Abstract
Nitroglycerine-induced vasodilation (NID) is usually measured as a control test for flow-mediated vasodilation (FMD). However, NID per se is also associated with atherosclerosis. The purpose of this study was to determine the relationships among NID, FMD and blood pressure, and to evaluate the effects of antihypertensive therapy on NID in patients with hypertension. We measured NID and FMD simultaneously in 94 subjects, including 35 normotensive subjects, 26 patients with stage 1 hypertension (⩾140/90 mm Hg) and 33 patients with stage 2 hypertension (⩾160/100 mm Hg), and we evaluated the effect of antihypertensive therapy for 4 weeks on vascular function in 14 patients with hypertension. NID was smaller in patients with stage 2 hypertension than in patients with stage 1 hypertension and normotensive subjects (10.5±3.9% vs. 13.8±5.0% and 16.2±5.7%; P<0.05, respectively), whereas there was no significant difference in NID between normotensive subjects and patients with stage 1 hypertension. FMD was smaller in patients with stage 2 and stage 1 hypertension than in normotensive subjects (3.1±2.7% and 4.1±1.5% vs. 6.4±2.7%; P<0.05, respectively), whereas there was no significant difference in FMD between patients with stage 1 hypertension and those with stage 2 hypertension. After 4 weeks of antihypertensive therapy, NID was enhanced from 11.9±3.4% to 14.0±3.7% (P=0.03) in patients with hypertension. There was a significant relationship between the decrease in diastolic blood pressure and the increase in NID (r=−0.35, P=0.04). Both NID and FMD were impaired in patients with stage 2 hypertension. Four-week antihypertensive therapy improved NID in patients with hypertension.
Similar content being viewed by others
Introduction
Endothelial function is established in the initial step in the pathogenesis of atherosclerosis and has an important role in the development of this condition.1, 2 Recently, measurement of flow-mediated vasodilation (FMD) in the brachial artery has been widely used as a method for assessing endothelial function in humans.3, 4, 5, 6 As a control test for FMD, measurement of nitroglycerine-induced vasodilation (NID) assessed by sublingually administered nitroglycerine is simultaneously performed to differentiate endothelium-dependent vasodilation from endothelium-independent vasodilation for ascertainment that vascular response to hyperemia is not affected by underlying vascular smooth muscle dysfunction or vascular structural alterations but is truly a consequence of endothelial function.7, 8 However, results of recent studies have demonstrated that NID per se is impaired in patients with multiple cardiovascular risk factors, coronary artery disease or peripheral artery disease and have raised the possibility that NID may be used as a marker of atherosclerosis.9, 10, 11, 12
Hypertension is associated with endothelial dysfunction.13, 14, 15 We and several investigators have reported that treatment with antihypertensive agents and lifestyle modifications improve endothelial function in patients with hypertension.14, 16, 17, 18 These findings suggest that endothelial dysfunction is reversible and can be restored through an appropriate intervention. As for the relationship between hypertension and NID, response to nitric oxide (NO) donors in resistance arteries of patients with hypertension has been shown to be impaired.19, 20 In addition, it has been reported that NID in the conduit brachial artery is impaired in patients with hypertension.21, 22 However, there is little information on the difference between NID and FMD in association with blood pressure level. In addition, it remains unclear whether NID is reversible and can be restored by antihypertensive therapy. We therefore measured NID and FMD in naive patients with essential hypertension and normotensive subjects, and we evaluated the effect of antihypertensive therapy for 4 weeks on NID.
Methods
Subjects
A total of 94 subjects who were never treated with antihypertensive agents (mean age, 53.0±13.9 years; age range, 20–79 years) were recruited from subjects who underwent health-screening examinations at the Hiroshima University Hospital. All employees have an obligation to undergo health screening every year under regulation of the society-managed health insurance union in Japan. In accordance with its regulation, we performed health-screening examinations at our institute. Hypertension was defined as a systolic blood pressure ⩾140 mm Hg and/or a diastolic blood pressure ⩾90 mm Hg. Blood pressure was measured in a sitting position and the average of three measurements was considered for the analysis. Patients with hypertension (n=59) were classified into two groups according to blood pressure level on the basis of the criteria of Joint National Committee VII:23 stage 1 hypertension (n=26) and stage 2 hypertension (n=33). Patients with secondary forms of hypertension were excluded on the basis of complete history; physical examination; radiological and ultrasound examinations; urinalysis; plasma rennin activity; plasma aldosterone and norepinephrine concentrations; serum creatinine, potassium, calcium and free thyroxine concentrations and 24-h urinary excretion of 17-hydroxycorticosteroids, 17-ketogenic steroids and vanillymandelic acid. Patients with a history of diabetes mellitus, coronary heart disease, cerebrovascular disease or peripheral artery disease were also excluded. Dyslipidemia was defined according to the third report of the National Cholesterol Education Program.24 One pack-year was equivalent to 20 cigarettes per day for 1 year. The ethical committees of our institutions approved the study protocol. Written informed consent for participation in the study was obtained from all subjects.
Study protocol 1: relationships between blood pressure level and vascular function
We measured vascular responses to reactive hyperemia and sublingually administered nitroglycerine in the brachial artery in all of the subjects. The subjects fasted the previous night for at least 12 h. The study began at 0830 hours. The subjects were kept in the supine position in a quiet, dark, air-conditioned room (constant temperature of 22–25 °C) throughout the study. A 23-G polyethylene catheter was inserted into the left deep antecubital vein to obtain blood samples. Thirty minutes after maintaining the supine position, basal brachial artery diameter was measured. Then FMD was measured. After completion, we next measured NID with confirmation that the brachial artery diameter had recovered to the baseline value. The observers were blind to the form of examination.
Study protocol 2: effect of antihypertensive therapy on vascular function in patients with hypertension
Vascular function, including FMD and NID, was measured in a manner identical to that of the Study protocol 1 before and after 4 weeks of the treatment in 8 patients with stage 1 hypertension and 12 patients with stage 2 hypertension.
Measurement of FMD and NID
Vascular response to reactive hyperemia in the brachial artery was used for the assessment of endothelium-dependent FMD. A high-resolution linear artery transducer was coupled to computer-assisted analysis software (UNEXEF18G, UNEX, Nagoya, Japan) that used an automated edge detection system for measurement of brachial artery diameter. A blood pressure cuff was placed around the forearm. The brachial artery was scanned longitudinally 5–10 cm above the elbow. When the clearest B-mode image of the anterior and posterior intimal interfaces between the lumen and vessel wall was obtained, the transducer was held at the same point throughout the scan by a special probe holder (UNEX) to ensure consistency of the image. Depth and gain setting were set to optimize the images of the arterial lumen wall interface. When the tracking gate was placed on the intima, the artery diameter was automatically tracked, and the waveform of diameter changes over the cardiac cycle was displayed in real time using the FMD mode of the tracking system. This allowed the ultrasound images to be optimized at the start of the scan and the transducer position to be adjusted immediately for optimal tracking performance throughout the scan. Pulsed Doppler flow was assessed at baseline and during peak hyperemic flow, which was confirmed to occur within 15 s after cuff deflation. Blood flow velocity was calculated from the color Doppler data and was displayed as a waveform in real time. The baseline longitudinal image of the artery was acquired for 30 s, and then the blood pressure cuff was inflated to 50 mm Hg above systolic pressure for 5 min. The longitudinal image of the artery was recorded continuously until 5 min after cuff deflation. Pulsed Doppler velocity signals were obtained for 20 s at baseline and for 10 s immediately after cuff deflation. Changes in brachial artery diameter were immediately expressed as percentage change relative to the vessel diameter before cuff inflation. FMD was automatically calculated as the percentage change in peak vessel diameter from the baseline value. Percentage of FMD [(Peak diameter-Baseline diameter)/Baseline diameter] was used for analysis. Blood flow volume was calculated by multiplying the Doppler flow velocity (corrected for the angle) by heart rate and vessel cross-sectional area (−r2). Reactive hyperemia was calculated as the maximum percentage increase in flow after cuff deflation compared with baseline flow.
The response to nitroglycerine was used for assessment of endothelium-independent vasodilation. NID was measured as described previously.11 Briefly, after acquiring baseline rest images for 30 s, a sublingual tablet (75 μg nitroglycerine) was given, and images of the artery were recorded continuously until the dilation reached a plateau after administration of nitroglycerine. Subjects in whom the sublingually administered nitroglycerine tablet was not dissolved during the measurement were excluded from this study. NID was automatically calculated as a percent change in peak vessel diameter from the baseline value. Percentage of NID [(Peak diameter − Baseline diameter)/Baseline diameter] was used for analysis. Inter- and intra-coefficients of variation for the brachial artery diameter were 1.6% and 1.4%, respectively, in our laboratory.
Measurement of brachial intima-media thickness (IMT)
IMT of the brachial artery was measured as described previously.25 Briefly, before FMD measurement, baseline longitudinal ultrasonographic images of the brachial artery, obtained at the end of diastole (defined as the R wave of an electrocardiogram) from each of 10 cardiac cycles, were automatically stored on a hard disk for off-line assessment of IMT with a linear, phased-array high-frequency (10 MHz) transducer using an UNEXEF18G ultrasound unit (UNEX). Measurement of IMT was automatically performed on A-mode images of the far wall of the brachial artery. The analysis system automatically chose the measurement point where an image of the posterior intimal interface was clearly obtained. If the measurement point was inappropriate, another clear image site could be manually selected for measurement. A total of 21 points over a 3-mm length of IMT in the 10-mm longitudinal image depicted in the analysis display were measured and the mean value per image was automatically calculated. IMT was measured at the same point in each image. The average of mean values obtained from 10 cardiac cycles was defined as IMT of the brachial artery.
Statistical analysis
Results are presented as means±s.d. All reported probability values were two-sided, and a probability value of <0.05 was considered statistically significant. Categorical variables were compared by means of the χ2 test. Continuous variables were compared by using analysis of variance with Bonferroni’s test for post-hoc comparisons for multiple groups. Univariate linear regression analyses were performed to assess the relationships among the variables. Multivariate regression analysis was performed to identify independent variables associated with NID and FMD among risk factors and laboratory data. In addition to age and sex, potential confounders (P<0.20) were entered into the analysis. Two-tailed Student’s paired t-test was used to compare the data before and after treatment. The data were processed using the software package Stata version 9 (Stata, College Station, TX, USA).
Results
Study protocol 1: relationships between blood pressure level and vascular function
The baseline clinical characteristics are summarized in Table 1. Of the 94 subjects, 65 (69.1%) were men and 29 (30.9%) were women. Mean systolic blood pressure was 144.9±23.1 mm Hg and mean diastolic blood pressure was 86.7±14.8 mm Hg. The mean value of NID was 13.5±5.4% and that of FMD was 4.6±2.8%. NID correlated significantly with systolic blood pressure (r=−0.42, P<0.001) and diastolic blood pressure (r=−0.40, P<0.001). FMD also correlated significantly with systolic blood pressure (r=−0.51, P<0.001) and diastolic blood pressure (r=−0.50, P<0.001). There was a significant inverse correlation between NID and IMT of the brachial artery (r=−0.31, P=0.004). Multivariate analysis revealed that both systolic blood pressure and diastolic blood pressure were independent variables of NID and FMD (Table 2).
We next divided subjects into three groups according to the blood pressure level. The baseline clinical characteristics of the three groups are summarized in Table 1. Body mass index and heart rate were significantly higher in patients with stage 1 hypertension than in normotensive subjects. IMT of the brachial artery was significantly higher in patients with stage 1 or stage 2 hypertension than in normotensive subjects. The prevalence of hyperlipidemia was significantly higher in patients with stage 2 hypertension than in normotensive subjects. All other variables, including baseline brachial artery diameter, were similar among the three groups.
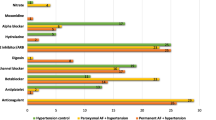
The relationship between NID and blood pressure classification is presented in Figure 1a. NID was significantly smaller in patients with stage 2 hypertension than in normotensive subjects and patients with stage 1 hypertension, whereas there was no significant difference in NID between normotensive subjects and patients with stage 1 hypertension (normotension, 16.2±5.7%; stage 1 hypertension, 13.8±5.0%; stage 2 hypertension, 10.5±3.9%; P=0.17 for normotension vs. stage 1 hypertension; P<0.001 for normotension vs. stage 2 hypertension; P=0.03 for stage 1 hypertension vs. stage 2 hypertension, Figure 1a). Even after multivariate adjustment with a post-hoc test (mean±s.e.m. adjusted for age, sex, heart rate, body mass index, dyslipidemia and smoking pack-year), the relationship between NID and blood pressure classification was unchanged (normotension, 16.0±1.0%; stage 1 hypertension, 14.5±1.0%; stage 2 hypertension, 10.8±1.0%; P=0.95 for normotension vs. stage 1 hypertension; P=0.001 for normotension vs. stage 2 hypertension; P=0.02 for stage 1 hypertension vs. stage 2 hypertension, Supplementary Figure 1A in the online-only Data Supplement). The relationship between FMD and blood pressure classification is presented in Figure 1b. FMD was significantly smaller in patients with stage 1 and stage 2 hypertension than in normotensive subjects, whereas there was no significant difference in FMD between patients with stage 1 hypertension and those with stage 2 hypertension (normotension, 6.4±2.7%; stage 1 hypertension, 4.1±1.5%; stage 2 hypertension, 3.1±2.7%; P=0.001 for normotension vs. stage 1 hypertension; P<0.001 for normotension vs. stage 2 hypertension; P=0.26 for stage 1 hypertension vs. stage 2 hypertension, Figure 1b). Even after multivariate adjustment with a post-hoc test (mean±s.e.m. adjusted for age, sex, heart rate, body mass index, dyslipidemia and smoking pack-year), the relationship between FMD and blood pressure classification was unchanged (normotension, 6.1±0.5%; stage 1 hypertension, 4.2±0.5%; stage 2 hypertension, 3.2±0.4%; P=0.03 for normotension vs. stage 1 hypertension; P<0.001 for normotension vs. stage 2 hypertension; P=0.49 for stage 1 hypertension vs. stage 2 hypertension, Supplementary Figure 1B in the online-only Data Supplement).
Study protocol 2: effect of antihypertensive therapy on vascular function in patients with hypertension
Four patients with stage 1 hypertension and two patients with stage 2 hypertension did not respond to the treatment and remained in the same categories of blood pressure after 4 weeks of treatment. Therefore, 4 patients with stage 1 hypertension and 10 patients with stage 2 hypertension whose blood pressure was reduced by the treatment and category of blood pressure classification was shifted to one lower stage after 4 weeks of treatment were enrolled in study protocol 2, the aim which was to determine the effect of antihypertensive therapy on vascular function through reduction of blood pressure. In all, 7 of the 14 patients were treated with an angiotensin type I receptor blocker and 7 of the 14 patients were treated with a calcium channel blocker. The clinical characteristics and the effects of antihypertensive therapy on baseline parameters are shown in Table 3. Systolic blood pressure decreased from 162.5±13.4 mm Hg to 136.5±9.1 mm Hg and diastolic blood pressure decreased from 94.5±12.5 mm Hg to 82.4±9.8 mm Hg. Other parameters including heart rate and brachial artery diameter were not altered by the treatment.
NID before and that after 4 weeks of antihypertensive therapy are shown in Figure 2. Treatment for 4 weeks improved NID from 11.9±3.4 to 14.0±3.7% (P=0.03). There was a significant correlation between change in brachial artery diameter and change in NID (r=−0.68, P=0.008). The decrease in diastolic blood pressure correlated significantly with the increase in NID (r=−0.35, P=0.04), but there was no significant correlation between the decrease in systolic blood pressure and increase in NID (r=−0.31, P=0.08). There was no significant difference in FMD before and after 4 weeks of treatment (3.2±2.4% vs. 3.6±2.9%, P=0.72).
Discussion
In the present study, we demonstrated that (1) both NID and FMD correlated significantly with blood pressure, (2) compared with that in normotensive subjects, FMD was impaired in patients with stage 1 and stage 2 hypertension, whereas NID was impaired in patients with stage 2 hypertension but not in those with stage 1 hypertension and (3) antihypertensive therapy for 4 weeks improved NID in patients with hypertension whose blood pressure was reduced after the treatment with a significant correlation between the decrease in diastolic blood pressure and the increase in NID. To our knowledge, this is the first report showing that there was a difference between NID and FMD in association with blood pressure and that NID can be restored by antihypertensive therapy through reduction of blood pressure.
NID in the conduit brachial artery is usually assessed as a control test for FMD to confirm that vascular response to hyperemia is not affected by underlying abnormality of endothelium-independent vasodilation but is truly a consequence of endothelium-dependent vasodilation.7, 8 However, NID per se has been demonstrated to be impaired in patients with cardiovascular risk factors or cardiovascular diseases.9, 10, 11, 12, 26 Gokce et al. demonstrated that NID is lower in hypertensive patients than in normotensive subjects.21 Olsen et al. reported that NID correlates negatively with median 24-h ambulatory systolic blood pressure in hypertensive patients with electrocardiographic left ventricular hypertrophy.22 Consistent with the results of these previous studies, NID correlated significantly with systolic blood pressure and diastolic blood pressure in the present study. In addition, blood pressure was an independent predictor of NID. Iiyama et al. reported that there was no significant association between NID in the brachial artery and blood pressure in 26 Japanese subjects, including 13 patients with hypertension (⩾160/95 mm Hg).27 Although we do not know the reasons for the discrepancy in the results of our study and the results of that previous study, it is possible that the small number of subjects enrolled in the previous study resulted in the insignificant difference in NID between patients with and those without hypertension. Endothelium-independent vasodilation assessed by exogenous NO as well as endothelium-dependent vasodilation were impaired in rats with angiotensin II-induced hypertension.28 It has been reported that attenuation of NID is due, at least in part, to reduced expression of soluble guanylate cyclase (sGC) and to reduced activity of NO-dependent sGC in animal models of hypertension.29, 30, 31 Although the mechanisms by which expression of sGC is reduced in hypertension are not entirely clear, activity of sGC is inhibited by superoxide produced by uncoupled endothelial NO synthase and nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, resulting in suppression of the NO/cGMP intravascular signaling pathway in vascular smooth muscle cells and consequent less response of the vasculature to a vasodilatory stimulus.32 Vascular structural change in intima-media layers induced, in part, by mechanical strain on the arterial wall33 may also be involved in reduced vascular response to nitroglycerine. An increased connective tissue matrix in thickened-intima-media layers may contribute to limitation of relaxation, and proliferation of vascular smooth muscle cells may cause a relative reduction in nitroglycerine-derived NO, leading to impaired vasodilatory response to nitroglycerine. Indeed, in the present study, IMT of the brachial artery significantly correlated with NID, indicating that there is an association between thickened intima-media layers and impaired NID in the brachial artery.
Although Olsen et al. measured NID and FMD simultaneously in hypertensive patients with left ventricular hypertrophy, they did not evaluate the difference between NID and FMD in association with blood pressure level.22 In the present study, FMD was significantly smaller in patients with stage 1 hypertension and those with stage 2 hypertension than in normotensive subjects, whereas NID was significantly smaller in patients with stage 2 hypertension but not in those with stage 1 hypertension. These findings suggest that endothelial dysfunction is an early event that precedes the impairment of endothelium-independent vasodilation. An impairment of endothelium-independent vasodilation may occur at a higher blood pressure level. We should regard patients with stage 2 hypertension as a high-risk atherosclerosis group since both endothelium-independent vasodilation and endothelium-dependent vasodilation are impaired in those patients. An abnormality in endothelium-independent vasodilation as well as impaired endothelium-dependent vasodilation might contribute to the increase in the risk of hypertension-related cardiovascular complications.
We also demonstrated that 4-week antihypertensive therapy improved NID in patients with hypertension whose blood pressure was reduced by the treatment. These findings suggest that endothelium-independent vasodilation is reversible and can be restored by an appropriate intervention in hypertensive patients. Risk of hypertension-related cardiovascular complications may be reduced by improvement in NID with antihypertensive therapy. In previous studies, some investigators have shown that antihypertensive therapy does not improve NID in patients with hypertension.34, 35, 36 Although we do not know the precise reasons for the discrepancy in the results of our study and previous studies, some possibilities are postulated. When evaluating the effect of antihypertensive therapy on NID, previous studies included all patients with hypertension who had reduced blood pressure and were non-responders to antihypertensive therapy. In the present study, we limited the subjects to patients with hypertension whose blood pressure was decreased by antihypertensive drugs. Therefore, the results showing no significant improvement in NID after antihypertensive therapy in previous studies may be, in part, due to the subject selection for analyses. Interestingly, Raitakari et al. demonstrated that a high dose of nitroglycerine elicits maximal artery dilation, whereas a low dose of nitroglycerine induces less artery dilation in patients with coronary artery disease, leading to escaped detection of impaired NID.10 Therefore, the difference in the dose of administered nitroglycerine (25, 300 and 400 μg vs. 75 μg) might lead to the misinterpretation that there was no antihypertensive therapy-induced improvement in NID in patients with hypertension who were successfully treated.
Although the precise mechanism by which antihypertensive therapy improves vasodilatory response to nitroglycerine in the brachial artery is unclear, previous studies using animal models of hypertension demonstrated that reduction of blood pressure per se or treatment with antioxidant agents normalizes or even enhances sGC expression.29, 37 In the present study, the decrease in diastolic blood pressure correlated significantly with the increase in NID without significant changes in any other parameters except blood pressure after 4 weeks of the treatment. Reduction of blood pressure per se may contribute to the enhancement of NID. With regard to the association between NID and vascular structural alterations, it is unlikely that structural change is involved in the improvement in NID since there was no significant difference in IMT of the brachial artery before and after the treatment. Although we observed a significant improvement of NID after successful treatment in patients with hypertension, the sample size of treated patients is relatively small. In addition, we could not draw a definite conclusion whether improvement in NID is related to the class effect of an antihypertensive agent used in antihypertensive therapy because of the design and an inadequate number of patients enrolled. Further studies enrolling a large number of patients are warranted to reinforce the conclusion drawn from this study and to explore the mechanism underlying the improvement in NID by antihypertensive therapy.
FMD should be interpreted as an index of vascular function reflecting both endothelium-dependent and endothelium-independent vasodilation, and it is expected that FMD will also be increased after 4-week antihypertensive therapy if NID, as an index of endothelium-independent vasodilation, increases. However, there was no significant increase in FMD after 4-week antihypertensive therapy in the present study. The 4-week treatment may be too short for improvement in endothelial function per se. In addition, endothelium-dependent vasodilatory stimulus mediated by reactive hyperemia may not be sufficient to reflect the improvement of endothelium-independent vasodilation, resulting in no significant increase in FMD.
In conclusion, both NID and FMD are inversely correlated with blood pressure. FMD was significantly smaller in patients with stage 1 hypertension and those with stage 2 hypertension than in normotensive subjects, whereas NID was significantly smaller in patients with stage 2 hypertension but not in those with stage 1 hypertension. Furthermore, antihypertensive therapy for 4 weeks improved NID in patients with hypertension whose blood pressure was reduced. Impairment of endothelium-independent vasodilation as well as endothelial dysfunction may contribute to the increased risk of cardiovascular events, especially in patients with stage 2 hypertension. Endothelium-independent vasodilation is reversible and can be restored by antihypertensive therapy. Further studies are needed to determine whether improvement in NID reduces future cardiovascular events in patients with hypertension.
References
Ross R . Atherosclerosis—an inflammatory disease. N Engl J Med 1999; 340: 115–126.
Higashi Y, Noma K, Yoshizumi M, Kihara Y . Endothelial function and oxidative stress in cardiovascular diseases. Circ J 2009; 73: 411–418.
Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, Lloyd JK, Deanfield JE . Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992; 340: 1111–1115.
Benjamin EJ, Larson MG, Keyes MJ, Mitchell GF, Vasan RS, Keaney JF Jr., Lehman BT, Fan S, Osypiuk E, Vita JA . Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham Heart Study. Circulation 2004; 109: 613–619.
Yeboah J, Folsom AR, Burke GL, Johnson C, Polak JF, Post W, Lima JA, Crouse JR, Herrington DM . Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation 2009; 120: 502–509.
Soga J, Noma K, Hata T, Hidaka T, Fujii Y, Idei N, Fujimura N, Mikami S, Maruhashi T, Kihara Y, Chayama K, Kato H, Liao JK, Higashi Y,, ROCK Study Group. Rho-associated kinase activity, endothelial function, and cardiovascular risk factors. Arterioscler Thromb Vasc Biol 2011; 31: 2353–2359.
Corretti MC, Anderson TJ, Benjamin EJ, Celermajer D, Charbonneau F, Creager MA, Deanfield J, Drexler H, Gerhard-Herman M, Herrington D, Vallance P, Vita J, Vogel R . Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 2002; 39: 257–265.
Inoue T, Matsuoka H, Higashi Y, Ueda S, Sata M, Shimada KE, Ishibashi Y, Node K . Flow-mediated vasodilation as a diagnostic modality for vascular failure. Hypertens Res 2008; 31: 2105–2113.
Adams MR, Robinson J, McCredie R, Seale JP, Sorensen KE, Deanfield JE, Celermajer DS . Smooth muscle dysfunction occurs independently of impaired endothelium-dependent dilation in adults at risk of atherosclerosis. J Am Coll Cardiol 1998; 32: 123–127.
Raitakari OT, Seale JP, Celermajer DS . Impaired vascular responses to nitroglycerin in subjects with coronary atherosclerosis. Am J Cardiol 2001; 87: 217–219 A218.
Maruhashi T, Soga J, Fujimura N, Idei N, Mikami S, Iwamoto Y, Kajikawa M, Matsumoto T, Hidaka T, Kihara Y, Chayama K, Noma K, Nakashima A, Goto C, Higashi Y . Nitroglycerine-induced vasodilation for assessment of vascular function: a comparison with flow-mediated vasodilation. Arterioscler Thromb Vasc Biol 2013; 33: 1401–1408.
Maruhashi T, Nakashima A, Matsumoto T, Oda N, Iwamoto Y, Iwamoto A, Kajikawa M, Kihara Y, Chayama K, Goto C, Noma K, Higashi Y . Relationship between nitroglycerine-induced vasodilation and clinical severity of peripheral artery disease. Atherosclerosis 2014; 235: 65–70.
Panza JA, Quyyumi AA, Brush JE Jr., Epstein SE . Abnormal endothelium-dependent vascular relaxation in patients with essential hypertension. N Engl J Med 1990; 323: 22–27.
Higashi Y, Sasaki S, Kurisu S, Yoshimizu A, Sasaki N, Matsuura H, Kajiyama G, Oshima T . Regular aerobic exercise augments endothelium-dependent vascular relaxation in normotensive as well as hypertensive subjects: role of endothelium-derived nitric oxide. Circulation 1999; 100: 1194–1202.
Davis PA, Pagnin E, Dal Maso L, Caielli P, Maiolino G, Fusaro M, Paolo Rossi G, Calo LA . SIRT1, heme oxygenase-1 and NO-mediated vasodilation in a human model of endogenous angiotensin II type 1 receptor antagonism: implications for hypertension. Hypertens Res 2013; 36: 873–878.
Schiffrin EL, Deng LY . Comparison of effects of angiotensin I-converting enzyme inhibition and beta-blockade for 2 years on function of small arteries from hypertensive patients. Hypertension 1995; 25: 699–703.
Higashi Y, Sasaki S, Nakagawa K, Ueda T, Yoshimizu A, Kurisu S, Matsuura H, Kajiyama G, Oshima T . A comparison of angiotensin-converting enzyme inhibitors, calcium antagonists, beta-blockers and diuretic agents on reactive hyperemia in patients with essential hypertension: a multicenter study. J Am Coll Cardiol 2000; 35: 284–291.
Takagi H, Umemoto T . A meta-analysis of randomized controlled trials of telmisartan for flow-mediated dilatation. Hypertens Res 2014; 37: 845–851.
Kelm M, Preik M, Hafner DJ, Strauer BE . Evidence for a multifactorial process involved in the impaired flow response to nitric oxide in hypertensive patients with endothelial dysfunction. Hypertension 1996; 27: 346–353.
Preik M, Kelm M, Feelisch M, Strauer BE . Impaired effectiveness of nitric oxide-donors in resistance arteries of patients with arterial hypertension. J Hypertens 1996; 14: 903–908.
Gokce N, Holbrook M, Duffy SJ, Demissie S, Cupples LA, Biegelsen E, Keaney JF Jr., Loscalzo J, Vita JA . Effects of race and hypertension on flow-mediated and nitroglycerin-mediated dilation of the brachial artery. Hypertension 2001; 38: 1349–1354.
Olsen MH, Wachtell K, Aalkjaer C, Dige-Petersen H, Rokkedal J, Ibsen H . Vasodilatory capacity and vascular structure in long-standing hypertension: a LIFE substudy. Losartan Intervention For Endpoint-Reduction in Hypertension. Am J Hypertens 2002; 15: 398–404.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr., Jones DW, Materson BJ, Oparil S, Wright JT Jr., Roccella EJ., National Heart L, Blood Institute Joint National Committee on Prevention DE, Treatment of High Blood P, National High Blood Pressure Education Program Coordinating C. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003; 289: 2560–2572.
Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–2497.
Iwamoto Y, Maruhashi T, Fujii Y, Idei N, Fujimura N, Mikami S, Kajikawa M, Matsumoto T, Kihara Y, Chayama K, Noma K, Nakashima A, Higashi Y . Intima-media thickness of brachial artery, vascular function, and cardiovascular risk factors. Arterioscler Thromb Vasc Biol 2012; 32: 2295–2303.
Hartman ML, Shirihai OS, Holbrook M, Xu G, Kocherla M, Shah A, Fetterman JL, Kluge MA, Frame AA, Hamburg NM, Vita JA . Relation of mitochondrial oxygen consumption in peripheral blood mononuclear cells to vascular function in type 2 diabetes mellitus. Vasc Med 2014; 19: 67–74.
Iiyama K, Nagano M, Yo Y, Nagano N, Kamide K, Higaki J, Mikami H, Ogihara T . Impaired endothelial function with essential hypertension assessed by ultrasonography. Am Heart J 1996; 132: 779–782.
Rajagopalan S, Kurz S, Munzel T, Tarpey M, Freeman BA, Griendling KK, Harrison DG . Angiotensin II-mediated hypertension in the rat increases vascular superoxide production via membrane NADH/NADPH oxidase activation. Contribution to alterations of vasomotor tone. J Clin Invest 1996; 97: 1916–1923.
Bauersachs J, Bouloumie A, Fraccarollo D, Hu K, Busse R, Ertl G . Hydralazine prevents endothelial dysfunction, but not the increase in superoxide production in nitric oxide-deficient hypertension. Eur J Pharmacol 1998; 362: 77–81.
Ruetten H, Zabel U, Linz W, Schmidt HH . Downregulation of soluble guanylyl cyclase in young and aging spontaneously hypertensive rats. Circ Res 1999; 85: 534–541.
Mollnau H, Wendt M, Szocs K, Lassegue B, Schulz E, Oelze M, Li H, Bodenschatz M, August M, Kleschyov AL, Tsilimingas N, Walter U, Forstermann U, Meinertz T, Griendling K, Munzel T . Effects of angiotensin II infusion on the expression and function of NAD(P)H oxidase and components of nitric oxide/cGMP signaling. Circ Res 2002; 90: E58–E65.
Munzel T, Feil R, Mulsch A, Lohmann SM, Hofmann F, Walter U . Physiology and pathophysiology of vascular signaling controlled by guanosine 3',5'-cyclic monophosphate-dependent protein kinase [corrected]. Circulation 2003; 108: 2172–2183.
Williams B . Mechanical influences on vascular smooth muscle cell function. J Hypertens 1998; 16: 1921–1929.
Koh KK, Han SH, Chung WJ, Ahn JY, Jin DK, Kim HS, Park GS, Kang WC, Ahn TH, Shin EK . Comparison of effects of losartan, irbesartan, and candesartan on flow-mediated brachial artery dilation and on inflammatory and thrombolytic markers in patients with systemic hypertension. Am J Cardiol 2004; 93: 1432–1435 A1410.
Morimoto S, Yano Y, Maki K, Sawada K . Renal and vascular protective effects of telmisartan in patients with essential hypertension. Hypertens Res 2006; 29: 567–572.
Ghiadoni L, Magagna A, Versari D, Kardasz I, Huang Y, Taddei S, Salvetti A . Different effect of antihypertensive drugs on conduit artery endothelial function. Hypertension 2003; 41: 1281–1286.
Marques M, Millas I, Jimenez A, Garcia-Colis E, Rodriguez-Feo JA, Velasco S, Barrientos A, Casado S, Lopez-Farre A . Alteration of the soluble guanylate cyclase system in the vascular wall of lead-induced hypertension in rats. J Am Soc Nephrol 2001; 12: 2594–2600.
Acknowledgements
We thank Megumi Wakisaka, Miki Kumiji, Ki-ichiro Kawano and Satoko Michiyama for their excellent secretarial assistance. Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (1859081500 and 21590898 to YH) and a Grant in Aid of Japanese Arteriosclerosis Prevention Fund (to YH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Maruhashi, T., Nakashima, A., Kishimoto, S. et al. Reduction in blood pressure improves impaired nitroglycerine-induced vasodilation in patients with essential hypertension. Hypertens Res 38, 862–868 (2015). https://doi.org/10.1038/hr.2015.93
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.93
Keywords
This article is cited by
-
Isolated diastolic hypertension is not associated with endothelial dysfunction
Hypertension Research (2022)
-
Cardiovascular risk in patients receiving antihypertensive drug treatment from the perspective of endothelial function
Hypertension Research (2022)