Abstract
The purpose of this study is to examine the use of anti-methicillin-resistant Staphylococcus aureus (MRSA) drugs, such as vancomycin (VCM), teicoplanin (TEIC), arbekasin (ABK) and linezolid (LZD), and the antibiotic susceptibilities of MRSAs in Kobe University Hospital. We investigated MRSA isolation and use of anti-MRSA drugs and susceptibilities of MRSA, using linear regression analysis, from 2007 to 2011, and checked for correlation between the use of these drug and the antibiotic susceptibilities of MRSA. The overall monthly isolation rates of MRSA decreased from a mean of 84.8% in 2007 to 70.0% in 2011 (r=0.946, P=0.015, b=−0.220), and the monthly isolation rate of MRSA in inpatients decreased from a mean of 78.6% in 2007 to 57.7% in 2011 (r=0.952, P=0.012, b=−0.160). From 2007 to 2011, VCM consumption significantly increased (r=0.916, P=0.029, b=0.055), whereas TEIC and LZD use remained stable during the study period. In addition, ABK use significantly decreased from 23.8 defined daily dose (DDD) per 1000 patient-days in 2007 to 5.2 DDD per 1000 in 2011 (r=0.902, P=0.036, b=−0.216). Susceptibility rates of MRSA were almost 100% to TEIC and VCM. The rates of MRSA to ABK and LZD significantly increased (r=0.959, P=0.010, b=2.137 for ABK and r=0.933, P=0.020, b=3.111 for LZD). In conclusion, our findings indicated a decreased MRSA isolation rate and the effective use of anti-MRSA drugs (VCM, TEIC, ABK and LZD), and improved susceptibility rates to anti-MRSA drugs, suggesting the possibilities that appropriate and early use of anti-MRSA drugs may cause the decrease of MRSA isolation.
Similar content being viewed by others
Introduction
Many resistant strains have been reported recently, and physicians and researchers have focused on their treatment or eradication, but challenges remain. Resistant strains may cause several problems:1, 2 (1) the available antibiotics are limited; (2) methicillin-resistant Staphylococcus aureus (MRSA) tends to cause hospitalized infections; (3) resistant strains may be partly generated by inappropriate antibiotic use; (4) it is difficult to discriminate between infection and colonization, and the treatment indications may not be clear in some cases; (5) the rates of antimicrobial resistance may be higher in countries with higher rates of antimicrobial consumption.
MRSA is one of representative resistant strains, and research for its prevention and treatment was carried out.3–5 The concept that MRSA infection presents different indications for treatment and diagnoses of colonization is controversial, but the differential diagnosis between bacterial infection and bacterial colonization is necessary to prevent unnecessary use of anti-MRSA drugs.6, 7
Currently, four or five types of established anti-MRSA drugs are available in Japan.8, 9 The representative anti-MRSA drug vancomycin (VCM) has been reported to have lost its clinical effectiveness because of the development of MRSA strains with resistance or reduced susceptibility to VCM.10, 11, 12, 13, 14 This might be, in part, the result of repeated use of this drug, including its unnecessary use for MRSA colonization, for instance.15, 16, 17
The treatment of staphylococcal infections has become more challenging because of the following: (1) a rising frequency of isolation of multidrug-resistant isolates, particularly in the subset of infections caused by MRSA; (2) emergence of highly virulent strains of MRSA in the community setting; and (3) lack of clinical data to reliably support the use of antibiotics containing VCM in the treatment of severe infections caused by S. aureus. Moreover, the emergence and spread of resistance to compounds used as alternatives of VCM (that is, linezolid (LZD)) appears to be on the rise among clinical isolates of MRSA. To prevent the spread of resistant pathogens, it is necessary to detect resistant pathogens and monitor antimicrobial consumption volumes and bacterial susceptibilities.18
In this study, we examined recent anti-MRSA drug use and MRSA isolations in patients, and susceptibilities to anti-MRSA drugs, such as VCM, teicoplanin (TEIC), arbekasin (ABK) or LZD, to grasp recent MRSA.
Results
MRSA isolation
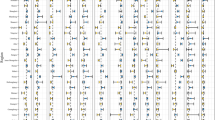
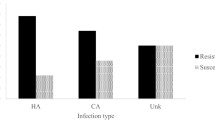
A total of 7200 specimens of S. aureus were isolated during the study period and were tested for methicillin resistance. The overall isolation rates of the monthly analyzed MRSA decreased from a mean of 84.8% in 2007 to 70.0% in 2011 (r=0.946, P=0.015, b=−0.220), and the monthly isolation rate of MRSA in inpatients decreased from a mean of 78.6% in 2007 to 57.7% in 2011 (r=0.952, P=0.012, b=−0.160), whereas the monthly isolation rate of MRSA in outpatients increased from a mean of 6.2% in 2007 to 12.4% in 2011 (r=0.949, P=0.014, b=0.553; Figure 1 and Table 1).
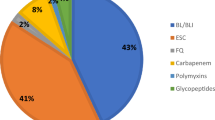
Annual anti-MRSA drug consumption
The use of each individual antimicrobial agent varied with time (Figure 2 and Table 2). VCM consumption significantly increased from a mean of 78.1 defined daily dose (DDD) per 1000 patient-days in 2007 to 130 DDD per 1000 patient-days in 2011 (r=0.916, P=0.029, b=0.055). In contrast, TEIC and LZD use remained stable during the study period (r=0.790, P=0.112, b=−0.137 for TEIC and r=0.723, P=0.167, b=0.254 for LZD). In addition, the trend in consumption of ABK significantly decreased from 23.8 DDD per 1000 patient-days in 2007 to 5.2 DDD per 1000 patient-days in 2011 (r=0.902, P=0.036, b=−0.216).
Susceptibilities to anti-MRSA drugs
The antibiotic susceptibility rates of MRSA to VCM, TEIC, ABK and LZD every year are shown in Table 3. A total of 3171 MRSA isolates were tested for susceptibility. Susceptibility rates of MRSA were all 100% to TEIC and to VCM, except to VCM in 2010 which was 99.8%. From 2007 to 2011, the susceptibility rates of MRSA to ABK significantly increased from 95.8% in 2007 to 97.7% in 2011 (r=0.959, P=0.010, b=2.137), and those of MRSA to LZD significantly increased from 98.9% in 2007 to 100% in 2011 (r=0.933, P=0.020, b=3.111).
Discussion
MRSA have been recognized as representative resistant strains and their isolation has been recently reported to be increasing.19, 20 VCM, TEIC, ABK and LZD have been established as anti-MRSA drugs for worldwide use. In the last couple of years, newly established daptomycin have become commercially available.21, 22
In our hospitals, physicians check the therapeutic drug monitoring of VCM or TEIC every 2–3 days to determine appropriate doses for treatment and the risks of adverse events, such as renal dysfunction.23, 24 This measure can be useful for several reasons: (1) to familiarize physicians with current antibiotic pharmacokinetics/pharmacodynamics theories; (2) to prevent drug-induced adverse events by paying attention to therapeutic drug monitoring; and (3) to rapidly report to the infection control team or Department of Infectious Diseases if a treatment is not effective and a patients’ condition is not improving. It is also important to discuss diagnoses and consider whether the isolation of bacteria represents infection or bacterial colonization, to prevent the unnecessary use of antibiotics.
In the present study, the first finding was that the trend in the rate of MRSA isolation significantly decreased during the study period. In particular, the trend in the rate of MRSA inpatients significantly decreased, suggesting that the change and diversification of the characterization of outpatients have been shown, and this was supported by the studies showing that community-acquired MRSA has been increasing.25, 26, 27 The second finding was that the trend in the overall consumption of anti-MRSA drugs (ABK) significantly decreased. TEIC and LZD use remained stable, while VCM use significantly increased. The third finding was that the high susceptibilities of MRSA to VCM and TEIC remained stable in the study periods, and the trend in the susceptibilities to ABK and LZD significantly increased. Furthermore, our data revealed a good association between the susceptibility rates of MRSA and the consumption of TEIC, ABK and LZD. This finding indicated that the decrease in total antibiotic use was significant and might be the main trigger of improved drug susceptibility. These results suggest that the enhanced support of the infection control team at the Kobe University Hospital has been effective of this time period because of the intervention of these drug uses, the reports of MRSA isolations and their susceptibilities to these drugs. Infection control team was established in 2002, to prevent the occurrence and spread of hospital-acquired infection in our hospital.
Other studies have reported that MRSA prevalence was associated with the use of antibiotics containing glycopeptides.28, 29 From 1996 to 2003, a noticeable rise in MRSA was significantly correlated with the increased consumption of glycopeptides, and switching to other anti-MRSA drugs, such as daptomycin, was recommended.27 Recently Meyer et al.29 reported on trends in MRSA resistance and glycopeptides consumption in Germany from 2001 to 2008.28 Surveillance of antibiotic-resistant bacteria isolation rates and changes in drug susceptibility are critical information for hospital infection control. Our results of decreased isolation rate of MRSA and increased use of VCM with keeping good susceptibilities to VCM possibly may be valued as the following points: (1) the physicians who take care that infected patients tended to use VCM as the initial antibiotic treatment more often than before once MRSA infection was suspected, partly owing to the intervention by infection control team and spread of VCM therapeutic drug monitoring report; and (2) this trend and treatment finally led to inhibition of MRSA isolation.30, 31
There were some limitations to this study. This study was a retrospective study and included all the isolates obtained from the hospital, meaning that the culture test orders depended on the physicians’ discretion and no interventions were included.
In conclusion, we found increased use of anti-MRSA drugs and good susceptibilities (almost 100%) to anti-MRSA drugs, and decreased MRSA isolation over a 5-year period. This may suggest the possibilities that appropriate and early use of anti-MRSA drugs may cause these results. Further surveillance will be necessary to monitor MRSA isolation and the consumption of anti-MRSA drugs, to maintain good susceptibilities of MRSA to anti-MRSA drugs.
Methods
MRSA bacteria
The materials were MRSA isolated during the period between January 2007 and December 2011 in our institution. Isolates were taken from samples of urine, sputum, blood, nasal secretions or pus. The bacteria were from the isolation of 105 or more colony-forming units per ml in urine specimens, 1 or more colonies in 10 ml of blood in blood specimens, 1 or more colonies in sputum specimens, 1 or more colonies per plate in nasal secretions and 1 or more colonies in pus specimens.
Anti-MRSA drug use
We totaled the amount of anti-MRSA drugs (VCM, TEIC, ABK and LZD) used every month whole in the hospital based on the calculation of the number of vials ordered in the hospital pharmacy. These monthly data on anti-MRSA drug use were obtained from the computerized pharmacy databases. Consumption was expressed as DDD and normalized per 1000 patient-days. The DDD are the standard adult daily dose of an antimicrobial agent for a 1-day treatment defined by the World Health Organization.32
Susceptibility testing
Bacterial susceptibility tests to anti-MRSA drugs were performed, and the results were interpreted and reported using the reference broth microdilution method as described by the Clinical and Laboratory Standards Institute.33 Minimal inhibitory concentration was defined as the lowest antimicrobial concentration that totally inhibited bacterial growth. Susceptibilities were evaluated by the Clinical and Laboratory Standards Institute category, and we tested bacterial strains against the following anti-MRSA drugs: VCM, TEIC, ABK and LZD. Susceptibility data were analyzed for each year. S. aureus ATCC29213 was used for quality control.
Statistical analyses
Statistical analysis was conducted using linear regression analysis with the PASW Statistics 17.0 software package (for Windows; SPSS, Chicago, IL, USA). The trends in MRSA isolation rate and annual consumption of antimicrobial agents were analyzed for each month, and the susceptibility of isolated strains to antimicrobial agents was analyzed for each year. Statistical significance was established at the 0.05 level.
References
Harbarth, S. & Samore, M. H. Antimicrobial resistance determinants and future control. Emerg. Infect. Dis. 11, 794–801 (2005).
Goossens, H., Ferech, M., Vander Stichele, R. & Elseviers, M., ESAC Project Group Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet 365, 579–587 (2005).
Givney, R., Vickery, A., Holliday, A., Pegler, M. & Benn, R. Evolution of an endemic methicillin-resistant Staphylococcus aureus population in an Australian hospital from 1967 to 1996. J. Clin. Microbiol. 36, 552–556 (1998).
Hiramatsu, K., Cui, L., Kuroda, M. & Ito, T. The emergence and evolution of methicillin-resistant Staphylococcus aureus. Trends Microbiol. 9, 486–493 (2001).
Muto, C. A. et al. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect. Control Hosp. Epidemiol. 24, 362–386 (2003).
Shlaes, D. M. et al. Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: guidelines for the prevention of antimicrobial resistance in hospitals. Clin. Infect. Dis. 25, 584–599 (1997).
Fridkin, S. K. et al. Determinants of vancomycin use in adult intensive care units in 41 United States hospitals. Clin. Infect. Dis. 28, 1119–1125 (1999).
Reynolds, R. et al. Lack of upward creep of glycopeptide MICs for methicillin-resistant Staphylococcus aureus (MRSA) isolated in the UK and Ireland 2001-07. J. Antimicrob. Chemother. 67, 2912–2918 (2012).
Yanagihara, K. et al. Antimicrobial susceptibility and molecular characteristics of 857 methicillin-resistant Staphylococcus aureus isolates from 16 medical centers in Japan (2008-2009): nationwide survey of community-acquired and nosocomial MRSA. Diagn. Microbiol. Infect. Dis. 72, 253–257 (2012).
Charles, P. G., Ward, P. B., Johnson, P. D., Howden, B. P. & Grayson, M. L. Clinical features associated with bacteremia due to heterogeneous vancomycin-intermediate Staphylococcus aureus. Clin. Infect. Dis. 38, 448–451 (2004).
Howden, B. P. et al. Treatment outcomes for serious infections caused by methicillin-resistant Staphylococcus aureus with reduced vancomycin susceptibility. Clin. Infect. Dis. 38, 521–528 (2004).
Soriano, A. et al. Influence of vancomycin minimum inhibitory concentration on the treatment of methicillin-resistant Staphylococcus aureus bacteremia. Clin. Infect. Dis. 46, 193–200 (2008).
Finks, J. et al. Vancomycin-resistant Staphylococcus aureus, Michigan, USA, 2007. Emerg. Infect. Dis. 15, 943–945 (2009).
Nannini, E., Murray, B. E. & Arias, C. A. Resistance or decreased susceptibility to glycopeptides, daptomycin, and linezolid in methicillin-resistant Staphylococcus aureus. Curr. Opin. Pharmacol. 10, 516–521 (2010).
Steinkraus, G., White, R. & Friedrich, L. Vancomycin MIC creep in non-vancomycin-intermediate Staphylococcus aureus (VISA), vancomycin-susceptible clinical methicillin-resistant S. aureus (MRSA) blood isolates from 2001-05. J. Antimicrob. Chemother. 60, 788–794 (2007).
Rybak, M. J. et al. Characterization of vancomycin-heteroresistant Staphylococcus aureus from the metropolitan area of Detroit, Michigan, over a 22-year period (1986 to 2007). J. Clin. Microbiol. 46, 2950–2954 (2008).
Sakoulas, G. & Moellering, R. C. Increasing antibiotic resistance among methicillin-resistant Staphylococcus aureus strains. Clin. Infect. Dis. 46, S360–S367 (2008).
Monnet, D.L. Methicillin-resistant Staphylococcus aureus and its relationship to antimicrobial use: possible implications for control. Infect. Control Hosp. Epidemiol. 19, 552–559 (1998).
Gu, B., Kelesidis, T., Tsiodras, S., Hindler, J. & Humphries, R. M. The emerging problem of linezolid-resistant Staphylococcus. J. Antimicrob. Chemother. 68, 4–11 (2013).
Kos, V. N. et al. Comparative genomics of vancomycin-resistant Staphylococcus aureus strains and their positions within the clade most commonly associated with Methicillin-resistant S.aureus hospital-acquired infection in the United States. MBio. 3, e00112–e00112 (2012).
van Hal, S. J. & Paterson, D. L. New Gram-positive antibiotics: better than vancomycin? Curr. Opin. Infect. Dis. 24, 515–520 (2011).
Vilhena, C. & Bettencourt, A. Daptomycin: a review of properties, clinical use, drug delivery and resistance. Mini Rev. Med. Chem. 12, 202–209 (2012).
Roberts, J. A. & Lipman, J. Antibacterial dosing in intensive care: pharmacokinetics, degree of disease and pharmacodynamics of sepsis. Clin. Pharmacokinet. 45, 755–773 (2006).
Yamazaki, S. et al. Unexpected serum level of vancomycin after oral administration in a patient with severe colitis and renal insufficiency. Int. J. Clin. Pharmacol. Ther. 47, 701–706 (2009).
Coombs, G. W. et al. Prevalence of MRSA strains among Staphylococcus aureus isolated from outpatients, 2006. Commun. Dis. Intell. 33, 10–20 (2009).
Moellering, R. C. Current treatment options for community-acquired methicillin-resistant Staphylococcus aureus infection. Clin. Infect. Dis. 46, 1032–1037 (2008).
NeVille-Swensen, M. & Clayton, M. Outpatient management of community-associated methicillin-resistant Staphylococcus aureus skin and soft tissue infection. J. Pediatr. Health Care 25, 308–315 (2011).
Hsueh, P. R., Chen, W. H., Teng, L. J. & Luh, K. T. Nosocomial infections due to methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci at a university hospital in Taiwan from 1991 to 2003: resistance trends, antibiotic usage and in vitro activities of newer antimicrobial agents. Int. J. Antimicrob. Agents 26, 43–49 (2005).
Meyer, E., Schwab, F., Schroeren-Boersch, B. & Gastmeier, P. Dramatic increase of third-generation cephalosporin-resistant E. coli in German intensive care units: secular trends in antibiotic drug use and bacterial resistance, 2001 to 2008. Crit. Care 14, R113 (2010).
Niwa, T. et al. Outcome measurement of extensive implementation of antimicrobial stewardship in patients receiving intravenous antibiotics in a Japanese university hospital. Int. J. Clin. Pract. 66, 999–1008 (2012).
Sekimoto, M. et al. Impact of hospital accreditation on infection control programs in teaching hospitals in Japan. Am. J. Infect. Control 36, 212–219 (2008).
World Health Organization WHO Global Strategy for Containment of Antimicrobial Resistance. WHO/CDS/CSR/DRS/2001.2 (2001).
Clinical Laboratory Standards Institute.. Performance Standards for Antimicrobial Susceptibility Testing: Seventh Informational Supplement M100-S20, CLSI, Wayne: Pennsylvania, USA, (2010).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shigemura, K., Osawa, K., Mukai, A. et al. Anti-MRSA drug use and antibiotic susceptibilities of MRSA at a university hospital in Japan from 2007 to 2011. J Antibiot 66, 273–276 (2013). https://doi.org/10.1038/ja.2013.14
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2013.14
Keywords
This article is cited by
-
Euvesperins A and B, new circumventors of arbekacin resistance in MRSA, produced by Metarhizium sp. FKI-7236
The Journal of Antibiotics (2016)
-
Synthesis and antibacterial activity of 4″ or 6″-alkanoylamino derivatives of arbekacin
The Journal of Antibiotics (2015)
-
Optimal vancomycin doses for methicillin-resistant Staphylococcus aureus infection in urological renal dysfunction patients
International Urology and Nephrology (2015)