Abstract
Individualized targeted therapies for cancer patients require accurate and reproducible assessment of biomarkers to be able to plan treatment accordingly. Recent studies have shown highly variable effects of preanalytical variables on gene expression profiling and protein levels of different tissue types. Several publications have described protein degradation of tissue samples as a direct result of delay of formalin fixation of the tissue. Phosphorylated proteins are more labile and epitope degradation can happen within 30 min of cold ischemic time. To address this issue, we evaluated the change in antigenicity of a series of phosphoproteins in paraffin-embedded samples from breast tumors as a function of time to formalin fixation. A tissue microarray consisting of 93 breast cancer specimens with documented time-to-fixation was used to evaluate changes in antigenicity of 12 phosphoepitopes frequently used in research settings as a function of cold ischemic time. Analysis was performed in a quantitative manner using the AQUA technology for quantitative immunofluorescence. For each marker, least squares univariate linear regression was performed and confidence intervals were computed using bootstrapping. The majority of the epitopes tested revealed changes in expression levels with increasing time to formalin fixation. Some phosphorylated proteins, such as phospho-HSP27 and phospho-S6 RP, involved in post-translational modification and stress response pathways increased in expression or phosphorylation levels. Others (like phospho-AKT, phosphor-ERK1/2, phospho-Tyrosine, phospho-MET, and others) are quite labile and loss of antigenicity can be reported within 1–2 h of cold ischemic time. Therefore specimen collection should be closely monitored and subjected to quality control measures to ensure accurate measurement of these epitopes. However, a few phosphoepitopes (like phospho-JAK2 and phospho-ER) are sufficiently robust for routine usage in companion diagnostic testing.
Similar content being viewed by others
Main
Recently, efforts have been made to improve individualized targeted therapy for cancer patients according to the expression of specific genes and proteins1, 2, 3, 4 and according to their status of activation as characterized by phosphorylation of specific epitopes. Phosphorylation of proteins is one of the most important modulatory mechanisms of activation of a number of molecular pathways and a potential indicator of cellular proliferation, migration, and other cellular functions.5, 6, 7, 8, 9 Thus, identification of activated pathways in tumor specimens is an essential element in efficient cancer diagnosis and treatment.6, 7, 8, 9, 10, 11 Protein phosphorylation is a dynamic balance between two opposite events: phosphorylation by highly specific kinases and dephosphorylation by less-specific phosphatases.12, 13, 14 To utilize phosphoproteins as markers of cellular signaling activity and tumor proliferation,6, 8, 9 it is crucial to assess their expression levels in tissue specimens that reflect the in vivo status as accurately as possible. Elevated expression levels of phospho-AKT, phospho-ERK1/2, phospho-mTor, and phospho-p20S6K, for example, have been described to be associated with tamoxifen resistance in postmenopausal breast cancer patients.15 Similarly elevated phospho-S6 kinase-1 and phospho-AKT levels are said to predict resistance to neoadjuvant chemotherapy16 Recent studies have emphasized the importance of tissue handling and standardization of preanalytical variables as these can have dramatic impact on the quality of harvested tissue and therefore on protein expression levels.17, 18, 19, 20, 21, 22, 23 This often requires special attention to tissue handling avoiding modification of protein levels after vessel ligation and removal of the tissue.24
Routinely, specimen samples obtained from biopsies or surgical procedures are examined by pathologists before further processing or formalin fixation.25, 26, 27 However, the current standard methods of measurement on FFPE material may have significant limitations in accuracy. The American Society of Clinical Oncologists and College of American Pathologists has published guidelines for the assessment of estrogen receptor (ER) and progesteron receptor in breast cancer, capping cold ischemic time at 1 h.28 However, these guidelines do not address the assessment of other markers in the research setting. Specifically, these guidelines do not mention phosphoepitopes that have been shown to be altered by delays in time-to-fixation.18, 20
There are relatively few studies or quantitative data about phosphoproteins and how their expression is affected by tissue extraction, preservation methods, processing, and time-to-fixation. The standard practices of ex vivo tissue handling are based on old protocols for tissue formalin fixation, often with no special care to reduce the time-to-fixation.25 The use of these routinely handled samples for assessment of phosphoepitopes may lead to inaccuracy and nonreproducibility.To address this question, we have quantitatively evaluated the expression of a series of phosphoepitopes in paraffin-embedded samples from breast tumors. We seek to determine which phosphoepitopes may be studied on routine tissue and which would require special handling.
MATERIALS AND METHODS
Our study was focused on evaluation of 12 phosphospecific antibodies, which have an important role in cell proliferation pathways as phosphorylated-activated proteins, which are reported to be involved in development of resistance to therapeutic regimens, and might potentially, become companion diagnostic tests for new targeted therapies. The antibodies, clones, their significance for research and clinical setting, and antibody specific heat induced antigen retrieval (HIER) methods are summarized in Table 1.
Patient Cohorts
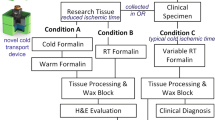
For the assessment of possible changes in protein expression as a function of time to formalin fixation, a cohort of breast cancer cases, was prospectively collected at the Rochester University, School of Medicine in New York. For this cohort preanalytical variables in tissue processing were tightly controlled and documented, with a focus on cold ischemic time. After collection and formalin fixation of the tissue specimens, a tissue microarray (TMA) was constructed to enable high-throughput analysis of various biomarkers. This array consists of FFPE tissues of twofold redundant specimens from 93 breast cancer patients (two histospots per case) with recorded time from surgical resection to immersion of the specimen in formalin. Time to formalin fixation or cold ischemic time of these cases ranges from 25 to 415 min, with 70% of the cases being formalin fixed within 120 min after surgical removal of the tissue (Table 2 and Supplementary Figure 1). All tissue was used after approval from the Institutional Review Boards at both Yale University and University of Rochester. Written informed consent was obtained from all patients for their tissue to be used in research.
Immunohistochemical Staining
Slides were deparaffinized with xylene and rehydrated with ethanol. Antigen retrieval was performed using citrate buffer (pH=6) or Tris EDTA buffer (pH=8), at a temperature of 97 °C for 20 min. After blocking of endogenous peroxidase with methanol and hydroxyl peroxide, slides were preincubated with 0.3% bovine serum albumin in 0.1 mol/l of Tris-buffered saline for 30 min at room temperature. This was followed by incubation of the slides with the primary antibody and cytokeratin over night at 4 °C. Mouse/rabbit EnVision reagent (Dako North America, Inc., Carpinteria, CA, USA; neat) and Alexa 546 conjugated goat anti-rabbit/mouse secondary antibody (Molecular Probes, Eugene, OR, USA 1 to 100) were used as secondary antibodies followed by Cy5-tyramide (Perker Elmer, Life Science, MA, USA). DAPI staining containing 4′6-diamidino-2-phenylindole was used to identify tissue nuclei. All staining was performed using the Lab Vision Autostainer 720 from Thermo Scientific (Waltham, MA, USA).
Antibody Validation
Each antibody was validated using an abbreviated, previously described, protocol.29 In brief, each antibody was titrated on test TMAs, consisting of 40 breast cancer samples. The breast cancer samples represented on the test TMA are formalin fixed and paraffin embedded, and were collected from the Yale Archives (New Haven, CT, USA). Exact processing time for these specimens is not recorded. However, cold ischemic time of routinely processed breast cancer samples does not exceed 1 h, following the ASCO/CAP guidelines. Specificity of staining was determined and an optimal titer for the evaluated antibody was chosen according to an expression range graph, which allows objective assessment of the optimal dynamic range, as well as signal-to-noise ratio of the marker of interest. The optimal dynamic range is calculated as the ratio between the top 10% to the lowest 10% AQUA scores for a given biomarker. Specificity was further determined by immunoblotting and detection of a single band at the right molecular weight. These efforts were followed by staining and QIF analysis of a cell line TMA, containing cell lines used for immunoblotting and correlation of these results with the immunoblot. Reproducibility of the antibody was assessed with AQUA analysis of serial sections of test arrays stained under the same conditions on different days. Assessment of this test TMA with 40 breast cancer samples and of the cell line TMA consisting of breast cancer cell lines allowed us to identify positive and negative surgical specimens and cell lines for the protein of interest. These TMAs served then as positive and negative controls for phosphatase assays and quality control and reproducibility for the following assays. Specificity of the antibodies targeting phosphorylated proteins was evaluated by phosphatase assays. In brief, test TMAs were incubated with Lambda protein phosphatase (New England Biolabs, Danvers, MA, USA) according to the manufacturer’s instructions, followed by regular immunostaining as described above. Positive controls of test TMAs without phosphatase treatment were simultaneously incubated with the given antibody. Phosphorylated antibodies were considered as validated and were used for further measurements only when the phosphatase-treated slides showed a reduction in AQUA score levels at or below the signal-to-noise cutpoint (Supplementary Figure 2).
AQUA Analysis
Protein expression levels were quantified using the AQUA method of quantitative immunofluorescence (QIF) described previously. AQUA allows exact and objective measurement of fluorescence intensity within a defined tissue area, as well as within subcellular compartments.30 Briefly, a series of monochromatic high-resolution images were captured using an epifluorescent microscope platform and signal intensity of the target of interest was measured according to a previously described algorithm. For each TMA histospot, images were obtained for each fluorescence channel, DAPI (nuclei), Alexa 546 (cytokeratin), or Cy5 (target probe). To distinguish tumor from stroma and other parts, an epithelial tumor ‘mask’ was created by dichotomizing the cytokeratin signal and target protein was quantified only in the tumor by dividing the target protein compartment pixel intensities by the area of the compartment within which they were measured.
Statistical Analysis
To assess reproducibility of the assays and correlation of AQUA scores for each marker between corresponding histospots on the TMAs, we used Pearson’s correlation coefficient. On the TMA series, two histospots were measured and averaged. The average sample intensities were then log2-transformed and standardized; the time-to-fixation was also log2-transformed. For each marker, we performed least squares univariate linear regressions and computed the slope and intercept. Confidence intervals (CIs) were computed using bootstrapping; we also computed empirical CIs for a sample consisting of 10 times the number of available observations, also using bootstrapping. This procedure has been previously described.17 Because of missing values, different markers had different numbers of observed pairs of intensity and time-to-fixation measurements.
In detail, separately for each marker, a new sample of size M was constructed by sampling with replacement from the available M measurements, where M was the number of nonmissing specimen histospot measurements of the given marker. Ordinary least squares estimates for the slope and intercept were computed for the bootstrapped sample, together with the predicted values for the entire time-to-fixation domain. The process was repeated 100 000 times. For each time-to-fixation in the range between 0.1 and 7 h, we computed the 95% CI of the estimated log2-transformed standardized intensity. To examine the sample size effect on the 95% CI, we also estimated the 95% CIs for a sample of 10 times the number of nonmissing pairs of intensity and time-to-fixation (10 × M). A 90% CI of the slopes and of the fitted log2-transformed standardized marker intensity was also computed for completeness.
We divided the markers into five categories. A marker was labeled as ‘increase’ when the 95th percentile of the slopes obtained by bootstrapping for n=M was >0. Similarly, a marker was labeled as ‘decrease’ when the 95th percentile of the slopes obtained by bootstrapping for n=M was <0. A marker was labeled as ‘no change’ when the 95% CI for the slope with both n=M and n=10 × M included the zero slope. A marker was labeled as ‘trend up’ or ‘trend down’ when the 95% CI for the slope with n=M included the zero slope, however, the 95% CI for the slope with n=10 × M did not include it. In this situation, it is possible that a larger sample size might have enabled detection of a monotonic relationship between the measured intensities and the time-to-fixation.
Statistical analyses were performed using the R package (www.r-project.org).
RESULTS
Phosphoantibodies commonly used in research settings, were tested for specificity and reproducibility. Out of 17 antibodies tested, 12 antibodies validated according to the above described validation protocol for specificity and reproducibility. These proteins revealed the correct subcellular localization for QIF, the immunoblot showed the correct molecular weight and correlated with QIF analysis of the TMA containing corresponding cell lines. Reproducibility of the antibody was assessed with AQUA analysis of serial sections of test arrays stained under the same conditions on different days. An r2 of 0.75 and above was defined as sufficient antibody reproducibility. Also, the phosphatase experiments showed sufficient reduction of signal for the antibodies. The validated phosphoantibodies and epitopes, and specific staining conditions are summarized in Table 1.
The validated antibodies were subsequently tested on the time-to-fixation array to evaluate possible changes of expression levels, according to increasing cold ischemic time of tissue specimens. After QIF analysis of the proteins on the time-to-fixation cohort, least square univariate regressions were performed for each marker, the slope, intercept, and CI were computed. This procedure was performed for each marker for the number of nonmissing samples and for 10 times the number of available observations, which were computed by bootstrapping and resampling. Although 12 phosphoantibodies validated according to the described protocol and all of these proteins were assessed on the time-to-fixation TMA, we report results on 11 epitopes only. Owing to the limited number of patient samples showing Her2 amplification or an equivocal Her2 status, the number of samples with elevated phospho-Her2 levels was limited too. This cohort collection consists of 93 patient samples, out of which 24 cases are positive for Her2, and only a percentage of those show levels of phospho-Her2 expression above the threshold to noise signal as measured by QIF. The cohort is therefore statistically underpowered to draw conclusions regarding epitope stability of this analyte according to cold ischemic time.
Phosphorylated Proteins Which do not Show Any Change in Antigenicity within the Cold Ischemic Time Tested
Within the time-to-fixation range of the specimens collected, two antibodies, phospho-ER and phospho-Jak2, do not detect any change in antigenicity as a function of time-to-fixation (phospho-ER: P-value 0.3 for n=M and 0.17 for n=10 × M; phospho-Jak2: P=0.61 for n=M; and P=0.11 for n=10 × M ). The 95% CIs of the slopes for M samples, as well as 10 × M samples, where M stands for the number of nonmissing cases, include the zero slope, therefore showing consistent protein expression along the time line recorded here (Figure 1a). Also calculations for 90% CI confirm results for this patient cohort (data not shown).
All validated phosphoantibodies were tested on the time-to-fixation TMA. The average sample intensities and the cold ischemic time were then log2-transformed. Least squares univariate linear regressions were perfomed. Confidence intervals (CIs) were computed using bootstrapping for the number of nonmissing values (n=M) and for 10 times the number of nonmissing values (n=10 × M). (a) Summary of phosphorylated epitopes that do not show any change of expression levels with increasing cold ischemic time, whereas others reveal marked loss of phosphoepitopes as shown in (b). Several markers include the zero slope for the 95% CI for n=M, whereas the zero slope is not included for the 95% CI for n=10 × M suggesting that a bigger sample size might be necessary to reach statistical significance (c). Markers of post-translational modification, such as phospho-S6 and phospho-HSP27 show a significant increase in expression levels with delayed time to formalin fixation (d).
Phosphorylated Proteins that Lose Antigenicity with Increased Cold Ischemic Time
The proteins phospho-Tyrosine 4G10 and phospho-Erk1/2 show dramatic loss of antigenicity within a short period of cold ischemic time as demonstrated in Figure 1b and Table 2 (P<0.0005 for n=M and n=10 × M for phospho-Tyrosin; P=0.053 for n=M and P<0.0005 for n=10 × M for phospho-Erk1/2). There is a trend toward loss of epitope for a number of phosphoproteins tested. These include phospho-AKT 473, phospho-mTor, phospho-Stat3, phospho-SAPK, and phospho-Met. For these proteins the 95% CIs for n=M includes the zero slope whereas the 95% CI for n=10 × M does not include the zero slope, suggesting that these trends may be uncovered by testing larger sample sizes, or longer cold ischemic times (Figure 1c and Table 2). Although loss of antigenicity according to increased time to formalin fixation for these proteins does not reach statistical significance, a negative result in assays with these antibodies should be considered as a potential false-negative one until the antibody is validated for the specific specimen type and fixation times to be used in the routine assay.
Upregulation of Protein Expression as a Response to Increased Cold Ischemic Time
After vessel ligation and removal of the specimen, the tissue is still viable for some period of time, although it rapidly becomes hypoxic. The tissue may show reaction to this stress by upregulation of signaling pathways associated with metabolic stress and hypoxia. In this context, we see an increase in antigenicity of the heat-shock protein phospho-HSP27 (P=0.058 for n=M and P<0.0005 for n=10 × M) and a trend towards elevated levels of the ribosomal protein phospho-S6 (P=0.36 for n=M and P=0.0042 for n=10 × M) as demonstrated in Figure 1c and Table 2. Eventually, we would expect these increases to plateau and ultimately decrease, but in the relatively short cold ischemic time examined in this study, these markers show a measurable positive change.
DISCUSSION
The study described here is an assessment of the effect of time-to-fixation on the expression of several signaling transduction phosphoproteins in breast cancer specimens using the method of QIF. However, beyond time-to-fixation, there are many other variables that can alter tissue quality and should be considered in assessment of biomarkers using antibody probes. This list includes the origin of the excised organ or tissue, surgical practices including anesthetic, pathology practices for tissue preservation and handling, classes of signal pathway proteins under analysis, and many other unknown factors with confounding impact in molecular analysis and immunohistochemistry (IHC). Moreover these problems may be confounded by inaccurate measurement. Conventional IHC is not a quantitative method and thus sometimes obscures differences in expression levels caused by preanalytic variables.31, 32, 33 In this study, we use QIF to provide a reliable, reproducible and reader-independent method of quantification of analytes in efforts to more precisely define the specific effects of cold ischemic time. To focus on cold ischemic time, the design of this study, using a prospectively collected patient cohort with recorded cold ischemic time, provided additional reliability for these measurements. However, even with these focused efforts, we are unable to exclude the effects of other preanalytic variables on phosphoepitope stability and encourage assay development teams to consider all preanalytic variables in their assay design.
The results of our analysis show a statistically significant loss and a clear trend of loss of epitopes with increasing time-to-fixation for the majority of the phosphoproteins tested. These results of loss of phosphoepitopes are consistent with some of the previous studies testing stability of phosphorylated proteins in cancer tissues. Baker et al12 assessed the expression of phospho-Ser473-AKT by IHC on a series of paired biopsies and resections reporting significant decrease of the phosphoprotein levels in tumor resections compared with biopsies. This group suggests that post-excisional dephosphorylation of proteins might occur in tissue specimens over time before formalin fixation. Bai et al20 reported previously a significant loss of the phosphoproteins phospho-Erk, phospho-Akt, and phospho-S6K1 on tissue resections on a retrospectively collected series of breast cancer cohorts of paired core needle biopsies and tumor resections. Pinhel et al18 reported similar results for phopho-ERK and phospho-AKT. These and similar studies enhance the speculation that there is an important dephosphorylation of proteins in surgical specimens as a result of endogenous tumor phosphatase activity related to delayed fixation. Phosphoepitopes on tissue specimens of routine surgical resections are likely to have undergone changes of post-translational modification and might not reflect the in vivo status of the tumor.19
Interestingly, we report an increase in epitope levels of phospho-HSP27, a small heat-shock induced protein and apoptosis modulator, as a function of prolonged cold ischemic time. It is believed that this protein in the phosphorylated form has a role in increasing cell survival in stress situations and is upregulated in breast and other cancers.34, 35, 36 Espina et al19 have previously provided evidence about the post-excisional reactivity and dynamic state of tissues and the major molecular events and adoptive cellular mechanisms in response to stress, hypoxia, and other environmental factors.This result was also consistent with the previous study from our team showing that some proteins that are expressed in response to hypoxia, presented increased expression with increased time-to-fixation.17
We did not observe any change in expression levels of phospho-ER that are potentially valuable as a companion diagnostic test for breast cancer specimens. It has been shown that phospho-HER2 is seen in only a subset of HER2 amplified breast cancers and there is some data suggesting that it is a prognostic factor.37 However, only a small subset of patients in our cohort is HER2 amplified and an even smaller subset shows high expression of phospho-HER2. Thus interpretation of these results is limited owing to a very small sample size of the population. Therefore this variable has been omitted from consideration in this series.
Another limitation of our study is that the assessment of the phosphoepitopes was performed with one epitope specific antibody for each protein, respectively one polyclonal antibody. The results reported here are therefore only applicable to the specific antibody, which was investigated. Although we evaluated antibodies most commonly used in research settings and validated them rigorously, we are unable to generalize our findings of loss of epitope expression to overall biomarker stability, but rather describe the influence of cold ischemic time on the specific epitopes tested here. Furthermore our study was performed on a single cohort. However, similar trends of loss of phosphoepitopes have been reported previously,18, 20 None the less, validation on another cohort could strengthen these results. Also, the trends seen here may become statistically stronger with larger sample sizes and other patient cohorts. Finally, another weakness of this work consists of the fact that analysis was performed on breast cancer tissue only. Different tumor types may show different reactions to preanalytic variables as a function of the variable cellular composition of different specimens.38, 39, 40
To our knowledge, this study is the first to show quantitative assessment and reporting on a series of different phosphoepitopes that might be altered through preanalytical variables. This study and others suggest future work that is specific to other tumor types and other preanalytic variables to help guide protocols for future companion diagnostic tests. We hope to see the evidence produced here and by other investigators to help establish guidelines for immunohistochemisty with respect to preanalytic variables.
References
Ludwig JA, Weinstein JN . Biomarkers in cancer staging, prognosis and treatment selection. Nat Rev Cancer 2005;5:845–856.
Lamparella N, Barochia A, Almokadem S . Impact of genetic markers on treatment of non-small cell lung cancer. Adv Exp Med Biol 2013;779:145–164.
Rossi A, Torri V, Garassino MC et al. The impact of personalized medicine on survival: Comparisons of results in metastatic breast, colorectal and non-small-cell lung cancers. Cancer Treat Rev 2013;40:485–494.
Ogino S, Lochhead P, Giovannucci E et al. Discovery of colorectal cancer PIK3CA mutation as potential predictive biomarker: power and promise of molecular pathological epidemiology. Oncogene 2013;33:2949–2955.
Hunter T . A thousand and one protein kinases. Cell 1987;50:823–829.
Araujo RP, Liotta LA, Petricoin EF . Proteins, drug targets and the mechanisms they control: the simple truth about complex networks. Nat Rev Drug Discov 2007;6:871–880.
Collins MO, Yu L, Choudhary JS . Analysis of protein phosphorylation on a proteome-scale. Proteomics 2007;7:2751–2768.
Petricoin EF 3rd, Bichsel VE, Calvert VS et al. Mapping molecular networks using proteomics: a vision for patient-tailored combination therapy. J Clin Oncol 2005;23:3614–3621.
Schmelzle K, White FM . Phosphoproteomic approaches to elucidate cellular signaling networks. Curr Opin Biotech 2006;17:406–414.
Gulmann C, Espina V, Petricoin E 3rd et al. Proteomic analysis of apoptotic pathways reveals prognostic factors in follicular lymphoma. Clin Cancer Res 2005;11:5847–5855.
Haab BB . Antibody arrays in cancer research. Mol Cell Proteomics 2005;4:377–383.
Baker AF, Dragovich T, Ihle NT et al. Stability of phosphoprotein as a biological marker of tumor signaling. Clin Cancer Res. 2005;11:4338–4340.
Khan IH, Mendoza S, Rhyne P et al. Multiplex analysis of intracellular signaling pathways in lymphoid cells by microbead suspension arrays. Mol Cell Proteomics 2006;5:758–768.
De Marzo AM, Fedor HH, Gage WR et al. Inadequate formalin fixation decreases reliability of p27 immunohistochemical staining: probing optimal fixation time using high-density tissue microarrays. Hum Pathol 2002;33:756–760.
Beelen K, Opdam M, Severson TM et al. Phosphorylated p-70S6K predicts tamoxifen resistance in postmenopausal breast cancer patients randomized between adjuvant tamoxifen versus no systemic treatment. Breast Cancer Res 2014;16:R6.
Kim EK, Kim JH, Kim HA et al. Phosphorylated S6 kinase-1: a breast cancer marker predicting resistance to neoadjuvant chemotherapy. Anticancer Res 2013;33:4073–4079.
Neumeister VM, Anagnostou V, Siddiqui S et al. Quantitative assessment of effect of preanalytic cold ischemic time on protein expression in breast cancer tissues. J Natl Cancer Inst 2012;104:1815–1824.
Pinhel IF, Macneill FA, Hills MJ et al. Extreme loss of immunoreactive p-Akt and p-Erk1/2 during routine fixation of primary breast cancer. Breast Cancer Res 2010;12:R76.
Espina V, Edmiston KH, Heiby M et al. A portrait of tissue phosphoprotein stability in the clinical tissue procurement process. Mol Cell Proteomics 2008;7:1998–2018.
Bai Y, Tolles J, Cheng H et al. Quantitative assessment shows loss of antigenic epitopes as a function of pre-analytic variables. Lab Invest 2011;91:1253–1261.
Yildiz-Aktas IZ, Dabbs DJ, Bhargava R . The effect of cold ischemic time on the immunohistochemical evaluation of estrogen receptor, progesterone receptor, and HER2 expression in invasive breast carcinoma. Mod Pathol 2012;25:1098–1105.
De Cecco L, Musella V, Veneroni S et al. Impact of biospecimens handling on biomarker research in breast cancer. BMC Cancer 2009;9:409.
Apple S, Pucci R, Lowe AC et al. The effect of delay in fixation, different fixatives, and duration of fixation in estrogen and progesterone receptor results in breast carcinoma. Am J Clin Pathol 2011;135:592–598.
Hunter T . Protein-tyrosine phosphatases: the other side of the coin. Cell 1989;58:1013–1016.
Titford ME, Horenstein MG . Histomorphologic assessment of formalin substitute fixatives for diagnostic surgical pathology. Arch Pathol Lab Med 2005;129:502–506.
Lehmann U, Kreipe H . Real-time PCR analysis of DNA and RNA extracted from formalin-fixed and paraffin-embedded biopsies. Methods 2001;25:409–418.
Belloni B, Lambertini C, Nuciforo P et al. Will PAXgene substitute formalin? A morphological and molecular comparative study using a new fixative system. J Clin Pathol 2013;66:124–135.
Hammond ME, Hayes DF, Dowsett M et al. American Society of Clinical Oncology/College of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer (unabridged version). Arch Pathol Lab Med 2010;134:e48–e72.
Bordeaux J, Welsh A, Agarwal S et al. Antibody validation. Biotechniques 2010;48:197–209.
Camp RL, Chung GG, Rimm DL . Automated subcellular localization and quantification of protein expression in tissue microarrays. Nat Med 2002;8:1323–1327.
Moeder CB, Giltnane JM, Moulis SP et al. Quantitative, fluorescence-based in-situ assessment of protein expression. Methods Mol Biol 2009;520:163–175.
Giltnane JM, Molinaro A, Cheng H et al. Comparison of quantitative immunofluorescence with conventional methods for HER2/neu testing with respect to response to trastuzumab therapy in metastatic breast cancer. Arch Pathol Lab Med 2008;132:1635–1647.
Bamias A, Yu Z, Weinberger PM et al. Automated quantitative analysis of DCC tumor suppressor protein in ovarian cancer tissue microarray shows association with beta-catenin levels and outcome in patients with epithelial ovarian cancer. Ann Oncol 2006;17:1797–1802.
Huot J, Roy G, Lambert H et al. Increased survival after treatments with anticancer agents of Chinese hamster cells expressing the human Mr 27,000 heat shock protein. Cancer Res 1991;51:5245–5252.
Conroy SE, Latchman DS . Do heat shock proteins have a role in breast cancer? Brit J Cancer 1996;74:717–721.
Casado P, Zuazua-Villar P, del Valle E et al. Vincristine regulates the phosphorylation of the antiapoptotic protein HSP27 in breast cancer cells. Cancer Lett 2007;247:273–282.
Thor AD, Liu S, Edgerton S et al. Activation (tyrosine phosphorylation) of ErbB-2 (HER-2/neu): a study of incidence and correlation with outcome in breast cancer. J Clin Oncol 2000;18:3230–3239.
Davis BW, Zava DT, Locher GW et al. Receptor heterogeneity of human breast cancer as measured by multiple intratumoral assays of estrogen and progesterone receptor. Eur J Cancer Clin Oncol 1984;20:375–382.
Douglas-Jones AG, Collett N, Morgan JM et al. Comparison of core oestrogen receptor (ER) assay with excised tumour: intratumoral distribution of ER in breast carcinoma. J Clin Pathol 2001;54:951–955.
Sapino A, Marchio C, Senetta R et al. Routine assessment of prognostic factors in breast cancer using a multicore tissue microarray procedure. Virchows Arch 2006;449:288–296.
Acknowledgements
We thank Ms Lori Charette and her team at Yale Pathology Tissue Services for TMA construction and tissue sectioning. This project has been funded in whole or in part with federal funds from the National Cancer Institute, National Institutes of Health, under Contract No. HHSN261200800001E. Also this work was supported by Ricerca Sanitaria Finalizzata RF-2010-2310674.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
A tissue microarray of breast cancer specimens was used to evaluate changes in antigenicity of 12 phospho-epitopes frequently used in research settings as a function of cold ischemic time. The majority of the epitopes revealed changes in expression levels with increasing time to formalin fixation. Therefore, specimen collection should be closely subjected to quality control measures to ensure accurate measurement of these epitopes.
Rights and permissions
About this article
Cite this article
Vassilakopoulou, M., Parisi, F., Siddiqui, S. et al. Preanalytical variables and phosphoepitope expression in FFPE tissue: quantitative epitope assessment after variable cold ischemic time. Lab Invest 95, 334–341 (2015). https://doi.org/10.1038/labinvest.2014.139
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2014.139
This article is cited by
-
Qualifying antibodies for image-based immune profiling and multiplexed tissue imaging
Nature Protocols (2019)
-
Impact of delayed and prolonged fixation on the evaluation of immunohistochemical staining on lung carcinoma resection specimen
Virchows Archiv (2019)
-
Comparison of protein expression between formalin-fixed core-cut biopsies and surgical excision specimens using a novel multiplex approach
Breast Cancer Research and Treatment (2019)
-
Tumor Pre-Analytics in Molecular Pathology: Impact on Protein Expression and Analysis
Current Pathobiology Reports (2018)
-
Molecular Pathology and Pre-Analytic Variables: Impact on Clinical Practice From a Breast Pathology Perspective
Current Pathobiology Reports (2018)