Abstract
A diagnosis of idiopathic inflammatory bowel disease requires synthesis of clinical, radiographic, endoscopic, surgical, and histologic data. While most cases of inflammatory bowel disease can be specifically classified as either ulcerative colitis or Crohns disease, 5–10% of patients have equivocal features placing them into the indeterminate colitis category. This study examines whether microRNA biomarkers assist in the classification of classically diagnosed indeterminate inflammatory bowel disease. Fresh frozen colonic mucosa from the distal-most part of the colectomy from 53 patients was used (16 indeterminate colitis, 14 Crohns disease, 12 ulcerative colitis, and 11 diverticular disease controls). Total RNA extraction and quantitative reverse-transcription-PCR was performed using five pairs of microRNA primers (miR-19b, miR-23b, miR-106a, miR-191, and miR-629). Analysis of variance was performed assessing differences among the groups. A significant difference in expressions of miR-19b, miR-106a, and miR-629 was detected between ulcerative colitis and Crohns disease groups (P<0.05). The average expression level of all five microRNAs was statistically different between indeterminate colitis and Crohns disease groups (P<0.05); no significant difference was present between indeterminate and ulcerative colitis groups. Among the 16 indeterminate colitis patients, 15 showed ulcerative colitis-like and one Crohns disease-like microRNA pattern. MicroRNA expression patterns in indeterminate colitis are far more similar to those of ulcerative colitis than Crohns disease. MicroRNA expression patterns of indeterminate colitis provide molecular evidence indicating that most cases are probably ulcerative colitis—similar to the data from long-term clinical follow-up studies. Validation of microRNA results by additional long-term outcome data is needed, but the data presented show promise for improved classification of indeterminate inflammatory bowel disease.
Similar content being viewed by others
Main
Knowledge of indeterminate colitis continues to evolve as the concept was first introduced by Dr Ashley Price in 1978.1 While most of inflammatory bowel disease cases are further classified into either ulcerative colitis or Crohns disease, 5–10% of inflammatory bowel disease patients bear equivocal features, falling into the category of indeterminate colitis.2, 3, 4
According to the World Congress of Gastroenterology Montreal Recommendations,5 the diagnosis of indeterminate inflammatory bowel disease should be made only after colectomy, in cases where definitive features of Crohns disease and ulcerative colitis are absent. Although the nature of disease of most indeterminate inflammatory bowel disease patients becomes evident over time, a portion of patients remain indeterminate. As Crohns disease is an important contradiction for ileal pouch-anal anastomosis for continence restoration after colectomy, more precise classification of indeterminate inflammatory bowel disease is a highly sought after clinical goal.
Some serological markers, such as anti-Saccharomyces cerevisiae and perinuclear antineutrophil cytoplasmic antibodies, have been applied to attempt improved classification of indeterminate inflammatory bowel disease.6 However, these markers have low specificity and sensitivity as born out by long-term clinical outcomes. Better markers are greatly needed.
MicroRNAs, are small noncoding RNAs, that have an important role in cellular processes of differentiation and apoptosis.7 Furthermore, microRNAs have been shown to regulate chronic inflammation in autoimmune disease.8, 9 microRNAs were reported to be differentially expressed in colonic mucosal tissue of Crohns disease patients in a microRNA microarray study, compared with the normal noninflammatory bowel disease controls or ulcerative colitis patients.10, 11 This study now examines the role of five differentially expressed microRNA between ulcerative colitis and Crohns disease for distinguishing classically diagnosed indeterminate inflammatory bowel disease.
Materials and methods
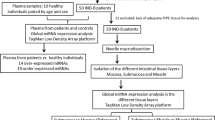
Human Colonic Tissues
Fresh frozen colonic mucosa was sampled from colectomies of the following patient groups: 16 indeterminate inflammatory bowel disease, 14 Crohns disease, 12 ulcerative colitis, and a normal control group of 11 patients with diverticular disease. Institutional review board approval was strictly maintained. The biopsy samples were obtained from the distal-most involved part of the colectomy specimens, snap frozen in liquid nitrogen, and held at −80°C. Frozen sections were performed to confirm the nondysplastic histology and to evaluate the degree of the inflammation in each sample. Patients had a medical diagnosis of ulcerative colitis, Crohns disease, indeterminate inflammatory bowel disease, or diverticular disease and the pathologic colectomy diagnosis was confirmed in each. The slides were reviewed by two gastrointestinal pathologists (JL and MPB).
The demographic features were summarized in Table 1. The mean time from initial presentation of inflammatory bowel disease to colectomy in indeterminate inflammatory bowel disease group was 9 years 3 months, ranging from 3 months to 27 years. The mean postcolectomy follow-up time of indeterminate inflammatory bowel disease patients was 4 years 5 months, with a range from 1 year 1 month to 7 years 9 months. Seven indeterminate colitis patients had pouch constructed with a follow-up period ranging from 21 months to 93 months (Table 3). Most of them had no pouch complications during follow-up, except one patient whose pouch ultimately failed and was resected 1 year and 9 months later due to recurrent inflammatory bowel disease (patient 13).
Diagnostic Criteria for Ulcerative Colitis, Crohns Disease, and Indeterminate Inflammatory Bowel Disease
Briefly, the cardinal pathologic features of ulcerative colitis are those of a chronic colitis with superficial disease that is usually diffuse but occasionally patchy. Ulcerative colitis may develop fulminant deep ulcers but it lacks the transmural discrete lymphoid aggregates remote from ulcers and noncrypt rupture granulomas typical of Crohns disease. Ileal involvement as backwash ileitis in direct continuity with pancolonic ulcerative colitis was also permitted for the diagnosis of ulcerative colitis, as validated by long-term pouch outcome studies,12 but it lacked the diagnostic mural features of Crohns disease (discrete lymphoid aggregates remote from ulcers and/or strictures, adhesions or fistula). The diagnosis of Crohns disease required chronic colitis with transmural discrete lymphoid aggregates remote from ulcers, with or without noncrypt rupture granulomas, strictures, adhesions, or fistula. Diverted rectal specimens were not used to differentiate ulcerative colitis and Crohns disease, due to their well reported tendency to nonspecifically mimic the transmural features of Crohns disease.13, 14, 15, 16 Indeterminate inflammatory bowel disease was diagnosed in cases with overlapping or poorly formed features of ulcerative colitis and Crohns disease. This typically entailed some diffuse superficial chronic active colitis but with focal poorly developed transmural lymphoid aggregates away from ulcers, or with nonmucin granulomas, or poorly formed strictures. Fulminant inflammatory bowel disease with diffuse colonic ulceration making it impossible to assess for transmural discrete lymphoid aggregates remote from ulcers or impossible to assess the significance of fistula, was other findings considered indeterminate. The demographic and pathologic features of the study and control groups are summarized in Table 1. Among sixteen selected indeterminate colitis patients, seven were initially thought having indeterminate inflammatory bowel disease clinically. Five of them were thought to have ulcerative colitis, and four of them were thought to have Crohns disease clinically. The involvement of the pathologic features in the sixteen selected indeterminate colitis patients, including diffuse or segmental chronic colitis, ileitis, transmural lymphoid aggregates remote from ulcers, strictures, fistula and granulomas, do fall between the groups of ulcerative colitis and Crohns disease. This demonstrates that the selected cases in our study do fit the definition of indeterminate inflammatory bowel disease.
Total Small RNA Extraction
The frozen tissues were dissolved in 700 μl of Qiazol reagent (Qiagen, USA) and total small RNA was extracted using miRNeasy mini isolation kit (Qiagen, USA) according to the manufacturers’ instructions. The RNA samples were stored at −80°C.
Quantitative Reverse-Transcription-PCR
The microRNA enrichment from the study and control groups was performed using TaqMan® microRNA Reverse Transcription Kit (Applied Biosystems by Life Technologies, USA) and TaqMan® Universal PCR Master Mix system (Applied Biosystems by Life Technologies, USA). Briefly, 50 ng of small RNA was converted to complementary DNA. Commercially available microRNA primers were used (Applied Biosystems by Life Technologies, USA). The expression of each microRNA in the sampled colonic mucosa was calculated as a value relative to U6B, a ubiquitously expressed small nuclear RNA that has been widely accepted as a stably expressed internal control. The levels of each target microRNA in the study groups were normalized to the mean value of the control group. Each sample was performed in duplicate.
Statistical Analysis
Experimental results were expressed as mean values. Univariate analysis of variance was performed to investigate differences in microRNA expression between the study and control groups. The SAS Proc General Linear Model was used to fit analysis of variance models because the sample sizes of the groups compared were different (ie, unbalanced data). If there was an overall statistically significant difference, post hoc pairwise comparisons would be performed to test which specific pairs were significant. A P value of <0.05 was considered significant. Discriminant analysis was conducted to evaluate the capacity of five markers, as a whole, to differentiate and classify the diseases of interest. All analyses were performed with SAS (version 9.2, SAS Institute Inc., Cary, NC, USA).
Results
MicroRNAs Differentially Expressed in Colonic Tissue Between Ulcerative Colitis and Crohns Disease Patients
In this study, we first confirmed the expression pattern of five microRNAs, miR-19b, miR-23b, miR-106a, miR-191, and miR-629, in the colonic mucosal tissue from patients with ulcerative colitis, Crohns disease and the control group. The expression of each microRNA was normalized to its internal control, U6B, and then each value in the study groups was standardized to the mean value of the control group (Table 2). Analysis of variance showed significant difference in expression of miR-19b, miR-23b, miR-106a, and miR-629 between the Crohns disease group and control group (P<0.05, data not shown). No differences were observed between the ulcerative colitis and control groups in all five microRNAs (P>0.05, data not shown), which is consistent with the finding in the previous study.11 Finally, three microRNAs, miR-19b, miR-106a, and miR-629, were statistically differentially expressed in colonic tissue between ulcerative colitis and Crohns disease groups, respectively (P<0.05).
Five MicroRNAs Differentially Expressed in Colonic Tissue Between Indeterminate Inflammatory Bowel Disease and Crohns Disease Patients, but not Between Indeterminate Inflammatory Bowel Disease and Ulcerative Colitis Patients
The differential expression of the five tested microRNAs between ulcerative colitis and Crohns disease groups makes them suitable markers to characterize the features of indeterminate inflammatory bowel disease. As shown in Table 2, the expression of all five microRNAs was significantly different between indeterminate inflammatory bowel disease and Crohns disease groups (P<0.05), respectively. Interestingly, there was no difference between indeterminate inflammatory bowel disease and ulcerative colitis groups in any of these microRNAs (P>0.05, data not shown). Thus, the expression level of the five selected microRNAs in indeterminate inflammatory bowel disease, as a whole, is similar to that of ulcerative colitis, not Crohns disease.
Discriminant Analysis of Five MicroRNAs to Distinguish Crohns Disease-Like Pattern From Ulcerative Colitis-Like Expression Pattern
Discriminant analysis was performed to study whether, as a whole, the five microRNA markers had a good capacity in distinguishing diseases of interest. Nine of 14 Crohns disease patients had Crohns disease-like microRNA expression pattern; the prediction accuracy was 64.3%. All ulcerative colitis patients had ulcerative colitis-like microRNA expression pattern with 100% prediction accuracy.
Five Panel MicroRNA Expression Pattern in Indeterminate Inflammatory Bowel Disease
Among the 16 indeterminate inflammatory bowel disease patients, fifteen showed ulcerative colitis-like and one Crohns disease-like microRNA expression pattern (patient 10 in Table 3 without pouch construction.
The Degree of Inflammation of the Frozen Tissue
The involvement of inflammation of each frozen sample was evaluated based on the degree of inflammation and was classified into no inflammation, cryptitis, crypt abscess, numerous crypt abscesses (>3/high-power field) and ulceration. As shown in Table 4, most of the controls showed no active inflammation; however, most of the specimens of the study groups, including Crohns disease, ulcerative colitis and indeterminate colitis demonstrated variable degrees of inflammation, ranging from cryptitis, crypt abscess, to ulceration. The expression levels of five miRNAs were not associated with the degree of inflammation in the current study (data not shown).
Discussion
Idiopathic inflammatory bowel disease of indeterminate type represents a heterogenous group of patients that bear equivocal features of both ulcerative colitis and Crohns disease. These patients manifest a spectrum of disease with classical ulcerative colitis and classical Crohns disease at either end. Knowledge of indeterminate inflammatory bowel disease patients accumulates from clinical observation and long-term follow-up that can delay or even prevent definitive pouch surgery to restore continence. Thus, the most pertinent question regarding the surgical decisions in indeterminate inflammatory bowel disease patients is whether to provide an ileal pouch-anal anastomosis for continence restoration. Ileal pouch-anal anastomosis is most clearly indicated for ulcerative colitis patients, but remains contraindicated in most if not all Crohns disease patients, as pouch complication rates are markedly elevated and typically severe in known Crohns disease.17, 18, 19 Based on long-term clinical outcome studies, it appears that most indeterminate inflammatory bowel disease patients will ultimately behave clinically like ulcerative colitis patients.20, 21 Accordingly, indeterminate inflammatory bowel disease patients are often deemed appropriate candidates for ileal pouch-anal anastomosis, although they have an increased complication rate compared with ulcerative colitis.17, 22 Ultimately, the best means of selecting ileal pouch-anal anastomosis candidates within the indeterminate inflammatory bowel disease population remains an important clinical question. To further advance this clinical need, a simple strategy by sorting microRNA expression patterns of indeterminate inflammatory bowel disease into Crohns disease-like versus ulcerative colitis-like would be practical. Based on this rationale, we applied discriminant analysis of microRNA expression of a panel of five markers in each indeterminate inflammatory bowel disease patient studied.
The underlying molecular mechanism governing the diagnoses of ulcerative colitis, Crohns disease and indeterminate inflammatory bowel disease remain a mystery. In this paper, we explored the expression pattern of microRNAs in indeterminate inflammatory bowel disease in comparison to the other two major groups of inflammatory bowel disease, namely ulcerative colitis and Crohns disease. Our data provide molecular evidence, for the first time to our knowledge, that microRNA expression patterns in indeterminate inflammatory bowel disease, as a whole, are similar to those of ulcerative colitis and not Crohns disease. Clinically, most indeterminate inflammatory bowel disease patients behave similarly to those of ulcerative colitis patients in long-term follow-up, which is supported by the parallel microRNA background in both, as demonstrated in this paper. The advantage of microRNA analysis is its immediate determination at the time of colectomy without the need for long-term clinical outcome validation of ulcerative colitis-like biology.
A two-tier system of classifying indeterminate inflammatory bowel disease into Crohns disease-like versus ulcerative colitis-like microRNA expression pattern using discriminant analysis, although simple, could be of practical value from the clinical point of view. In this study, most of the indeterminate inflammatory bowel disease patients had no pouch complications during follow-up, except one patient whose pouch ultimately failed because of the severe pouchitis and was resected 1 year and 9 months postcolectomy (patient 13). Of course, Crohns disease is only one of many reasons that pouches fail. Owing to the small size of the current study, further validation of microRNA expression patterns in large series with the long-term pouch and overall clinical outcomes will be essential. Ideally, we want to establish a discriminant analysis model to distinguish each individual indeterminate inflammatory bowel disease patients by combining both clinicopathologic and microRNA data to aid treatment decisions as whether they should or should not receive pouch surgery. The added molecular evidence could therefore provide further assurance that indeterminate inflammatory bowel disease patients have been correctly selected for pouch restorative surgery.
All five selected miRNAs show differential expression pattern between the Crohns disease and the ulcerative colitis groups, which makes them useful markers to distinguish the two major subclass of inflammatory bowel disease. No differences were observed between the ulcerative colitis and control groups in all five microRNAs, which is consistent with the finding in the previous study.11 All five markers are upregulated in Crohns disease group in the current study; however, two of them, miR-19b and miR-629, showed decreased expression in Wu’s study.11 These two miRNAs demonstrate good differential expression with solid controls in our study; however, we don’t know how to explain the difference compared with the prior study. May be it is confounded by the different sample cohorts, the different location of the colon from where the frozen tissue was sampled, or the different degree of inflammation of the frozen tissue. As shown in our study, there is no association between the expression levels of miRNAs and the degree of inflammation.
Among the five selected microRNAs studied, aberrant expression of miR-106a is known to be associated with a variety of diseases, including inflammatory diseases in the other organ system and colon cancer.23, 24, 25, 26 miR-106a posttranscriptionally regulates the expression of interleukine-10 (IL-10), which is a key modulator of the immune system. On the other hand, miR-106a expression is regulated by tumor necrosis factor alpha and lipopolysaccharide.24 The role of miR-106a seems to be involved in finely tuning the critical expression of IL-10 in response to particular external stimuli. Thus, miR-106a and its regulators comprise a complex regulatory network. The overexpression of microRNAs, including miR-106a, and their subsequent downstream target protein expression in Crohns disease, not in ulcerative colitis and most indeterminate inflammatory bowel disease, may be associated with the particular clinical presentation of Crohns disease and its related clinical outcome. As such, microRNAs are potential molecular markers to classify the subtype of inflammatory bowel disease, especially at an early stage when the disease has not clarified itself.
In summary, microRNA expression patterns for the five-marker panel used in this study provide molecular evidence that most indeterminate inflammatory bowel disease cases are probably ulcerative colitis. This parallels the established clinical findings, but has the considerable advantage of being testable at the time of colectomy for improved pouch surgery selection. Our study did find one indeterminate patient with a Crohns disease-like microRNA expression pattern, and the utility of this type of analysis will be to better define such patients for pouch selection. Long-term clinical validation remains a necessity, but these microRNA results are promising for improving the classification of indeterminate inflammatory bowel disease. MicroRNA may be a potential diagnostic and prognostic marker to better delineate indeterminate inflammatory bowel disease patients, and prevent possible Crohns-related pouch complications.
References
Price AB . Overlap in the spectrum of non-specific inflammatory bowel disease--'colitis indeterminate'. J Clin Pathol 1978;31:567–577.
Hildebrand H, Fredrikzon B, Holmquist L et al Chronic inflammatory bowel disease in children and adolescents in Sweden. J Pediatr Gastroenterol Nutr 1991;13:293–297.
Moum B, Vatn MH, Ekbom A et al Incidence of ulcerative colitis and indeterminate colitis in four counties of southeastern Norway, 1990-93. A prospective population-based study. The Inflammatory Bowel South-Eastern Norway (IBSEN) Study Group of Gastroenterologists. Scand J Gastroenterol 1996;31:362–366.
Meucci G, Bortoli A, Riccioli FA et al Frequency and clinical evolution of indeterminate colitis: a retrospective multi-centre study in northern Italy. GSMII (Gruppo di Studio per le Malattie Infiammatorie Intestinali). Eur J Gastroenterol Hepatol 1999;11:909–913.
Silverberg MS, Satsangi J, Ahmad T et al Toward an integrated clinical, molecular and serological classification of inflammatory bowel disease: Report of a Working Party of the 2005 Montreal World Congress of Gastroenterology. Can J Gastroenterol 2005;19 (Suppl A):5–36.
Joossens S, Reinisch W, Vermeire S et al The value of serologic markers in indeterminate colitis: a prospective follow-up study. Gastroenterology 2002;122:1242–1247.
Ambros V . The functions of animal microRNAs. Nature 2004;431:350–355.
Xiao C, Rajewsky K . MicroRNA control in the immune system: basic principles. Cell 2009;136:26–36.
Pauley KM, Cha S, Chan EK . MicroRNA in autoimmunity and autoimmune diseases. J Autoimmun 2009;32:189–194.
Wu F, Zikusoka M, Trindade A et al MicroRNAs are differentially expressed in ulcerative colitis and alter expression of macrophage inflammatory peptide-2 alpha. Gastroenterology 2008;135:e24.
Wu F, Zhang S, Dassopoulos T et al Identification of microRNAs associated with ileal and colonic Crohn's disease. Inflamm Bowel Dis 2010;16:1729–1738.
Arrossi AV, Kariv Y, Bronner MP et al Backwash ileitis does not affect pouch outcome in patients with ulcerative colitis with restorative proctocolectomy. Clin Gastroenterol Hepatol 2011;9:981–988.
Warren BF, Shepherd NA, Bartolo DC et al Pathology of the defunctioned rectum in ulcerative colitis. Gut 1993;34:514–516.
Feakins RM . Diversion proctocolitis with granulomatous vasculitis in a patient without inflammatory bowel disease. Histopathology 2000;36:88–89.
Ma CK, Gottlieb C, Haas PA . Diversion colitis: a clinicopathologic study of 21 cases. Hum Pathol 1990;21:429–436.
Asplund S, Gramlich T, Fazio V et al Histologic changes in defunctioned rectums in patients with inflammatory bowel disease: a clinicopathologic study of 82 patients with long-term follow-up. Dis Colon Rectum 2002;45:1206–1213.
Brown CJ, Maclean AR, Cohen Z et al Crohn's disease and indeterminate colitis and the ileal pouch-anal anastomosis: outcomes and patterns of failure. Dis Colon Rectum 2005;48:1542–1549.
Braveman JM, Schoetz DJ, Marcello PW et al The fate of the ileal pouch in patients developing Crohn’s disease. Dis Colon Rectum 2004;47:1613–1619.
Tekkis PP, Heriot AG, Smith O et al Long-term outcomes of restorative proctocolectomy for Crohn's disease and indeterminate colitis. Colorectal Dis 2005;7:218–223.
Murrell ZA, Melmed GY, Ippoliti A et al A prospective evaluation of the long-term outcome of ileal pouch-anal anastomosis in patients with inflammatory bowel disease-unclassified and indeterminate colitis. Dis Colon Rectum 2009;52:872–878.
Pishori T, Dinnewitzer A, Zmora O et al Outcome of patients with indeterminate colitis undergoing a double-stapled ileal pouch-anal anastomosis. Dis Colon Rectum 2004;47:717–721.
McIntyre PB, Pemberton JH, Wolff BG et al Indeterminate colitis. Long-term outcome in patients after ileal pouch-anal anastomosis. Dis Colon Rectum 1995;38:51–54.
Sharma A, Kumar M, Aich J et al Posttranscriptional regulation of interleukin-10 expression by hsa-miR-106a. Proc Natl Acad Sci USA 2009;106:5761–5766.
Jiang X, Li N . Induction of MiR-17-3p and MiR-106a [corrected] by TNFalpha and LPS. Cell Biochem Funct 2011;29:164–170.
Diaz R, Silva J, Garcia JM et al Deregulated expression of miR-106a predicts survival in human colon cancer patients. Genes Chromosomes Cancer 2008;47:794–802.
Ma Y, Zhang P, Yang J et al Candidate microRNA biomarkers in human colorectal cancer: Systematic review profiling studies and experimental validation. Int J Cancer 2011, (e-pub ahead of print).
Acknowledgements
We would like to thank Bonnie Shadrach and Jennifer Lewis for their help in procuring the frozen tissue and Tracey Bender for her assistance in the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflicts of interest.
Rights and permissions
About this article
Cite this article
Lin, J., Cao, Q., Zhang, J. et al. MicroRNA expression patterns in indeterminate inflammatory bowel disease. Mod Pathol 26, 148–154 (2013). https://doi.org/10.1038/modpathol.2012.131
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.2012.131
Keywords
This article is cited by
-
Serum miRNA signature diagnoses and discriminates murine colitis subtypes and predicts ulcerative colitis in humans
Scientific Reports (2017)
-
MicroRNA signatures differentiate Crohn’s disease from ulcerative colitis
BMC Immunology (2015)
-
Novel specific microRNA biomarkers in idiopathic inflammatory bowel disease unrelated to disease activity
Modern Pathology (2014)