Abstract
Although many studies have suggested that estrogen prevents postmenopausal bone loss partially due to its anti-apoptosis effects in osteoblasts, the underlying mechanism has not been fully elucidated. In the present study, we found that 17β-estradiol (17β-E2), one of the primary estrogens, inhibited endoplasmic reticulum (ER) stress-induced apoptosis in MC3T3-E1 cells and primary osteoblasts. Interestingly, 17β-E2-promoted Grp78 induction, but not CHOP induction in response to ER stress. We further confirmed that Grp78-specific siRNA reversed the inhibition of 17β-E2 on ER stress-induced apoptosis by activating caspase-12 and caspase-3. Moreover, we found that 17β-E2 markedly increased the phosphorylated TFII-I levels and nuclear localization of TFII-I in ER stress conditions. 17β-E2 stimulated Grp78 promoter activity in a dose-dependent manner in the presence of TFII-I and enhanced the binding of TFII-I to the Grp78 promoter. In addition, 17β-E2 notably increased phosphorylated ERK1/2 levels and Ras kinase activity in MC3T3-E1 cells. The ERK1/2 activity-specific inhibitor U0126 remarkably blocked 17β-E2-induced TFII-I phosphorylation and Grp78 expression in response to ER stress. Together, 17β-E2 protected MC3T3-E1 cells against ER stress-induced apoptosis by promoting Ras-ERK1/2-TFII-I signaling pathway-dependent Grp78 induction.
Similar content being viewed by others
Main
Osteoporosis is a skeletal disease characterized by reduced bone mass, reduced bone strength, deterioration in the microarchitecture of bone tissue and an increased risk of fracture. An imbalance between bone formation and bone resorption is the predominant mechanism resulting in osteoporosis.1, 2, 3 As new bone formation is primarily dependent on osteoblasts, factors that act by increasing apoptosis of osteoblasts can induce osteoporosis.4, 5 Many diseases are associated with an increase in apoptosis, but to date, the active involvement of apoptosis during osteoporosis pathogenesis is inconclusive.
Endoplasmic reticulum (ER) stress has received growing attention because it is considered a cause of various diseases through ER stress-induced apoptosis.6, 7 The ER is a central cellular organelle engaged in protein synthesis, folding, and maturation in eukaryotic cells. Various physiopathological conditions, including hypoxia, protein misfolding, nutritional deprivation, viral infection, Ca2+ overload, and oxidative injury may affect ER function and result in ER stress. Excessive or prolonged ER stress may result in apoptosis via mitochondria-dependent or mitochondria-independent mechanisms.8, 9, 10 To avoid ER stress-induced apoptosis, eukaryotic cells suppress protein translation and refold the unfolded proteins by the induction of ER molecular chaperones.11 Glucose-regulated protein 78 (Grp78) is one of the most important ER molecular chaperones. It is induced in response to ER stress and serves to refolding of misfolded or incompletely assembled proteins.12, 13 Grp78 is known to inhibit caspase-mediated cell death by forming complexes with procaspases-7 and procaspases-12. The expression of Grp78 protects against various types of cell death induced by ER stress. If induction of Grp78 fails, cells go into ER stress-induced apoptosis.14, 15, 16 Interestingly, ER stress is tightly regulated, particularly for professional secretory cells such as collagen-secreting osteoblasts, which have a well-developed ER to synthesize large amounts of bone matrix proteins. Recent reports have shown that several osteogenic cytokines, such as bone morphogenetic protein-2 (BMP-2) could induce osteoblasts ER stress during osteogenic differentiation.17, 18 Some ER stress-associated proteins have a significant role in bone formation. For example, old astrocyte specifically induced substance (OASIS), an ER stress transducer, has been implicated to be involved in bone formation through the transcription of COL1A1 and the secretion of bone matrix proteins.19 Moreover, the ER stress-specific transcription factor XBP1 could directly bind to the Runx2 promoter and promote expression of Runx2, which is also an essential transcription factor in bone formation.20 In addition, ATF4, another fundamental transcription factor of ER stress promotes bone formation by favoring collagen synthesis and amino-acid import in osteoblasts.21 However, it has also reported that ER molecular chaperones, such as Grp78 and PDI (protein disulfide isomerase), are downregulated in osteoblasts from osteoporosis patients.22 ER stress-associated osteoblast apoptosis is one of the most predominant pathogenesis of osteoporosis.23, 24, 25, 26 Thus, an intriguing question in osteoblasts is an outcome of survival in ER stress. The balance between cell death responses and cell survival responses may decide the occurrence and development of osteoporosis. In stressed but surviving osteoblasts, little is known about the molecular mechanism that osteoblasts were protected from ER stress-induced apoptosis. Therefore, a better understanding of ER stress-induced apoptosis in osteoblasts can assist the development of new prophylaxis and therapies for osteoporosis.
Estrogen deficiency is a major contributor to osteoporosis, which gives rise to increased risk of bone mass loss after menopause. Many studies have shown that apoptosis of osteoblasts is increased in postmenopausal osteoporosis, which leads to inevitable bone mass reduction.27, 28 It has been reported that 17β-estradiol (17β-E2), one of the primary estrogens, increases cell survival and the viability of various cells, including osteoblasts. Recent studies have identified that 17β-E2 activates several survival signaling pathways via estrogen receptors. 17β-E2 could prevent cells against oxidative stress-induced apoptosis through activating the MAPK pathway.29, 30, 31 In addition, the subsequent researchers found that the anti-apoptotic effect of 17β-E2 is dependent on estrogen receptors-mediated upregulation of the expression of anti-apoptotic proteins Bcl-2 and Bcl-xL.32, 33, 34 Although, the role of 17β-E2 in the maintenance of cell survival is widely recognized, whether 17β-E2 is involved in ER stress-induced apoptosis during osteoporosis pathogenesis is still inconclusive. In this study, we found that by promoting TFII-I activity through Ras-ERK1/2 pathway, 17β-E2 enhances induction of Grp78 and then inhibits activation of caspase-12 and caspase-3, thus reducing cell apoptosis of MC3T3-E1 cells in response to ER stress.
MATERIALS AND METHODS
Cell Culture
The mouse calvaria osteoblasts MC3T3-E1 were purchased from American Type Culture Collection (ATCC) and cultured in α-minimum essential medium (α-MEM) (Gibco, Grand Island, USA) supplemented with 10% fetal bovine serum (FBS) and antibiotics (100 U/ml of penicillin G and 100 μg/ml of streptomycin) at 37 °C in a humidified atmosphere of 5% CO2. Primary osteoblasts were isolated from calvaria of newborn mice (purchased from the Laboratory Animal Center of the Fourth Military Medical University). Calvaria were gently digested at 37 °C for 10 min four times with 0.1% collagenase and 0.25% trypsin, and the last two fractionated cells were collected. Cells were cultured in α-MEM supplemented with 10% FBS, 100 U/ml penicillin, and 100 mg/l streptomycin and kept at 37 °C in a humidified atmosphere of 5% CO2. Culture medium was replaced every 3 days thereafter. The experimental procedures in this study were approved the Ethics Committee for Animal Experimentation of the Fourth Military Medical University, P.R. China.
Western Blot Analysis
Cells were lysed in 1% OG buffer (20 mM Tris–HCl, pH 8.0, 150 mM NaCl, 1% OG, 1 mM EDTA, 10 μg/ml leupeptin, 2 μg/ml aprotinin and 1 mM PMSF). A BCA Protein Assay Kit (Pierce Biotechnology, Rockford, Illinois) was then used to determine the total protein density, and equal amounts of protein were separated by 10% SDS–PAGE and transferred to a polyvinylidene fluoride (PVDF) microporous membrane (Millipore Billerica, MA). After being blocked with 5% non-fat milk, the membrane was incubated for 2 h at room temperature with the designated antibody. A Western-Light Chemiluminescent Detection System (Applied Biosystems, Foster, CA) was used for immunodetection.
Reverse Transcriptase Polymerase Chain Reaction
Total RNA was extracted from the cells with TRIzol reagents (Invitrogen) and reversely transcribed into cDNA with the ReverTra Ace qPCR RT Kit (Toyobo). The primers were synthesized by Shanghai Sangon as follows: Grp78, forward primer 5′-CACAGACGGGTCATTCC-3′, reverse primer 5′-CCTATGTCGCCTTCACT-3′; CHOP, forward primer 5′-GACGCTTCACTACTCTTGACCCTGCG-3′, reverse primer 5′-GGATGTGCGTGTGACCTCTGT-3′; GAPDH, forward primer 5′-AATGTCACCGTTGTCCAGTTGC-3′, reverse primer 5′-CACCATCTT AGGAGGAGGAGTAGC-3′. GAPDH mRNA was used as an internal control. The PCR conditions were 1 cycle of 94 °C for 5 min; 35 cycles of 94 °C for 60 s, 57 °C for 40 s, and 72 °C for 40 s; and finally 72 °C for 5 min. PCR products were electrophoresed on 1% agarose gels.
MTT Assay
Cell viability was determined by 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay. After treatment with Tg for 24 h, cultures were washed with PBS. MTT (0.5 mg/ml) was then added to each well and the mixture was incubated for 4 h at 37 °C. Culture medium was then replaced with an equal volume of DMSO to dissolve formazan crystals. After the mixture was shaken at room temperature for 30 min, absorbance of each well was determined at 550 nm.
TUNEL Assay
Apoptosis in osteoblasts and mice tibias sections were detected using the DeadEnd Fluorometric TUNEL System (Promega, WI, USA), which end-labels the DNA from the fragmented apoptotic cells using a modified TUNEL staining according to the manufacturer’s instructions. Briefly, samples were fixed with 4% methanol-free formaldehyde solution, rinsed with PBS twice, then end-labeled the fragmented DNA of the apoptotic cells using the fluorescein-12-dUTP and covered slides in DAPI to stain nuclei. Samples were immediately analysed under a fluorescence microscope using a standard fluorescein filter set (Olympus, Tokyo, Japan) to view the green fluorescence of apoptotic cells at 520 nm and blue DAPI-stained nuclei at 460 nm.
In Vivo Experiments
C57BL/6 J mice (age range: 4–6 weeks) were obtained from the Laboratory Animal Center of the Fourth Military Medical University. The animals were maintained under a 12/12 h light–dark cycle and at 25 °C. The mice were randomly divided into five groups (n=10). Group A: blank control group; Group B: mice with Tg treatment and supplemented with vehicle group; Group C: mice with Tg treatment and supplemented with 1 μg/kg 17β-E2 group; Group D: mice with Tg treatment and supplemented with 10 μg/kg 17β-E2 group; and Group E: mice with Tg treatment and supplemented with 50 μg/kg 17β-E2 group. Tg treatment was adopted by local injection of 10 nM Tg into tibias of mice. Meanwhile, these mice received daily subcutaneous injection of different doses of 17β-E2 (diluted in a sesame oil solution) on the back of the neck for 2 weeks. Then mice were killed by decapitation. Tibias of mice were dissected and placed in 4% methanol-free formaldehyde solution for further TUNEL analysis. The experimental procedures in this study were approved by the Ethics Committee for Animal Experimentation of the Fourth Military Medical University, P.R. China.
Detection of Caspase-12 Activity
Caspase-12 activity was measured spectrophotometrically via the detection of free AFC cleavage by caspase-12-specific substrates. These experiments were completed using a Caspase-12 Assay Kit (Biovision, San Francisco, CA, USA). After the cell lysates were incubated with ATAD-AFC for 2 h at 37 °C, the samples were read at 505 nm.
Detection of Caspase-3 Activity
Caspase-3 activity was measured spectrophotometrically via the detection of pNA cleavage by caspase-3-specific substrates. These experiments were completed using a Caspase-3 Assay Kit (Beyotime, Shanghai, China). After the cell lysates were incubated with Ac-DEVD-pNA for 2 h at 37 °C, the samples were read at 405 nm.
Gene Silencing
The sense sequences for Grp78 small interfering RNA (siRNA) were 5′-GGAGCGCAUUGAUACUAGA-3′ (Ambion). The cells were transfected with Grp78 siRNA using the Lipofectamine 2000 reagent (Invitrogen, CA, USA) according to the manufacturer’s instructions. Silencer negative control siRNA (control siRNA) (Ambion) was used as a negative control under similar conditions.
Annexin V/Propidium Iodide Double Staining
The number of apoptosis cells was determined by Annexin V/propidium iodide (PI) double staining. Cells were exposed to 10 nM Tg for 24 h and then incubated with FITC-conjugated Annexin V in binding buffer (0.01 M HEPES, 0.14 M NaCl and 2.5 mM CaCl2, pH 7.4) for 30 min at 37 °C in the dark. After incubation, the cells were washed and resuspended in 200 μl PBS with 1% FCS and additionally incubated with 10 μl of 1 mg/ml PI solution. The Annexin V-positive cells were detected using a FACSCalibur flow cytometer (BD Biosciences, San Jose, USA), and the results were analyzed using CellQuest software (BD Biosciences, San Jose, USA). Annexin V-FITC conjugates were detected with the FL1 channel of the FACSCalibur machine. PI was read on the FL2 channel.
Nuclear and Cytoplasmic Protein Extraction
Nuclear and cytoplasmic protein extractions were performed using a Nuclear and Cytoplasmic Protein Extraction Kit (Beyotime, Shanghai, China). Briefly, 2 × 106 cells were resuspended in 200 μl of cytoplasmic protein isolation solution A and homogenized on ice. Next, 10 μl cytoplasmic protein isolation solution B was added, and the cells were homogenized on ice. The homogenate was centrifuged at 10 000 × g for 5 min at 4 °C. The resulting supernatant was the cytoplasmic protein fraction. The pellet was resuspended in 50 μl nuclear protein isolation solution, homogenized on ice and centrifuged at 10,000 × g for 10 min. The resulting supernatant was the nuclear protein fraction.
Plasmid Construction
The expression vector containing full-length TFII-I and Grp78 promoter–reporter gene constructs were developed in our lab.35 Briefly, full-length TFII-I was PCR-amplified using an Advantage-GC Genomic PCR kit (Clontech, Palo Alto, CA, USA), and the primers (synthesized by the Shanghai Sangon) were designed as follows: forward primer, 5′-TTGGATCCCGCCCCCCCGCTTCCCCGCACGCGC-3′ (BamHI) and reverse primer, 5′-GCTCTAGAAAACTATGCCGTCACAG-3′ (XbaI). The products were confirmed by sequencing (Shanghai Sangon, Shanghai, China) and then cloned into the pcDNA3.1 vector (Promega, Madison, WI, USA). The Grp78 promoter subregions (−149/+7, which contains all three ERSEs) was synthesized and cloned into the pGL3-Basic vector (Promega, Madison, WI, USA) by Wolsen Biological Technology.
Reporter Gene Assays
For the luciferase assay, cells were grown to 60–80% confluence. Grp78 promoter–reporter gene constructs were then co-transfected with or without the TFII-I vector using Lipofectamine 2000 (Invitrogen) as recommended by the manufacturer. The amount of total DNA was normalized by the addition of an empty vector to the reaction mixture. For stress induction, the cells were treated with 10 nM Tg in the absence or presence of 17β-E2 (10 nM) for 24 h. The cells were then prepared for the luciferase assays using the Dual-Luciferase Reporter Assay System (Promega, Madison, WI). The relative activity was defined as the ratio of firefly luciferase activity to renilla luciferase activity.
Chromatin Immunoprecipitation
Chromatin Immunoprecipitation (ChIP) assay was performed using the ChIP-IT kit (Millipore, Billerica, MA) according to the manufacturer’s protocol. Briefly, the cells were exposed to 10 nM Tg in the absence or presence of 17β-E2 (10 nM) for 24 h. Cell lysates were incubated with anti-immunoglobulin G (IgG) or anti-TFII-I antibody (Abcam, British). The immunoprecipitated DNA was amplified by the Grp78 promoter-specific primers. The experimental PCR reactions generated a 160-bp product from the regulatory region of the Grp78 promoter containing three ERSEs, whereas the negative control PCR reactions generated a 160-bp product from a distal region without any ERSEs. Grp78 ChIP primer: forward 5′-GCGAAGCTTAGCCGCCGCCGGTCGA-3′, reverse 5′-CGAGTAGGCGACGG TGAGGT-3′. Grp78 negative control primer: forward 5′-TCTGTCTAACTGG ATAACCCCACAA-3′, reverse 5′-TGCTCCTGTGCTACGGC-3′.
Statistical Analysis
Statistical analysis was performed using SPSS 13.0 statistical software. The results were expressed as mean values±s.d. And the Student’s t-test or one-way ANOVA were used to evaluate the statistical significance in the groups. The differences were considered significant when P<0.05.
RESULTS
17β-E2 Inhibits ER Stress-Induced Apoptosis in Osteoblasts
Previous studies have shown that exposure of the cultures to Thapsigargin (Tg), a inhibitor of Ca2+ ATPase in the ER, causes osteoblasts ER stress.36 To investigate the protective effect of 17β-E2 against ER stress in osteoblasts, mouse calvaria osteoblasts MC3T3-E1 cells and primary osteoblasts were incubated with 10 nM Tg for 24 h to induce ER stress. DMSO was used as a negative control. The results showed that Grp78 and C/EBP-homologous protein (CHOP) protein levels were markedly increased in cells treated with Tg compared with control cells (P<0.05, Figure 1a). In addition, the mRNA levels of Grp78 and CHOP were also remarkably increased in Tg-treated cells compared with control cells (P<0.05, Figure 1b). These findings support previous work that treatment of osteoblasts with Tg causes ER stress.36 ER stress might be a mediator of cell death, thus the survival rate of MC3T3-E1 cells and primary osteoblasts were examined by MTT survival assay after Tg treatments. The results demonstrated that Tg treatment significantly reduced the survival rate of MC3T3-E1 cells and primary osteoblasts (P<0.05, Figure 1c). However, pretreatment with increasing concentration of 17β-E2 remarkably reversed survival rate inhibited by Tg and the effects plateaued at 10 nm (P<0.05, Figure 1c). These results suggested that 17β-E2 could inhibit ER stress-induced cell death. To determine whether cell death was apoptotic like, TUNEL assay was performed. Because the responses to 10 nM and 100 nM 17β-E2 were virtually identical, 10 nM 17β-E2 was thereafter employed. The statistic data showed that the percentage of apoptotic cells increased after Tg treatment. However, pretreated with 10 nM 17β-E2 reduced the percentage of apoptotic cells induced by Tg (P<0.05, Figure 1d and e). Activation of caspase-12 is associated with ER stress-induced apoptosis of murine.37 Thus, the effect of 17β-E2 on activation of caspase-12 was investigated. We found that the activity of caspase-12 was significantly increased after Tg treatment, but pretreated with 10 nM 17β-E2 markedly reduced the activity of caspase-12 induced by Tg in MC3T3-E1 cells and primary osteoblasts (P<0.05, Figure 1f). Caspase-3 (also named CPP32, apopain, and YAMA) has been identified as a key mediator of apoptosis in mammalian cells.38 We further assessed the activation of caspase-3. The results showed that Tg treatment enhanced caspase-3 activation, and the increase was blocked by 17β-E2 pretreatment in MC3T3-E1 cells and primary osteoblasts (P<0.05, Figure 1g). To further validate the protective effect of 17β-E2 against osteoblasts apoptosis in vivo, we induce local osteoblasts apoptosis of tibias in mice by the local injection of Tg into tibias of mice. Meanwhile, these mice received daily subcutaneous injection of different doses of 17β-E2. Then mice were killed and osteoblasts apoptosis in tibias were tested by TUNEL analysis. The results demonstrate that Tg treatment significantly increased the apoptosis of osteoblasts in tibias. However, treatment with increasing concentration of 17β-E2 remarkably reversed apoptosis induced by Tg (P<0.05, Figure 1h and i). Together, these results suggest that 17β-E2 protects osteoblasts against ER stress-induced apoptosis in vitro and vivo.
17β-E2 protects osteoblasts from ER stress-induced apoptosis. The cultured MC3T3-E1 cells and primary osteoblasts were treated with or without Tg (10 nM) for 24 h. (a) Western blot was used to examine the expression levels of Grp78 and CHOP in MC3T3-E1 cells and primary osteoblasts. (b) Grp78 and CHOP mRNA levels were tested by RT–PCR in MC3T3-E1 cells and primary osteoblasts. (c) 17β-E2 was applied to the MC3T3-E1 cells and primary osteoblasts at 0.1, 1, 10, or 100 nM (final concentration). After 12 h, the cultures were incubated with Tg (10 nM) for 24 h in the presence of 17β-E2 and then cell survival was determined by MTT assay. (d) The cultured MC3T3-E1 cells and primary osteoblasts were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h. Cell apoptosis was quantified by TUNEL assay. Scale=100 μm. (e) Quantitation of cell apoptosis in MC3T3-E1 cells and primary osteoblasts as indicated in panel d. (f) Caspase-12 activity was detected by caspase-12 assay kit in MC3T3-E1 cells and primary osteoblasts that were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h. (g) Caspase-3 activity was detected by caspase-3 assay kit in MC3T3-E1 cells and primary osteoblasts that were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h. (h) The mice were randomly divided into five groups (n=10). Group A: blank control group; Group B: mice with Tg treatment and supplemented with vehicle group; Group C: mice with Tg treatment and supplemented with 1 μg/kg 17β-E2 group; Group D: mice with Tg treatment and supplemented with 10 μg/kg 17β-E2 group; and Group E: mice with Tg treatment and supplemented with 50 μg/kg 17β-E2 group. Tg treatment was adopted by local injection of 10 nM Tg into tibias of mice. Meanwhile these mice received daily subcutaneous injection of different doses of 17β-E2 for 2 weeks. Then the mice were killed and osteoblast apoptosis in tibias was tested by TUNEL analysis. Scale=100μm. (i) Quantitation of osteoblasts apoptosis in vivo as indicated in panel h. Bars represent each sample performed in triplicate, and the error bars represent the s.d. *P<0.05, by ANOVA analysis or Student’s t-test.
17β-E2 Promotes Grp78 Induction to Protect Osteoblasts Cells from ER Stress-Induced Apoptosis
We examined the protein and mRNA levels of Grp78 and CHOP in ER stress condition. The results showed that 17β-E2 treatments increased Grp78 protein and mRNA levels following Tg treatments in MC3T3-E1 cells and primary osteoblasts (Figure 2a and b). However, 17β-E2 treatments were not able to alter CHOP protein and mRNA levels following Tg treatments in MC3T3-E1 cells and primary osteoblasts (Figure 2a and b). These results suggested that 17β-E2 was involved in ER stress-induced Grp78 expression, but not involved in CHOP induction. To examine whether the protective effect of 17β-E2 on ER stress-induced apoptosis is dependent on Grp78, we used siRNA to knock down Grp78 in MC3T3-E1 cells. Grp78 siRNA led to a marked reduction of Grp78 protein and mRNA levels (Figure 2c and d). When the cells were transfected with Grp78 siRNA, 17β-E2 treatments did not decrease the percentage of apoptotic cell compared with corresponding control cells (P>0.05, Figure 2e). To further validate this finding, we examined the activities of caspase-12 and caspase-3 in the condition that Grp78 induction was inhibited with Grp78 siRNA. The results showed that 17β-E2 treatments decreased activities of caspase-12 and caspase-3 following control siRNA treatments (P<0.05, Figure 2f and g). However, 17β-E2 treatments were not able to inhibit activities of caspase-12 and caspase-3 following Grp78 siRNA treatments (P>0.05, Figure 2f and g). These results suggested that 17β-E2 protects MC3T3-E1 cells from ER stress-induced apoptosis by promoting Grp78 induction.
17β-E2 promotes Grp78 induction to protect osteoblasts from ER stress-induced apoptosis. The cells were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h. (a) Western blot was used to examine the expression levels of Grp78 and CHOP in MC3T3-E1 cells and primary osteoblasts. (b) Grp78 and CHOP mRNA levels were tested by RT–PCR in MC3T3-E1 cells and primary osteoblasts. (c) Western blot was performed to examine Grp78 protein levels in MC3T3-E1 cells transduced with Grp78 siRNA. (d) RT–PCR was performed to examine Grp78 mRNA in MC3T3-E1 cells transduced with Grp78 siRNA. (e) The MC3T3-E1 cells were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h after transfected with Grp78 siRNA. Annexin V/PI double staining was performed to detect the apoptotic cells. (f) Caspase-12 activity was detected by Caspase-12 assay kit in MC3T3-E1 cells that were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h after transfected with Grp78 siRNA. (g) Caspase-3 activity was detected by caspase-3 assay kit in MC3T3-E1 cells that were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h after transfected with Grp78 siRNA. Bars represent each sample performed in triplicate, and the error bars represent the s.d. *P<0.05, by Student’s t-test.
17 β -E2 Induces Phosphorylation of TFII-I and the Binding of TFII-I to the Grp78 Promoter to Increase the Transcription of Grp78 in Response to ER Stress
Previous studies indicated that the Grp78 promoter contained multiple copies of the ER stress response elements (ERSEs). NF-Y, YY1, ATF6 and TFII-I are four key factors that bind to the ERSEs of Grp78 promoter and subsequently promote the expression of Bip.39, 40 Therefore, we examined the expression levels of NF-Y, YY1 and ATF6 in MC3T3-E1 cells treated with or without 17β-E2. Unexpectedly, 17β-E2 did not significantly change these proteins expression levels following Tg treatment (Figure 3a). We then tested the phosphorylation and expression levels of TFII-I. We observed that 17β-E2 did not alter the TFII-I expression levels in MC3T3-E1 cells. However, 17β-E2 markedly increased the phosphorylated TFII-I levels after Tg treatment (Figure 3b). These results indicate that 17β-E2 may induce phosphorylation of TFII-I in response to ER stress. To further detect whether 17β-E2-promoted Grp78 induction was mediated through TFII-I, a Grp78 (−149/+7)/Luc promoter construct was co-transfected with TFII-I expression plasmids into MC3T3-E1 cells. We observed that 17β-E2 moderately enhanced the Grp78 promoter activity in the absence of TFII-I after Tg treatment. However, 17β-E2 could enhance the Grp78 promoter activity in a dose-dependent manner in the presence of TFII-I after Tg treatment (Figure 3c). The results suggested that 17β-E2-promoted Grp78 induction is predominantly mediated by TFII-I in ER stress condition. Transcription factors might have roles via their translocation from the cytoplasm to the nucleus. Thus, cytoplasmic and nuclear proteins were extracted and analyzed. We observed that TFII-I phosphorylation significantly increased in the nucleus of 17β-E2-treated MC3T3-E1 cells after Tg treatment (Figure 3d). To directly elucidate the effects of 17β-E2 on the binding of TFII-I to the Grp78 promoter, ChIP assays were performed in MC3T3-E1 cells after Tg treatment. We observed that the binding activity of TFII-I to the Grp78 promoter was low in control cells, whereas the binding activity of TFII-I to the Grp78 promoter was markedly increased in 17β-E2-treated cells (Figure 3e). These results suggested that 17β-E2 increased binding activity of TFII-I to the Grp78 promoter of MC3T3-E1 cells in ER stress condition. These results indicated that 17β-E2 induces TFII-I nuclear localization and binding to Grp78 promoter in response to ER stress in MC3T3-E1 cells.
17β-E2 induces phosphorylation of TFII-I and the binding of TFII-I to the Grp78 promoter to increase the transcription of Grp78 in response to ER stress in MC3T3-E1 cells. The cultured MC3T3-E1 cells were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h. (a) The expression levels of NY-F, YY1 and ATF6 were examined by western blot. (b) The phosphorylation levels and the expression levels of TFII-I were examined by western blot. (c) Grp78 promoter–reporter gene constructs were co-transfected with or without the TFII-I vector into MC3T3-E1 cells. Twelve hours after transfection, cells were then treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h, and the luciferase activity was measured. (d) The TFII-I phosphorylation levels were tested in the nuclear and cytoplasmic fractions. Protein expression levels in the nuclear and cytosolic fractions were normalized to Lamin B1 and β-actin, respectively. (e) ChIP assay using antibody against TFII-I was performed in MC3T3-E1 cells that were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h. The normal IgG was used as a negative control and input indicates 5% input DNA, a positive amplification control. The fragment was amplified by the Grp78 promoter-specific primers that contains the TFII-I binding sequence, whereas the negative control PCR reactions generated a fragment that does not contain any TFII-I binding sequence. Bars represent each sample performed in triplicate, and the error bars represent the s.d. *P<0.05, **P<0.01, by one-way ANOVA analysis.
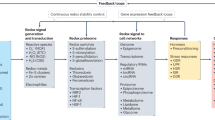
17 β -E2 Activates Ras-ERK1/2 Signaling Pathway to Promote Grp78 Induction in Response to ER Stress in MC3T3-E1 Cells
TFII-I is a multifunctional transcription factor that can be a direct substrate for ERK1/2 and Src. It has been reported that the ERK1/2 and Src regulate the activity of TFII-I by direct phosphorylation.41, 42 To identify whether ERK1/2 or Src was involved in 17β-E2-induced TFII-I tyrosine phosphorylation, the phosphorylation and expression levels of ERK1/2 and Src were tested. Although, 17β-E2 did not alter the phosphorylation and expression levels of Src, 17β-E2 markedly increased phosphorylated ERK1/2 levels in MC3T3-E1 cells after Tg treatment (Figure 4a). In addition, we observed that addition of 17β-E2 markedly promoted the Ras kinase activity after Tg treatment (Figure 4b). These data indicated that 17β-E2 may activate the Ras-ERK1/2 signaling pathway of MC3T3-E1 cells in ER stress condition. To examine whether 17β-E2-induced Grp78 induction was dependent on the Ras-ERK1/2 signaling pathway, the ERK1/2 activity-specific inhibitor U0126 was used. We observed that the addition of ERK1/2 inhibitor U0126 significantly blocked the promotive effect of 17β-E2 on TFII-I phosphorylation and Grp78 expression in MC3T3-E1 cells (Figure 4c). Moreover, we confirmed that the addition of ERK1/2 inhibitor blocked the promotive effect of 17β-E2 on Grp78 mRNA expression in MC3T3-E1 cells (Figure 4d). These results suggested that Ras-ERK1/2 signaling pathway is involved in 17β-E2-induced Grp78 expression.
17β-E2 activates Ras-ERK1/2 pathway to promote Grp78 induction in response to ER stress in MC3T3-E1 cells. The cultured MC3T3-E1 cells were treated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h. (a) Western blot was used to examine the phosphorylation and the expression levels of ERK1/2 and Src. (b) The activity and the expression levels of Ras were examined by western blot. The MC3T3-E1 cells were pretreated with ERK1/2 inhibitor U0126 (100 nM) and then incubated with Tg (10 nM) in the absence or presence of 17β-E2 (10 nM) for 24 h. (c) Western blot was performed to examine the phosphorylation level of TFII-I, expression levels of TFII-I and expression levels of Grp78 in MC3T3-E1 cells. (d) Grp78 mRNA levels were tested by RT–PCR in MC3T3-E1 cells.
DISCUSSION
Osteoporosis is characterized by low bone mass resulting from an imbalance between bone resorption by osteoclasts and bone formation by osteoblasts. Therefore, decreased bone formation by osteoblasts may cause the development of osteoporosis, and the rate of osteoblast apoptosis is responsible for the regulation of bone formation.1, 2, 3, 4, 5 ER stress has been implicated as a crucial mechanism of apoptosis in various cell death processes, including osteoblast apoptosis during the development of osteoporosis.22, 23, 24, 25, 26 Protective effects of estrogen on apoptosis of various cells have been indicated.32, 33, 34 However, it is not entirely clear if estrogen can protect osteoblasts against ER stress-induced apoptosis. In this study, we examined the effects of 17β-E2, one of the primary estrogens, on ER stress-induced apoptosis in osteoblasts. We found that by promoting TFII-I activity through Ras-ERK1/2 pathway, 17β-E2 enhances induction of Grp78 and then inhibits activation of caspase-12 and caspase-3, thus reducing cell apoptosis of osteoblasts in response to ER stress.
ER stress has been reported to be involved in apoptosis induction that occurs during various pathophysiological progresses, including osteoporosis.22, 23, 24, 25, 26 The ER stress is generally activated in response to various stressful conditions, such as hypoxia, the accumulation of unfolded or misfolded proteins, the alterations of calcium homeostasis, low glucose levels and others.8, 9, 10 Recent reports have shown that ER stress occurs during osteogenic differentiation.17, 18, 19, 20, 21 ER stress-induced apoptosis of osteoblasts has also been implicated in the pathogenesis of osteoporosis.22, 23, 24, 25, 26 Our study found that the MC3T3-E1 cells, the mouse calvaria osteoblasts, were led into the decrease of cellular viability in response to ER stress. However, pretreatment with 17β-E2 can increase the viability of osteoblasts in ER stress in a dose-dependent manner between 0.1 nM and 100 nM and the effects plateaued at 10 nM. TUNEL assay further confirmed that 17β-E2 inhibited apoptosis of osteoblasts in ER stress. These results demonstrated that 17β-E2 could protect osteoblasts from ER stress-induced apoptosis.
Caspases are the primary mediators of apoptosis. It has been demonstrated that activation of caspase-12 and caspase-3 have key roles in ER stress-induced apoptosis.43, 44 Caspase-12 is a particular mediator of the ER stress-induced apoptosis in skeletal tissue. It is reported that cells knockout of caspase-12 are resistant to ER stress-induced apoptosis. Excessive ER stress can trigger apoptosis through the activation of caspase-12, which is cleaved and activated during ER stress.37 Caspase-12 triggers the activation of caspases-7, caspases-9, and caspases-3 in a cytochrome c-independent manner.45 Caspase-3 is of particular interest as it appears to be a common downstream apoptosis effector. It exists as proenzyme in most cells, including osteoblasts, and is processed and activated by caspase-8 and caspase-9 to the heterodimeric form.38 In this study, we found that 17β-E2 was shown to attenuate ER stress-induced activation of caspase-12 and caspase-3. The results further confirmed that 17β-E2 could protect osteoblasts from ER stress-induced apoptosis that was mediated by caspases.
ER stress-induced apoptosis is predominantly mediated by upregulation of the CCAAT/enhancer binding protein (C/EBP) family member CHOP, which is a major ER stress pro-apoptotic transcription factor.45 CHOP mediates cell death through the induction of various genes including GADD34 and ERO1, which may tip the balance toward apoptosis. In particular, CHOP is the first molecule identified to mediate ERS-induced apoptosis. CHOP inhibits expression of Bcl-2, depletes glutathione, facilitates translocation of pro-apoptotic protein Bax, thereby inducing apoptosis.46, 47 Unexpectedly, we found that 17β-E2 did not alter CHOP expression in responses to ER stress. In an attempt to diminish ER stress-induced apoptosis, cells are known to suppress general transcriptional activities and initiate preferential translation of ER chaperone.11 Grp78, also referred to as Bip, is a major ER chaperone and has a critical role in protein folding and assembly, targeting misfolded protein for degradation and controlling the activation of transmembrane ER stress sensors. Grp78 upregulation is believed to increase the capacity to buffer stressful insults initiating from the ER. Furthermore, due to its anti-apoptotic property, expression of Grp78 represents an important pro-survival response. Grp78 can alleviate misfolded protein aggregation in the ER, thus reducing cell apoptosis.12, 13 In addition to its chaperoning function, Grp78 can bind and specifically block the activation of ER transmembrane signaling molecules such as ATF6, PERK and IRE1 in non-stressed cells. Grp78 is known to inhibit caspase-mediated cell death by forming complexes with procaspases-7 and procaspases-12, and Grp78 disassociation facilitates procaspase-12 activation. In support of this mechanism, Grp78 co-precipitates with caspase-12 in vivo, and recombinant Grp78 can suppress activation of caspase-12 and caspase-3.14, 15, 16 It has reported that Grp78 is downregulated in osteoblasts from osteoporosis patients.22 We demonstrated that 17β-E2 increased Grp78 expression in responses to ER stress. Furthermore, Grp78-specific siRNA reversed the inhibition of 17β-E2 on apoptosis as well as activation of caspase-12 and caspase-3 in ER stress, suggesting that Grp78 expression is an obligatory event in protective effect of 17β-E2 on ER stress-induced apoptosis.
The Grp78 promoter contains multiple copies of the ERSEs.39 Previous reports observed that a protein exhibits increased binding to the ERSEs of Grp78 promoters following Tg treatment. Subsequently, the protein binding to the ERSEs of Grp78 promoters has been identified as the multifunctional transcription factor TFII-I.48 It is reported that ER stress results in a marked increase of TFII-I phosphorylation and localization of phosphorylated TFII-I to the nucleus. It is also reported that TFII-I is required for optimal induction of Grp78 in ER stress. TFII-I was discovered as a co-activator for ATF6. It can stabilize ATF6 binding to the ERSEs of Grp78 promoters, in cooperation with other binding factors such as YY1 and NF-Y.39, 40 We found that 17β-E2 could promote TFII-I phosphorylation and nuclear localization and enhance the Grp78 promoter activity in a dose-dependent manner in the presence of TFII-I in response to ER stress. ChIP analysis further revealed that 17β-E2 enhanced binding of TFII-I to the Grp78 promoter in ER stress. These findings suggested that 17β-E2-promoted Grp78 expression is dependent on TFII-I.
TFII-I is a multifunctional protein that appears to have functions in both signal transduction and transcription, and its activity is regulated by phosphorylation. One kinase that regulates phosphorylated TFII-I is Src. It has been reported that TFII-I undergoes a Src kinase-dependent phosphorylation and nuclear localization in response to growth factor signaling.35, 42 It has also been reported that ERK1/2, which is a downstream target of Ras, regulates the activity of TFII-I by direct phosphorylation. ERK1/2 forms an in vivo complex with TFII-I and dominant-negative Ras abrogates this interaction.41 Consistent with previous findings, we found that 17β-E2-promoted Ras-ERK1/2 signal cascades activity. In addition, our observations that the addition of ERK1/2 inhibitor U0126 significantly blocked the promotive effect of 17β-E2 on TFII-I phosphorylation and Grp78 expression further confirmed that 17β-E2 activated Ras-ERK1/2 signal cascades to promote TFII-I phosphorylation. The 17β-E2 signal is transmitted by binding with the estrogen receptors.34 Although recent studies have shown that estrogen receptors contribute to various cell functions mediated by Ras-ERK1/2 cascade, the mechanism by which the estrogen receptors activate Ras-ERK1/2 cascade is not entirely clear.49, 50
In summary, our present results support that 17β-E2 protects osteoblasts against ER stress-induced apoptosis through promoting Ras-ERK1/2 signaling pathway-dependent TFII-I activity to enhance the induction of Grp78. ER stress-induced apoptosis acts as a causative agent of osteoporosis.22, 23, 24, 25, 26 Our observations indicated that 17β-E2 may contribute to protective effects on ER stress-induced apoptosis in osteoblasts. Osteoporosis is a highly prevalent disease and results in massive costs both to the individual and to the society through associated fragility fractures.2, 3 Therefore, an understanding of the mechanism of protective effects of estrogen in bone have very important implications for the prevention and treatment of osteoporosis. These findings may provide important information concerning the effect of postmenopausal estrogen replacement therapy for osteoporosis.
References
Karsenty G, Wagner EF . Reaching a genetic and molecular understanding of skeletal development. Dev Cell 2002;2:389–406.
Rodan GA, Martin TJ . Therapeutic approaches to bone diseases. Science 2000;289:1508–1514.
Raisz LG . Pathogenesis of osteoporosis: concepts, conflicts, and prospects. J Clin Invest 2005;115:3318–3325.
Weinstein RS, Manolagas SC . Apoptosis and osteoporosis. Am J Med 2000;108:153–164.
Hock JM, Krishnan V, Onyia JE et al. Osteoblast apoptosis and bone turnover. J Bone Miner Res 2001;16:975–984.
Hamamura K, Yokota H . Stress to endoplasmic reticulum of mouse osteoblasts induces apoptosis and transcriptional activation for bone remodeling. FEBS Lett 2007;581:1769–1774.
Cui W, Ma J, Wang X et al. Free fatty acid induces endoplasmic reticulum stress and apoptosis of β-cells by Ca2+/Calpain-2 pathways. PLoS One 2013;8:e59921.
Schroder M . Endoplasmic reticulum stress responses. Cell Mol Life Sci 2008;65:862–894.
Boyce M, Yuan J . Cellular response to endoplasmic reticulum stress: a matter of life or death. Cell Death Differ 2006;13:363–373.
Hotamisligil GS . Endoplasmic reticulum stress and the inflammatory basis of metabolic disease. Cell 2010;140:900–917.
Wu J, Kaufman RJ . From acute ER stress to physiological roles of the unfolded protein response. Cell Death Differ 2006;13:374–384.
Kaufman RJ . Stress signaling from the lumen of the endoplasmic reticulum: coordination of gene transcriptional and translational controls. Genes Dev 1999;13:1211–1233.
Sherman MY, Goldberg AL . Cellular defenses against unfolded proteins: a cell biologist thinks about neurodegenerative diseases. Neuron 2001;29:15–32.
Fu Y, Li J, Lee AS . GRP78/BiP inhibits endoplasmic reticulum BIK and protects human breast cancer cells against estrogen starvation-induced apoptosis. Cancer Res 2007;67:3734–3740.
Reddy RK, Mao C, Baumeister P et al. Endoplasmic reticulum chaperone protein GRP78 protects cells from apoptosis induced by topoisomerase inhibitors: role of ATP binding site in suppression of caspase-7 activation. J Biol Chem 2003;278:20915–20924.
Wang M, Ye R, Barron E et al. Essential role of the unfolded protein response regulator GRP78/BiP in protection from neuronal apoptosis. Cell Death Differ 2010;17:488–498.
Saito A, Ochiai K, Kondo S et al. Endoplasmic reticulum stress response mediated by the PERK-eIF2(alpha)-ATF4 pathway is involved in osteoblast differentiation induced by BMP2. J Biol Chem 2011;286:4809–4818.
Liberman M, Johnson RC, Handy DE et al. Leopold bone morphogenetic protein-2 activates NADPH oxidase to increase endoplasmic reticulum stress and human coronary artery smooth muscle cell calcification. Biochem Biophys Res Commun 2011;413:436–441.
Murakami T, Saito A, Hino S et al. Signalling mediated by the endoplasmic reticulum stress transducer OASIS is involved in bone formation. Nat Cell Biol 2009;11:1205–1211.
Liu Y, Zhou J, Zhao W et al. XBP1S associates with RUNX2 and regulates chondrocyte hypertrophy. J Biol Chem 2012;287:34500–34513.
Elefteriou F, Benson MD, Sowa H et al. ATF4 mediation of NF1 functions in osteoblast reveals a nutritional basis for congenital skeletal dysplasiae. Cell Metab 2006;4:441–451.
Hino SI, Kondo S, Yoshinaga K et al. Regulation of ER molecular chaperone prevents bone loss in a murine model for osteoporosis. J Bone Miner Metab 2010;28:131–138.
Park SJ, Kim KJ, Kim WU et al. Involvement of endoplasmic reticulum stress in homocysteine-induced apoptosis of osteoblastic cells. J Bone Miner Metab 2012;30:474–484.
Tang CH, Chiu YC, Huang CF et al. Arsenic induces cell apoptosis in cultured osteoblasts through endoplasmic reticulum stress. Toxicol Appl Pharmacol 2009;241:173–181.
Lisse TS, Thiele F, Fuchs H et al. ER stress-mediated apoptosis in a new mouse model of osteogenesis imperfect. PLoS Genet 2008;4:e7.
He L, Lee J, Jang JH et al. Osteoporosis regulation by salubrinal through eIF2α mediated differentiation of osteoclast and osteoblast. Cell Signal 2013;25:552–560.
Kousteni S, Chen JR, Bellido T et al. Reversal of bone loss in mice by nongenotropic signaling of sex steroids. Science 2002;298:843–846.
Delmas PD . Treatment of postmenopausal osteoporosis. Lancet 2002;359:2018–2026.
Neugarten J, Medve I, Lei J et al. Estradiol suppresses mesangial cell type I collagen synthesis via activation of the MAP kinase cascade. Am J Physiol 1999;277:F875–F881.
Song RX, McPherson RA, Adam L et al. Linkage of rapid estrogen action to MAPK activation by ERα-Shc association and Shc pathway activation. Mol Endocrinol 2002;16:116–127.
Chen CC, Lee WR, Safe S . Egr-1 is activated by 17β-estradiol in MCF-7 cells by mitogen-activated protein kinase-dependent phosphorylation of ELK-1. J Cell Biochem 2004;93:1063–1074.
Brinton RD, Tran J, Proffitt P et al. 17β-Estradiol enhances the outgrowth and survival of neocortical neurons in culture. Neurochem Res 1997;22:1339–1351.
Pike CJ . Estrogen modulates neuronal Bcl-xL expression and β-amyloid-induced apoptosis: relevance to Alzheimer’s disease. J Neurochem 1999;72:1552–1563.
Nakamura T, Imai Y, Matsumoto T et al. Estrogen prevents bone loss via estrogen receptor α and induction of Fas ligand in osteoclasts. Cell 2007;130:811–823.
Tang J, Guo YS, Zhang Y et al. CD147 induces UPR to inhibit apoptosis and chemosensitivity by increasing the transcription of Bip in hepatocellular carcinoma. Cell Death Differ 2012;19:1779–1790.
Hamamura K, Liu Y, Yokota H . Microarray analysis of thapsigargin-induced stress to the endoplasmic reticulum of mouse osteoblasts. J Bone Miner Metab 2008;26:231–240.
Nakagawa T, Zhu H, Morishima N et al. Caspase-12 mediates endoplasmic- reticulum-specific apoptosis and cytotoxicity by amyloid-beta. Nature 2000;403:98–103.
Porter AG, Janicke RU . Emerging roles of caspase-3 in apoptosis. Cell Death Differ 1999;6:99–104.
Parker R, Phan T, Baumeister P et al. Identification of TFII-I as the endoplasmic reticulum stress response element binding factor ERSF: its autoregulation by stress and interaction with ATF6. Mol Cell Biol 2001;21:3220–3233.
Yoshida H, Okada T, Haze K et al. Endoplasmic reticulum stress-induced formation of transcription factor complex ERSF including NF-Y (CBF) and activating transcription factors 6alpha and 6beta that activates the mammalian unfolded protein response. Mol Cell Biol 2001;21:1239–1248.
Kim DW, Cochran BH . Extracellular signal-regulated kinase binds to TFII-I and regulates its activation of the c-fos promoter. Mol Cell Biol 2000;20:1140–1148.
Hong M, Lin MY, Huang JM et al. Transcriptional regulation of the Grp78 promoter by endoplasmic reticulum stress. J Biol Chem 2005;280:16821–16828.
Slee EA, Adrain C, Martin SJ . Serial killers: ordering caspase activation events in apoptosis. Cell Death Differ 1999;6:1067–1074.
Morishima N, Nakanishi K, Takenouchi H et al. An endoplasmic reticulum stress-specific caspase cascade in apoptosis. Cytochrome c-independent activation of caspase-9 by caspase-12. J Biol Chem 2002;277:34287–34294.
Oyadomari S, Mori M . Roles of CHOP/GADD153 in endoplasmic reticulum stress. Cell Death Differ 2004;11:381–389.
Chen CM, Wu CT, Chiang CK et al. C/EBP homologous protein (CHOP) deficiency aggravates hippocampal cell apoptosis and impairs memory performance. PLoS One 2012;7:e40801.
McCullough KD, Martindale JL, Klotz LO et al. Gadd153 sensitizes cells to endoplasmic reticulum stress by down-regulating Bcl2 and perturbing the cellular redox state. Mol Cell Biol 2001;21:1249–1259.
Grueneberg DA, Henry RW, Brauer A et al. A multifunctional DNA-binding protein that promotes the formation of serum response factor/homeodomain complexes: identity to TFII-I. Genes Dev 1997;11:2482–2493.
Wong CW, McNally C, Nickbarg E et al. Estrogen receptor-interacting protein that modulates its nongenomic activity-crosstalk with Src/Erk phosphorylation cascade. Proc Natl Acad Sci USA 2002;99:14783–14788.
Zhao L, Brinton RD . Estrogen receptor alpha and beta differentially regulate intracellular Ca(2+) dynamics leading to ERK phosphorylation and estrogen neuroprotection in hippocampal neurons. Brain Res 2007;1172:48–59.
Acknowledgements
The authors gratefully acknowledge professor Zhi-Nan Chen and professor Jian-Li Jiang for excellent assistance. This work is supported by the National Nature Science Foundation of China (31101005), National Basic Research Program of China (2011CB964703) and Program for Changjiang Scholars and Innovative Research Team in University (IRT1053).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Although estrogen prevents postmenopausal bone loss partially due to its anti-apoptosis effects in osteoblasts, the underlying mechanism has not been fully elucidated. In this study, the authors show that by promoting activity of the transcription factor TFII-I through the Ras-ERK1/2 pathway, 17β-estradiol enhances induction of the molecular chaperone Grp78, thus reducing cell apoptosis of osteoblasts in response to endoplasmic reticulum stress.
Rights and permissions
About this article
Cite this article
Guo, YS., Sun, Z., Ma, J. et al. 17β-Estradiol inhibits ER stress-induced apoptosis through promotion of TFII-I-dependent Grp78 induction in osteoblasts. Lab Invest 94, 906–916 (2014). https://doi.org/10.1038/labinvest.2014.63
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2014.63
Keywords
This article is cited by
-
Bone and the Unfolded Protein Response: In Sickness and in Health
Calcified Tissue International (2023)
-
Estrogen inhibits endoplasmic reticulum stress and ameliorates myocardial ischemia/reperfusion injury in rats by upregulating SERCA2a
Cell Communication and Signaling (2022)
-
Estrogen Regulates Endoplasmic Reticulum Stress–Mediated Apoptosis by ERK-p65 Pathway to Promote Endometrial Angiogenesis
Reproductive Sciences (2021)
-
MicroRNA-495 downregulates AQP1 and facilitates proliferation and differentiation of osteoblasts in mice with tibial fracture through activation of p38 MAPK signaling pathway
Scientific Reports (2019)
-
Concomitant high expression of ERα36, GRP78 and GRP94 is associated with aggressive papillary thyroid cancer behavior
Cellular Oncology (2018)