Abstract
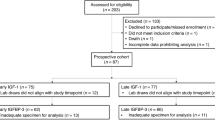
Low birth weight followed by rapid postnatal weight gain is associated with increased risks for obesity and diabetes in adulthood. Modulation of glucagon-like-peptide 1 (GLP-1) secretion by (epi)genetic mechanisms or nutrition may, in part, influence this risk. Formula-fed infants born small-for-gestational-age (SGA) have higher circulating GLP-1 at age 4 months than breastfed SGA or appropriate-for-gestational-age (AGA) infants. Here we assessed GLP-1 concentrations in healthy AGA (n=149) and SGA (n=107) subjects at age 12 months and their association with endocrine-metabolic and body composition parameters and GLP-1 receptor (GLP-1R) rs6923761 and rs3765467 polymorphisms. At birth, cord GLP-1 concentrations were comparable in AGA and SGA infants. At age 12 months, insulin-like growth factor I (IGF-I) and GLP-1 levels were higher than at birth; SGA infants displayed higher IGF-I and GLP-1 concentrations than AGA infants (both P<0.001) that were unrelated to neonatal nutrition or GLP-1R genotype and that were paralleled by a significant increase in weight Z-score (P<0.001 vs AGA). In conclusion, SGA infants have augmented IGF-I and prefeeding GLP-1 concentrations in late infancy. Increased GLP-1 levels may impair hypothalamic and/or peripheral GLP-1R signaling, exert long-term negative effects on the hypothalamic nuclei regulating energy homeostasis and increase the risks for obesity and diabetes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Leunissen RW, Kerkhof GF, Stijnen T, Hokken-Koelega A . Timing and tempo of first-year rapid growth in relation to cardiovascular and metabolic risk profile in early adulthood. JAMA 2009; 30: 2234–2242.
Barker DJ, Osmond C, Forsén TJ, Kajantie E, Eriksson JG . Trajectories of growth among children who have coronary events as adults. N Engl J Med 2005; 353: 1802–1809.
Singhal A . Long-term adverse effects of early growth acceleration or catch-up growth. Ann Nutr Metab 2017; 70: 236–240.
de Zegher F, Sebastiani G, Diaz M, Gómez-Roig MD, López-Bermejo A, Ibáñez L . Breast-feeding vs formula-feeding for infants born small-for-gestational-age: divergent effects on fat mass and on circulating IGF-I and high-molecular-weight adiponectin in late infancy. J Clin Endocrinol Metab 2013; 98: 1242–1247.
Díaz M, Bassols J, Sebastiani G, López-Bermejo A, Ibáñez L, de Zegher F . Circulating GLP-1 in infants born small-for-gestational-age: breast-feeding versus formula-feeding. Int J Obes (Lond) 2015; 39: 1501–1503.
Beiroa D, Imbernon M, Gallego R, Senra A, Herranz D, Villarroya F et al. GLP-1 agonism stimulates brown adipose tissue thermogenesis and browning through hypothalamic AMPK. Diabetes 2014; 63: 3346–3358.
Steculorum SM, Collden G, Coupe B, Croizier S, Lockie S, Andrews ZB et al. Neonatal ghrelin programs development of hypothalamic feeding circuits. J Clin Invest 2015; 125: 846–858.
Koole C, Wootten D, Simms J, Miller LJ, Christopoulos A, Sexton PM . Differential impact of amino acid substitutions on critical residues of the human glucagon-like peptide-1 receptor involved in peptide activity and small-molecule allostery. J Pharmacol Exp Ther 2015; 353: 52–63.
Sathananthan A, Man CD, Micheletto F, Zinsmeister AR, Camilleri M, Giesler PD et al. Common genetic variation in GLP1R and insulin secretion in response to exogenous GLP-1 in nondiabetic subjects: a pilot study. Diabetes Care 2010; 33: 2074–2076.
Han E, Park HS, Kwon O, Choe EY, Wang HJ, Lee YH et al. A genetic variant in GLP1R is associated with response to DPP-4 inhibitors in patients with type 2 diabetes. Medicine 2016; 95: e5155.
Javorský M, Gotthardová I, Klimčáková L, Kvapil M, Židzik J, Schroner Z et al. A missense variant in GLP1R gene is associated with the glycaemic response to treatment with gliptins. Diabetes Obes Metab 2016; 18: 941–944.
Díaz M, García C, Sebastiani G, de Zegher F, López-Bermejo A, Ibáñez L . Placental and cord blood methylation of genes envolved in energy homeostasis: association with fetal growth and neonatal body composition. Diabetes 2017; 66: 779–784.
Ibáñez L, Sebastiani G, Diaz M, López-Bermejo A, Gómez-Roig MD . de Zegher F. Gender specificity of body adiposity and circulating adiponectin, visfatin, insulin and IGF-I at term birth: relation to prenatal growth. J Clin Endocrinol Metab 2008; 93: 2774–2778.
Kreymann B, Ghatei MA, Domin J, Kanse S, Bloom SR . Developmental patterns of glucagon-like peptide-1-(7-36) amide and peptide-YY in rat pancreas and gut. Endocrinology 1991; 129: 1001–1005.
Kawamori D, Shirakawa J, Liew CW, Hu J, Morioka T, Duttaroy A et al. GLP-1R signalling compensates for impaired insulin signalling in regulating beta cell proliferation in βIRKO mice. Diabetologia 2017; 60: 1442–1453.
Carlessi R, Chen Y, Rowlands J, Cruzat VF, Keane KN, Egan L et al. GLP-1R receptor signalling promotes β-cell glucose metabolism via mTOR-dependent HIF-1α activation. Sci Rep 2017; 7: 2661.
Cornu M, Modi H, Kawamori D, Kulkarni RN, Joffraud M, Thorens B . Glucagon-like peptide-1 increases beta-cell glucose competence and proliferation by translational induction of insulin-like growth factor-1 receptor expression. J Biol Chem 2010; 285: 10538–10545.
Hirasawa A, Tsumaya K, Awaji T, Katsuma S, Adachi T, Yamada M et al. Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR120. Nat Med 2005; 11: 90–94.
Hall E, Dayeh T, Kirkpatrick CL, Wollheim CB, Dekker Nitert M, Ling C . DNA methylation of the glucagon-like peptide 1 receptor (GLP1R) in human pancreatic islets. BMC Med Genet 2013; 14: 76.
Milovanovic I, Njuieyon F, Deghmoun S, Chevenne D, Levy-Marchal C, Beltrand J . SGA children with moderate catch-up growth are showing the impaired insulin secretion at the age of 4. PLoS One 2014; 9: e100337.
Acknowledgements
LI, MD and CG-B are investigators of CIBERDEM (www.ciberdem.org). AL-B is an investigator of the I3 Fund for Scientific research (Ministry of Education and Science, Spain). LI and AL-B had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on International Journal of Obesity website
Rights and permissions
About this article
Cite this article
Díaz, M., García-Beltran, C., López-Bermejo, A. et al. GLP-1 and IGF-I levels are elevated in late infancy in low birth weight infants, independently of GLP-1 receptor polymorphisms and neonatal nutrition. Int J Obes 42, 915–918 (2018). https://doi.org/10.1038/ijo.2017.271
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ijo.2017.271