Abstract
Objective:
To evaluate Decisional Conflict and Regret among parents regarding the decision on initiating comfort or active care in extreme prematurity and to relate these to decision-making characteristics.
Study Design:
A nationwide, multicenter, cross-sectional study using an online survey in the Netherlands. Data were collected from March 2015 to March 2016 among all parents with infants born at 24+0/7–24+6/7 weeks gestational age in 2010–2013. The survey contained a Decisional Conflict and Decision Regret Scale (potential scores range from 0 to 100) and decision-making characteristics.
Results:
Sixty-one surveys were returned (response rate 27%). The median Decisional Conflict score was 28. From the subscores within Decisional Conflict, ‘values clarity’ revealed the highest median score of 42—revealing that parents felt unclear about personal values for benefits and risks of the decision on either comfort care or active care. The median Decision Regret score was 0. Regret scores were influenced by the actual decision made and by outcome: Decision Regret was lower in the active care group and in the survivor group.
Conclusion:
We found little Decisional Conflict and no Decision Regret among parents regarding decision-making at 24 weeks gestation.
Similar content being viewed by others
Introduction
When an extreme premature birth is imminent, (non)treatment decisions have to be made. There is a gray zone in which resuscitation is discretionary. This zone starts at 22 or 23 weeks and runs up to 24 or 25 weeks gestation—regional differences have been described.1, 2, 3, 4, 5, 6, 7, 8 Within this gray zone, shared decision-making is the preferred decision model2, 9, 10 and thus parental involvement is necessary.
Professionals’ concerns exist on the burden that decision-making may put on parents,11, 12 but it is shown that parents themselves do want to participate.13, 14 Parental involvement in neonatal end-of-life decisions (evaluated 3 or 13 months after the death of the baby) was rarely considered to be too burdensome.14 Furthermore, the perception of a shared decision is associated (in the long term) with lower grief scores compared with informed or paternalistic decision-making.15 Kaempf et al.9 found hardly any significant concern among parents using their counseling framework in extreme prematurity. Besides that, there is little information about the psychological consequences of parental decisions in the neonatal intensive care unit; information on long-term impact (for example, stress, regret, impact on families) on parents is needed.12 It is acknowledged that making treatment decisions can exert a substantial negative emotional effect on surrogates,16 though this is not specifically researched for prenatal decision-making in extreme prematurity. No data on Decisional Conflict or Regret among parents exist, but it is known that Decisional Conflict and uncertainty in decision-making is greater when persons feel uninformed about the options, are unclear about personal values or feel unsupported in deciding.17 Parents have described exactly these circumstances in decision making in extreme prematurity.13, 18, 19, 20 Since 2010, the Dutch guideline on perinatal practice in extreme prematurity has lowered the limit of viability from 25+0/7 to 24+0/7 weeks gestational age (GA) and requires parental informed consent for active treatment.21
Therefore, we aimed to evaluate Decisional Conflict and Regret in extreme prematurity regarding initiating comfort or active care and to relate these to decision-making characteristics (participation in the decision, which decision was made, outcome).
Methods
Study design
A nationwide, multicenter, cross-sectional study using a survey among parents with infants born at 24+0/7–24+6/7 weeks GA.
Setting
This survey is part of the Dutch PreCo study evaluating care and counseling in extreme prematurity (clinicaltrials.gov, NCT02782650 and NCT02782637) with the ultimate goal of developing a framework to support prenatal counseling in extreme prematurity. We conducted this nationwide PreCo parents’ survey in all 10 Dutch perinatal care centers. The study protocol was approved by the central institutional review board (IRB) and confirmed by local boards.
Study population
Medical databases were used to identify infants born at 24+0/7–24+6/7 weeks GA in the first 3 years after introduction of the new Dutch guideline (2010 October to 2013 September). The only exclusion criterion was active termination of pregnancy. There was no standard approach to prenatal counseling. All eligible parents of these infants received an introductory letter through clinicians of the hospital of birth. A closed envelope was accompanying this letter, containing comprehensive patient information, informed consent forms and a return envelope—subjects could choose whether they wanted to open it. This adapted form of ‘opt-in’ recruitment strategy was agreed upon with the IRB. Informed consent was returned to the lead investigator who was also available to subjects to answer questions at any stage. After informed consent, a written survey or web-link (as preferred) was sent to parents. Data were collected from March 2015 to March 2016, so at least 1.5 years and up to 5.5 years after birth of their infant. No reminders were sent on explicit decision of the IRB.
Survey design and data collection
The PreCo parents’ survey addressed both parents’ experiences on prenatal counseling and on decision-making in extreme prematurity. This study concerns the results of the decision-making part, regarding the decision on initiating active care or comfort care. We were particularly interested in the Decisional Conflict and Decision Regret of parents and wanted to relate these to (perceived) characteristics of the decision-making. These decision-making characteristics were: who made the decision (parents/joint decision parents decisive/joint decision equally decisive/joint decision doctor decisive/doctor), whether parents felt they had a choice (yes/no), the actual decision made (comfort care/active care/other), outcome of their baby (survival/death), and self-reported child morbidity (minor, -/major, -/severe physical or intellectual disabilities). The original validated Decisional Conflict Scale (DCS)17, 22 (version: statement format) and Decision Regret Scale (DRS)23, 24 were translated into Dutch and adapted to the decision-making in the situation in extreme prematurity.25 Subsequently, the project team members reviewed the questionnaire as well as the members of the Dutch patient support group (Vereniging Ouders van Couveusekinderen). Furthermore, input from the IRB was used for further improvement. Our adapted DCS consisted of 15 items, versus 16 items in the original scale; the question: ‘I expect to stick with my decision’ was not included owing to the nature of this decision and the timing of the survey. Parents were instructed to remember how they felt at the time of decision-making while filling out the DCS and statements were written in past tense. Our adapted DRS consisted of five items, identical to the original scale. Cronbach’s alpha was calculated for our DCS and DRS (for the original validated DCS a Cronbach’s alpha of >0.78 was reported,17 and for the DRS 0.81–0.9223). The DRS was presented to all participants but at explicit request of the patient support group the DCS only to the parents who felt that they had a choice in decision-making.
Data analysis
Summary statistics were calculated as frequencies and proportions of the respondents for that specific question. Conforming to the user manuals, item scores on the DCS and DRS were first mirrored when applicable and thereafter summed to reach a sum score, which ranged from 0 to 100 on both scales; 0 meaning low conflict or regret. A DCS score <25 is associated with implementing decisions and scores >37.5 are associated with decision delay or feeling unsure about implementation,17 for DRS no formal cutoff score exists, but others considered 0 as no regret, 1–25 mild regret and >25 moderate-to-strong regret.26 For analysis of reliability of the adapted DCS and DRS scale, Cronbach’s alphas were calculated. To compare scores between groups based on decision-making characteristics, Mann–Whitney U (2 groups) or Kruskal–Wallis (>2 groups) were used. Exact P-values were provided, and values <0.05 were considered statistically significant. Statistical analyses were conducted using IBM SPSS Statistics (Version 20.0. Armonk, NY, USA: IBM Corp).
Results
Out of the 229 approached parent(s), 67 gave informed consent, and 61 surveys were returned (response rate 27%). Backgrounds of the participants are presented in Table 1. Of the participants, 84% opted for active treatment, 9% for comfort care and 7% for ‘other’. In the last group, the plan could be described as a ‘wait-and-see’ approach or the plan was unclear. The decision-making information shows that 80% felt that they had a choice in deciding whether to initiate care or not. According to the parents, most decisions were made together by the doctor and parents (62%).
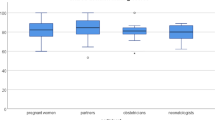
Figures 1 shows the DCS. Median DCS was 28 (interquartile range 17–35), with a Cronbach’s alpha of 0.86. When DCS scores between different groups were compared based on ‘who made the decision’, ‘actual decision made’, ‘outcome’ and ‘morbidity’, no significant differences were found (P=0.60, P=0.09, P=0.29 and P=0.12, respectively). The median scores for the subscales within the Decisional Conflict Scale were as follows: uncertainty 33, informed 17, values clarity 42, support 17, and effective decision 17.
Figure 2 shows the DRS. Median DRS was 0 (interquartile range 0–15), with a Cronbach’s alpha of 0.79. When DRS scores between different groups were compared based on ‘who made the decision’, ‘whether parents felt they had a choice’ and ‘morbidity’, no significant differences were found (P=0.54, P=0.30 and P=0.052, respectively). When comparing DRS between the different ‘actual decision made’, there was a significant difference (P=0.004): a median DRS of 0 in the active care group, 5 in the comfort care group, and 30 in the group ‘other’. Significant differences also existed based on ‘outcome’ (P=0.025): a median DRS of 0 in the survivor group, 7.5 in the deceased despite active care group, and 10 in the group ‘both’.
Discussion
Prenatal decisions on initiating care in extreme prematurity have a major impact on parents. In this Dutch study, parents retrospectively reported having relatively little Decisional Conflict and even lower Decision Regret regarding the decision to initiate active care at 240/7–24+6/7 weeks GA. At this age, active care is discretionary in the Netherlands. We are aware of the regional differences in both lower and upper limits of gestation in which both active and comfort care are optional, but a zone in which parents will be involved in this decision-making exists almost everywhere. In our study, scores were not dependent on who had made the decision (for DRS and DCS) and on whether parents felt they had a choice (for DRS only). Decision Regret may be influenced by both the actual decision made (active care versus comfort care versus ‘other’) and the outcome (survival when decided active care). A median Decisional Conflict score of 28 in our sample indicates a low ‘state of uncertainty about a course of action’ regarding the decision on initiating active care at 24 weeks GA.17 The degree of Decisional Conflict appears to be partly inherent to the type of decision that is unmodifiable. However, some factors that influence the degree of Decisional Conflict can potentially be modified. Uncertainty appears to be greater when a person (1) feels uninformed about the alternatives, benefits and risks, (2) is unclear about personal values and (3) feels unsupported in making a choice or feels pressured to choose on course of action.17 As the subscore value clarity was highest, the second situation seems to occur. Decisional Conflict can be lowered with information and support. Shared decision-making, using the steps as described by Stiggelbout et al.,27 and decision-supporting interventions, such as decision-aids,28 can be helpful. In this situation, these may help bringing out personal values. Caeymaex et al.15 supports shared decision-making also in the long term, describing lower grief in decisions to forego life-sustaining treatment when parents had the perception of a shared decision. Decision-aids have already been studied and considered useful for prenatal decisions in extreme prematurity.29, 30
In this sample, participants had low Decision Regret.31 It has been suggested before that individuals bring well-articulated preexisting preferences to prenatal decisions on initiating care.32 This could be an explanation for the low Decision Regret: the decisions might have matched personal values. We think that coping style might also have an influence; it might be easier to to live with the decision when there is no regret.
Though the absolute numbers are low, higher Decision Regret scores seemed to exist when no clear decision (comfort care versus active care) could be defined: two participants described their situation as a ‘wait-and-see’ approach, one baby died antenatal before a decision was made, and in the fourth situation the decision was unclear to the participant. It is known that a wait-and-see approach is outdated and it is recommended that decisions regarding resuscitation are well communicated and agreed upon before birth and should not be conditional on the newborns’ appearance at birth.2, 33, 34 Furthermore, the outcome has an influence on regret: survival when active care was chosen was associated with no regret, and although within the same category of no-to-mild regret, scores were a little higher when an infant has died. It is known that serious adverse physical health outcomes are associated with higher decisional regret.31
This is, to the best of our knowledge, the first data on Decisional Conflict and Regret in prenatal decisions on initiating care in extreme prematurity, providing valuable knowledge on the impact of these decisions on parents. A unique nationwide cohort is used and our adapted DCS and DRS have acceptable Cronbach’s alpha values. Its limitations are the sample size and response rate. The sample is potentially underpowered to exclude influence of the non-significant decision-making characteristics on Decisional Conflict and Regret. Permission to send out reminders would potentially have improved the response rate. Also, a selection bias cannot be ruled out. As the questionnaire was not allowed to contain identifying information and could not be linked to the medical file, we unfortunately do not have data to systematically compare responders versus non-responders. However, we do have information on some aspects. First, we did an additional analysis to compare socio-economic status based on postal area codes between responders and non-responders; this showed no significant differences in socio-economic status between these groups (data not shown). Second, a Dutch cohort (infants of 24 weeks of gestation from the first year after initiation of the guideline) has been described and showed that in 92% active care and in 8% comfort care was chosen35—comparable to our sample, suggesting that an overrepresentation of comfort care in the non-responders is unlikely. The national sample makes it uncertain to what extent these results can be generalized to an international population, although a GA zone where parents are involved in decision-making exists everywhere even though the upper and lower limits might differ. Furthermore, the DCS was retrospectively collected and not collected from all participants. Owing to ethical considerations in study design and the low prevalence of these decisions, larger cohorts might be hard to compose.
Conclusion
Our study reports that parents confronted with decision-making in extreme prematurity have little Decisional Conflict and even lower Decision Regret regarding the decision on initiating care in extreme prematurity. Regret scores were influenced by the actual decision made and by outcome. Professionals should be aware of this in prenatal counseling and may pay extra attention to their role in supporting the parents to clarify their personal values regarding the decision on initiating active versus comfort care.
Change history
23 August 2017
Correction to: Journal of Perinatology advance online publication, 15 June 2017; doi:10.1038/jp.2017.90 In the ‘Decision-making information’ section of Table 1, the n values for ‘Joint decision parent(s) and doctor, parental opinion decisive’ should be 12/54, not 13/54, and the percentage is therefore 22 instead of 23.
References
Guillen U, Weiss EM, Munson D, Maton P, Jefferies A, Norman M et al. Guidelines for the Management of Extremely Premature Deliveries: a systematic review. Pediatrics 2015; 136 (2): 343–350.
Cummings J, Committee on Fetus and Newborn. Antenatal counseling regarding resuscitation and intensive care before 25 weeks of gestation. Pediatrics 2015; 136: 588–95.
Gallagher K, Martin J, Keller M, Marlow N . European variation in decision-making and parental involvement during preterm birth. Arch Dis Child Fetal Neonatal Ed 2014; 99 (3): F245–F249.
Pignotti MS, Donzelli G . Perinatal care at the threshold of viability: an international comparison of practical guidelines for the treatment of extremely preterm births. Pediatrics 2008; 121 (1): e193–e198.
Geurtzen R, Draaisma J, Hermens R, Scheepers H, Woiski M, van Heijst A et al. Perinatal practice in extreme premature delivery: variation in Dutch physicians' preferences despite guideline. Eur J Pediatr 2016; 175: 1039–1046.
Condie J, Caldarelli L, Tarr L, Gray C, Rodriquez T, Lantos J et al. Have the boundaries of the 'grey zone' of perinatal resuscitation changed for extremely preterm infants over 20 years? Acta Paediatr 2013; 102 (3): 258–262.
Tucker Edmonds B, McKenzie F, Farrow V, Raglan G, Schulkin J . A national survey of obstetricians' attitudes toward and practice of periviable intervention. J Perinatol 2015; 35 (5): 338–343.
Mehrotra A, Lagatta J, Simpson P, Kim UO, Nugent M, Basir MA . Variations among US hospitals in counseling practices regarding prematurely born infants. J Perinatol 2013; 33 (7): 509–513.
Kaempf JW, Tomlinson MW, Tuohey J . Extremely premature birth and the choice of neonatal intensive care versus palliative comfort care: an 18-year single-center experience. J Perinatol 2016; 36 (3): 190–195.
Lemyre B, Daboval T, Dunn S, Kekewich M, Jones G, Wang D et al. Shared decision making for infants born at the threshold of viability: a prognosis-based guideline. J Perinatol 2016; 36 (7): 503–509.
Haward MF, Kirshenbaum NW, Campbell DE . Care at the edge of viability: medical and ethical issues. Clin Perinatol 2011; 38 (3): 471–492.
Lantos JD . International and cross-cultural dimensions of treatment decisions for neonates. Semin Fetal Neonatal Med 2015; 20: 368–372.
Boss RD, Hutton N, Sulpar LJ, West AM, Donohue PK . Values parents apply to decision-making regarding delivery room resuscitation for high-risk newborns. Pediatrics 2008; 122 (3): 583–589.
McHaffie HE, Lyon AJ, Hume R . Deciding on treatment limitation for neonates: the parents' perspective. Eur J Pediatr 2001; 160 (6): 339–344.
Caeymaex L, Jousselme C, Vasilescu C, Danan C, Falissard B, Bourrat MM et al. Perceived role in end-of-life decision making in the NICU affects long-term parental grief response. Arch Dis Child Fetal Neonatal Ed 2013; 98 (1): F26–F31.
Wendler D, Rid A . Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med 2011; 154 (5): 336–346.
O'Connor A . User Manual - Decisional Conflict Scale (16 Item Statement Format). Ottawa Hospital Research Institute: Ottawa, Canada, 1993 (updated 2010): 16.
Keenan HT, Doron MW, Seyda BA . Comparison of mothers' and counselors' perceptions of predelivery counseling for extremely premature infants. Pediatrics 2005; 116 (1): 104–111.
Grobman WA, Kavanaugh K, Moro T, DeRegnier RA, Savage T . Providing advice to parents for women at acutely high risk of periviable delivery. Obstet Gynecol 2010; 115 (5): 904–909.
Geurtzen R, Hogeveen M, Rajani AK, Chitkara R, Antonius T, van Heijst A et al. Using simulation to study difficult clinical issues: prenatal counseling at the threshold of viability across American and Dutch cultures. Simul Healthc 2014; 9 (3): 167–173.
de Laat MW, Wiegerinck MM, Walther FJ, Boluyt N, Mol BW, van der Post JA et al. [Practice guideline 'Perinatal management of extremely preterm delivery']. Ned Tijdschr Geneeskd 2010; 154: A2701.
O'Connor AM . Validation of a decisional conflict scale. Med Decis Mak 1995; 15 (1): 25–30.
O'Connor A . User Manual - Decision Regret Scale. Ottawa Hospital Research Institute: Ottawa, Canada, 1996 (modified 2003).
Brehaut JC, O'Connor AM, Wood TJ, Hack TF, Siminoff L, Gordon E et al. Validation of a decision regret scale. Med Decis Mak 2003; 23 (4): 281–292.
Garvelink MM, ter Kuile MM, Stiggelbout AM, de Vries M . Values clarification in a decision aid about fertility preservation: does it add to information provision? BMC Med Inform Decis Mak 2014; 14: 68.
Hong P, Gorodzinsky AY, Taylor BA, Chorney JM . Parental decision making in pediatric otoplasty: The role of shared decision making in parental decisional conflict and decisional regret. Laryngoscope 2016; 126 (Suppl 5): S5–S13.
Stiggelbout AM, Pieterse AH, De Haes JC . Shared decision making: concepts, evidence, and practice. Patient Educ Couns 2015; 98 (10): 1172–1179.
Stacey D, Legare F, Col NF, Bennett CL, Barry MJ, Eden KB et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2014; 1: CD001431.
Kakkilaya V, Groome LJ, Platt D, Kurepa D, Pramanik A, Caldito G et al. Use of a visual aid to improve counseling at the threshold of viability. Pediatrics 2011; 128 (6): e1511–e1519.
Guillen U, Suh S, Munson D, Posencheg M, Truitt E, Zupancic JA et al. Development and pretesting of a decision-aid to use when counseling parents facing imminent extreme premature delivery. J Pediatr 2012; 160 (3): 382–387.
Becerra Perez MM, Menear M, Brehaut JC, Legare F . Extent and predictors of decision regret about health care decisions: a systematic review. Med Decis Making 2016; 36: 777–790.
Haward MF, John LK, Lorenz JM, Fischhoff B . Effects of description of options on parental perinatal decision-making. Pediatrics 2012; 129 (5): 891–902.
Manley BJ, Dawson JA, Kamlin CO, Donath SM, Morley CJ, Davis PG . Clinical assessment of extremely premature infants in the delivery room is a poor predictor of survival. Pediatrics 2010; 125 (3): e559–e564.
Singh J, Fanaroff J, Andrews B, Caldarelli L, Lagatta J, Plesha-Troyke S et al. Resuscitation in the "gray zone" of viability: determining physician preferences and predicting infant outcomes. Pediatrics 2007; 120 (3): 519–526.
de Kluiver E, Offringa M, Walther FJ, Duvekot JJ, de Laat MWM et al, Implementatiegroep Richtlijn Extreem Prematuren. Perinatal policy in cases of extreme prematurity; an investigation into the implementation of the guidelines. Perinataal beleid bij extreme vroeggeboorte; een onderzoek naar de implementatie van de richtlijn. Ned Tijdschr Geneeskd 2013; 157 (38): A6362.
Acknowledgements
We thank all participating parents. Furthermore, special thanks to B Wissink, a medical student who helped set up this study. Also special thanks to the local obstetrical and neonatal investigators: AH van Kaam (neonatology, AMC), M de Laat (obstetrics, AMC currently: Australia), JF Koper (neonatology UMCG), L Duin (obstetrics UMCG), M van der Hoeven (neonatology MUMC+), R Kornelisse (neonatology, ErasmusMC), JJ Duvekot (obstetrics, ErasmusMC), S Bambang Oetomo (neonatology, MMC), P van Runnard Heimel (obstetrics, MMC), HN Lafeber (neonatology, VU), C Bax (obstetrics, VU), M van der Heide Jalving (neonatology, UMCU), M Bekker (obstetrics UMCU), SM Mulder (neonatology, Isala), J v Eyck (obstetrics, Isala), E Lopriore (neonatology, LUMC), and KWM Bloemenkamp (obstetrics, LUMC, currently UMCU).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Geurtzen, R., Draaisma, J., Hermens, R. et al. Prenatal (non)treatment decisions in extreme prematurity: evaluation of Decisional Conflict and Regret among parents. J Perinatol 37, 999–1002 (2017). https://doi.org/10.1038/jp.2017.90
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2017.90
This article is cited by
-
Decision-making in imminent extreme premature births: perceived shared decision-making, parental decisional conflict and decision regret
Journal of Perinatology (2021)
-
Preferred prenatal counselling at the limits of viability: a survey among Dutch perinatal professionals
BMC Pregnancy and Childbirth (2018)