF receptor-induced vascular alteration in mouse healthy tissues. Proc. Natl Acad. Sci. USA 110, 12018–12023 (2013).
Jubb, A. M. et al. Expression of vascular endothelial growth factor, hypoxia inducible factor 1α, and carbonic anhydrase IX in human tumours. J. Clin. Pathol. 57, 504–512 (2004).
Lee, S. L. et al. Hypoxia-induced pathological angiogenesis mediates tumor cell dissemination, invasion, and metastasis in a zebrafish tumor model. Proc. Natl Acad. Sci. USA 106, 19485–19490 (2009).
Hegde, P. S. et al. Predictive impact of circulating vascular endothelial growth factor in four phase III trials evaluating bevacizumab. Clin. Cancer Res. 19, 929–937 (2013).
Wong, A. K. et al. Excessive tumor-elaborated VEGF and its neutralization define a lethal paraneoplastic syndrome. Proc. Natl Acad. Sci. USA 98, 7481–7486 (2001).
Xue, Y. et al. Anti-VEGF agents confer survival advantages to tumor-bearing mice by improving cancer-associated systemic syndrome. Proc. Natl Acad. Sci. USA 105, 18513–18518 (2008).
Zhang, D. et al. Antiangiogenic agents significantly improve survival in tumor-bearing mice by increasing tolerance to chemotherapy-induced toxicity. Proc. Natl Acad. Sci. USA 108, 4117–4122 (2011).
Houck, K. A. et al. The vascular endothelial growth factor family: identification of a fourth molecular species and characterization of alternative splicing of RNA. Mol. Endocrinol. 5, 1806–1814 (1991).
Tischer, E. et al. The human gene for vascular endothelial growth factor. Multiple protein forms are encoded through alternative exon splicing. J. Biol. Chem. 266, 11947–11954 (1991).
Jiang, X. & Couchman, J. R. Perlecan and tumor angiogenesis. J. Histochem. Cytochem. 51, 1393–1410 (2003).
Park, J. E., Keller, G. A. & Ferrara, N. The vascular endothelial growth factor (VEGF) isoforms: differential deposition into the subepithelial extracellular matrix and bioactivity of extracellular matrix-bound VEGF. Mol. Biol. Cell 4, 1317–1326 (1993).
Morbidelli, L. et al. Distinct capillary density and progression promoted by vascular endothelial growth factor-A homodimers and heterodimers. Angiogenesis 1, 117–130 (1997).
Gerhardt, H. et al. VEGF guides angiogenic sprouting utilizing endothelial tip cell filopodia. J. Cell Biol. 161, 1163–1177 (2003).
Poltorak, Z., Cohen, T. & Neufeld, G. The VEGF splice variants: properties, receptors, and usage for the treatment of ischemic diseases. Herz 25, 126–129 (2000).
Vempati, P., Mac Gabhann, F. & Popel, A. S. Quantifying the proteolytic release of extracellular matrix-sequestered VEGF with a computational model. PLoS ONE 5, e11860 (2010).
Ding, G. X. et al. Paraneoplastic symptoms: cachexia, polycythemia, and hypercalcemia are, respectively, related to vascular endothelial growth factor (VEGF) expression in renal clear cell carcinoma. Urol. Oncol. 31, 1820–1825 (2013).
Richardson, G. E. & Johnson, B. E. Paraneoplastic syndromes in lung cancer. Curr. Opin. Oncol. 4, 323–333 (1992).
Pelosof, L. C. & Gerber, D. E. Paraneoplastic syndromes: an approach to diagnosis and treatment. Mayo Clin. Proc. 85, 838–854 (2010).
Aoyagi, T., Mori, I., Ueyama, Y. & Tamaoki, N. Sinusoidal dilatation of the liver as a paraneoplastic manifestation of renal cell carcinoma. Hum. Pathol. 20, 1193–1197 (1989).
Jacobi, G. H., Abdelhamid, S. & Philipp, T. [Stauffer syndrome, paraneoplastic hepatic dysfunction syndrome associated with renal cell carcinoma (author's transl.)]. Urologe A. 15, 78–82 (1976).
Seizinger, B. R. et al. Von Hippel-Lindau disease maps to the region of chromosome 3 associated with renal cell carcinoma. Nature 332, 268–269 (1988).
Maxwell, P. H. et al. The tumour suppressor protein VHL targets hypoxia-inducible factors for oxygen-dependent proteolysis. Nature 399, 271–275 (1999).
Koch, C. A. et al. Somatic VHL gene alterations in MEN2-associated medullary thyroid carcinoma. BMC Cancer 6, 131 (2006).
Kamba, T. et al. VEGF-dependent plasticity of fenestrated capillaries in the normal adult microvasculature. Am. J. Physiol. Heart Circ. Physiol. 290, H560–H576 (2006).
Ebos, J. M., Lee, C. R., Christensen, J. G., Mutsaers, A. J. & Kerbel, R. S. Multiple circulating proangiogenic factors induced by sunitinib malate are tumor-independent and correlate with antitumor efficacy. Proc. Natl Acad. Sci. USA 104, 17069–17074 (2007).
Chen, J., Connor, K. M., Aderman, C. M. & Smith, L. E. Erythropoietin deficiency decreases vascular stability in mice. J. Clin. Invest. 118, 526–533 (2008).
Xue, Y. et al. PDGF-BB modulates hematopoiesis and tumor angiogenesis by inducing erythropoietin production in stromal cells. Nat. Med. 18, 100–110 (2011).
Bocci, G. et al. Increased plasma vascular endothelial growth factor (VEGF) as a surrogate marker for optimal therapeutic dosing of VEGF receptor-2 monoclonal antibodies. Cancer Res. 64, 6616–6625 (2004).
LeCouter, J., Zlot, C., Tejada, M., Peale, F. & Ferrara, N. Bv8 and endocrine gland-derived vascular endothelial growth factor stimulate hematopoiesis and hematopoietic cell mobilization. Proc. Natl Acad. Sci. USA 101, 16813–16818 (2004).
Stacker, S. A., Achen, M. G., Jussila, L., Baldwin, M. E. & Alitalo, K. Lymphangiogenesis and cancer metastasis. Nat. Rev. Cancer 2, 573–583 (2002).
Adams, R. H. & Alitalo, K. Molecular regulation of angiogenesis and lymphangiogenesis. Nat. Rev. Mol. Cell Biol. 8, 464–478 (2007).
Gilbert, M. R. et al. A randomized trial of bevacizumab for newly diagnosed glioblastoma. N. Engl. J. Med. 370, 699–708 (2014).
Sandler, A. et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N. Engl. J. Med. 355, 2542–2550 (2006).
Motzer, R. J. et al. Pazopanib versus sunitinib in metastatic renal-cell carcinoma. N. Engl. J. Med. 369, 722–731 (2013).
Escudier, B. et al. Bevacizumab plus interferon α-2a for treatment of metastatic renal cell carcinoma: a randomised, double-blind phase III trial. Lancet 370, 2103–2111 (2007).
McDermott, D. F. Immunotherapy of metastatic renal cell carcinoma. Cancer 115, 2298–2305 (2009).
Jain, R. K. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science 307, 58–62 (2005).
van der Wall, E., Beijnen, J. H. & Rodenhuis, S. High-dose chemotherapy regimens for solid tumors. Cancer Treat. Rev. 21, 105–132 (1995).
D'Agostino, R. B., Sr. Changing end points in breast-cancer drug approval—the Avastin story. N. Engl. J. Med. 365, e2 (2011).
Perren, T. J. et al. A phase 3 trial of bevacizumab in ovarian cancer. N. Engl. J. Med. 365, 2484–2496 (2011).
Burger, R. A. et al. Incorporation of bevacizumab in the primary treatment of ovarian cancer. N. Engl. J. Med. 365, 2473–2483 (2011).
Miles, D. W. et al. Biomarker results from the AVADO phase 3 trial of first-line bevacizumab plus docetaxel for HER2-negative metastatic breast cancer. Br. J. Cancer 108, 1052–1060 (2013).
Bear, H. D. et al. Bevacizumab added to neoadjuvant chemotherapy for breast cancer. N. Engl. J. Med. 366, 310–320 (2012).
van der Veldt, A. A., Lammertsma, A. A. & Smit, E. F. Reduction in thyroid perfusion after bevacizumab treatment. Thyroid 23, 1329–1330 (2013).
Ahmadieh, H. & Salti, I. Tyrosine kinase inhibitors induced thyroid dysfunction: a review of its incidence, pathophysiology, clinical relevance, and treatment. Biomed Res. Int. 2013, 725410 (2013).
Funakoshi, T. & Shimada, Y. J. Risk of hypothyroidism in patients with cancer treated with sunitinib: a systematic review and meta-analysis. Acta Oncol. 52, 691–702 (2013).
van Cruijsen, H., van der Veldt, A. & Hoekman, K. Tyrosine kinase inhibitors of VEGF receptors: clinical issues and remaining questions. Front. Biosci. (Landmark Ed.) 14, 2248–2268 (2009).
Reismüller, B. et al. Feasibility and tolerability of bevacizumab in children with primary CNS tumors. Pediatr. Blood Cancer 54, 681–686 (2010).
Eisen, T. et al. Targeted therapies for renal cell carcinoma: review of adverse event management strategies. J. Natl Cancer Inst. 104, 93–113 (2012).
Desai, J. et al. Hypothyroidism after sunitinib treatment for patients with gastrointestinal stromal tumors. Ann. Intern. Med. 145, 660–664 (2006).
Wolter, P. et al. The clinical implications of sunitinib-induced hypothyroidism: a prospective evaluation. Br. J. Cancer 99, 448–454 (2008).
Mannavola, D. et al. A novel tyrosine-kinase selective inhibitor, sunitinib, induces transient hypothyroidism by blocking iodine uptake. J. Clin. Endocrinol. Metab. 92, 3531–3534 (2007).
Salem, A. K., Fenton, M. S., Marion, K. M. & Hershman, J. M. Effect of sunitinib on growth and function of FRTL-5 thyroid cells. Thyroid 18, 631–635 (2008).
Wong, E. et al. Sunitinib induces hypothyroidism in advanced cancer patients and may inhibit thyroid peroxidase activity. Thyroid 17, 351–355 (2007).
Braun, D. et al. Tyrosine kinase inhibitors noncompetitively inhibit MCT8-mediated iodothyronine transport. J. Clin. Endocrinol. Metab. 97, E100–E105 (2012).
Kappers, M. H. et al. Sunitinib-induced hypothyroidism is due to induction of type 3 deiodinase activity and thyroidal capillary regression. J. Clin. Endocrinol. Metab. 96, 3087–3094 (2011).
Maynard, M. A. et al. Thyroid hormone inactivation in gastrointestinal stromal tumors. N. Engl. J. Med. 370, 1327–1334 (2014).
Hershman, J. M. & Liwanpo, L. How does sunitinib cause hypothyroidism? Thyroid 20, 243–244 (2010).
Fischer, C. et al. Anti-PlGF inhibits growth of VEGF(R)-inhibitor-resistant tumors without affecting healthy vessels. Cell 131, 463–475 (2007).
Wei, K. et al. A liver Hif-2α-Irs2 pathway sensitizes hepatic insulin signaling and is modulated by Vegf inhibition. Nat. Med. 19, 1331–1337 (2013).
Taniguchi, C. M. et al. Cross-talk between hypoxia and insulin signaling through Phd3 regulates hepatic glucose and lipid metabolism and ameliorates diabetes. Nat. Med. 19, 1325–1330 (2013).
Rock, E. P. et al. Food and Drug Administration drug approval summary: Sunitinib malate for the treatment of gastrointestinal stromal tumor and advanced renal cell carcinoma. Oncologist 12, 107–113 (2007).
Yoshino, T. et al. A case of acute adrenal insufficiency unmasked during sunitinib treatment for metastatic renal cell carcinoma. Jpn J. Clin. Oncol. 42, 764–766 (2012).
Tisdale, M. J. Cachexia in cancer patients. Nat. Rev. Cancer 2, 862–871 (2002).
Folkman, J. & Kalluri, R. Cancer without disease. Nature 427, 787 (2004).
Cao, Y. et al. Vascular endothelial growth factor C induces angiogenesis in vivo. Proc. Natl Acad. Sci. USA 95, 14389–14394 (1998).
Dvorak, H. F., Senger, D. R., Dvorak, A. M., Harvey, V. S. & McDonagh, J. Regulation of extravascular coagulation by microvascular permeability. Science 227, 1059–1061 (1985).
Cao, Y. Tumor angiogenesis and therapy. Biomed. Pharmacother. 59 (Suppl 2), S340–S343 (2005).
Wang, Y. et al. Norrin/Frizzled4 signaling in retinal vascular development and blood brain barrier plasticity. Cell 151, 1332–1344 (2012).
Lyden, D. et al. Impaired recruitment of bone-marrow-derived endothelial and hematopoietic precursor cells blocks tumor angiogenesis and growth. Nat. Med. 7, 1194–1201 (2001).
Acknowledgements
Y.C. thanks Dr S. Lim, at the Department of Microbiology, Tumour and Cell Biology, Karolinska Institute, for the design of Figure 3. Y.C.'s laboratory is supported by research grants from the Swedish Research Council, the Swedish Cancer Foundation, the Karolinska Institute Foundation, the Karolinska Institute Distinguished Professor Award, the Torsten Söderbergs Foundation, the Novo Nordisk Foundation, and the European Research Council advanced grant ANGIOFAT (Project no. 250,021).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Y.C. receives grant support from the Novo Norodisk Foundation and is the founder and a share holder of Clanotech, a Karolinska Development-based biotechnology company that focuses on developing drugs for the treatment of ocular diseases.
Rights and permissions
About this article
Cite this article
Cao, Y. VEGF-targeted cancer therapeutics—paradoxical effects in endocrine organs. Nat Rev Endocrinol 10, 530–539 (2014). https://doi.org/10.1038/nrendo.2014.114
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2014.114
This article is cited by
-
Novel heavily fucosylated glycans as a promising therapeutic target in colorectal cancer
Journal of Translational Medicine (2023)
-
Nuclear PD-L1 promotes EGR1-mediated angiogenesis and accelerates tumorigenesis
Cell Discovery (2023)
-
Targeting angiogenesis in oncology, ophthalmology and beyond
Nature Reviews Drug Discovery (2023)
-
Vascular endothelial growth factor and its receptors regulation in gestational diabetes mellitus and eclampsia
Journal of Translational Medicine (2022)
-
Tubulin carboxypeptidase activity of vasohibin-1 inhibits angiogenesis by interfering with endocytosis and trafficking of pro-angiogenic factor receptors
Angiogenesis (2021)