Abstract
Uropathogenic Escherichia coli (UPEC) is the major cause of urinary tract infections (UTIs). In the present study, 198 E. coli isolates from patients with UTIs in Shanghai in 2008 were examined by susceptibility testing, with an extremely high number (153/198) showing multidrug resistance (MDR). And, the expression of extended-spectrum β-lactamases (ESBLs) reached 48.5% (96/198). The resistance rates to penicillins, fluoroquinolone, folate pathway inhibitors and first- and second-generation cephalosporins were high. Molecular analyses showed that the CTX-M-9 group (70/96) was the most common CTX-M group among UPEC, followed by the CTX-M-1 group (27/96). Phylogenetic group D accounted for 42.4% (84/198) of the isolates, exhibiting the highest ESBLs (50/84) and MDR (75/84) rates. Virulence genes were present in a significantly high proportion in the phylogenetic group B2 isolates, except for the afaBC gene. The ESBL-producing strains analyzed by pulsed-field gel electrophoresis (PFGE) were clustered into six groups at a cutoff of 67%. Notably, the findings that afaBC was specific to phylogenetic group D and PFGE group I and was correlated with the CTX-M-9 group were different from a previous report. In conclusion, knowledge of antimicrobial resistance data and virulence factors may enable clinicians to tailor empirical antibiotic treatments for UTIs.
Similar content being viewed by others
Introduction
Uropathogenic Escherichia coli (UPEC) isolates are among the most important pathogens causing urinary tract infections (UTIs) and are responsible for up to 90% of community-acquired and 50% of hospital-acquired UTIs.1
Furthermore, the increase in E. coli drug resistance has become a major concern in recent years. According to statistics from CHINET, which surveils the clinical drug resistance of pathogens to common antimicrobial agents in 14 hospitals in China, the expression of extended-spectrum β-lactamases (ESBLs) in E. coli rose from 17.9% in 2000 to 56.5% in 2009. The resistance genes associated with efficiently mobile genetic elements and the intercontinental spread of B2-O25b-ST131 plasmid-borne CTX-M-15-producing E. coli may explain such rapidly increasing drug resistance.2, 3, 4 However, antibiotic susceptibility profiling and molecular epidemiology studies can provide timely epidemiologic data pertaining to the trend of drug resistance, allowing clinicians to tailor empirical antibiotic treatments for UTIs.
UPEC possesses a set of virulence factors that promote its ability to colonize and survive in the urinary tract.1 The bacteria typically attaches to urinary tract epithelial cells via type 1-fimbrial adhesins (fim), P-fimbrial adhesins (pap), afimbrial adhesins (afa) and S-fimbrial adhesins (sfa),5 and recognized virulence factors of UPEC also include siderophore (for example, iucD), capsule, hemolytic and cytotoxic necrotizing factors. These virulence factors facilitate the invasion of the host and interfere with the host defense system.1, 6 Thus, investigation into the molecular bases for the pathogenic behavior and host predilections of this pathogen are needed for the development of strategies for managing and preventing UPEC infections.7
Moreover, gene distribution in clonally correlated strains should be evaluated because vertical or horizontal gene transfer may be reflected and pathogenic behavior can be predicted by the phylogenetic background, such as hypervirulence in phylogenetic group B2.8 Clarification of the correlations among drug resistance, virulence factors and phylogenetic background would be helpful for clinicians of restriction in detection accessible to predict other pathogenic behavior of such bacteria.
In this study, we provide important information regarding the distribution and association of the antimicrobial susceptibility, virulence factors and phylogenetic background of UPEC isolates from Shanghai. To our knowledge, such molecular epidemiologic data are not available for this region.
Materials and methods
Collection and identification of UPEC
We retrospectively identified the strains collected in 2008 at Shanghai Ruijin Hospital, a prominent general hospital in China, along with the following patient data: (i) gender, (ii) age and (iii) outpatient or in-patient. Patients presenting irritated bladder symptoms were considered and confirmed by microbial testing. Only fresh, midstream urine samples processed within 2 h of collection containing more than 105 colony-forming unit per milliliter of isolates were included in the study.9 Isolates suspected as E. coli by routine clinical methods in the consecutive period of April to November were collected and confirmed by biochemical identification. E. coli was recognized by the following: negative for urease, citrate utilization and hydrogen sulfide generation, and positive for motility, lysine decarboxylase, lactose fermentation, glucose fermentation and aerogenesis.10
Antimicrobial susceptibility testing
Antimicrobial susceptibility testing was performed by the Kirby–Bauer method in accordance with the Clinical and Laboratory Standards Institute (2008) recommendations.11 The following antimicrobial agent classes were tested: aminoglycosides (amikacin, gentamicin), penicillins (ampicillin (AMP), piperacillin (PIP)), penicillins with β-lactamase inhibitors (sulbactam-ampicillin (SAM), tazobactam-piperacillin (TZP)), cephalosporins (cefazolin (CFZ), cefaclor (CEC), cefuroxime (CXM), cefotaxime (CTX), ceftazidime (CAZ), cefepime (FEP), sulbactam-cefoperazone (SCF)), carbapenems (imipenem (IPM), meropenem (MEM)), fluoroquinolones (ciprofloxacin (CIP)) and folate pathway inhibitors (sulfamethoxazole-trimethoprim (SXT)). Screening for ESBLs production was performed with 30 μg cefotaxime and ceftazidime disks (Oxoid Ltd., Basingstoke, UK), with or without 10 μg clavulanic acid, according to the Clinical and Laboratory Standards Institute guidelines.11 Multidrug resistanc (MDR) was defined as the resistance to more than three antibiotics from different classes.
PCR for drug resistance genes and virulence genes
Drug resistance and virulence genes were detected by PCR. We detected eight virulence genes that have been largely reported to be associated with UPEC. The adhesion genes included fimH, sfaDE, papEF and afaBC genes, which represent type 1-fimbrial, S-fimbrial, P-fimbrial and afimbrial adhesions, respectively. Toxins genes, including hlyA and cnf1, which have known associations with UPEC,1 the siderophore system, including aerobactin (iucD), and capsule referring to group II (kpsMT II) were also under consideration.
The primers used are listed in Supplementary Table S1 and were separated into four multi-PCR groups: group 1 for detecting blaCTX-M-1, blaCTX-M-2, blaCTX-M-9, blaVEB-1 and blaPER-1; group 2 for detecting blaCTX-M-8, blaCTX-M-25, blaSHV and blaTEM; group 3 for detecting papEF, fimH and kpsMTII; and group 4 for detecting sfaDE, afaBC, iucD, cnf1 and hlyA. The amplification conditions for groups 1 to 3 were an initial denaturation at 94 °C for 7 min, 30 cycles of 94 °C for 50 s, 55 °C for 45 s and 72 °C for 1 min, and a final elongation at 72 °C for 7 min. The annealing temperature and extension time for group 4 were adjusted to 63 °C and 2 min, 15 s. The PCR products were separated by electrophoresis and observed after staining. Some positive products were sequenced to verify the bands for corresponding gene.
Phylogenetic analysis
A triplex PCR was performed to segregate each isolate into one of the four main phylogenetic groups (A, B1, B2 and D) by targeting two marker genes (chuA and yjaA) and a DNA fragment, TSPE4.C2.12 The PCR conditions were the same as those described by Clermont et al.12
Pulsed-field gel electrophoresis
Ninety-six ESBL-producing strains were analyzed for genetic relationships by pulsed-field gel electrophoresis (PFGE) using the restriction enzyme XbaI according to the guidelines for E. coli O157:H7, Salmonella and Shigella.13, 14
Briefly, electrophoresis was performed using 1% SeaKem agarose and 0.5% Tris-borate-EDTA under the following running conditions: a switch time from 2.16 to 54.17 s at a gradient of 6 V cm−1 and an included angle of 120° for 19 h at 14 °C. The Salmonella enteric serovar Braenderup H9812 universal marker (kindly provided by the Shanghai Municipal Center for Disease Control and Prevention) was used as an MW standard. The analysis of the PFGE profiles was performed using Bionumerics software v.3.5 (Applied Maths, Sint-Martens-Latem, Belgium), applying the Dice similarity coefficient on the basis of the unweighted-pair group method by average linkages, with a 1.5% band tolerance. Isolates with a similarity of ⩾67% were considered a cluster.
Statistical analysis
SPSS software version 20.0 (IBM Corporation, Armonk, NY, USA) was used for the statistical analysis. The differences in the distribution of ESBLs and virulence-related genes and the relationships among the antimicrobial agents, specific patients and phylogenetic groups were analyzed by a χ2 test. We set α, the size of a test or called significance level, as 0.05. The Holm method was used for adjustments for the multiple comparisons.
Results
Bacterial collection
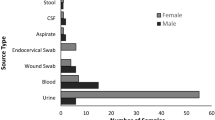
In the eight-month consecutive period from April to November in 2008, 198 qualified strains from the urine samples of UTIs patients were confirmed as E. coli by biochemical identification. There were more specimens from females (166/198) than males (32/198). The median age was 64 years, and the quartile ranged from 53 to 77 years old. A total of 129 isolates originated from community outpatients, and another 69 were from hospital in-patients.
Antimicrobial susceptibility
The susceptibility data are presented in Table 1; the rate of drug intermediate, which can be calculated from the rates of susceptible and resistant pathogens, was omitted. The UPEC strains showed the highest rates of susceptibility to MEM (99.5%), followed by IPM (99.0%), amikacin (87.9%), TZP (87.9%), CAZ (85.4%), SCF (81.8%) and FEP (76.8%). In contrast, low susceptibility rates were found for AMP (13.1%), PIP (17.2%), CIP (24.7%), CXM (27.3%), SXT (40.4%), SAM (40.9%), gentamicin (43.4%), CFZ (43.4%), CEC (45.5%) and CTX (51.0%). The community-acquired isolates were slightly more susceptible to the following antimicrobial agents than the hospital-acquired isolates but without valid significance (the susceptible rates for isolates from the in- and outpatients, respectively): CIP (29.5% and 15.9%) (P=0.036); SXT (47.3% and 27.5%) (P=0.007); amikacin (92.2% and 79.7%) (P=0.010); and gentamicin (48.8% and 33.3%) (P=0.036) (Table 1).
Ninety-six isolates (48.5%) were found to be ESBL producers by antimicrobial susceptibility testing. As indicated in Table 1, the percentage of susceptible isolates was significantly lower among the ESBL producers than that among the non-ESBL producers with regard to AMP, PIP, SAM, CIP, SXT, CFZ, CEC, CXM, CTX, CAZ, FEP and SCF. However, the high rate of susceptibility to IPM and MEM in the two populations did not differ significantly (Table 1).
One hundred and fifty-three isolates (78.1%) were found to exhibit MDR, and the MDR rate of the pathogens from the in-patients was significantly higher than that from the outpatients (P=0.002) (Supplementary Table S2).
Characterization of resistance genes
The β-lactamases are classified by molecular and functional classification systems.15, 16 The vast majority of ESBLs belong to the TEM-, SHV-, CTX-M-, PER- and VEB-type enzymes of group 2be.17 Updated information of ESBLs and other β-lactamases can be found at http://www.lahey.org/Studies/. In this study, we detected genes of ESBL type (blaTEM, blaSHV), genes of the CTX-M type (five groups from blaCTX-M named by their representative gene, blaCTX-M-1, blaCTX-M-2, blaCTX-M-8, blaCTX-M-9, blaCTX-M-25) and specific genes predominant in a respective type (blaPER-1, blaVEB-1). Ninety-two isolates were positive by PCR for blaCTX-M, with 27 for the CTX-M-1 group and 70 for the CTX-M-9 group (five isolates were positive for both). Two isolates were positive for blaSHV and 1 for blaVEB-1. Conversely, no blaPER-1, blaCTX-M-2, blaCTX-M-8 and blaCTX-M-25 genes were found. In addition, a total of 108 isolates were positive for blaTEM.
No significant difference was found in the distributions of blaCTX-M-1 (13.0% and 14.0% gene-positive rates for isolates from the in- and outpatients, respectively, P=0.859), blaCTX-M-9 (43.5 and 31.0%, P=0.080) and blaTEM (56.5 and 53.3%, P=0.683) among the in- and outpatients (Table 2).
Overall, these CTX-M-producing strains exhibited a high rate of resistance to AMP, PIP, SAM, CFZ, CEC, CXM, CTX, FEP and SCF (Supplementary Table S3). In addition, the CTX-M-1 producers also shared significantly high resistance rates to CAZ, whereas the CTX-M-9 producers shared significantly high resistance rates to CIP and SXT. Moreover, the blaTEM-positive isolates exhibited high rates of resistance to AMP, PIP, SXT and gentamicin (Supplementary Table S3).
Prevalence of virulence genes among UPEC isolates
The targeted virulence genes were detected in 188 (94.9%) isolates, whereas the remaining 10 isolates were negative for virulence genes. According to the adhesion gene analyses, fimH (87.4%) was the most prevalent among the 198 E. coli isolates, followed by papEF, sfaDE and afaBC (24.7%, 8.1%, and 10.1%, respectively). With regard to toxins, hlyA (11.6%) was more prevalent than cnf1 (7.1%), and the prevalence of aerobactin (iucD) and group II capsule (kps MT II) were 65.7% and 60.6%, respectively.
The virulence genes displayed distinct and complex associations with each other (Table 3). kpsMT II was associated with seven other virulence genes detected in this study, and papEF was related to the other virulence genes, with the exception of afaBC. Instead, cnf1 occurred exclusively in sfaDE- or hlyA-positive strains, which were strongly associated with each other, and afaBC was related to iucD.
An analysis of the relationship between the virulence and drug resistance genes showed that afaBC was associated with blaCTX-M-9, whereas sfaDE and cnf1 appeared to be negatively correlated with blaCTX-M-9 and blaTEM (Table 3).
Phylogenetic characterization
All four major phylogenetic lineages (A, B1, B2 and D) were found among the 198 urinary E. coli isolates: phylogenetic group D (42.4%) predominated, followed by B2 (29.8%), A (19.2%) and B1 (8.6%). Phylogenetic groups D and A were observed for most of the ESBL-producing E. coli isolates (Supplementary Table S2). The blaCTX-M-9-positive rate was highest in phylogenetic group D (44.0%, 37/84), followed by groups A (42.1%, 16/38), B1 (23.5%, 4/17) and B2 (22.0%, 13/59) (Table 2). When the relationship between phylogenicity and virulence was evaluated, a prevalence of the fimH, papEF, kpsMT II, iucD and hlyA genes was significantly higher in phylogenetic groups D and B2 compared with those in the other phylogenetic groups (Table 2). The sfaDE and cnf1 genes were frequently found in the group B2 isolates, whereas the afaBC gene was only found in the group D isolates (Table 2).
The results showed that cnf1 (1.3%), sfaDE (2.0%) and hlyA (7.2%) were significantly uncommon in the MDR isolates (Table 2). Moreover, cnf1 (3.1%) and papEF (17.7%) were to some extent uncommon in the ESBL-producing isolates, whereas afaBC was more common in these isolates (19.8%, 19/96) compared with the non-ESBL-producing isolates (1.0%, 1/102) (Table 2). It appeared that cnf1, sfaDE, hlyA and papEF were related to low drug resistance, whereas afaBC was associated with high drug resistance. Furthermore, the sfaDE, cnf1 and hlyA genes were found related to a CIP-susceptible phenotype (P<0.001 all) (Supplementary Table S3).
Pulsed-field gel electrophoresis
The 96 ESBL-producing isolates were analyzed for genetic relationships by PFGE. PFGE profiles were obtained for 88 isolates, whereas the results for the other eight isolates displayed unexpected smearing. There was no predominant PFGE type. A total of 84 PFGE patterns and six clusters (PFGE group I–PFGE group VI) were identified with a cutoff of 67%. More than one isolate was found in three of the PFGE patterns (Figure 1).
Pulsed-field gel electrophoresis (PFGE) and gene profiles of extended-spectrum β-lactamase (ESBL)-producing uropathogenic Escherichia coli (UPEC). The strain numbers and PFGE profiles of 88 ESBL-producing UPEC strains are shown on the left. Six groups marked I to VI were clustered at 67% similarity. Other information; such as age, gender, in- or outpatient status, MDR, phylogenetic group and virulence genes, are illustrated as a heatmap on the right side of the figure. The squares in gray denote positivity for genes or descriptions, whereas the other squares in the columns showing multicategory information are distinguished by colors.
Combining PFGE with former results of ESBL-producing isolates, Figure 1 visually illustrated the association of the antimicrobial susceptibility, virulence factors and phylogenetic background.
Discussion
UPEC isolates are major cause of UTIs and may be responsible for nearly 90% of UTIs. This study was designed to characterize local isolates of UPEC with respect to phylogenicity and the distribution of drug resistance genes and virulence factors. Although a number of studies on this subject have been conducted in various parts of the world, such data are not available for Shanghai.
Our study provides important information regarding the antimicrobial susceptibility, virulence factor distribution and phylogenetic background of UPEC from this region. The data demonstrate that the resistance rates for several antimicrobial agents normally used to treat UTIs are high in this locality. It is worth emphasizing that fluoroquinolone is one of the first-line agents recommended for the empirical treatment of UTIs in Shanghai. Our finding of 71.2% (Table 1) resistance to fluoroquinolone was higher than the rate of 58.7% reported by CHINET 2008. Indeed, the resistance to fluoroquinolones was so high that the empirical use of this agent for UTIs in this locality should be avoided. It is suggested that alternative agents, such as fosfomycin and nitrofurantoin, should now be used as empirical treatments for UTIs.18, 19, 20 The high resistance level of fluoroquinolone appears to be linked to the use of antibiotics in this region. A resistance rate of UPEC under 10% was found only for IPM, MEN, TZP, SCF and CAZ, which may represent optimistic options for the empiric therapy of UTIs. According to an old interpretation (M100-S18), the ESBL-producing strains should not be reported as susceptible to cephalosporins, whereas the test interpretations for these agents do not need to be changed into resistance according to new interpretation (M100-S20).21 It is noteworthy that approximately 63.5% of the ESBL-producing strains were susceptible to CAZ according to the new interpretation (M100-S20), and therefore the treatment options for these strains would be enhanced.
Similar to other studies in China, this study found a high incidence (48.5%) of ESBLs production in UPEC. The ESBLs rates were equally high in both hospital- and community-acquired infections (Supplementary Table S2), and no valid significant differences in drug susceptibility rates between the in- and outpatient groups were found, indicating a very large reservoir of ESBLs in the Shanghai community, similar to the phenomena in other regions of China22 and other countries, such as Ireland and South Korea.23, 24
In the present study, the blaCTX-M genotype (95.8%, 92/96) was found to be the predominant ESBL. The diversity of blaCTX-M genotypes detected in our study showed that the CTX-M-9 group (70/96) was the most common CTX-M type in Shanghai, followed by the CTX-M-1 group (27/96), which was in accordance with the epidemic of the CTX-M type in China.22, 25
PFGE showed that the MDR or ESBL-producing isolates were genetically diverse, which indicated that such factors as the horizontal transfer of plasmids and other mobile genetic elements may have an important role in resistance gene dissemination.
Furthermore, we found that 42.4% of our isolates belonged to a single phylogenetic group, group D; this high percentage of group D is in agreement with some other studies in China,26 yet is distinct from other countries, such as the prevalence of group A in Russia and B2 in Norway.27
According to our data, it is clear that the MDR and ESBLs rates were highest in phylogenetic group D and lowest in group B2 (Supplementary Table S2). These findings are in accordance with previous studies showing that drug resistance is associated with non-B2 phylogenetic groups in UPEC.28 Therefore, the prevalence of phylogenetic group D was consistent with the high ESBLs rate in China. We also found that virulence genes were present in a significantly high proportion of the phylogenetic group B2 isolates, with the exception of the afaBC gene, which was more frequent in the group D isolates (Table 2). It appears that there is a correlation between drug resistance and reduced virulence, and a number of studies have shown that UPEC resistant to ampicillin, sulfonamides, tetracycline, streptomycin and fluoroquinolone are typically less virulent than their susceptible counterparts.29, 30 It has also been reported that biofilm-forming E. coli are more susceptible to nalidixic acids than those negative for biofilm formation.31 Here, we show similar results that resistance to AMP, PIP, SAM, TZP, CIP, SXT, GEN, CFZ, CEC, CXM and CTX is associated with a lower prevalence of most virulence genes (Supplementary Table S3). Although the mechanism of the correlation between drug resistance and reduced virulence remains unclear, it has been proposed that the loss of incompatible pathogenicity islands in high-resistance strains may contribute to this phenotype. However, this has not yet been proven.
In contrast to other virulence genes, afaBC, which encodes a urinary tract adhesin, was found to be positively associated with drug resistance in this study. A higher prevalence of afaBC-positive strains resistant to tetracycline, ampicillin, sulfamethoxazole and streptomycin has been noted previously.32 We also found a preferential occurrence of afaBC in the strains resistant to PIP, SAM, CIP, CFZ, CEC, CXM, CTX and FEP (Supplementary Table S3), which was also related to ESBLs and MDR to some extent (Table 2). Furthermore, afaBC was specific to PFGE group I and absent in the other five E. coli lineages (Figure 1). Thus, the acquisition or retention of the afaBC gene may require a particular genetic background, or there may be barriers to its horizontal movement into other groups. Moreover, afaBC was only detected in phylogenetic group D and showed a high relationship with the CTX-M-9 group, results that differed from the report of Karisik relating afaBC to phylogenetic group B2 and the CTX-M-1 group,33 which might reflect difference in the epidemic strains and correlation deviation.
In summary, our data showed that ESBLs rates were equally high in both hospital- and community-acquired UTI E. coli isolates. The UPEC isolates exhibited a battery of virulence factors, with high rates of resistance to first- and second-generation cephalosporins and fluoroquinolone, which could result in serious public health risks. A high drug resistance and low virulence were associated with phylogenetic group D, whereas a high virulence and low drug resistance were correlated with group B2. Moreover, afaBC was found to be specific to PFGE group I and phylogenetic group D and correlated with CTX-M-9 group. These findings will contribute to the ability of clinicians to devise empirically antibiotic treatments and pathogenic behavior prediction in efforts to prevent UPEC infections.
References
Sussman, M . Molecular Medical Microbiology, Academic Press: New York, NY, (2002).
Dolejska, M . et al. CTX-M-15-producing Escherichia coli clone B2-O25b-ST131 and Klebsiella spp. isolates in municipal wastewater treatment plant effluents. J. Antimicrob. Chemother. 66, 2784–2790 (2011).
Nicolas-Chanoine, M. H . et al. Intercontinental emergence of Escherichia coli clone O25:H4-ST131 producing CTX-M-15. J. Antimicrob. Chemother. 61, 273–281 (2008).
Peirano, G . & Pitout, J. D . Molecular epidemiology of Escherichia coli producing CTX-M beta-lactamases: the worldwide emergence of clone ST131 O25:H4. Int. J. Antimicrob. Agents 35, 316–321 (2010).
Bashir, S ., Haque, A ., Sarwar, Y ., Ali, A . & Anwar, I . Virulence profile of different phylogenetic groups of locally isolated community acquired uropathogenic E. coli from Faisalabad region of Pakistan. Ann. Clin. Microbiol. Antimicrob. 11, 23 (2012).
Johnson, J. R . & Stell, A. L . Extended virulence genotypes of Escherichia coli strains from patients with urosepsis in relation to phylogeny and host compromise. J. Infect. Dis. 181, 261–272 (2000).
Johnson, J. R . & Russo, T. A Molecular epidemiology of extraintestinal pathogenic (uropathogenic) Escherichia coli. Int. J. Med. Microbiol. 295, 383–404 (2005).
Picard, B . et al. The link between phylogeny and virulence in Escherichia coli extraintestinal infection. Infect. Immun. 67, 546–553 (1999).
Tabibian, J. H . et al. Uropathogens and host characteristics. J. Clin. Microbiol. 46, 3980–3986 (2008).
R.Murray, P . Manual of Clinical Microbiology, American Society for Microbiology: Washington, DC, (2007).
Institute CaLS Performance Standards for Antimicrobial Susceptibility Testing Eighteenth Informational Supplement M100-S18 edn. (Institute CaLS, Wayne, PA, USA, (2008).
Clermont, O ., Bonacorsi, S . & Bingen, E . Rapid and simple determination of the Escherichia coli phylogenetic group. Appl. Environ. Microbiol. 66, 4555–4558 (2000).
Herschleb, J ., Ananiev, G . & Schwartz, D. C . Pulsed-field gel electrophoresis. Nat. Protoc. 2, 677–684 (2007).
Ribot, E. M . et al. Standardization of pulsed-field gel electrophoresis protocols for the subtyping of Escherichia coli O157:H7, Salmonella, and Shigella for PulseNet. Foodborne Pathogen. Dis. 3, 59–67 (2006).
Bush, K . & Jacoby, G. A . Updated functional classification of beta-lactamases. Antimicrob. Agents Chemother. 54, 969–976 (2010).
Bush, K ., Jacoby, G. A . & Medeiros, A. A . A functional classification scheme for beta-lactamases and its correlation with molecular structure. Antimicrob. Agents Chemother. 39, 1211–1233 (1995).
Akinci, E . & Vahaboglu, H . Minor extended-spectrum beta-lactamases. Expert Rev. Anti Infect. Ther. 8, 1251–1258 (2010).
Kurt, G . et al. Urogenital Infections, Grafos: Spain, (2010).
Naber, K. G ., Schito, G ., Botto, H ., Palou, J . & Mazzei, T . Surveillance study in Europe and Brazil on clinical aspects and Antimicrobial Resistance Epidemiology in Females with Cystitis (ARESC): implications for empiric therapy. Eur. Urol. 54, 1164–1175 (2008).
Wagenlehner, F. M ., Wullt, B . & Perletti, G . Antimicrobials in urogenital infections. Int. J. Antimicrob. Agents 38 (suppl: 3–10) (2011).
Institute CaLS Performance Standards for Antimicrobial Susceptibility Testing Twentieth Informational Supplement M100-S20 edn (Institute CaLS, Wayne, PA, USA, (2010).
Cao, X . et al. Molecular characterization and antimicrobial susceptibility testing of Escherichia coli isolates from patients with urinary tract infections in 20 Chinese hospitals. J. Clin. Microbiol. 49, 2496–2501 (2011).
Fennell, J . et al. Increasing prevalence of ESBL production among Irish clinical Enterobacteriaceae from 2004 to 2008: an observational study. BMC Infect. Dis. 12, 116 (2012).
Park, S. H . et al. Molecular epidemiology of extended-spectrum beta-lactamase-producing Escherichia coli in the community and hospital in Korea: emergence of ST131 producing CTX-M-15. BMC Infect. Dis. 12, 149 (2012).
Liu, W . et al. Novel CTX-M {beta}-lactamase genotype distribution and spread into multiple species of Enterobacteriaceae in Changsha, Southern China. J. Antimicrob. Chemother. 63, 895–900 (2009).
Abdallah, K. S ., Cao, Y . & Wei, D. J . Epidemiologic Investigation of Extra-intestinal pathogenic E. coli (ExPEC) based on PCR phylogenetic group and fimH single nucleotide polymorphisms (SNPs) in China. Int. J. Mol. Epidemiol. Genet. 2, 339–353 (2011).
Grude, N . et al. A comparison of phylogenetic group, virulence factors and antibiotic resistance in Russian and Norwegian isolates of Escherichia coli from urinary tract infection. Clin. Microbiol. Infect. 13, 208–211 (2007).
Moreno, E . et al. Quinolone, fluoroquinolone and trimethoprim/sulfamethoxazole resistance in relation to virulence determinants and phylogenetic background among uropathogenic Escherichia coli. J. Antimicrob. Chemother. 57, 204–211 (2006).
Johnson, J. R . et al. Association of carboxylesterase B electrophoretic pattern with presence and expression of urovirulence factor determinants and antimicrobial resistance among strains of Escherichia coli that cause urosepsis. Infect. Immun. 59, 2311–2315 (1991).
Johnson, J. R ., van der Schee, C ., Kuskowski, M. A ., Goessens, W . & van Belkum, A . Phylogenetic background and virulence profiles of fluoroquinolone-resistant clinical Escherichia coli isolates from the Netherlands. J. Infect. Dis. 186, 1852–1856 (2002).
Soto, S. M . et al. Biofilm formation in uropathogenic Escherichia coli strains: relationship with prostatitis, urovirulence factors and antimicrobial resistance. J. Urol. 177, 365–368 (2007).
Ejrnaes, K . Bacterial characteristics of importance for recurrent urinary tract infections caused by Escherichia coli. Dan. Med. Bull. 58, B4187 (2011).
Karisik, E ., Ellington, M. J ., Livermore, D. M . & Woodford, N . Virulence factors in Escherichia coli with CTX-M-15 and other extended-spectrum beta-lactamases in the UK. J. Antimicrob. Chemother. 61, 54–58 (2008).
Acknowledgements
This work was supported in part by the National Natural Science Foundation of China (grant nos. 30770820, 30970125, 81271793, 81201334, 81261160321, 81101264 and 81171587), the National High Technology Research and Development Program of China Program (grant no. 2011AA02A119) and the Natural Science Foundation of Shanghai (grant no. 13ZR1423000). We gratefully acknowledge the Department of Clinical Microbiology at Shanghai Ruijin Hospital for specimen collection and thank the lab of Microbiology at Shanghai Municipal Center for Disease Control and Prevention for the PFGE platform.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on The Journal of Antibiotics website
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, Y., Zhao, S., Han, L. et al. Drug resistance and virulence of uropathogenic Escherichia coli from Shanghai, China. J Antibiot 67, 799–805 (2014). https://doi.org/10.1038/ja.2014.72
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2014.72
This article is cited by
-
Prevalence of USP and hlyA Genes and Association with Drug Resistance in Uropathogenic Escherichia coli Isolated from Patients in a Tertiary Hospital from Southeast China
Bulletin of Experimental Biology and Medicine (2022)
-
Virulence factors and antimicrobial resistance of uropathogenic Escherichia coli (UPEC) isolated from urinary tract infections: a systematic review and meta-analysis
BMC Infectious Diseases (2021)
-
Distribution of virulence genes and phylogenetics of uropathogenic Escherichia coli among urinary tract infection patients in Addis Ababa, Ethiopia
BMC Infectious Diseases (2020)
-
Urinary tract infections: microbial pathogenesis, host–pathogen interactions and new treatment strategies
Nature Reviews Microbiology (2020)
-
Ciprofloxacin resistance in community- and hospital-acquired Escherichia coli urinary tract infections: a systematic review and meta-analysis of observational studies
BMC Infectious Diseases (2015)