Abstract
Exposure to forest fire smoke (FFS) is associated with multiple adverse health effects, mostly respiratory. Findings for cardiovascular effects have been inconsistent, possibly related to the limitations of conventional methods to assess FFS exposure. In previous work, we developed an empirical model to estimate smoke-related fine particulate matter (PM2.5) for all populated areas in British Columbia (BC), Canada. Here, we evaluate the utility of our model by comparing epidemiologic associations between modeled and measured PM2.5. For each local health area (LHA), we used Poisson regression to estimate the effects of PM2.5 estimates and measurements on counts of medication dispensations and outpatient physician visits. We then used meta-regression to estimate the overall effects. A 10 μg/m3 increase in modeled PM2.5 was associated with increased sabutamol dispensations (RR=1.04, 95% CI 1.03–1.06), and physician visits for asthma (1.06, 1.04–1.08), COPD (1.02, 1.00–1.03), lower respiratory infections (1.03, 1.00–1.05), and otitis media (1.05, 1.03–1.07), all comparable to measured PM2.5. Effects on cardiovascular outcomes were only significant using model estimates in all LHAs during extreme fire days. This suggests that the exposure model is a promising tool for increasing the power of epidemiologic studies to detect the health effects of FFS via improved spatial coverage and resolution.
Similar content being viewed by others
INTRODUCTION
Forest fires are increasing in frequency and intensity as the global climate changes,1 and they can be responsible for periods of extremely poor air quality. Exposure to fine particulate matter (PM2.5) from forest fire smoke (FFS) has been associated with a range of adverse health effects, from decreased birth weight to premature mortality.2, 3, 4 However, the clearest evidence is from studies of acute respiratory effects,5, 6, 7 with inconsistent and inconclusive results for cardiovascular effects6,8, 9, 10 and cause-specific mortality.4,11, 12, 13, 14 These inconsistencies are unexpected, given that daily PM2.5 has been associated with cardiovascular effects15,16 and cause-specific mortality17, 18, 19 in urban environments. It is unclear whether the discrepancies between smoke-related and urban PM2.5 are because of differences in the constituents of the particulate matter, or limited power to detect the effects of FFS, or both.
FFS events are typically acute, and they often affect rural populations that do not provide the statistical power necessary to detect relatively small increases in health outcomes. In addition, conventional exposure assessment methods that use existing PM2.5 monitoring networks are limited because the instruments are spatially sparse compared with the smoke that can cover vast geographic areas. Many novel exposure assessment methods are incorporating satellite data and modeling to address these spatial limitations,8,9,20,21 but epidemiologic comparisons between conventional and novel methods have been rare.6,22 New methods have the potential to improve fire smoke epidemiology by better characterizing population variability in exposures, and by allowing inclusion of heavily affected rural areas in population-based analyses. Epidemiologic studies with more accurate exposure assessment and larger populations will have more power to detect small increases in health outcomes because of FFS if they actually exist. It is therefore important to evaluate how new exposure assessment methods compare with conventional methods whenever possible.
Recently the British Columbia Centre for Disease Control (BCCDC) in the province of British Columbia (BC), Canada, developed a spatially resolved model of PM2.5 exposure for use in its BC Asthma Medication Surveillance (BCAMS) system.23 The model was optimized to capture FFS events because evidence suggests that asthmatics are a particularly susceptible subpopulation.7 The BCCDC model combines daily PM2.5 measurements, aerosol optical depth from the Moderate Resolution Imaging Spectroradiometer (MODIS) instruments, fire radiative power from MODIS, manual tracings of FFS plumes from the US National Oceanic and Atmospheric Administration (NOAA) Hazard Mapping System, and meteorological forecasts of atmospheric venting conditions. Daily estimates are made for all populated areas of the province. Although the model was developed to support real-time public health surveillance, it has the potential to be useful for epidemiologic exposure assessment. The BC context provides a unique opportunity to evaluate that potential by comparing modeled with measured PM2.5 across the many areas where both metrics are available, and then to extend analyses using modeled PM2.5 to the entire province. Here we evaluate the effects of PM2.5 on pharmaceutical dispensations and outpatient physician visits for a range of respiratory and cardiovascular outcomes.
Methods
Study Area and Period
BC is located on the west coast of Canada, with an area of 944,735 km2 and a population of 4,243,580 in the census year of 2006. The province is divided into 89 local health areas (LHAs) for the purposes of health administration, and their 2006 populations ranged from 542 to 352,783 individuals. The study period covers the forest fire seasons (1 April to 30 September) of 2003 through 2010, during which the annual area burned averaged 1608 km2 and ranged from 132 to 3371 km2. The central and southern interior areas are most prone to forest fires, especially following damage done by an extensive infestation of the mountain pine beetle.24 The province has a dense air quality monitoring network relative to the size of its population (Figure 1).
Exposure Assessment
Measured PM2.5
The air quality monitoring network is maintained by the BC Ministry of Environment. Particulate matter was continuously measured during the study period in 29 of the 89 LHAs using PM2.5 and/or PM10 tapered element oscillating microbalances (Figure 1). All data were converted to PM2.5 equivalent concentrations as described elsewhere.5 Daily average concentrations measured at the monitoring sites were used to represent the exposure of the entire population of the LHA in which the monitor was located. Despite the large geographic areas covered by some rural LHAs, monitors were typically located in the largest community.
Modeled PM2.5
The BCCDC has developed an empirical FFS exposure model for public health surveillance, as described elsewhere.23 Briefly, the model estimates daily average PM2.5 at a spatial resolution of 5 × 5 km for all populated areas of the province by combining measured concentrations with remote sensing data and meteorological forecasts. The remote sensing data include: aerosol optical depth from MODIS, which is a measure of the total aerosol in any atmospheric column unobstructed by cloud;25 the local sum of fire radiative power (FRP) from hot spots detected by MODIS, which is proportional to their aerosol emissions;26 and smoke plumes hand drawn by NOAA analysts, which integrate images from seven different satellites for the Hazard Mapping System.27 The meteorological forecasts are summarized using the BC Ministry of Environment venting index that describes overall mixing in the atmosphere.28 We assigned daily average, population-weighted PM2.5 estimates to the entire populations of all LHAs. The model estimates were weighted using population data from the 2006 census dissemination areas (DAs) that typically have populations ranging from 400 to 700 individuals.29 Model estimates were assigned to the DA centroids, and their populations were used to calculate the overall population-weighted averages for each LHA. This resulted in two different exposure metrics for the 29 LHAs with air quality monitoring stations, and only the modeled metric for the other 60 LHAs.
Extreme Fire Days
Although the exposure model has inputs specific to FFS, it reflects PM2.5 from all sources because it includes measurements from the air quality network and aerosol optical depth as two of its important covariates. To further evaluate the effect of PM2.5 specifically from FFS, we used the FRP from MODIS to identify extreme fire days in BC. All thermal anomalies detected by MODIS include this measure of energy output by the detected fire. We calculated the daily sum FRP for all fires in BC for each day of the study period, and we defined days with summed FRP values above 90th percentile as extreme fire days. The assumption is that during these extreme fire days, fire smoke is more likely to be the dominant source of PM2.5 in the province.
Administrative Health Data
Daily counts of pharmaceutical dispensations for each LHA were retrieved from the BC PharmaNet database. We assessed the effect of daily PM2.5 on dispensations of salbutamol sulfate and fast-acting nitroglycerin. Salbutamol sulfate is commonly used to relieve acute exacerbations of asthma, chronic obstructive pulmonary disease (COPD), and other obstructive lung diseases. Previous studies in BC have found that increased FFS exposure is associated with increased salbutamol sulfate dispensations.22,30 Fast-acting nitroglycerin is commonly used to relieve acute exacerbations of angina. One previous study has suggested an association between exposure to smoke from a peat fire and emergency department visits for angina.8
Daily counts of cause-specific outpatient physician visits were retrieved from the BC Medical Services Plan billings database. Data were extracted by the International Classifications of Diseases, 9th revision (ICD-9) codes for asthma (493), COPD (490–492, 494–496), upper respiratory infections (460–466), lower respiratory infections (480–486), otitis media (381–382), and all cardiovascular diseases combined (390–459). No previous studies have evaluated the association between FFS and otitis media, but evidence from urban environments indicates a relationship with PM2.5 from vehicular sources31 and residential woodsmoke.32
Statistical Analyses
For each LHA, we used a generalized linear Poisson regression model to estimate the effect of PM2.5 on the rates of pharmaceutical dispensations and outpatient physician visits. Measured and modeled PM2.5 values were used for the 29 LHAs where both were available, and modeled values were used for all 89 LHAs. Individual models were run for all days and for extreme fire days only. All models were adjusted for temperature using a natural cubic spline of daily maximum apparent temperature with 3 d.f. Short- and long-term temporal trends were controlled using a factor variable that indicated the year, month, and day of week. A fixed lag of 0–1 days was chosen for all analyses, meaning that PM2.5 on the day before the pharmaceutical dispensation or physician visit was averaged with PM2.5 on the day of the event. This lag was chosen because it produced the best-fitted models in previous studies on FFS exposure in BC.9,30 The rate ratios (RRs) associated with modeled PM2.5 estimates were mapped for individual LHAs on extreme fire days to qualitatively evaluate the spatial relationships between the locations of large fires and affected populations. All RRs were calculated for a 10 μg/m3 increase in measured or modeled PM2.5.
After fitting models to the individual LHAs, we conducted a random effects meta-regression using the inverse variance method to estimate the overall effects for: (1) measured PM2.5 in the 29 LHAs with monitoring stations; (2) modeled PM2.5 in the 29 LHAs with monitoring stations; (3) modeled PM2.5 in the 60 LHAs without monitoring stations; and (4) modeled PM2.5 in all 89 LHAs. Meta-regressions were conducted for all days and for extreme fire days. When restricting the analyses to extreme fire days, models for some of the 60 LHAs without monitoring stations did not converge or the variance of the estimates was extremely large (SE >0.5), mostly because of their small populations. These LHAs were excluded from the meta-analyses, and excluded LHAs were indicated in the maps of RR estimates for individual LHAs. From herein meta-regression estimates for modeled PM2.5 in the 60 LHAs without monitors and in all 89 LHAs refer to results calculated with a varying number (between 2 and 12) of LHAs excluded.
RESULTS
Descriptive Statistics
Daily rates of pharmaceutical dispensations and physician visits were comparable for the 29 LHAs with monitoring stations and the 60 LHAs without. Similarly, the measured PM2.5 was comparable with the modeled PM2.5 in both cases (Table 1). Both measured and modeled exposure estimates were higher for the extreme fire days. In the 29 LHAs with monitors, the mean correlation coefficient between measured and modeled exposure within each LHA was 0.70 (ranging from 0.25 to 0.91) for all days, and 0.72 (ranging from 0.29 to 0.95) for extreme fire days. Correlations tended to be higher in heavily fire-affected LHAs and lower in LHAs where populations were distributed farther away from the monitors. In addition, more large fires occurred in the 60 LHAs without monitors.
Pharmaceutical Dispensations
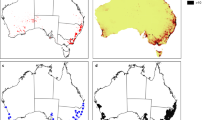
For the 29 LHAs with air quality monitoring stations, a 10 μg/m3 increase in measured PM2.5 was associated with a 4% increase (RR=1.04; 95% CI=1.03–1.06) in the meta-regression estimate for salbutamol dispensations during all fire season days. The same increase was observed for the modeled PM2.5 estimates in the same 29 LHAs, the 60 LHAs without monitors, and in all 89 LHAs. When restricted to the most extreme fire days, the estimates increased for all exposure groups (Figure 2). Individual LHA estimates for modeled PM2.5 on the most extreme fire days showed that rates were elevated in areas affected by large fires (Figure 3).
Meta-regression results for the associations between pharmaceutical dispensations and measured and modeled PM2.5 in the 29 LHAs with monitors, modeled PM2.5 in 60 LHAs without monitors, and all 89 LHAs, for all days of fire seasons and extreme fire days. Varying numbers (indicated in Figure 3) of LHAs were excluded from the analyses for 60 LHAs and all 89 LHAs in extreme fire days.
Dispensations of fast-acting nitroglycerin showed a different pattern. There was no significant effect of measured or modeled PM2.5 during all fire season days, but the effects were significantly elevated for modeled PM2.5 on extreme fire days. A 10 μg/m3 increase was associated with a 3% increase (RR=1.03; 95% CI=1.01–1.05) in the meta-regression estimate for nitroglycerin dispensations across all 89 LHAs (Figure 2). Once again, results for the individual LHAs show elevated rates in areas affected by large fires on the most extreme fire days (Figure 3).
Physician Visits
There was generally good agreement between meta-regression estimates for measured and modeled PM2.5 across the 29 LHAs with monitoring stations for all types of physician visits. One exception was a significant effect of measured PM2.5 on upper respiratory infections on all fire season days (RR=1.03; 95% CI=1.02–1.05), with no similar effect observed with the modeled estimates. Both measured and modeled PM2.5 were consistently associated with increased physician visits for asthma, lower respiratory infections, and otitis media on extreme fire days, and not associated with increased visits for upper respiratory infections. The consistency of the associations for COPD and cardiovascular visits was less clear. For COPD, the effects of measured PM2.5 were the same on all days and extreme fire days, whereas the effects of modeled PM2.5 were elevated on the extreme fire days. The effects of PM2.5 were small for cardiovascular visits, and significantly protective for measured PM2.5 in the 29 LHAs on all fire season days. Effects were slightly greater for modeled PM2.5 in those LHAs, and greater still for modeled PM2.5 in the 60 LHAs without monitors, and in all 89 LHAs (Figure 4). Effects of modeled PM2.5 were small but marginally significant on the most extreme fire days (RR=1.01; 95% CI=1.00–1.02) for all 89 LHAs.
Meta-regression results for the associations between physician visits and measured and modeled PM2.5 in the 29 LHAs with monitors, modeled PM2.5 in 60 LHAs without monitors, and all 89 LHAs, for all days of fire seasons and extreme fire days. Varying numbers (indicated in Figure 5) of LHAs were excluded from the analyses for 60 LHAs and all LHAs in extreme fire days.
Mapping results from the modeled PM2.5 estimates for all 89 LHAs on the most extreme fire days showed spatial overlap between affected areas and large fires for asthma, COPD, and otitis media. The overlap was less consistent for respiratory infections and cardiovascular disease. There were also strong associations for otitis media throughout the urban areas of Greater Vancouver and Victoria that are far removed from fires but still affected by smoke on extreme fire days (Figure 5). For example, Keane33 found that the Greater Vancouver area was affected by FFS in 30% of the summer days during the intense fire season in 2009, with an average PM2.5 increase of 5 μg/m3 on smoke-affected days.
Discussion
We found consistent associations between measured and modeled PM2.5 in 29 LHAs for salbutamol dispensations, and physician visits for asthma, lower respiratory infections, and otitis media. For every 10 μg/m3 increase in both measured and modeled PM2.5 on all fire season days, there was a 4% increase in salbutamol dispensations, a 6% increase in asthma visits, a 3% increase in lower respiratory infection visits, and a 5% increase in otitis media visits. These results are consistent with other studies on similar health outcomes. Elliott et al.30 reported that a 10 μg/m3 increase in PM2.5 was associated with a 6% increase in salbutomol dispensations in fire-affected populations in BC during the same fire seasons. Yao et al.22 reported that a 10 μg/m3 increase in PM2.5 was associated with a 4% increase in salbutomol dispensations and a 3% increase in asthma physician visits, respectively, during the 2010 fire season in BC. Similarly, Henderson et al.34 reported a 6% increase in odds of asthma physician visits during the 2003 fire season in BC. Null results for upper respiratory infections were also reported in previous studies that examined this outcome.34,35 These internal and external consistencies provide confidence in the PM2.5 estimates from the BCCDC exposure model, and therefore confidence in the effect estimates derived using health data from all 89 LHAs, including those 60 LHAs with no PM2.5 measurements available.
There were some outcomes that indicated discordance between the measured and modeled PM2.5 estimates for the 29 LHAs. These included nitroglycerin dispensations, COPD, and upper respiratory infections on all fire season days. These differences are likely because of differences in the exposure assignment for the two metrics. For measured values, the PM2.5 concentration recorded by the monitoring station or the PM2.5 equivalent of its PM10 measurement30 was applied to the entire population of the LHA. On the other hand, only the available PM2.5 measurements were used in the PM2.5 model on any given day, the estimates in each 5 × 5 km grid cell were population weighted, and then applied to the entire population of the LHA. For geographically large LHAs with dispersed populations, the modeled exposure can be quite different from the measured exposure, even though the measured exposure is one of many variables included in the modeled exposure. The population-weighted average distance to a monitoring station ranged from 2 to 32 km for the 29 LHAs, with a mean of 10 km. The LHA with the smallest correlation between measured and modeled values (LHA60, r=0.25) had a population-weighted average distance of 20 km from the monitoring station within the LHA.
To the best of our knowledge, this is the first study to examine the effects of FFS on otitis media. However, previous studies have found increased risk of childhood otitis media associated with exposure to environmental tobacco smoke, traffic-related air pollution, and residential wood smoke.31,32,36, 37, 38 Our study demonstrated a 5% increase in otitis media visits for population of all ages. Among all the otitis media visits, approximately half of them were visits by children under the age of 10 years. Restricting the analyses to this age group yielded the same point estimate (RR=1.05, 95% CI=1.03–1.08).
The meta-regression estimates for nitroglycerin dispensations and physician visits for cardiovascular diseases were null in most cases, but the associations with modeled PM2.5 in all 89 LHAs became statistically significant when restricting the data to extreme fire days. On fire days with the provincial sum of FRP in the 90th percentile, a 10 μg/m3 increase in modeled PM2.5 was associated with a 3% increase in nitroglycerin dispensations and a 1% increase in all cardiovascular physician visits. These effects were not significant for measured or modeled PM2.5 in the 29 LHAs with monitoring stations. One possible explanation is that the effects of FFS exposure on cardiovascular diseases are more prominent in rural areas where monitors are not available, and where access to care may be limited. This may also explain the null findings in many previous studies, mostly conducted using monitoring measurements in urban or densely populated areas.9,34,39, 40, 41 Another possible explanation is that inclusion of an entire population over an unprecedentedly long time series provides enough power to detect differences that have gone undetected by other studies. Only two other studies have found statistically significant effects on cardiovascular health outcomes from FFS, both by comparing outcomes in an area or time period affected by fires with outcomes in the same area or time period when it was not affected by fire.11,35
In this study, we evaluated the application of the FFS exposure model in epidemiologic studies by comparing the health effects related to the modeled PM2.5 with those related to measured PM2.5. The comparable effects observed for most respiratory health outcomes give us confidence in the model performance and utility. Modeled PM2.5 in all 89 LHAs was associated with cardiovascular outcomes during extreme fire days, but measured and modeled PM2.5 in the 29 LHAs was not. This suggests that the improved spatial coverage of the model may improve our ability to capture the population health effects of FFS exposure that may be more prominent in rural areas without air quality monitoring stations. The generally larger point estimates from modeled PM2.5 in the 29 LHAs compared with measured PM2.5 on extreme fire days suggested that the model might detect effects specific to FFS more sensitively, with the addition of smoke-specific information and the finer spatial resolution of estimates for exposure assignment.
There are several limitations in this study. First, the approach was ecologic and the entire population of an LHA, some with very large geographic areas, was assigned the same daily exposure level. Although the use of population-weighted average model estimates has improved the representativeness of the exposure assignment compared with using single monitors, misclassification is still likely to exist. Further studies on exposure and health responses at the individual level are needed to address this limitation. Second, the statistical approach we used was not able to estimate the effects in LHAs with very small populations (<5000) with small daily heath outcome counts (<10), and thus not able to include their effects in the overall meta-analysis. This could be an important limitation, especially if these remote and small communities responded to FFS exposure differently from the rest of the province, possibly because of their differences in population composition, access to health care, or social economic status.
In conclusion, we find consistent associations between measured and modeled PM2.5 for multiple cardiopulmonary health outcomes. The effects for modeled estimates are comparable with the effects for measured estimates on respiratory outcomes, and the effects of modeled estimates are generally stronger than the effects of measured estimates on cardiovascular outcomes. This suggests that the exposure model is a promising tool for increasing the power of epidemiologic studies to detect the health effects of FFS via improved spatial coverage and possibly via improved spatial resolution compared with conventional approaches.
References
Wotton BM, Nock CA, Flannigan MD . Forest fire occurrence and climate change in Canada. Inte J Wildland Fire 2010: 19 (3): 253–271.
Naeher LP, Brauer M, Lipsett M, Zelikoff JT, Simpson CD, Koenig JQ et al. Woodsmoke health effects: a review. Inhal Toxicol 2007: 19 (1): 67–106.
Holstius DM, Reid CE, Jesdale BM, Morello-Frosch R . Birth weight following pregnancy during the 2003 Southern California wildfires. Environ Health Perspect 2012: 120 (9): 1340–1345.
Johnston F, Hanigan I, Henderson S, Morgan G, Bowman D . Extreme air pollution events from bushfires and dust storms and their association with mortality in Sydney, Australia 1994-2007. Environ Res 2011: 111 (6): 811–816.
Elliott C, Henderson S, Wan V . Time series analysis of fine particulate matter and asthma reliever dispensations in populations affected by forest fires. Environ Health 2013: 12 (1): 11.
Henderson SB, Brauer M, Macnab YC, Kennedy SM . Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environ Health Perspect 2011: 119 (9): 1266–1271.
Henderson SB, Johnston FH . Measures of forest fire smoke exposure and their associations with respiratory health outcomes. Curr Opin Allergy Clin Immunol 2012: 12 (3): 221–227.
Rappold AG, Stone SL, Cascio WE, Neas LM, Kilaru VJ, Carraway MS et al. Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environ Health Perspect 2011: 119 (10): 1415–1420.
Delfino RJ, Brummel S, Wu J, Stern H, Ostro B, Lipsett M et al. The relationship of respiratory and cardiovascular hospital admissions to the southern California wildfires of 2003. Occup Environ Med 2009: 66 (3): 189–197.
Hanigan IC, Johnston FH, Morgan GG . Vegetation fire smoke, indigenous status and cardio-respiratory hospital admissions in Darwin, Australia, 1996-2005: a time-series study. Environ Health 2008: 7: 42.
Analitis A, Georgiadis I, Katsouyanni K . Forest fires are associated with elevated mortality in a dense urban setting. Occup Environ Med 2012: 69 (3): 158–162.
Hanninen OO, Salonen RO, Koistinen K, Lanki T, Barregard L, Jantunen M . Population exposure to fine particles and estimated excess mortality in Finland from an East European wildfire episode. J Expo Sci Environ Epidemiol 2009: 19 (4): 414–422.
Morgan G, Sheppeard V, Khalaj B, Ayyar A, Lincoln D, Jalaludin B et al. Effects of bushfire smoke on daily mortality and hospital admissions in Sydney, Australia. Epidemiology 2010: 21 1: 47–55.
Vedal S, Dutton SJ . Wildfire air pollution and daily mortality in a large urban area. Environ Res 2006: 102 (1): 29–35.
Martinelli N, Olivieri O, Girelli D . Air particulate matter and cardiovascular disease: a narrative review. Eur J Intern Med 2013: 24 (4): 295–302.
Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation 2010: 121 (21): 2331–2378.
Dockery DW, Pope CA, Xu X, Spengler JD, Ware JH, Fay ME et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med 1993: 329 (24): 1753–1759.
Pope CA, Thun MJ, Namboodiri MM, Dockery DW, Evans JS, Speizer FE et al. Particulate air pollution as a predictor of mortality in a prospective study of U.S. adults. Am J Respir Crit Care Med 1995: 151 (3_pt_1): 669–674.
Zanobetti A, Schwartz J . The effect of fine and coarse particulate air pollution on mortality: a national analysis. Environ Health Perspect 2009: 117 (6): 898–903.
van Donkelaar A, Martin RV, Levy RC, da Silva AM, Krzyzanowski M, Chubarova NE et al. Satellite-based estimates of ground-level fine particulate matter during extreme events: a case study of the Moscow fires in 2010. Atmos Environ 2011: 45 (34): 6225–6232.
Rappold AG, Cascio WE, Kilaru VJ, Stone SL, Neas LM, Devlin RB et al. Cardio-respiratory outcomes associated with exposure to wildfire smoke are modified by measures of community health. Environ Health 2012: 11: 71.
Yao J, Brauer M, Henderson SB . Evaluation of a wildfire smoke forecasting system as a tool for public health protection. Environ Health Perspect 2013: 121: 1142–1147.
Yao J, Henderson SB . An empirical model to estimate daily forest fire smoke exposure over a large geographic area using air quality, meteorological, and remote sensing data. J Expo Sci Environ Epidemiol 2013: 24: 328–335.
Kurz WA, Dymond CC, Stinson G, Rampley GJ, Neilson ET, Carroll AL et al. Mountain pine beetle and forest carbon feedback to climate change. Nature 2008: 452 (7190): 987–990.
Chu DA, Kaufman YJ, Ichoku C, Remer LA, Tanre D, Holben BN . Validation of MODIS aerosol optical depth retrieval over land. Geophys Res Lett 2002: 29 (12): MOD2-1–MOD2-4.
Ichoku C, Kaufman YJ . A method to derive smoke emission rates from MODIS fire radiative energy measurements. IEEE T Geosci Remote 2005: 43 (11): 2636–2649.
Ruminski M, Kondragunta S, Draxler R, Zeng J., Recent changes to the hazard mapping system. 15th International Emission Inventory Conference; New Orleans, Louisiana, 2006.
Air BC, Quality. Venting Index. 2014 (cited 28 March 2014); Available from http://www.bcairquality.ca/readings/ventilation-index.html.
Statistics Canada. Census Dictionary, In:Statistics: Canada, (ed)2011 pp 114.
Elliott CT, Henderson SB, Wan V . Time series analysis of fine particulate matter and asthma reliever dispensations in populations affected by forest fires. Environ Health 2013: 12: 11.
Brauer M, Gehring U, Brunekreef B, de Jongste J, Gerritsen J, Rovers M et al. Traffic-related air pollution and otitis media. Environ Health Perspect 2006: 114 (9): 1414–1418.
MacIntyre EA, Karr CJ, Koehoorn M, Demers PA, Tamburic L, Lencar C et al. Residential air pollution and otitis media during the first two years of life. Epidemiology 2011: 22 (1): 81–89.
Keane JC . Air quality and visibility in Southwestern British Columbia during forest fire smoke events. Master’s thesis. University of British Columbia: Vancouver, Canada, 2012.
Henderson SB, Brauer M, Macnab YC, Kennedy SM . Three measures of forest fire smoke exposure and their associations with respiratory and cardiovascular health outcomes in a population-based cohort. Environ Health Perspect 2011: 119 (9): 1266–1271.
Rappold AG, Stone SL, Cascio WE, Neas LM, Kilaru VJ, Carraway MS et al. Peat bog wildfire smoke exposure in rural North Carolina is associated with cardiopulmonary emergency department visits assessed through syndromic surveillance. Environ Health Perspect 2011: 119 (10): 1415–1420.
Stenstrom R, Bernard PAM, Ben-Simhon H . Exposure to environmental tobacco smoke as a risk factor for recurrent acute otitis media in children under the age of five years. Int J Pediatr Otorhinolaryngol 1993: 27 (2): 127–136.
Strachan DP, Cook DG . Health effects of passive smoking. 4. Parental smoking, middle ear disease and adenotonsillectomy in children. Thorax 1998: 53 (1): 50–56.
MacIntyre E, Karr C, Kochoorn M, Demers P, Tamburic L, Lencar C et al. Urban air pollution and acute otitis media in a population-based birth cohort. Epidemiology 2009: 20 (6): S77–S77.
Martin KL, Hanigan IC, Morgan GG, Henderson SB, Johnston FH . Air pollution from bushfires and their association with hospital admissions in Sydney, Newcastle and Wollongong, Australia 1994-2007. Aust NZ J Public Health 2013: 37 (3): 238–243.
Crabbe H . Risk of respiratory and cardiovascular hospitalisation with exposure to bushfire particulates: new evidence from Darwin, Australia. Environ Geochem Hlth 2012: 34 (6): 697–709.
Morgan G, Sheppeard V, Khalaj B, Ayyar A, Lincoln D, Jalaludin B et al. Effects of bushfire smoke on daily mortality and hospital admissions in Sydney, Australia. Epidemiology 2010: 21 (1): 47–55.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Yao, J., Eyamie, J. & Henderson, S. Evaluation of a spatially resolved forest fire smoke model for population-based epidemiologic exposure assessment. J Expo Sci Environ Epidemiol 26, 233–240 (2016). https://doi.org/10.1038/jes.2014.67
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2014.67
Keywords
This article is cited by
-
Health Impacts of Wildfire Smoke on Children and Adolescents: A Systematic Review and Meta-analysis
Current Environmental Health Reports (2023)
-
Cardiovascular health impacts of wildfire smoke exposure
Particle and Fibre Toxicology (2021)
-
Mortality associated with wildfire smoke exposure in Washington state, 2006–2017: a case-crossover study
Environmental Health (2020)
-
Particulate matter modelling techniques for epidemiological studies of open biomass fire smoke exposure: a review
Air Quality, Atmosphere & Health (2020)
-
Comparative chemistry and toxicity of diesel and biomass combustion emissions
Analytical and Bioanalytical Chemistry (2015)