Abstract
Contemporary management of coronary artery disease relies increasingly on percutaneous techniques combined with medical therapy. Although percutaneous coronary intervention (PCI) can be performed successfully in most lesions, several difficult lesion subsets continue to present unique technical challenges. These complex lesions may be classified according to anatomic criteria, including extensive calcification, thrombus, and chronic occlusions, or by location, such as bifurcations, saphenous vein grafts and unprotected left main. PCI of these lesions often requires novel devices, such as drug-eluting stents, hydrophilic guidewires, distal protection balloons or filters, thrombectomy catheters, rotational atherectomy, and cutting balloons. An integrated approach that combines these devices with specialized techniques and adjunctive pharmacologic agents has greatly improved PCI success rates for these complex lesions.
Key Points
-
Percutaneous coronary intervention, combined with optimal medical therapy, is currently a safe, effective and reliable treatment option for millions of patients with coronary artery disease (CAD)
-
Substantial advances in interventional equipment, novel techniques and adjunctive devices have greatly expanded the scope of percutaneous coronary intervention to include many complex coronary lesion subsets
-
The percutaneous treatment of several types of coronary lesions remains challenging and is associated with increased risk of adverse outcomes
-
Multiple large-scale registries and subgroup analyses of randomized studies have shown similar outcomes following percutaneous or surgical revascularization of unprotected left main disease
-
Incorporating angiographic parameters of CAD severity, the SYNTAX score can be used to risk-stratify and identify the optimal revascularization approach for patients with complex CAD
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Hochman, J. S. et al. Coronary intervention for persistent occlusion after myocardial infarction. N. Engl. J. Med. 355, 2395–2407 (2006).
Shaw, L. J. et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 117, 1283–1291 (2008).
Keeley, E. C., Boura, J. A. & Grines, C. L. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 361, 13–20 (2003).
Seung, K. B. et al. Stents versus coronary-artery bypass grafting for left main coronary artery disease. N. Engl. J. Med. 358, 1781–1792 (2008).
Wilensky, R. L. et al. Relation of percutaneous coronary intervention of complex lesions to clinical outcomes (from the NHLBI Dynamic Registry). Am. J. Cardiol. 90, 216–221 (2002).
Meier, B. et al. Risk of side branch occlusion during coronary angioplasty. Am. J. Cardiol. 53, 10–14 (1984).
Al Suwaidi, J. et al. Immediate and long-term outcome of intracoronary stent implantation for true bifurcation lesions. J. Am. Coll. Cardiol. 35, 929–936 (2000).
Pan, M. et al. Simple and complex stent strategies for bifurcated coronary arterial stenosis involving the side branch origin. Am. J. Cardiol. 83, 1320–1325 (1999).
Sheiban, I. et al. Immediate and long-term results of “T” stenting for bifurcation coronary lesions. Am. J. Cardiol. 85, 1141–1144, A9 (2000).
Iakovou, I. et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 293, 2126–2130 (2005).
Medina, A., Suarez de Lezo, J. & Pan, M. A new classification of coronary bifurcation lesions [Spanish]. Rev. Esp. Cardiol. 59, 183 (2006).
Legrand, V. et al. Percutaneous coronary intervention of bifurcation lesions: state-of-the-art. Insights from the second meeting of the European Bifurcation Club. EuroIntervention 3, 44–49 (2007).
Lefevre, T. et al. Stenting of bifurcation lesions: a rational approach. J. Interv. Cardiol. 14, 573–585 (2001).
Teirstein, P. S. Kissing Palmaz-Schatz stents for coronary bifurcation stenoses. Cathet. Cardiovasc. Diagn. 37, 307–310 (1996).
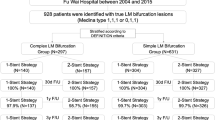
Steigen, T. K. et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation 114, 1955–1961 (2006).
Chevalier, B., Glatt, B., Royer, T. & Guyon, P. Placement of coronary stents in bifurcation lesions by the “culotte” technique. Am. J. Cardiol. 82, 943–949 (1998).
Colombo, A. et al. Modified T-stenting technique with crushing for bifurcation lesions: immediate results and 30-day outcome. Catheter Cardiovasc. Interv. 60, 145–151 (2003).
Sharma, S. K. et al. Simultaneous kissing stents (SKS) technique for treating bifurcation lesions in medium-to-large size coronary arteries. Am. J. Cardiol. 94, 913–917 (2004).
Zhang, F., Dong, L. & Ge, J. Simple versus complex stenting strategy for coronary artery bifurcation lesions in the drug-eluting stent era: a meta-analysis of randomised trials. Heart 95, 1676–1681 (2009).
Colombo, A. et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation 119, 71–78 (2009).
Hildick-Smith, D. et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation 121, 1235–1243 (2010).
Kawaguchi, R. et al. Impact of lesion calcification on clinical and angiographic outcome after sirolimus-eluting stent implantation in real-world patients. Cardiovasc. Revasc. Med. 9, 2–8 (2008).
Moussa, I. et al. Impact of coronary culprit lesion calcium in patients undergoing paclitaxel-eluting stent implantation (a TAXUS-IV sub study). Am. J. Cardiol. 96, 1242–1247 (2005).
Hoffmann, R. et al. Treatment of calcified coronary lesions with Palmaz-Schatz stents. An intravascular ultrasound study. Eur. Heart J. 19, 1224–1231 (1998).
Fourrier, J. L. et al. Percutaneous coronary rotational angioplasty in humans: preliminary report. J. Am. Coll. Cardiol. 14, 1278–1282 (1989).
Tran, T., Brown, M. & Lasala, J. An evidence-based approach to the use of rotational and directional coronary atherectomy in the era of drug-eluting stents: when does it make sense? Catheter Cardiovasc. Interv. 72, 650–662 (2008).
Ahn, S. S., Auth, D., Marcus, D. R. & Moore, W. S. Removal of focal atheromatous lesions by angioscopically guided high-speed rotary atherectomy. Preliminary experimental observations. J. Vasc. Surg. 7, 292–300 (1988).
Dill, T. et al. A randomized comparison of balloon angioplasty versus rotational atherectomy in complex coronary lesions (COBRA study). Eur. Heart J. 21, 1759–1766 (2000).
Guerin, Y. et al. Rotational atherectomy with adjunctive balloon angioplasty versus conventional percutaneous transluminal coronary angioplasty in type B2 lesions: results of a randomized study. Am. Heart J. 131, 879–883 (1996).
Clavijo, L. C. et al. Sirolimus-eluting stents and calcified coronary lesions: clinical outcomes of patients treated with and without rotational atherectomy. Catheter Cardiovasc. Interv. 68, 873–878 (2006).
Barath, P., Fishbein, M. C., Vari, S. & Forrester, J. S. Cutting balloon: a novel approach to percutaneous angioplasty. Am. J. Cardiol. 68, 1249–1252 (1991).
Okura, H. et al. Mechanisms of acute lumen gain following cutting balloon angioplasty in calcified and noncalcified lesions: an intravascular ultrasound study. Catheter Cardiovasc. Interv. 57, 429–436 (2002).
Brown, R., Kochar, G., Maniet, A. R. & Banka, V. S. Effects of coronary angioplasty using progressive dilation on ostial stenosis of the left anterior descending artery. Am. J. Cardiol. 71, 245–247 (1993).
Inoue, T. et al. Lower expression of neutrophil adhesion molecule indicates less vessel wall injury and might explain lower restenosis rate after cutting balloon angioplasty. Circulation 97, 2511–2518 (1998).
Stone, G. W. et al. Percutaneous recanalization of chronically occluded coronary arteries: a consensus document: part I. Circulation 112, 2364–2372 (2005).
Kahn, J. K. Angiographic suitability for catheter revascularization of total coronary occlusions in patients from a community hospital setting. Am. Heart J. 126, 561–564 (1993).
Katsuragawa, M., Fujiwara, H., Miyamae, M. & Sasayama, S. Histologic studies in percutaneous transluminal coronary angioplasty for chronic total occlusion: comparison of tapering and abrupt types of occlusion and short and long occluded segments. J. Am. Coll. Cardiol. 21, 604–611 (1993).
King, S. B. 3rd et al. A randomized trial comparing coronary angioplasty with coronary bypass surgery. Emory Angioplasty versus Surgery Trial (EAST). N. Engl. J. Med. 331, 1044–1050 (1994).
Anderson, H. V. et al. A contemporary overview of percutaneous coronary interventions. The American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). J. Am. Coll. Cardiol. 39, 1096–1103 (2002).
Hoye, A., van Domburg, R. T., Sonnenschein, K. & Serruys, P. W. Percutaneous coronary intervention for chronic total occlusions: the Thoraxcenter experience 1992–2002. Eur. Heart J. 26, 2630–2636 (2005).
Olivari, Z. et al. Immediate results and one-year clinical outcome after percutaneous coronary interventions in chronic total occlusions: data from a multicenter, prospective, observational study (TOAST-GISE). J. Am. Coll. Cardiol. 41, 1672–1678 (2003).
Horie, H. et al. Long-term beneficial effect of late reperfusion for acute anterior myocardial infarction with percutaneous transluminal coronary angioplasty. Circulation 98, 2377–2382 (1998).
Silva, J. C. et al. Late coronary artery recanalization effects on left ventricular remodelling and contractility by magnetic resonance imaging. Eur. Heart J. 26, 36–43 (2005).
Valenti, R. et al. Impact of complete revascularization with percutaneous coronary intervention on survival in patients with at least one chronic total occlusion. Eur. Heart J. 29, 2336–2342 (2008).
de Labriolle, A. et al. Comparison of safety, efficacy, and outcome of successful versus unsuccessful percutaneous coronary intervention in “true” chronic total occlusions. Am. J. Cardiol. 102, 1175–1181 (2008).
Stone, G. W. et al. Percutaneous recanalization of chronically occluded coronary arteries: procedural techniques, devices, and results. Catheter Cardiovasc. Interv. 66, 217–236 (2005).
Baim, D. S. et al. Utility of the Safe-Cross-guided radiofrequency total occlusion crossing system in chronic coronary total occlusions (results from the Guided Radio Frequency Energy Ablation of Total Occlusions Registry Study). Am. J. Cardiol. 94, 853–858 (2004).
Grube, E. et al. High-frequency mechanical vibration to recanalize chronic total occlusions after failure to cross with conventional guidewires. J. Invasive Cardiol. 18, 85–91 (2006).
Melzi, G. et al. A novel approach to chronic total occlusions: the crosser system. Catheter Cardiovasc. Interv. 68, 29–35 (2006).
Weisz, G. & Moses, J. W. New percutaneous approaches for chronic total occlusion of coronary arteries. Expert Rev. Cardiovasc. Ther. 5, 231–241 (2007).
Saito, S. Different strategies of retrograde approach in coronary angioplasty for chronic total occlusion. Catheter Cardiovasc. Interv. 71, 8–19 (2008).
Sheiban, I. et al. The retrograde coronary approach for chronic total occlusions: mid-term results and technical tips & tricks. J. Interv. Cardiol. 20, 466–473 (2007).
Rathore, S. et al. Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ. Cardiovasc. Interv. 2, 124–132 (2009).
Migliorini, A. et al. Drug-eluting stent-supported percutaneous coronary intervention for chronic total coronary occlusion. Catheter Cardiovasc. Interv. 67, 344–348 (2006).
Ge, L. et al. Immediate and mid-term outcomes of sirolimus-eluting stent implantation for chronic total occlusions. Eur. Heart J. 26, 1056–1062 (2005).
Chaitman, B. R. et al. Angiographic prevalence of high-risk coronary artery disease in patient subsets (CASS). Circulation 64, 360–367 (1981).
Campeau, L., Corbara, F., Crochet, D. & Petitclerc, R. Left main coronary artery stenosis: the influence of aortocoronary bypass surgery on survival. Circulation 57, 1111–1115 (1978).
Takaro, T., Hultgren, H. N., Lipton, M. J. & Detre, K. M. The VA cooperative randomized study of surgery for coronary arterial occlusive disease II. Subgroup with significant left main lesions. Circulation 54, III107–III117 (1976).
Kushner, F. G. et al. 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction (updating the 2004 Guideline and 2007 Focused Update) and ACC/AHA/SCAI Guidelines on Percutaneous Coronary Intervention (updating the 2005 Guideline and 2007 Focused Update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 120, 2271–2306 (2009).
Serruys, P. W. et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N. Engl. J. Med. 360, 961–972 (2009).
Palmerini, T. et al. Ostial and midshaft lesions vs. bifurcation lesions in 1111 patients with unprotected left main coronary artery stenosis treated with drug-eluting stents: results of the survey from the Italian Society of Invasive Cardiology. Eur. Heart J. 30, 2087–2094 (2009).
Chieffo, A. et al. Percutaneous treatment with drug-eluting stent implantation versus bypass surgery for unprotected left main stenosis: a single-center experience. Circulation 113, 2542–2547 (2006).
Buszman, P. E. et al. Acute and late outcomes of unprotected left main stenting in comparison with surgical revascularization. J. Am. Coll. Cardiol. 51, 538–545 (2008).
Lee, M. S. et al. Comparison of coronary artery bypass surgery with percutaneous coronary intervention with drug-eluting stents for unprotected left main coronary artery disease. J. Am. Coll. Cardiol. 47, 864–870 (2006).
Kereiakes, D. J. & Faxon, D. P. Left main coronary revascularization at the crossroads. Circulation 113, 2480–2484 (2006).
Park, S. J. et al. Duration of dual antiplatelet therapy after implantation of drug-eluting stents. N. Engl. J. Med. 362, 1374–1382 (2010).
Park, S. J. et al. Elective stenting of unprotected left main coronary artery stenosis: effect of debulking before stenting and intravascular ultrasound guidance. J. Am. Coll. Cardiol. 38, 1054–1060 (2001).
Ito, H. et al. Clinical implications of the 'no reflow' phenomenon. A predictor of complications and left ventricular remodeling in reperfused anterior wall myocardial infarction. Circulation 93, 223–228 (1996).
Stone, G. W. et al. Impact of normalized myocardial perfusion after successful angioplasty in acute myocardial infarction. J. Am. Coll. Cardiol. 39, 591–597 (2002).
Topol, E. J. & Yadav, J. S. Recognition of the importance of embolization in atherosclerotic vascular disease. Circulation 101, 570–580 (2000).
Henriques, J. P. et al. Incidence and clinical significance of distal embolization during primary angioplasty for acute myocardial infarction. Eur. Heart J. 23, 1112–1117 (2002).
Ross, A. M., Gibbons, R. J., Stone, G. W., Kloner, R. A. & Alexander, R. W. A randomized, double-blinded, placebo-controlled multicenter trial of adenosine as an adjunct to reperfusion in the treatment of acute myocardial infarction (AMISTAD-II). J. Am. Coll. Cardiol. 45, 1775–1780 (2005).
Amit, G. et al. Intracoronary nitroprusside for the prevention of the no-reflow phenomenon after primary percutaneous coronary intervention in acute myocardial infarction. A randomized, double-blind, placebo-controlled clinical trial. Am. Heart J. 152, 887.e9–887.e14 (2006).
Hillegass, W. B., Dean, N. A., Liao, L., Rhinehart, R. G. & Myers, P. R. Treatment of no-reflow and impaired flow with the nitric oxide donor nitroprusside following percutaneous coronary interventions: initial human clinical experience. J. Am. Coll. Cardiol. 37, 1335–1343 (2001).
Hang, C. L. et al. Early administration of intracoronary verapamil improves myocardial perfusion during percutaneous coronary interventions for acute myocardial infarction. Chest 128, 2593–2598 (2005).
Gick, M. et al. Randomized evaluation of the effects of filter-based distal protection on myocardial perfusion and infarct size after primary percutaneous catheter intervention in myocardial infarction with and without ST-segment elevation. Circulation 112, 1462–1469 (2005).
Stone, G. W. et al. Distal microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction: a randomized controlled trial. JAMA 293, 1063–1072 (2005).
De Luca, G. et al. Adjunctive mechanical devices to prevent distal embolization in patients undergoing mechanical revascularization for acute myocardial infarction: a meta-analysis of randomized trials. Am. Heart J. 153, 343–353 (2007).
Bavry, A. A., Kumbhani, D. J. & Bhatt, D. L. Role of adjunctive thrombectomy and embolic protection devices in acute myocardial infarction: a comprehensive meta-analysis of randomized trials. Eur. Heart J. 29, 2989–3001 (2008).
Svilaas, T. et al. Thrombus aspiration during primary percutaneous coronary intervention. N. Engl. J. Med. 358, 557–567 (2008).
Kaltoft, A. et al. Routine thrombectomy in percutaneous coronary intervention for acute ST-segment-elevation myocardial infarction: a randomized, controlled trial. Circulation 114, 40–47 (2006).
Silva-Orrego, P. et al. Thrombus aspiration before primary angioplasty improves myocardial reperfusion in acute myocardial infarction: the DEAR-MI (Dethrombosis to Enhance Acute Reperfusion in Myocardial Infarction) study. J. Am. Coll. Cardiol. 48, 1552–1559 (2006).
Babaev, A. et al. Trends in management and outcomes of patients with acute myocardial infarction complicated by cardiogenic shock. JAMA 294, 448–454 (2005).
Sjauw, K. D. et al. A systematic review and meta-analysis of intra-aortic balloon pump therapy in ST-elevation myocardial infarction: should we change the guidelines? Eur. Heart J. 30, 459–468 (2009).
Abdel-Wahab, M. et al. Comparison of hospital mortality with intra-aortic balloon counterpulsation insertion before versus after primary percutaneous coronary intervention for cardiogenic shock complicating acute myocardial infarction. Am. J. Cardiol. 105, 967–971 (2010).
Sjauw, K. D. et al. Left ventricular unloading in acute ST-segment elevation myocardial infarction patients is safe and feasible and provides acute and sustained left ventricular recovery. J. Am. Coll. Cardiol. 51, 1044–1046 (2008).
Thiele, H. et al. Reversal of cardiogenic shock by percutaneous left atrial-to-femoral arterial bypass assistance. Circulation 104, 2917–2922 (2001).
Seyfarth, M. et al. A randomized clinical trial to evaluate the safety and efficacy of a percutaneous left ventricular assist device versus intra-aortic balloon pumping for treatment of cardiogenic shock caused by myocardial infarction. J. Am. Coll. Cardiol. 52, 1584–1588 (2008).
Motwani, J. G. & Topol, E. J. Aortocoronary saphenous vein graft disease: pathogenesis, predisposition, and prevention. Circulation 97, 916–931 (1998).
Cameron, A., Davis, K. B., Green, G. & Schaff, H. V. Coronary bypass surgery with internal-thoracic-artery grafts—effects on survival over a 15-year period. N. Engl. J. Med. 334, 216–219 (1996).
Campeau, L. et al. The relation of risk factors to the development of atherosclerosis in saphenous-vein bypass grafts and the progression of disease in the native circulation. A study 10 years after aortocoronary bypass surgery. N. Engl. J. Med. 311, 1329–1332 (1984).
Chen, L. et al. Angiographic features of vein grafts versus ungrafted coronary arteries in patients with unstable angina and previous bypass surgery. J. Am. Coll. Cardiol. 28, 1493–1499 (1996).
Douglas, J. S. Jr. Percutaneous approaches to recurrent myocardial ischemia in patients with prior surgical revascularization. Semin. Thorac. Cardiovasc. Surg. 6, 98–108 (1994).
Cameron, A., Kemp, H. G. Jr & Green, G. E. Reoperation for coronary artery disease. 10 years of clinical follow-up. Circulation 78, I158–I162 (1988).
Bhatt, D. L. & Topol, E. J. Percutaneous coronary intervention for patients with prior bypass surgery: therapy in evolution. Am. J. Med. 108, 176–177 (2000).
Hong, M. K. et al. Creatine kinase-MB enzyme elevation following successful saphenous vein graft intervention is associated with late mortality. Circulation 100, 2400–2405 (1999).
Le May, M. R. et al. Predictors of long-term outcome after stent implantation in a saphenous vein graft. Am. J. Cardiol. 83, 681–686 (1999).
Mautner, S. L. Mautner, G. C. Hunsberger, S. A. & Roberts, W. C. Comparison of composition of atherosclerotic plaques in saphenous veins used as aortocoronary bypass conduits with plaques in native coronary arteries in the same men. Am. J. Cardiol. 70, 1380–1387 (1992).
Webb, J. G. et al. Retrieval and analysis of particulate debris after saphenous vein graft intervention. J. Am. Coll. Cardiol. 34, 468–475 (1999).
Roffi, M. et al. Lack of benefit from intravenous platelet glycoprotein IIb/IIIa receptor inhibition as adjunctive treatment for percutaneous interventions of aortocoronary bypass grafts: a pooled analysis of five randomized clinical trials. Circulation 106, 3063–3067 (2002).
Baim, D. S. et al. Randomized trial of a distal embolic protection device during percutaneous intervention of saphenous vein aorto-coronary bypass grafts. Circulation 105, 1285–1290 (2002).
Stone, G. W. et al. Randomized comparison of distal protection with a filter-based catheter and a balloon occlusion and aspiration system during percutaneous intervention of diseased saphenous vein aorto-coronary bypass grafts. Circulation 108, 548–553 (2003).
Smith, S. C. Jr et al. ACC/AHA/SCAI 2005 Guideline Update for Percutaneous Coronary Intervention-Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention). J. Am. Coll. Cardiol. 47, 216–235 (2006).
Hanekamp, C. E. et al. Randomized study to compare balloon angioplasty and elective stent implantation in venous bypass grafts: the Venestent study. Catheter Cardiovasc. Interv. 60, 452–457 (2003).
Savage, M. P. et al. Stent placement compared with balloon angioplasty for obstructed coronary bypass grafts. Saphenous Vein De Novo Trial Investigators. N. Engl. J. Med. 337, 740–747 (1997).
Brilakis, E. S. et al. A randomized controlled trial of a paclitaxel-eluting stent versus a similar bare-metal stent in saphenous vein graft lesions the SOS (Stenting of Saphenous Vein Grafts) trial. J. Am. Coll. Cardiol. 53, 919–928 (2009).
Vermeersch, P. et al. Randomized double-blind comparison of sirolimus-eluting stent versus bare-metal stent implantation in diseased saphenous vein grafts: six-month angiographic, intravascular ultrasound, and clinical follow-up of the RRISC Trial. J. Am. Coll. Cardiol. 48, 2423–2431 (2006).
Vermeersch, P. et al. Increased late mortality after sirolimus-eluting stents versus bare-metal stents in diseased saphenous vein grafts: results from the randomized DELAYED RRISC Trial. J. Am. Coll. Cardiol. 50, 261–267 (2007).
Daemen, J. et al. Long-term safety and efficacy of percutaneous coronary intervention with stenting and coronary artery bypass surgery for multivessel coronary artery disease: a meta-analysis with 5-year patient-level data from the ARTS, ERACI-II, MASS-II, and SoS trials. Circulation 118, 1146–1154 (2008).
Sianos, G. et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 1, 219–227 (2005).
Acknowledgements
Laurie Barclay, freelance writer and reviewer, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the MedscapeCME-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Contributions
U. Baber researched data to include in the manuscript. A. Kini and S. Sharma contributed to discussion of content for the article. U. Baber and A. Kini wrote the first draft of the article. S. Sharma reviewed and edited the manuscript before submission. U. Baber and S. Sharma revised the manuscript in response to the peer-reviewers' comments.
Corresponding author
Ethics declarations
Competing interests
The journal Chief Editor B. Mearns and the CME questions author L. Barclay declare no competing interests.
Rights and permissions
About this article
Cite this article
Baber, U., Kini, A. & Sharma, S. Stenting of complex lesions: an overview. Nat Rev Cardiol 7, 485–496 (2010). https://doi.org/10.1038/nrcardio.2010.116
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2010.116
This article is cited by
-
Coronary orbital atherectomy using a five-French guiding catheter
Cardiovascular Intervention and Therapeutics (2022)
-
Ostial lesion of the anterior descending coronary artery treated via Szabo technique supported by stent boost imaging: a case report
Journal of Cardiothoracic Surgery (2021)
-
Contribution of ESC DAPT guideline-endorsed high thrombotic risk features to long-term clinical outcomes among patients with and without high bleeding risk after PCI
BMC Cardiovascular Disorders (2020)
-
Benefit-Risk Profile of DAPT Continuation Beyond 1 Year after PCI in Patients with High Thrombotic Risk Features as Endorsed by 2018 ESC/EACTS Myocardial Revascularization Guideline
Cardiovascular Drugs and Therapy (2020)
-
A “Train-Track” Technique in Anatomic Reconstruction of SVC Bifurcation Complicated by Cardiac Tamponade: An Introspection
CardioVascular and Interventional Radiology (2017)