Abstract
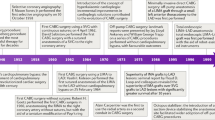
Patients who have undergone coronary artery bypass graft (CABG) surgery are susceptible to bypass graft failure and progression of native coronary artery disease. Although the saphenous vein graft (SVG) was traditionally the most-used conduit, arterial grafts (including the left and right internal thoracic arteries and the radial artery) have improved patency rates. However, the need for secondary revascularization remains common, and percutaneous coronary intervention (PCI) has become the most common modality of secondary revascularization after CABG surgery. Procedural characteristics and clinical outcomes differ considerably from those associated with PCI in patients without previous CABG surgery, owing to altered coronary anatomy and differences in conduit pathophysiology. In particular, SVG PCI carries an increased risk of complications, and operators are shifting their focus towards embolic protection strategies and complex native-vessel interventions, increasingly using SVGs as conduits to facilitate native-vessel PCI rather than pursuing SVG PCI. In this Review, we discuss the differences in conduit pathophysiology, changes in CABG surgery techniques, and the latest evidence in terms of PCI in patients with previous CABG surgery, with a particular emphasis on safety and long-term efficacy. We explore the subject of contemporary CABG surgery and subsequent percutaneous revascularization in this complex patient population.
Key points
-
Coronary artery bypass graft (CABG) surgery has evolved over the years because saphenous vein graft harvesting techniques and expanded use of arterial grafts have improved graft patency.
-
Peri-operative graft failure is a rare complication that can be difficult to recognize during CABG surgery.
-
Venous and arterial grafts vary in pathophysiology, which leads to differences in graft failure modes and relevant considerations in percutaneous coronary revascularization techniques.
-
The need for subsequent revascularization after CABG surgery might occur; the choice of revascularization method depends on patient anatomy and characteristics, with percutaneous coronary intervention being the main treatment modality.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Alexander, J. H. & Smith, P. K. Coronary-artery bypass grafting. N. Eng. J. Med. 374, 1954–1964 (2016).
Brilakis, E. S. et al. Percutaneous coronary intervention in native arteries versus bypass grafts in prior coronary artery bypass grafting patients: a report from the National Cardiovascular Data Registry. JACC Cardiovasc. Interv. 4, 844–850 (2011).
Hlatky, M. A. et al. Adoption and effectiveness of internal mammary artery grafting in coronary artery bypass surgery among Medicare beneficiaries. J. Am. Coll. Cardiol. 63, 33–39 (2014).
Hillis, L. D. et al. 2011 ACCF/AHA Guideline for Coronary Artery Bypass Graft Surgery. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Developed in collaboration with the American Association for Thoracic Surgery, Society of Cardiovascular Anesthesiologists, and Society of Thoracic Surgeons. J. Am. Coll. Cardiol. 58, e123–e210 (2011).
Neumann, F.-J. et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 40, 87–165 (2018).
Lopes, R. D. et al. Endoscopic versus open vein-graft harvesting in coronary-artery bypass surgery. N. Eng. J. Med. 361, 235–244 (2009).
Sastry, P. et al. The influence of endoscopic vein harvesting on outcomes after coronary bypass grafting: a meta-analysis of 267 525 patients. Eur. J. Cardiothorac. Surg. 44, 980–989 (2013).
Zenati, M. A. et al. Randomized trial of endoscopic or open vein-graft harvesting for coronary-artery bypass. N. Eng. J. Med. 380, 132–141 (2018).
Souza, D. S. et al. Harvesting the saphenous vein with surrounding tissue for CABG provides long-term graft patency comparable to the left internal thoracic artery: results of a randomized longitudinal trial. J. Thorac. Cardiovasc. Surg. 132, 373–378 (2006).
Deb, S. et al. SUPERIOR SVG: no touch saphenous harvesting to improve patency following coronary bypass grafting (a multi-centre randomized control trial, NCT01047449). J. Cardiothorac. Surg. 14, 85 (2019).
Gaudino, M. et al. Mechanisms, consequences, and prevention of coronary graft failure. Circulation 136, 1749–1764 (2017).
Gaudino, M. et al. Radial-artery or saphenous-vein grafts in coronary-artery bypass surgery. N. Engl. J. Med. 378, 2069–2077 (2018).
Gaudino, M. et al. The radial artery for percutaneous coronary procedures or surgery? J. Am. Coll. Cardiol. 71, 1167–1175 (2018).
Mounsey, C. A., Mawhinney, J. A., Werner, R. S. & Taggart, D. P. Does previous transradial catheterization preclude use of the radial artery as a conduit in coronary artery bypass surgery? Circulation 134, 681–688 (2016).
Ruzieh, M., Moza, A., Bangalore, B. S., Schwann, T. & Tinkel, J. L. Effect of transradial catheterisation on patency rates of radial arteries used as a conduit for coronary bypass. Heart Lung Circ. 26, 296–300 (2017).
Maniar, H. S. et al. Effect of target stenosis and location on radial artery graft patency. J. Thorac. Cardiovasc. Surg. 123, 45–52 (2002).
Desai Nimesh, D. et al. Impact of patient and target-vessel characteristics on arterial and venous bypass graft patency. Circulation 115, 684–691 (2007).
Leonard, J. R. et al. The radial artery: results and technical considerations. J. Card. Surg. 33, 213–218 (2018).
Patel, A. N. et al. Endoscopic radial artery harvesting is better than the open technique. Ann. Thorac. Surg. 78, 149–153 (2004).
Taggart, D. P. et al. Bilateral versus single internal-thoracic-artery grafts at 10 years. N. Engl. J. Med. 380, 437–446 (2019).
Yi, G., Shine, B., Rehman, S. M., Altman, D. G. & Taggart, D. P. Effect of bilateral internal mammary artery grafts on long-term survival: a meta-analysis approach. Circulation 130, 539–545 (2014).
Kurlansky, P. A. et al. Location of the second internal mammary artery graft does not influence outcome of coronary artery bypass grafting. Ann. Thorac. Surg. 91, 1378–1383 (2011).
Sabik Joseph, F. et al. Does location of the second internal thoracic artery graft influence outcome of coronary artery bypass grafting? Circulation 118, S210–S215 (2008).
Tatoulis, J., Buxton, B. F. & Fuller, J. A. The right internal thoracic artery: is it underutilized? Curr. Opin. Cardiol. 26, 528–535 (2011).
Tatoulis, J., Buxton, B. F. & Fuller, J. A. The right internal thoracic artery: the forgotten conduit — 5,766 patients and 991 angiograms. Ann. Thorac. Surg. 92, 9–15 (2011).
Glineur, D. et al. Bilateral internal thoracic artery configuration for coronary artery bypass surgery: a prospective randomized trial. Circ. Cardiovasc. Interv. 9, e003518 (2016).
Gaudino, M. et al. Radial artery versus right internal thoracic artery versus saphenous vein as the second conduit for coronary artery bypass surgery: a network meta-analysis of clinical outcomes. J. Am. Heart Assoc. 8, e010839 (2019).
Rocha, R. V. et al. Multiple arterial grafting is associated with better outcomes for coronary artery bypass grafting patients. Circulation 138, 2081–2090 (2018).
Gaudino, M. et al. Three arterial grafts improve late survival: a meta-analysis of propensity-matched studies. Circulation 135, 1036–1044 (2017).
Rocha, R. V. et al. Long-term outcomes associated with total arterial revascularization vs non-total arterial revascularization. JAMA Cardiol. 5, 507–514 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/show/NCT03217006 (2021).
McKavanagh, P., Yanagawa, B., Zawadowski, G. & Cheema, A. Management and prevention of saphenous vein graft failure: a review. Cardiol. Ther. 6, 203–223 (2017).
Thielmann, M. et al. Emergency re-revascularization with percutaneous coronary intervention, reoperation, or conservative treatment in patients with acute perioperative graft failure following coronary artery bypass surgery. Eur. J. Cardiothorac. Surg. 30, 117–125 (2006).
Zhao, D. X. et al. Routine intraoperative completion angiography after coronary artery bypass grafting and 1-stop hybrid revascularization results from a fully integrated hybrid catheterization laboratory/operating room. J. Am. Coll. Cardiol. 53, 232–241 (2009).
Harskamp, R. E., Lopes, R. D., Baisden, C. E., de Winter, R. J. & Alexander, J. H. Saphenous vein graft failure after coronary artery bypass surgery: pathophysiology, management, and future directions. Ann. Surg. 257, 824–833 (2013).
Campbell, P. G. et al. Non-invasive assessment of saphenous vein graft patency in asymptomatic patients. Br. J. Radiol. 82, 291–295 (2009).
Gaudino, M. et al. Effect of calcium-channel blocker therapy on radial artery grafts after coronary bypass surgery. J. Am. Coll. Cardiol. 73, 2299–2306 (2019).
Berger, A. et al. Long-term patency of internal mammary artery bypass grafts: relationship with preoperative severity of the native coronary artery stenosis. Circulation 110, Ii36–Ii40 (2004).
Harskamp, R. E. et al. Frequency and predictors of internal mammary artery graft failure and subsequent clinical outcomes: insights from the project of ex-vivo vein graft engineering via transfection (PREVENT) IV trial. Circulation 133, 131–138 (2016).
Shelton, M. E. et al. A comparison of morphologic and angiographic findings in long-term internal mammary artery and saphenous vein bypass grafts. J. Am. Coll. Cardiol. 11, 297–307 (1988).
Thielmann, M. et al. ESC Joint Working Groups on Cardiovascular Surgery and the Cellular Biology of the Heart Position Paper: Perioperative myocardial injury and infarction in patients undergoing coronary artery bypass graft surgery. Eur. Heart J. 38, 2392–2407 (2017).
Hausenloy, D. J., Boston-Griffiths, E. & Yellon, D. M. Cardioprotection during cardiac surgery. Cardiovasc. Res. 94, 253–265 (2012).
Laflamme, M. et al. Management of early postoperative coronary artery bypass graft failure. Interact. Cardiovasc. Thorac. Surg. 14, 452–456 (2012).
Alqahtani, F. et al. Incidence, predictors, and outcomes of in-hospital percutaneous coronary intervention following coronary artery bypass grafting. J. Am. Coll. Cardiol. 73, 415–423 (2019).
Sef, D. et al. Management of perioperative myocardial ischaemia after isolated coronary artery bypass graft surgery. Open Heart 6, e001027 (2019).
Chiesi. Cangrelor (KENGREAL®). Prescribing Information (Chiesi Ltd, 2016).
Anderson, J. R. & Riding, D. Glycoprotein IIb/IIIa inhibitors in patients with renal insufficiency undergoing percutaneous coronary intervention. Cardiol. Rev. 16, 213–218 (2008).
Rodés-Cabau, J. et al. Sealing intermediate nonobstructive coronary saphenous vein graft lesions with drug-eluting stents as a new approach to reducing cardiac events. Circ. Cardiovasc. Interv. 9, e004336 (2016).
Hlatky, M. A. et al. Use of medications for secondary prevention after coronary bypass surgery compared with percutaneous coronary intervention. J. Am. Coll. Cardiol. 61, 295–301 (2013).
Pinho-Gomes, A. C. et al. Compliance with guideline-directed medical therapy in contemporary coronary revascularization trials. J. Am. Coll. Cardiol. 71, 591–602 (2018).
Kulik, A. et al. Secondary prevention after coronary artery bypass graft surgery: a scientific statement from the American Heart Association. Circulation 131, 927–964 (2015).
Escaned, J. Secondary revascularization after CABG surgery. Nat. Rev. Cardiol. 9, 540–549 (2012).
Dangas, G. D. et al. Impact of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump on prognostically important clinical outcomes in patients undergoing high-risk percutaneous coronary intervention (from the PROTECT II randomized trial). Am. J. Cardiol. 113, 222–228 (2014).
O’Neill, W. W. et al. A prospective, randomized clinical trial of hemodynamic support with Impella 2.5 versus intra-aortic balloon pump in patients undergoing high-risk percutaneous coronary intervention: the PROTECT II study. Circulation 126, 1717–1727 (2012).
Tavano, D. et al. Percutaneous coronary intervention in patients with a single remaining vessel. Am. J. Cardiol. 99, 470–471 (2007).
Hess, C. N. et al. Saphenous vein graft failure after coronary artery bypass surgery: insights from PREVENT IV. Circulation 130, 1445–1451 (2014).
Fitzgibbon, G. M. et al. Coronary bypass graft fate and patient outcome: angiographic follow-up of 5,065 grafts related to survival and reoperation in 1,388 patients during 25 years. J. Am. Coll. Cardiol. 28, 616–626 (1996).
Xenogiannis, I. et al. Update on cardiac catheterization in patients with prior coronary artery bypass graft surgery. JACC Cardiovasc. Interv. 12, 1635–1649 (2019).
Brilakis, E. S. et al. Percutaneous coronary intervention in native coronary arteries versus bypass grafts in patients with prior coronary artery bypass graft surgery: insights from the Veterans Affairs Clinical Assessment, Reporting, and Tracking Program. JACC Cardiovasc. Interv. 9, 884–893 (2016).
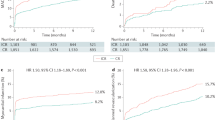
Rathod Krishnaraj, S. et al. Prior coronary artery bypass graft surgery and outcome after percutaneous coronary intervention: an observational study from the Pan-London percutaneous coronary intervention registry. J. Am. Heart Assoc. 9, e014409 (2020).
Ahmed, J. M. et al. Influence of gender on early and one-year clinical outcomes after saphenous vein graft stenting. Am. J. Cardiol. 87, 401–405 (2001).
Ahmed, J. M. et al. Influence of diabetes mellitus on early and late clinical outcomes in saphenous vein graft stenting. J. Am. Coll. Cardiol. 36, 1186–1193 (2000).
Coolong, A. et al. Saphenous vein graft stenting and major adverse cardiac events: a predictive model derived from a pooled analysis of 3958 patients. Circulation 117, 790–797 (2008).
Baim, D. S. et al. Randomized trial of a distal embolic protection device during percutaneous intervention of saphenous vein aorto-coronary bypass grafts. Circulation 105, 1285–1290 (2002).
Shoaib, A. et al. Outcomes following percutaneous coronary intervention in saphenous vein grafts with and without embolic protection devices. JACC Cardiovasc. Interv. 12, 2286–2295 (2019).
Valle, J. A. et al. Contemporary use of embolic protection devices during saphenous vein graft intervention. Circ. Cardiovasc. Interv. 12, e007636 (2019).
Levine, G. N. et al. 2011 ACCF/AHA/SCAI Guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 124, e574–e651 (2011).
Pereg, D. et al. Native coronary artery patency after coronary artery bypass surgery. JACC Cardiovasc. Interv. 7, 761–767 (2014).
Chirumamilla, A. P. et al. High platelet reactivity on clopidogrel therapy correlates with increased coronary atherosclerosis and calcification: a volumetric intravascular ultrasound study. JACC Cardiovasc. Imaging 5, 540–549 (2012).
Nikolakopoulos, I. et al. Follow-up outcomes after chronic total occlusion percutaneous coronary intervention in patients with and without prior coronary artery bypass graft surgery: insights from the PROGRESS-CTO registry. J. Invasive Cardiol. 32, 315–320 (2020).
Kirtane Ajay, J. et al. Treatment of higher-risk patients with an indication for revascularization. Circulation 134, 422–431 (2016).
Dautov, R., Manh Nguyen, C., Altisent, O., Gibrat, C. & Rinfret, S. Recanalization of chronic total occlusions in patients with previous coronary bypass surgery and consideration of retrograde access via saphenous vein grafts. Circ. Cardiovasc. Interv. 9, e003515 (2016).
Xenogiannis, I. et al. Retrograde chronic total occlusion percutaneous coronary intervention via saphenous vein graft. JACC Cardiovasc. Interv. 13, 517–526 (2020).
Tajti, P. et al. Retrograde CTO-PCI of native coronary arteries via left internal mammary artery grafts: insights from a multicenter U.S. Registry. J. Invasive Cardiol. 30, 89–96 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/show/NCT03805048 (2020).
Januszek, R. A. et al. Predictors of periprocedural complications in patients undergoing percutaneous coronary interventions within coronary artery bypass grafts. Cardiol. J. 26, 633–644 (2019).
Rogers, J. H. & Calhoun, R. F. 2nd Diagnosis and management of subclavian artery stenosis prior to coronary artery bypass grafting in the current era. J. Card. Surg. 22, 20–25 (2007).
Gruberg, L. et al. Percutaneous revascularization of the internal mammary artery graft: short- and long-term outcomes. J. Am. Coll. Cardiol. 35, 944–948 (2000).
Buch, A. N. et al. Comparison of outcomes between bare metal stents and drug-eluting stents for percutaneous revascularization of internal mammary grafts. Am. J. Cardiol. 98, 722–724 (2006).
Sharma, A. K. et al. Clinical outcomes following stent implantation in internal mammary artery grafts. Catheter. Cardiovasc. Interv. 59, 436–441 (2003).
Núñez-Gil, I. J. et al. Internal mammary artery graft failure: clinical features, management, and long-term outcomes. Indian Heart J. 70 (Suppl. 3), 329–337 (2018).
Elbadawi, A. et al. Outcomes of reoperative coronary artery bypass graft surgery in the United States. J. Am. Heart Assoc. 9, e016282 (2020).
Yap, C. H. et al. Contemporary results show repeat coronary artery bypass grafting remains a risk factor for operative mortality. Ann. Thorac. Surg. 87, 1386–1391 (2009).
Brener, S. J. et al. Predictors of revascularization method and long-term outcome of percutaneous coronary intervention or repeat coronary bypass surgery in patients with multivessel coronary disease and previous coronary bypass surgery. Eur. Heart J. 27, 413–418 (2006).
Morrison, D. A. et al. Percutaneous coronary intervention versus repeat bypass surgery for patients with medically refractory myocardial ischemia: AWESOME randomized trial and registry experience with post-CABG patients. J. Am. Coll. Cardiol. 40, 1951–1954 (2002).
Zhou, P. et al. Meta-analysis of repeat revascularization of off-pump and on-pump coronary artery bypass surgery. Ann. Thorac. Surg. 106, 526–531 (2018).
Michael, T. T. et al. A randomized comparison of the transradial and transfemoral approaches for coronary artery bypass graft angiography and intervention: the RADIAL-CABG trial (RADIAL Versus Femoral Access for Coronary Artery Bypass Graft Angiography and Intervention). JACC Cardiovasc. Interv. 6, 1138–1144 (2013).
Israeli, Z. et al. Radial versus femoral approach for saphenous vein grafts angiography and interventions. Am. Heart J. 210, 1–8 (2019).
Januszek, R. et al. Transradial and transfemoral approach in patients with prior coronary artery bypass grafting. J. Clin. Med. 9, 764 (2020).
Manly, D. A. et al. Characteristics and outcomes of patients with history of CABG undergoing cardiac catheterization via the radial versus femoral approach. JACC Cardiovasc. Interv. 14, 907–916 (2021).
Claessen, B. E. P. M., Henriques, J. P. S. & Dangas, G. D. in Interventional Cardiology: Principles & Practice Ch. 19, 2nd edn (eds Dangas, G. D., Di Mario, C. & Kipshidze, N. N.) 201–204 (Wiley, 2017).
Sirker, A. et al. Antiplatelet drug selection in PCI to vein grafts in patients with acute coronary syndrome and adverse clinical outcomes: insights from the British Cardiovascular Intervention Society database. Catheter. Cardiovasc. Interv. 92, 659–665 (2018).
Rha, S. W. et al. Bivalirudin versus heparin as an antithrombotic agent in patients who undergo percutaneous saphenous vein graft intervention with a distal protection device. Am. J. Cardiol. 96, 67–70 (2005).
Kumar, D. et al. Comparison of bivalirudin versus bivalirudin plus glycoprotein IIb/IIIa inhibitor versus heparin plus glycoprotein IIb/IIIa inhibitor in patients with acute coronary syndromes having percutaneous intervention for narrowed saphenous vein aorto-coronary grafts (the ACUITY trial investigators). Am. J. Cardiol. 106, 941–945 (2010).
Roffi, M. et al. Lack of benefit from intravenous platelet glycoprotein IIb/IIIa receptor inhibition as adjunctive treatment for percutaneous interventions of aortocoronary bypass grafts: a pooled analysis of five randomized clinical trials. Circulation 106, 3063–3067 (2002).
Sachdeva, A. et al. Discontinuation of long-term clopidogrel therapy is associated with death and myocardial infarction after saphenous vein graft percutaneous coronary intervention. J. Am. Coll. Cardiol. 60, 2357–2363 (2012).
Connolly, S. J. et al. Rivaroxaban with or without aspirin in patients with stable coronary artery disease: an international, randomised, double-blind, placebo-controlled trial. Lancet 391, 205–218 (2018).
Savage, M. P. et al. Stent placement compared with balloon angioplasty for obstructed coronary bypass grafts. Saphenous Vein De Novo Trial Investigators. N. Engl. J. Med. 337, 740–747 (1997).
Brilakis, E. S. et al. Drug-eluting stents versus bare-metal stents in saphenous vein grafts: a double-blind, randomised trial. Lancet 391, 1997–2007 (2018).
Bhogal, S. et al. Drug-eluting versus bare metal stents in saphenous vein graft intervention: an updated comprehensive meta-analysis of randomized trials. Cardiovasc. Revasc. Med. 20, 758–767 (2019).
Jeger, R. V. et al. Drug-eluting stents compared with bare metal stents improve late outcome after saphenous vein graft but not after large native vessel interventions. Cardiology 112, 49–55 (2009).
Vermeersch, P. et al. Increased late mortality after sirolimus-eluting stents versus bare-metal stents in diseased saphenous vein grafts: results from the randomized DELAYED RRISC trial. J. Am. Coll. Cardiol. 50, 261–267 (2007).
Mehilli, J. et al. Drug-eluting versus bare-metal stents in saphenous vein graft lesions (ISAR-CABG): a randomised controlled superiority trial. Lancet 378, 1071–1078 (2011).
Brilakis, E. S. et al. Continued benefit from paclitaxel-eluting compared with bare-metal stent implantation in saphenous vein graft lesions during long-term follow-up of the SOS (Stenting of Saphenous Vein Grafts) trial. JACC Cardiovasc. Interv. 4, 176–182 (2011).
Colleran, R. et al. Efficacy over time with drug-eluting stents in saphenous vein graft lesions. J. Am. Coll. Cardiol. 71, 1973–1982 (2018).
Shah, R. & Hesterberg, K. Drug-eluting stents versus bare-metal stents for saphenous vein graft interventions. J. Thorac. Dis. 11, S1257 (2019).
IJsselmuiden, A. et al. Comparison between the STENTYS self-apposing bare metal and paclitaxel-eluting coronary stents for the treatment of saphenous vein grafts (ADEPT trial). Neth. Heart J. 26, 94–101 (2018).
Yazdani, S. K. et al. Pathology of drug-eluting versus bare-metal stents in saphenous vein bypass graft lesions. JACC Cardiovasc. Interv. 5, 666–674 (2012).
Stone, G. W. et al. 5-year follow-up of polytetrafluoroethylene-covered stents compared with bare-metal stents in aortocoronary saphenous vein grafts the randomized BARRICADE (barrier approach to restenosis: restrict intima to curtail adverse events) trial. JACC Cardiovasc. Interv. 4, 300–309 (2011).
Vaknin-Assa, H. et al. Long term outcomes of MGuard stent deployment in saphenous vein grafts and native coronary arteries: a single center experience. Isr. Med. Assoc. J. 19, 172–176 (2017).
Latif, F. et al. Stent-only versus adjunctive balloon angioplasty approach for saphenous vein graft percutaneous coronary intervention: insights from DIVA trial. Circ. Cardiovasc. Interv. 13, e008494 (2020).
Iakovou, I. et al. Relation of final lumen dimensions in saphenous vein grafts after stent implantation to outcome. Am. J. Cardiol. 93, 963–968 (2004).
Hong, Y. J. et al. Outcome of undersized drug-eluting stents for percutaneous coronary intervention of saphenous vein graft lesions. Am. J. Cardiol. 105, 179–185 (2010).
Gruberg, L. et al. In-hospital and long-term results of stent deployment compared with balloon angioplasty for treatment of narrowing at the saphenous vein graft distal anastomosis site. Am. J. Cardiol. 84, 1381–1384 (1999).
Michaels, A. D. et al. Pretreatment with intragraft verapamil prior to percutaneous coronary intervention of saphenous vein graft lesions: results of the randomized, controlled vasodilator prevention on no-reflow (VAPOR) trial. J. Invasive Cardiol. 14, 299–302 (2002).
Zoghbi, G. J. et al. Pretreatment with nitroprusside for microcirculatory protection in saphenous vein graft interventions. J. Invasive Cardiol. 21, 34–39 (2009).
Kapoor, N., Yalamanchili, V., Siddiqui, T., Raza, S. & Leesar, M. A. Cardioprotective effect of high-dose intragraft adenosine infusion on microvascular function and prevention of no-reflow during saphenous vein grafts intervention. Catheter. Cardiovasc. Interv. 83, 1045–1054 (2014).
Huang, R. I. et al. Efficacy of intracoronary nicardipine in the treatment of no-reflow during percutaneous coronary intervention. Catheter. Cardiovasc. Interv. 68, 671–676 (2006).
Al-Qezweny, M. N. A. et al. in Coronary Graft Failure: State of the Art (eds Ţintoiu, I. C., Underwood, M. J., Cook, S.P., Kitabata, H. & Abbas, A.) 539–554 (Springer, 2016).
Acknowledgements
M.F.L.G. has received institutional grant/research support from the NIH and the Canadian Institutes of Health Research.
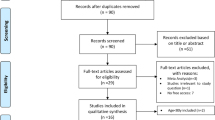
Review criteria
A search was performed for original articles published between 1980 and 2021 focusing on contemporary practices in both coronary artery bypass graft surgery as well as follow-up percutaneous coronary interventions in patients who have previously undergone coronary artery bypass graft surgery. The search terms used were ‘prior coronary artery bypass graft’, ‘saphenous vein graft’, ‘radial artery graft’, ‘bilateral internal thoracic artery’, ‘right internal thoracic artery’, ‘multiple artery grafting’, ‘total arterial revascularization’, ‘venous graft failure’, ‘arterial graft failure’, ‘perioperative graft failure’, ‘prior CABG revascularization’, ‘prior CABG medical treatment’, ‘saphenous vein graft PCI’, ‘native vessel PCI prior CABG’, ‘arterial graft PCI’, ‘repeat CABG surgery’, ‘radial PCI prior CABG’, ‘femoral PCI prior CABG’, ‘stent selection prior CABG’ and ‘EPD graft PCI’, alone and in combination. All articles identified were English-language, full-text papers. The reference lists of identified articles were also searched for further relevant papers.
Author information
Authors and Affiliations
Contributions
All the authors researched data for the article, contributed to discussions of its content, wrote the article, and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
R.M. and G.D.D. have received institutional grant/research support from Abbott Laboratories, AstraZeneca, Boston Scientific, Daiichi-Sankyo and Medtronic; have served as consultants for Biosensors; and have received speaker honoraria from Chiesi. The other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Cardiology thanks Y. Jang and C. Juergens for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Beerkens, F.J., Claessen, B.E., Mahan, M. et al. Contemporary coronary artery bypass graft surgery and subsequent percutaneous revascularization. Nat Rev Cardiol 19, 195–208 (2022). https://doi.org/10.1038/s41569-021-00612-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41569-021-00612-6
This article is cited by
-
Exploring the therapeutic potential of Sirt6-enriched adipose stem cell-derived exosomes in myocardial ischemia–reperfusion injury: unfolding new epigenetic frontiers
Clinical Epigenetics (2024)
-
Prevention of neointimal hyperplasia after coronary artery bypass graft via local delivery of sirolimus and rosuvastatin: network pharmacology and in vivo validation
Journal of Translational Medicine (2024)
-
Strategies for arterial graft optimization at the single-cell level
Nature Cardiovascular Research (2024)
-
Multi-slice CT coronary angiography versus invasive coronary angiography in the assessment of graft patency after coronary artery bypasses graft surgery
The Egyptian Heart Journal (2023)
-
Alterations in gut microbiota and host transcriptome of patients with coronary artery disease
BMC Microbiology (2023)