Abstract
Background:
Solid epidemiological evidences connect obesity with incidence, stage and survival in pancreatic cancer. However, the underlying mechanistic basis linking adipocytes to pancreatic cancer progression remain largely elusive. We hypothesized that factors secreted by adipocytes could be responsible for epithelial-to-mesenchymal transition (EMT) induction and, in turn, a more aggressive phenotype in models of pancreatic preneoplastic lesions.
Methods:
We studied the role of factors secreted by two adipogenic model systems from primary human bone marrow stromal cells (hBMSCs) in an in vitro experimental cell transformation model system of human pancreatic ductal epithelial (HPDE) cell stably expressing activated KRAS (HPDE/KRAS),
Results:
We measured a significant induction of EMT and aggressiveness in HPDE and HPDE/KRAS cell lines when cultured with medium conditioned by fully differentiated adipocytes (ADIPOCM) if compared with the same cells cultured with medium conditioned by hBMSC (hBMSCCM) from two different healthy donors. Several genes coding for soluble modulators of the non-canonical WNT signaling pathway, including FRZB, SFRP2, RSPO1, WNT5A and 5B were significantly overexpressed in fully differentiated adipocytes than in their respective in hBMSC. ADIPOCM induced the overexpression and the nuclear translocation of the Frizzled family member receptor tyrosine kinase-like orphan receptor (Ror) 2 in HPDE and HPDE/KRAS cells. Vantictumab, an anti-Frizzled monoclonal antibody, reduced ROR2 nuclear translocation and in turn the EMT and aggressiveness in HPDE and HPDE/KRAS cells.
Conclusions:
We demonstrated that adipocytes could induce EMT and aggressiveness in models of pancreatic preneoplastic lesions by orchestrating a complex paracrine signaling of soluble modulators of the non-canonical WNT signaling pathway that determine, in turn, the activation and nuclear translocation of ROR2. This signaling pathway could represent a novel target for pancreatic cancer chemoprevention. Most importantly, these factors could serve as novel biomarkers to select a risk population among obese subjects for screening and, thus, early diagnosis of pancreatic cancer.
Similar content being viewed by others
Introduction
Cancer and obesity are the two major epidemics of the 21th century.1 Pancreatic cancer is the fourth leading cause of cancer-related mortality among adults in the developed countries.2 The poor prognosis for patients with pancreatic cancer could be mainly attributed to its aggressive course, the limited efficacy of available systemic treatments, and, in particular, to the invariable metastatic behavior demonstrated along the progression of the disease.3 Thus, the identification of the earliest molecular events responsible for the metastatic dissemination of pancreatic cancer remains critical for early diagnosis, prevention and treatment interventions.4–6 Solid evidences supporting the model that metastasis is an early event in pancreatic carcinogenesis have been provided by using a genetically engineered murine model of pancreatic cancer in which the pancreatic epithelial cells could be tracked during tumor progression through the expression of yellow fluorescent protein allele into the KRas plus p53 or p16 mutant background. In this model, even low-grade PanINs showed evidence of cells that have crossed the basement membrane, migrated from the glandular epithelium into the surrounding tissue and circulatory system, and seeded the liver before pancreatic cancer formation. This behavior was associated with an early epithelial-to-mesenchymal transition (EMT) genetic program in the premalignant lesions.7
Several epidemiological studies demonstrated positive associations between the prevalence of obesity as judged by increased body mass index, cancer incidence,8 poorer treatment outcome, worsened prognosis and increased cancer-related mortality.9 Pancreatic cancer obeys this rule, as several studies reported elevated risks of developing this tumor in obese individuals compared with individuals with a normal weight.10, 11 In particular, a recent prospective cohort study demonstrated that higher prediagnostic body mass index was associated with a significantly decreased survival among patients with pancreatic cancer. This association was stronger for body mass index measured a greater number of years before cancer diagnosis, suggesting that chronic exposure to the consequences of obesity may be important in affecting patient survival. More interestingly, this study prospectively demonstrated a statistically significant association between prediagnostic body mass index and cancer stage, with more obese patients presenting with metastatic disease than patients with healthy weight.12
Although the epidemiological evidence connecting obesity with cancer incidence is strong, the underlying mechanistic basis linking obesity per se to tumor-initiating events remains largely elusive.13, 14 Three main mechanistic connections have been proposed for this association, including the antiapoptotic effects of obesity-associated hyperinsulinemia, the enhanced aromatization of sex steroids in adipose tissue, and the elaboration of paracrine and endocrine factors, or adipokines, which promote either tumorigenesis or angiogenesis directly from adipocytes and stromal cells within fat pads.15, 16 However, a comprehensive analysis aimed to directly identify the actual adipokines responsible for the paracrine molecular networks linking obesity and cancer progression has not been performed before.
In this present study, we hypothesized that factors secreted by adipocytes could be responsible for EMT induction and, in turn, a more aggressive phenotype in models of pancreatic preneoplastic lesions, representing the molecular mechanisms linking obesity with pancreatic cancer progression.
Materials and methods
Cell lines and reagents
Human papillomavirus type 16 early gene 6 and 7-immortalized human pancreatic ductal epithelial (HPDE) non-tumorigenic cells stably expressing activated KRAS (HPDE/KRAS) have been previously described in Carbone et al.17 The HPDE were routinely cultured in keratinocyte serum-free medium supplemented by epidermal growth factor and bovine pituitary extract (Life Technologies, Inc., Grand Island, NY, USA). Cell lines used in this study were authenticated using DNA fingerprinting at the genomic core facility at Wayne State University (2009) and tested for mycoplasma contamination. Vantictumab (OMP-18R5) was purchased by OncoMed Pharmaceuticals, (Redwood City, CA, USA) and was used at 1 μg ml–1.
Isolation and adipogenic differentiation of hBMSCs
hBMSCs were isolated and described as in Di Trapani et al.18 Briefly, human bone marrow stromal cells (hBMSCs) were isolated from bone marrow aspirates of healthy donors (informed consent, approved by Ethical Committee of Azienda Ospedaliera Universitaria Integrata Verona; N. 1828, 12 May 2010- “Institution of cell and tissue collection for biomedical research in Onco-Hematology”). Bone marrow aspirates were cultured in 225-cm2 flasks at 5 × 105 nucleated cells cm–2 concentration in alpha-minimal essential medium, 10% heat-inactivated fetal bovine serum, 100 U ml–1 penicillin and 100 μg ml–1 streptomycin (all from Gibco, ThermoFisher Scientific, Waltham, MA, USA). After 72 h, nonadherent cells were removed and the medium was replaced twice a week. Published protocol was followed to induce adipogenic differentiation of hBMSCs.19 hBMSCs were cultured at a density of 5000–6000 cells cm–2. After reaching confluence, hBMSCs were cultured for 1 more week and induced in adipogenic medium containing 0.5 mM isobutyl-methylxanthine (Sigma-Aldrich), 1 μM dexamethasone (Sigma-Aldrich, Missouri, MO, USA), 10 μM insulin (Roche, Basel, Switzerland), 100 μM indomethacin (Sigma-Aldrich) for 3 days and maintained in medium with 10 μM insulin for 1 day. The treatment was repeated four times, after which the cells were washed three times with phosphate-buffered saline and maintained in Dulbecco's modified Eagle's medium without fetal bovine serum for 4 days. The conditional medium was collected, centrifuged.
Isolation of adipocytes from healthy donor
Subcutaneous white adipose tissue was harvested from a healthy, 40-year-old subject with a body mass index of 23.8 kg m–2, and without diabetes and other metabolic or cardiac disorders, by a protocol optimized by Rigotti and colleagues.20 Lipoaspirate purification was obtained by the use of MACS adipose tissue dissociation kit following the manufacturer's instructions. Cellular suspension was filtered and placed in culture in Dulbecco's modified Eagle's medium added with 1% penicillin–streptomicin mixture (1:1 v/v), 10% of fetal bovine serum, 0.3% of amphotericin B and incubated for 48 h at 37 °C and 5% of CO2.
Oil red O staining
Cells were washed three times with phosphate-buffered saline and then fixed for 2 min with 3.7% formaldehyde. Oil red O (0.5% in isopropanol) was diluted with water (3:2) filtered through a 0.45 μm filter and incubated with the fixed cells for 1 h at room temperature. Cells were washed with water and the stained fat droplets in the cells were visualized by light microscopy and photographed.
Cell proliferation assay and western blotting
On day 0, 1.0 × 103 cells per well were seeded in 96-well plates. At the indicated hours, sulforhodamine B (Sigma, St Louis, MO, USA) assay was used to obtain relative estimates of viable cell number as previously described in Piro et al.21 Western blot analyses were carried out as described previously in Melisi et al.22 Briefly, cell lines were washed twice with cold phosphate-buffered saline and lysed at 4 °C into RIPA buffer (50 mM Tris–HCl, pH 8, 150 mM NaCl, 1% Nonidet P-40, 0.5% sodium deoxycholate and 0.1% sodium dodecyl sulfate) plus protease inhibitor mix (Sigma-Aldrich). Each lysate was separated by sodium dodecyl sulfate–polyacrylamide gel electrophoresis and probed with antibodies against E-cadherin, β-catenin (Abcam, Cambridge, UK), receptor tyrosine kinase-like orphan receptor 2 (ROR2), Histone H3, glycogen synthase kinase 3α/β (GSK3α/β) and p-GSK3β-(S9) (Cell Signaling Technology, Boston, MA, USA), vimentin (Dako, Glostrup, Denmark), glyceraldehyde-3-phosphate dehydrogenase (GAPDH) and γ-tubulin (Santa Cruz Biotechnology, Santa Cruz, CA, USA). Immunoreactive proteins were detected using an enhanced-chemiluminescence reagent (Millipore, Billerica, MA, USA) according to the manufacturer’s instructions. Images were captured by LAS4000 Digital Image Scanning System (GE Healthcare, Little Chalfont, UK).
Reverse transcription-PCR and real-time PCR
RNA was isolated by Trizol reagent as manufacturer’s instructions (Invitrogen, Carlsbad, CA, USA). Reverse transcription-PCR assay was performed accordingly with the High capacity cDNA reverse transcription kit (Applied Biosystems, Foster City, CA, USA) as previously described in Piro et al.23 The mRNA expression of CDH1, Vimentin, Leptin, ADIPOQ, WNT5A, WNT5B, FRZB, ZEB1, SFRP2, DKK1, DKK2 and DKK3 was quantified by using a SYBR green based real-time PCR analysis and the ABI Prism 7900 HT Sequence Detection System (Applied Biosystems). Each gene was tested in each cell line in four replicates and three independent experiments were performed. To quantify the relative changes in gene expression, the 2-ΔΔCT method was used and reactions were normalized to endogenous control gene β-actin expression levels.
Immunofluorescence
Immunofluorescence analyses were carried out as described previously in Carbone et al.24, 25 Briefly, HPDE cell lines were cultured for 24 h on cover slips in a 24-multi-well plate. The cells were harvested and the medium completely replaced with hBMSCCM, ADIPOCM with or without vantictumab. After 24 h, cells were fixed with 2.5% formalin and permeabilized with 0.1% Triton for 10 min at 4 °C. The cells were then incubated with the primary antibody specific for ROR2 (Abcam) or frizzled class receptor (FZD) for 1 h at room temperature and with fluorophore (FITC) or AlexaFluor546-conjugated as secondary antibody (Invitrogen). Nuclei were stained with To-Pro-3 (Invitrogen). Cover slips were mounted with pro-long antifade mountant (Invitrogen). The images were obtained with a confocal microscopy (LMS510, Zeiss, Oberkochen, Germany).
Wound-healing and transwell invasion assay
Wound-healing assay was performed as previously described in Carbone et al.17 and Dalla Pozza et al.26 Briefly, HPDE in vitro cell transformation model systems were seeded at 70% of confluence in 100 mm cell culture dishes. After 24 h, medium was completely replaced with hBMSCCM or ADIPOCM. After 48 h, a straight scratch was made using a pipette tip to simulate a wound. The cells were washed gently with cold PBS (PBS1X) and rinsed with hBMSCCM or ADIPOCM. Photographs of at least five different points were taken immediately and after 24 h of culture. In vitro invasion assay were performed using 24-well transwell unit with polycarbonate filters (Corning Costar, Cambridge, MA, USA). HPDE were suspended at density of 5 × 105/ml in culture medium and then placed in the upper part of transwell. Meanwhile, conditional medium from hBMSC and adipocyte cells with or without vantictumab (1 μg ml–1) were added at the lower wells of the chambers. Cells were incubated for 24 h, fixed with ethanol and stained with 0.05% Crystal violet for 30 min. Cells in the upper chamber were removed with cotton swab. Cells that invaded through the Matrigel (MatrigelTM Basement Membrane Matrix, BD Biosciences, Franklin Lakes, NK, USA) to the underside of the filters were counted and picture taken under a Leica DMIL-Led microscope equipped with a Leica EC3 camera (Leica, Wetzlar, Germany). Three invasion chambers were used for treated and untreated group. The values obtained were calculated by averaging the total number of the cells from three filters. All experiments were performed in triplicate.
Gene expression microarray and pathway analysis
Differences in gene expression between cell lines were examined using Illumina Human 44k gene chips (Illumina, Milan, Italy). Briefly, synthesis of complementary DNA and biotinylated complementary RNA was performed using the IlluminaTotalPrep RNA Amplification Kit (Ambion, ThermoFisher Scientific, Waltham, MA, USA), according to the manufacturer’s protocol using 500 ng of total RNA. Hybridization of complementary RNAs (750 ng) was carried out using Illumina Human 48 k gene chips (Human HT-12 V4 BeadChip). Array washing was performed using Illumina High Temp Wash Buffer for 10’ at 55 °C, followed by staining using streptavidin-Cy3 dyes (Amersham Biosciences, Buckinghamshire, UK). Probe intensity data were obtained using the Illumina Genome Studio software (Genome Studio V2011.1, San Diego, CA, USA). Raw data were loess normalized with the Lumi R package (https://bioconductor.org/biocLite.R) and further processed with Excel software. Each microarray experiment was repeated twice. Differentially expressed transcripts were tested for network and functional interrelatedness using the IPA software program (Ingenuity Systems, Redwood, CA, USA). Gene expression microarray data have been deposited in the GEO database with accession number (GSE104536).
Statistical analysis
All results were expressed as the 95% confidence interval for at least three independent experiments performed in triplicate. All of the statistical analyses were performed using the GraphPad Prism software program (version 4.0c; GraphPad Software, La Jolla, CA, USA).
Results
Adipocytes secreted factors induce EMT and aggressiveness in in vitro models of pancreatic preneoplastic lesions
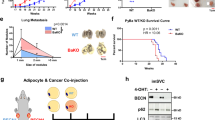
Initially, we established two adipogenic models from hBMSCs from healthy donors. hBMSC were grown in culture media able to induce hBMSC differentiation into mature and functionally active adipocytes, as confirmed by the formation of small cytoplasmic lipid droplets by light microscopy analysis and Oil Red O staining (Figure 1a). To further confirm adipocytes differentiation, we measured a significant increasing expression of ADIPOQ and leptin genes in hBMSC, pre-adipocytes and fully differentiated adipocytes (Figure 1b).
Adipocytes secreted factors induce EMT and aggressiveness in in vitro models of pancreatic preneoplastic lesions. (a) Isolation and adipogenic differentiation of hBMSCs. The morphology of adherent hBMSCs and adipogenic differentiation. The accumulation of cytoplasmic triglycerides was detected by Oil Red O staining and visualized under a microscope. (b) Quantitative real-time PCR analysis of leptin (Lep) and adiponectin (ADIPOQ) along adipogenic differentiation. The values represent the fold change in RNA expression between the gene of interest and b-actin. (c) Western blot analysis of EMT marker vimentin in HPDE models cultured with conditional medium (CM) from hBMSC (hBMSCCM) and adipocytes (ADIPOCM). γ-Tubulin was used as loading control. (d) Cell proliferation assay of HPDE and HPDE/KRAS cell lines cultured with the conditional medium from hMBSC and adipocytes. The mean values and 95% confidence interval (CI) from three independent experiments done in quadruplicate are shown. (e) Levels of cell migration in HPDE and HPDE/KRAS cell lines co-cultured with hBMSC and adipocytes. The mean values and 95% CI from three independent experiments done in quadruplicate are shown. ***P<0.001 by two-tailed unpaired Student’s t-tests. Photographs of the wound area were taken by using phase-contrast microscopy immediately at indicated time point after the incision. All these experiments were performed by using hBMSC isolated from the healthy donor 1 (#1) and its relative adipocytes.
To test the hypothesis that factors secreted by adipocytes could be responsible for EMT and aggressiveness of pancreatic preneoplastic lesions, we used an in vitro experimental cell transformation models consisting in the stable expression of activated KRAS (HPDE/KRAS) in HPDE cell line. These cell lines were cultured with medium conditioned by hBMSC (hBMSCCM), or by fully differentiated adipocytes (ADIPOCM). We measured a significantly higher expression of the mesenchymal marker vimentin in HPDE and HPDE/KRAS cell lines when cultured with ADIPOCM if compared with the same cells cultured with hBMSCCM from two different healthy donors (Figure 1c and Supplementary Figure 1). We measured significantly higher proliferation rates in HPDE and HPDE/KRAS cells cultured with ADIPOCM compared with hBMSCCM (Figure 1d). Moreover, we measured also a significantly higher migration rate of these cell lines when co-cultured with adipocytes cells compared with hBMSC control cells at early time points when the differences in proliferation were negligible (Figure 1e). Interestingly, in co-cultured conditions this effect was more evident for HPDE/KRAS cells with respect to HPDE control cells (Supplementary Figure S2).
To further confirm that adipose tissue could be responsible for pancreatic preneoplastic lesions aggressiveness, we established primary adipocytes culture from the white adipose tissue of a healthy subject (primary-ADIPO) (Supplementary Figure S3A). To validate that factors secreted by primary adipocytes could be responsible for EMT and aggressiveness of pancreatic preneoplastic lesions, HPDE and HPDE/KRAS cells were cultured with conditioned medium from primary-ADIPO (primary-ADIPOCM). We measured a significantly higher expression of the mesenchymal marker vimentin in HPDE and HPDE/KRAS cell lines when cultured with primary-ADIPOCM if compared with the same cells cultured with control medium (Supplementary Figure S3B). Moreover, we measured also a significantly higher migration rate of these cell lines when cultured with primary-ADIPOCM compared with control medium (Supplementary Figure S3C).
Adipocytes sustain pancreatic preneoplastic lesions aggressiveness through a WNT paracrine network
In order to identify the factors secreted by adipocytes that could be responsible for accelerating EMT in the pancreatic preneoplastic models, we compared gene expression profiles and narrowed our analysis to genes coding for proteins in the extracellular space that exhibited significantly higher expression in fully differentiated adipocytes than in their respective in hBMSC from two healthy donors. We found an overexpression of several genes coding for soluble modulators of the non-canonical WNT signaling pathway, including FRZB, SFRP2, RSPO1, WNT5A and 5B. Moreover, we measured the significant downregulation of genes encoding for members of the Dickkopf family proteins—DKK1, 3—that are known to antagonize WNT canonical pathway (Figures 2a and b). Consistently, we found a higher inhibitory phosphorylation of GSK3 in HPDE and HPDE/KRAS cells cultured with ADIPOCM compared with hBMSCCM (Figures 2c and d).
Adipocytes sustain pancreatic preneoplastic lesions aggressiveness through a WNT paracrine network. (a) Interaction network derived from secreted genes upregulated in adipocytes versus the hBMSC cells from two healthy donors. Each interaction is supported by at least one literature reference identified in the Ingenuity Pathway Knowledge Base, with solid lines representing direct interactions and dashed lines representing indirect interactions. In the heat map shown in this figure, the logarithms of the gene expression levels are shown in colors (green=decreased expression, red=increased expression). (b) Quantitative real-time PCR gene expression analysis of WNT5A, WNT5B, RSPO1, DKK1, DKK2, DKK3, SFRP2 and FRZB in hBMSC and relative adipocytes from two healthy donor (#1 and #2). The result values represent the values of the fold change in RNA expression between the gene of interest and b-actin. The mean values and 95% CI from three independent experiments done in quadruplicate are shown. ***P<0.001, **P<0.005 and *P<0.05, by two-tailed unpaired Student’s t-tests. (c, d) Western blot analysis for GSK3β and phospho-GSK3 β in HPDE and HPDE/KRAS cells cultured with conditional medium (CM) from hBMSC (hBMSCCM) or adipocytes (ADIPOCM) from two healthy donor. γ-Tubulin was used as loading control. The relative protein quantification, using ImageJ software (https://imagej.nih.gov/ij/), was performed and relative GSK3 and γ-tubulin ratio are indicated.
In order to demonstrate that these adipocyte-secreted WNT factors were indeed responsible for the EMT induced in HPDE cells, we used vantictumab, a monoclonal antibody directed against the extracellular portion of WNT receptors (FZDs). In this regard, we demonstrated a measurable reduction of the expression of vimentin, β-catenin and phospho-GSK3-β in HPDE and HPDE/KRAS cells when cultured with ADIPOCM and treated with vantictumab if compared with the same cells cultured with ADIPOCM and treated with a control mAb, at levels similar with those measured in the same cells cultured with hBMSCCM (Figure 3a). Consistently, we measured a significant reduction in the proliferation (Figure 3b), migration (Figure 3c) and invasion rates (Figure 3d) of HPDE and HPDE/KRAS cells when cultured with ADIPOCM and treated with vantictumab if compared with the same cells cultured with ADIPOCM and treated with mAb control. This effect was not observed in cells cultured with hBMSCCM (Figures 3b and d).
Adipocytes sustain pancreatic preneoplastic lesions aggressiveness through a WNT paracrine network. (a) Western blot analysis for Vimentin, β-catenin, phpspoGSK3 and total GSK3 of HPDE and HPDE/KRAS cultured with hBMSCCM or adipocytes (ADIPOCM) treated or untreated with vantictumab. γ-Tubulin was used as loading control. The relative protein quantification, using ImageJ software, was performed and relative GSK3 and γ-tubulin ratio are indicated. (b) Cell proliferation assay of HPDE and HPDE/KRAS cell lines cultured with the conditional medium from hMBSC and adipocytes treated or untreated with vantictumab. The mean values and 95% confidence interval (CI) from three independent experiments done in quadruplicate are shown. (c) Bar histograms of cell migration levels of HPDE and HPDE/KRAS cell lines cultured with the conditioned medium from hMBSC and adipocytes treated or untreated with vantictumab. The mean values and 95% CI from three independent experiments done in quadruplicate are shown. ***P<0.001 by two-tailed unpaired Student’s t-tests. Photographs of the wound area were taken by using phase-contrast microscopy immediately at indicated time point after the incision. All these experiments were performed using hBMSC isolated from the healthy donor 1 (#1) and its relative adipocytes. (d) Transwelll invasion assay of HPDE and HPDE/KRAS cell lines cultured with the conditioned medium from adipocytes and hBMSC control cells with or without vantictumab. The invasion chambers were used for treated and untreated group. The values obtained were calculated by averaging the total number of the cells from three filters. All experiments were performed in triplicate. The mean values and 95% CI from three independent experiments done in quadruplicate are shown. ***P< 0.001, **P<0.005, *P<0.05 and NS (Not Significative), by one-way analysis of variance and post Dunnett's mutiple comparison post test using hBMSC as control.
Collectively, these results provide strong evidences supporting a model in which the induction of an EMT phenotype in pancreatic premalignant lesions by adipocytes involve the binding of WNT proteins to the FZDs receptors.
ROR2 nuclear shuttling mediates pancreatic preneoplastic lesions aggressiveness induced by adipocytes-derived WNT paracrine factors
Ror2 is a Frizzled family protein, which belongs to the 7 trans-membrane class of receptors. Ror2 interact with several of the Wnt ligands to activate a combination of non-canonical and canonical Wnt signaling activity. In particular, WNT5A induced the formation of a complex between ROR2 and Frizzled, resulting in Ser/Thr phosphorylation of Ror2 and the recruitment of Dvl, Axin and GSK3β.27 We measured a significantly higher expression of ROR2 in HPDE and HPDE/KRAS cell lines when cultured with ADIPOCM if compared with the same cells cultured with hBMSCCM. Immunofluorescence analysis showed colocalization of FZD receptors and ROR2 in these cells. Treatment with vantictumab was able to modulate ROR2 expression and to interfere with binding of FZD with ROR2, triggering to ROR2 cellular rearrangement (Figures 4a and b).
Adipocytes-derived WNT secreted factors induced expression and cellular rearrangement of ROR2 in pancreatic preneoplastic lesions. (a) Western blot analysis for the expression of ROR2 in HPDE and HPDE/KRAS cultured with ADIPOCM and hBMSCCM treated or untreated with vantictumab. GAPDH was used as loading control. (b) Immunofluorescence colocalization analysis for ROR2 (red) and FZD (green) receptors in HPDE and HPDE/KRAS cells cultured with ADIPOCM or with hBMSCCM treated or untreated with vantictumab. Fluorescence intensity analysis was performed by ImageJ software. Fluorescence intensity analysis was performed by ImageJ software and bars represent mean±s.d. from analysis of four separate high-power field images. ***P<0.001, by two-tailed unpaired Student’s t-test.
Since recent evidences have been provided for the nuclear translocation of the other member of the ROR family, ROR1,28 we performed a bioinformatics analysis on the potential nuclear translocation of ROR2. Based on nuclear translocation sequences (NLS)-mapper software (http://nls-mapper.iab.keio.ac.jp/), we identified several NLSs that have good potential for ROR2 nuclear localization (Table 1). In this regard, we performed a western blotting and immunofluorescence analyses of ROR2 in the different cellular compartments, and we demonstrated that ADIPOCM induced not only a ROR2 overexpression but also the nuclear translocation of its 50 kDa short isoform. Treatment with vantictumab was able to modulate ROR2 expression and to interfere with its nuclear localization (Figures 5a and b).
ROR2 nuclear shuttling mediates pancreatic preneoplastic lesions aggressiveness induced by adipocytes-derived WNT paracrine factors. (a) Western blot analysis for the expression of both 105 and 50 kDA protein isoforms of ROR2 in cytosolic and nuclear compartment from HPDE and HPDE/KRAS cultured with ADIPOCM and hBMSCCM treated or untreated with vantictumab. GAPDH and Histone H3 were used as loading and cellular fraction compartment controls. (b) Immunofluorescence colocalization analysis for ROR2 (green) and nucleus (blue) in HPDE and HPDE/KRAS cells cultured with ADIPOCM or with hBMSCCM treated or untreated with vantictumab. Fluorescence intensity analysis was performed by ImageJ software.
These results suggest that the WNT paracrine factors secreted by adipocytes could sustain cell proliferation and invasion in pancreatic premalignant lesions by inducing the nuclear shuttling of ROR2.
Discussion
In this study, we demonstrated that adipocytes could induce EMT and aggressiveness in models of pancreatic preneoplastic lesions by orchestrating a complex paracrine signaling of soluble modulators of the non-canonical WNT signaling pathway that determine, in turn, the activation and nuclear translocation of ROR2.
The most compelling preclinical evidences about the link between obesity and pancreatic carcinogenesis indicated that a high-fat, high-calorie diet could accelerates early pancreatic neoplasia in the conditional K-Ras G12D mouse model.29 More recently, a complex cross-talk between adipocytes, tumor-associated neutrophils and pancreatic stellate cells has been described to promote desmoplasia, accelerate tumor growth and impair delivery/efficacy of chemotherapeutics, with interleukin-1β secreted by all these cells having a major role in this cooperation.30
Our study contributes to this field by providing evidence, through an inductive approach, of a role for several modulators of the non-canonical WNT signaling as the paracrine network between adipocytes and induction of EMT in preneoplastic pancreatic lesions. The anti-WNT receptors monoclonal antibody vantictumab was able to modulate these effects. Interestingly, EMT was established as one of the pharmacodynamic biomarker in surrogate tissues and tumor tissues from serial biopsies in the first-in-human Phase 1a study for vantictumab in patients with advanced solid tumors.31
ROR2 is a tyrosine kinase receptor with a well-established role in the activation of non-canonical WNT signaling pathways. Recent evidences showed that ROR2 was highly expressed in a number of different tumors,27 including pancreatic cancer,32 and could serve as a potential target for drug development. Depending on receptor context, WNT proteins are either able to activate the non-canonical pathway,33 and to antagonize the canonical pathway by promoting the activation of ROR1 and 2.34 In case of activation of the canonical WNT signaling, ROR2 expression is lost, supporting its role as a gatekeeper for the canonical pathway. Alternatively, in tumors driven by non-canonical WNT signaling, ROR2 expression is commonly increased and could have a critical role in driving tumorigenesis.32 In this regard, ROR2 specifically interacts only with non-canonical WNT5A35 by establishing a ligand/receptor complex including ROR2-WNT5A-FZD35, 33 In our present study, we demonstrated that WNT factors secreted by adipocytes could enhance the aggressiveness of pancreatic preneoplastic lesions through a mechanism that require the interaction of ROR2-WNT-FZD. Vantictumab reduced ROR2–FZD interaction and inhibited proliferation, migration and invasion rates of pancreatic preneoplastic lesions. Most importantly, we demonstrated for the first time the nuclear translocation of ROR2, and that vantictumab was able to inhibits its shuttling. Interestingly, tumor-derived WNT5A has also been recently indicated as responsible for a dedifferentiation process of adipocytes reprogramming toward a fibroblast-like phenotype in a model of co-culture with MiaPaCa2 pancreatic cancer and 3T3-L1 cells.36 Further investigations of this potential bidirectional cross-talk in more complex in vivo models are warranted.
This study, however, had some limitations. The effort to develop appropriate in vitro models that could closely recapitulate the cross-talk between human epithelial cells and normal adipocyte is hampered by the difficulty to directly culture and expand fully mature adipocytes. Moreover, different cell lines commonly used in the study of adipocyte biology could either derive from murine fibroblasts (3T3-L1 cells),37 or be developed from human metastatic liposarcoma (LS14 cells).38 In our study, we used two primary human adipogenic models in which bone marrow stromal cells from healthy donors were able to differentiate into mature and functionally active adipocytes. These models allowed a comparison between adipocytes and their respective undifferentiated counterparts, the only strategy to directly identify the actual secreted factors responsible for EMT induction and, in turn, a more aggressive phenotype in models of pancreatic preneoplastic lesions, an analysis that would be otherwise impossible by using only mature adipocytes. Moreover, we corroborated the clinical relevance of our findings by demonstrating that a similar induction of EMT in HPDE cells could be obtained also with conditioned medium from fully differentiated human primary adipocytes.
In conclusion, our present study demonstrated that a non-canonical WNT paracrine network secreted by adipocytes is responsible for EMT induction and, in turn, a more aggressive phenotype in models of pancreatic preneoplastic lesions, representing the molecular mechanisms linking obesity with pancreatic cancer progression. This signaling pathway could represent a novel target for pancreatic cancer chemoprevention. Most importantly, these factors could serve as novel biomarkers to select a risk population among obese subjects for screening and, thus, early diagnosis of pancreatic cancer.
References
Vucenik I, Stains JP . Obesity and cancer risk: evidence, mechanisms, and recommendations. Ann N Y Acad Sci 2012; 1271: 37–43.
Melisi D, Budillon A . Pancreatic cancer: between bench and bedside. Curr Drug Targets 2012; 13: 729–730.
Melisi D, Calvetti L, Frizziero M, Tortora G . Pancreatic cancer: systemic combination therapies for a heterogeneous disease. Curr Pharm Design 2014; 20: 6660–6669.
Vaccaro V, Sperduti I, Vari S, Bria E, Melisi D, Garufi C et al. Metastatic pancreatic cancer: is there a light at the end of the tunnel? World J Gastroenterol 2015; 21: 4788–4801.
Vaccaro V, Melisi D, Bria E, Cuppone F, Ciuffreda L, Pino MS et al. Emerging pathways and future targets for the molecular therapy of pancreatic cancer. Expert Opin Ther Targets 2011; 15: 1183–1196.
Melisi D, Piro G, Tamburrino A, Carbone C, Tortora G . Rationale and clinical use of multitargeting anticancer agents. Curr Opin Pharmacol 2013; 13: 536–542.
Rhim AD, Mirek ET, Aiello NM, Maitra A, Bailey JM, McAllister F et al. EMT and dissemination precede pancreatic tumor formation. Cell 2012; 148: 349–361.
Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M . Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet 2008; 371: 569–578.
Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ . Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med 2003; 348: 1625–1638.
Michaud DS, Giovannucci E, Willett WC, Colditz GA, Stampfer MJ, Fuchs CS . Physical activity, obesity, height, and the risk of pancreatic cancer. JAMA 2001; 286: 921–929.
Larsson SC, Orsini N, Wolk A . Body mass index and pancreatic cancer risk: a meta-analysis of prospective studies. Int J Cancer 2007; 120: 1993–1998.
Yuan C, Bao Y, Wu C, Kraft P, Ogino S, Ng K et al. Prediagnostic body mass index and pancreatic cancer survival. J Clin Oncol 2013; 31: 4229–4234.
Park J, Euhus DM, Scherer PE . Paracrine and endocrine effects of adipose tissue on cancer development and progression. Endocr Rev 2011; 32: 550–570.
Duong MN, Geneste A, Fallone F, Li X, Dumontet C, Muller C . The fat and the bad: mature adipocytes, key actors in tumor progression and resistance. Oncotarget 2017; 8: 57622–57641.
Rosen ED, Spiegelman BM . What we talk about when we talk about fat. Cell 2014; 156: 20–44.
Himbert C, Delphan M, Scherer D, Bowers LW, Hursting S, Ulrich CM . Signals from the adipose microenvironment and the obesity-cancer link-a systematic review. Cancer Prev Res (Phila) 2017; 10: 494–506.
Carbone C, Piro G, Fassan M, Tamburrino A, Mina MM, Zanotto M et al. An angiopoietin-like protein 2 autocrine signaling promotes EMT during pancreatic ductal carcinogenesis. Oncotarget 2015; 6: 13822–13834.
Di Trapani M, Bassi G, Ricciardi M, Fontana E, Bifari F, Pacelli L et al. Comparative study of immune regulatory properties of stem cells derived from different tissues. Stem Cells Dev 2013; 22: 2990–3002.
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD et al. Multilineage potential of adult human mesenchymal stem cells. Science 1999; 284: 143–147.
Sbarbati A, Accorsi D, Benati D, Marchetti L, Orsini G, Rigotti G et al. Subcutaneous adipose tissue classification. Eur J Histochem 2010; 54: e48.
Piro G, Giacopuzzi S, Bencivenga M, Carbone C, Verlato G, Frizziero M et al. TAK1-regulated expression of BIRC3 predicts resistance to preoperative chemoradiotherapy in oesophageal adenocarcinoma patients. Br J Cancer 2015; 113: 878–885.
Melisi D, Ossovskaya V, Zhu C, Rosa R, Ling J, Dougherty PM et al. Oral poly(ADP-ribose) polymerase-1 inhibitor BSI-401 has antitumor activity and synergizes with oxaliplatin against pancreatic cancer, preventing acute neurotoxicity. Clin Cancer Res 2009; 15: 6367–6377.
Piro G, Carbone C, Cataldo I, Di Nicolantonio F, Giacopuzzi S, Aprile G et al. An FGFR3 autocrine loop sustains acquired resistance to trastuzumab in gastric cancer patients. Clin Cancer Res 2016; 22: 6164–6175.
Carbone C, Piro G, Simionato F, Ligorio F, Cremolini C, Loupakis F et al. Homeobox B9 mediates resistance to anti-VEGF therapy in colorectal cancer patients. Clin Cancer Res 2017; 23: 4312–4322.
Carbone C, Piro G, Simionato F, Ligorio F, Cremolini C, Loupakis F et al. Homeobox B9 mediates resistance to anti-VEGF therapy in colorectal cancer patients. Clin Cancer Res 2017; 23: 4312–4322.
Dalla Pozza E, Dando I, Biondani G, Brandi J, Costanzo C, Zoratti E et al. Pancreatic ductal adenocarcinoma cell lines display a plastic ability to bidirectionally convert into cancer stem cells. Int J Oncol 2015; 46: 1099–1108.
Debebe Z, Rathmell WK . Ror2 as a therapeutic target in cancer. Pharmacol Ther 2015; 150: 143–148.
Tseng HC, Lyu PC, Lin WC . Nuclear localization of orphan receptor protein kinase (Ror1) is mediated through the juxtamembrane domain. BMC Cell Biol 2010; 11: 48.
Dawson DW, Hertzer K, Moro A, Donald G, Chang HH, Go VL et al. High-fat, high-calorie diet promotes early pancreatic neoplasia in the conditional KrasG12D mouse model. Cancer Prev Res (Phila) 2013; 6: 1064–1073.
Incio J, Liu H, Suboj P, Chin SM, Chen IX, Pinter M et al. Obesity-induced inflammation and Desmoplasia promote pancreatic cancer progression and resistance to chemotherapy. Cancer Discov 2016; 6: 852–869.
Smith DC, Rosen L, Wang M, Zhang C, Xu L, Chugh R et al. Abstract B24: biomarker analysis in the first-in-human phase 1a study for vantictumab (OMP-18R5; anti-Frizzled) demonstrates pharmacodynamic (PD) modulation of the Wnt pathway in patients with advanced solid tumors. Mol Cancer Ther 2013; 12 (11 Supplement): B24–B24.
Huang J, Fan X, Wang X, Lu Y, Zhu H, Wang W et al. High ROR2 expression in tumor cells and stroma is correlated with poor prognosis in pancreatic ductal adenocarcinoma. Sci Rep 2015; 5: 12991.
Grumolato L, Liu G, Mong P, Mudbhary R, Biswas R, Arroyave R et al. Canonical and noncanonical Wnts use a common mechanism to activate completely unrelated coreceptors. Genes Dev 2010; 24: 2517–2530.
Ho HY, Susman MW, Bikoff JB, Ryu YK, Jonas AM, Hu L et al. Wnt5a-Ror-dishevelled signaling constitutes a core developmental pathway that controls tissue morphogenesis. Proc Natl Acad Sci USA 2012; 109: 4044–4051.
Mikels AJ, Nusse R . Purified Wnt5a protein activates or inhibits beta-catenin-TCF signaling depending on receptor context. PLoS Biol 2006; 4: e115.
Zoico E, Darra E, Rizzatti V, Budui S, Franceschetti G, Mazzali G et al. Adipocytes WNT5a mediated dedifferentiation: a possible target in pancreatic cancer microenvironment. Oncotarget 2016; 7: 20223–20235.
Green H, Meuth M . An established pre-adipose cell line and its differentiation in culture. Cell 1974; 3: 127–133.
Hugo ER, Brandebourg TD, Comstock CE, Gersin KS, Sussman JJ, Ben-Jonathan N . LS14: a novel human adipocyte cell line that produces prolactin. Endocrinology 2006; 147: 306–313.
Acknowledgements
Part of the work was performed at the Laboratorio Universitario di Ricerca Medica (LURM) Research Center, University of Verona. We thank Dr Marzia Di Chio at the Department of Diagnostic and Public Health, University of Verona for technical execution of immunofluorescence analyses. This work was supported by the Investigator grant no. 19111 to DM and no. 18599 to GT through the Associazione Italiana per la Ricerca sul Cancro (AIRC), by the Basic Research Project 2015 through the University of Verona to DM, and by the Nastro Viola patients’ association donations to DM.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Carbone, C., Piro, G., Gaianigo, N. et al. Adipocytes sustain pancreatic cancer progression through a non-canonical WNT paracrine network inducing ROR2 nuclear shuttling. Int J Obes 42, 334–343 (2018). https://doi.org/10.1038/ijo.2017.285
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.285