Abstract
This literature review was conducted to provide better counsel to pregnant women who erroneously took angiotensin receptor blockers (ARBs) during the second and/or third trimesters regarding infant outcomes. Information was available on 83 fetuses in 34 literature reports, including one that we encountered recently. Fourteen pregnancies were terminated, and six were unknown regarding status of amniotic fluid volume (AFV). Fifty-eight and five fetuses did and did not show oligohydramnios, respectively, after being exposed to ARBs. Of the 58 fetuses that presented with oligohydramnios, 57 were exposed to ARBs at gestational week (GW)⩾20, and 19 exhibited resolution of oligohydramnios 1–6 weeks after cessation of ARBs. The 24 mothers without oligohydramnios at delivery ceased taking ARBs earlier (GW of 26.8±5.1 vs. 31.8±4.0, respectively, P=0.000) and had longer duration of gestation after cessation of ARBs (8.4±5.2 vs. 0.7±2.3 weeks, respectively, P=0.000). The mothers without oligohydramnios also had better outcomes in terms of favorable infant outcomes (63% (15/24) vs. 15% (6/39), respectively, P=0.000) and infant mortality rates (13% (3/24) vs. 56% (22/39), respectively, P=0.001) than the 39 with oligohydramnios. Thus, a favorable outcome may be feasible if the fetuses are not indicated for prompt delivery at presentation and exhibit normal AFV or resolution of oligohydramnios after cessation of ARBs. Although the prevalence rate of oligohydramnios was high in this study, it may have been due to publication bias. A prospective study suggested a lower prevalence rate than that reported in the present study.
Similar content being viewed by others
Introduction
Angiotensin receptor blockers (ARBs) are widely used in patients with hypertension, even in women of reproductive age. However, fetopathy, including oligohydramnios, fetal growth restriction, limb defects, hypocalvaria (reduced ossification in the skull), oligohydramnios-induced somatic deformities and death, can occur following exposure of the fetus to ARBs during the second or third trimester,1, 2 although the teratogenicity of ARBs given during the first trimester is still a matter of discussion.3, 4, 5
Fetopathy is thought to result from inhibition of the renin–angiotensin system in the fetus, which can lead to renal hypoperfusion and ischemia.6 Oligohydramnios and anhydramnios, which can occur in fetuses who have been exposed to ARBs,1 reflect fetal oliguria and anuria. Although deleterious effects of ARBs on fetuses are well known and their use in and after the second trimester is contraindicated, the erroneous use of ARBs by pregnant women continues to occur, and we encountered one such case recently. Therefore, it may be important to counsel pregnant women with erroneous ARB exposure regarding fetal outcome. However, most of the pertinent literature is in the form of single case reports and small case series.7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39 Although a review by Bullo et al.1 in 2012 is available and covers 50 cases that were exposed to ARBs during the second and/or third trimesters, no analyses were performed to determine how often oligohydramnios resolved after the cessation of ARBs, whether the resolution of oligohydramnios was associated with better outcomes, and which infants were likely to have better outcomes. Even in larger case series by Spaggiari et al.35 and Oppermann et al.,40 which were published after the review by Bullo et al.,1 information on the outcomes of pregnancies was available in 12 and 40 cases, respectively: eight women elected to undergo termination of the pregnancy among 20 cases presented in the report by Spaggiari et al.35 and 5 of 45 cases (prospective and retrospective cases were 29 and 16 cases, respectively) presented by Oppermann et al.40 were reported previously.7, 29
To provide better counseling to pregnant women who erroneously took ARBs during the second trimester or later, we performed an extensive literature search focusing on the outcomes of the infants. Here, we report the results of a literature search together with a case report describing a pregnant woman in whom ARBs were not discontinued until gestational week (GW) 24 and anhydramnios resolved after the cessation of ARBs. This presentation was conducted after receiving approval by the patient and the Institutional Review Board of the Ethics Committee of Hokkaido University Hospital.
Methods
Reports in the English, Spanish, French and Germany language literature of fetuses exposed to ARBs on and after GW 13 were identified using PubMed (July 2014). The search terms ‘angiotensin receptor blockers,’ ‘angiotensin receptor antagonist,’ ‘oligohydramnios,’ ‘prenatal exposure’ and ‘fetopathy’ were used. In addition, pertinent literature reports found in the reference lists of the retrieved studies were also searched. Among those literature reports describing the gestational age, substance used, period of medication intake (gestational trimester) and outcome of the single cases, we identified 34 literature reports7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40 describing pregnant women who took ARBs on and after GW 13. Among these 34 literature reports, single cases were described in 24 literatures reports,8, 9, 10, 11, 12, 13, 14, 16, 17, 19, 20, 21, 22, 25, 26, 27, 28, 31, 33, 34, 36, 37, 38, 39 two cases (including one set of twins15) in four reports,15, 18, 24, 32 three cases in one report,23 four cases in one report,30 five cases in one report,29 seven cases in one report,7 20 cases in one report35 and 45 cases in one report.40 Thus, information was obtained from these 34 reports regarding the clinical courses of 116 fetuses whose mothers took ARBs on and after GW 13. However, because 5 of the 45 cases reported by Oppermann et al.40 were reported previously7, 29 and data for 29 cases were prospectively collected, we excluded these 34 cases from the present analysis and will discuss the 29 prospectively observed cases by Oppermann et al.40 later. Thus, retrospective data for 82 fetuses who were exposed to ARBs in utero on and after GW 13 were available from 34 literature reports.
Five literature reports cited in the review by Bullo et al.1 were excluded from the present analysis because only women who took ARBs during the first trimester only were presented in four of the reports,41, 42, 43, 44 and no women with ARBs were presented in one study.45 Of the 34 literature reports analyzed in this study, one literature report published in 200633 was not cited by the review by Bullo et al.,1 and three35, 39, 40 were published after the review by Bullo et al.1
Surviving infants were classified into two groups according to the presence or absence of abnormal development in cognitive and/or motor function, kidney dysfunction and short stature (that is, favorable outcome and unfavorable outcome groups). Infants with unfavorable outcomes were defined as those who had one or more of following: variable degree of renal insufficiency at aged 1 month or older, nephrogenic diabetes insipidus at aged 1 year or older, motor dysfunction such as increased muscle tone with tremor, retardation of linguistic development, mental retardation and short stature of less than the 5th percentile for body height. Infants were judged to have favorable outcomes when no such definite adverse outcomes were described in the case reports.
We analyzed the outcomes of 83 fetuses, including our single case.
Here, we present a brief summary of our case. A 32-year-old nulliparous Japanese woman at GW 24−4/7 was referred to us for anhydramnios that was reconfirmed by ultrasound examination showing the deepest vertical pool of 0.0 cm. Since 27 years of age, her hypertension had been treated with valsartan at 160 mg per day and amlodipine at 20 mg per day until GW 24−1/7, at which time these drugs were replaced with nifedipine at 40 mg per day and carvedilol at 20 mg per day. An increase in amniotic fluid volume (AFV) occurred; deepest vertical pool of 1.7 and 2.7 cm and an amniotic fluid index of 12.8 cm were seen 9 (GW 25−3/7), 10 (GW 25−4/7) and 18 (GW 26−5/7) days, respectively, after cessation of valsartan and amlodipine. Thereafter, her course was unremarkable except for fetal growth restriction, showing amniotic fluid index ranging from 7.0 cm (at GW 36−0/7) to 15.0 cm (at GW 29−2/7). She gave birth to a baby boy by cesarean section, which was performed at GW of 38−0/7 after a positive result on oxytocin-stress test. The baby had Apgar scores of 8 and 9 at 1 and 5 min, respectively, and a weight of 1860 g. The neonate appeared to be normal except for being small for gestational age. Respiration and cranial ossification were normal. Ultrasound study of the kidneys was unremarkable. Urine output was good, and no protein was found in the urine. The serum creatinine levels were 1.0 mg dl−1 and 0.27 mg at 1 and 14 days old, respectively. However, both plasma renin activity and aldosterone concentration were elevated to 13.6 ng ml−1 h−1 and 1080 pg ml−1 at birth and 24.3 ng ml−1 h−1 and 652 pg ml−1 at 14 days old, respectively. Although he exhibited difficulty in the establishment of enteral nutrition, he was discharged from hospital at 14 days of age. The infant showed normal growth at 3 months and is being carefully followed up.
Data are presented as the median (range) or the mean±s.d. Statistical analyses were performed using the JMP10© statistical software package (SAS, Cary, NC, USA). Fisher’s exact probability test was used to compare categorical variables. In all analyses, P<0.05 indicated statistical significance.
Results
Eighty-three infants born to 82 women (one twin pregnancy) were erroneously exposed to various ARBs, including valsartan (n=27), candesartan (n=24), losartan (n=16), olmesartan (n=12), irbesartan (n=2), telmisartan (n=1) and eprosartan (n=1) in utero on and after GW 13. The median GW at cessation of ARBs was 29 and ranged from GW 13 to 42 (Table 1). Birth occurred at a median GW (range) of 33 (17–42), on and after GW33 in 52% (43/83) of infants and within 1 week after cessation of ARBs in 49% (41/83) of infants. Thus, approximately half of the fetuses who were exposed to ARBs were indicated for early delivery at presentation. Oligohydramnios or anhydramnios was noted in 93% (71/76) of cases (there was no description of AFV status in seven cases) (Table 1). Only five women had normal AFV.20, 26, 30, 40 Birth weight was not described in 42 infants,9, 15, 19, 20, 23, 30, 35, 40 including one set of twins.15 The median birth weight (range) was 1980 (860–3240) g in 41 infants with known birth weight.
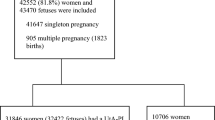
Fourteen mothers23, 30, 32, 35, 40 did not desire a live birth and underwent termination of pregnancy (Table 1, Figure 1). Intrauterine death occurred in six fetuses (7.2%) at GW 23, 30, 31, 32, 33 and 39.12, 28, 35, 40 Twenty-one infants (25%) died after live birth, within 7 days in 18 cases,7, 14, 15, 19, 21, 22, 23, 29, 35, 40 at 45 days old in one case,38 at 3 months old in one case,7 and at 6 months old in one case.40 Finally, 42 infants (51%) survived,7, 8, 9, 10, 11, 13, 16, 17, 18, 20, 24, 25, 26, 27, 29, 30, 31, 32, 33, 34, 35, 36, 37, 39, 40 including our case. Twenty-three of the 42 fetuses who survived had favorable outcomes, including our case,8, 10, 13, 16, 18, 20, 25, 26, 27, 29, 30, 32, 33, 34, 35, 36, 37, 40 and 19 had unfavorable outcomes (Figure 1).7, 9, 11, 17, 18, 24, 29, 31, 35, 38, 40 However, the length of follow-up varied markedly among cases. There were two,8, 36 two29, 31 and two7, 40 fetuses with unknown AFV status in the 23, 19 and 27 cases with favorable outcome, unfavorable outcome and death, respectively. Another case with unknown AFV status was terminated.30
Outcomes of 83 infants who were exposed to angiotensin receptor blockers in utero during the 2nd and/or 3rd trimesters. Among 83 cases (including one set of twins), 14 pregnancies were terminated, 6 fetuses died in utero and 21 neonates (born to 20 mothers) died after live birth. Among 42 survivors, unfavorable outcomes were described in 19 infants, including 13 with varying degrees of renal insufficiency7, 11, 29, 35, 39, 40 (including one with renal transplantation);35 two with mental retardation and diabetes insipidus;24 and one each with increased muscle tone and tremor,18 retarded linguistic development,31 reduced glomerular filtration rate17 and reduced body weight and height less than the 5th percentile.9 No definite adverse outcomes were described in the remaining 23 infants, in whom outcomes were assumed to be favorable.
After excluding 20 pregnancies that were terminated and/or had unknown AFV status, the demographic characteristics were compared among three groups divided by outcome: 21 infants with favorable outcome, 17 infants with unfavorable outcome and 25 infants who died in utero or after live birth (Table 2). When comparing the 21 infants with favorable outcome to the 25 infants who died, ARBs were stopped at a significantly earlier stage of pregnancy, a significantly larger number of cases ceased ARBs at GW ⩽30 (67% vs. 28%, respectively), the time interval after cessation of ARBs until delivery was significantly longer (7.1 ±5.9 vs. 1.2 ±3.1 weeks, respectively), a significantly larger number of cases had a time interval of ⩾3 weeks between the cessation of ARBs and delivery (71% vs. 12%, respectively), and a significantly larger number of fetuses exhibited resolution of oligo-/anhydramnios (67% vs. 8.3%, respectively).
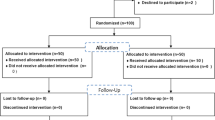
The outcome was analyzed in relation to the status of AFV in the 63 fetuses (Figure 2). Fifty-eight initially had oligo-/anhydramnios, and the remaining five had normal AFV.20, 26, 30, 40 Of the 58 fetuses with documented oligohydramnios, 19 exhibited resolution of oligohydramnios after cessation of ARBs. Finally, oligohydramnios was absent in 24 fetuses, including 5 with no history of oligohydramnios. When comparing these 24 fetuses with no oligohydramnios with those 39 fetuses with persisting oligohydramnios, ARBs were stopped at a significantly earlier GW, the time interval after cessation of ARBs until delivery was significantly longer and outcome was significantly better (see legend for Figure 2). Thus, as expected, a favorable outcome was associated with the early cessation of ARBs, the resolution of oligohydramnios, and a longer duration of gestation after cessation of ARBs.
Relationship between the status of the amniotic fluid volume and outcomes. See legend for Figure 1 for favorable and unfavorable outcomes. The outcomes of 63 fetuses,7, 9, 10, 11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 32, 33, 34, 35, 37, 38, 39, 40 including our case, were analyzed in relation to the status of amniotic fluid volume (AFV) after excluding 20 pregnancies consisting of 1423, 30, 32, 35, 40 terminated pregnancies and six7, 8, 29, 31, 36, 40 pregnancies with unspecified AFV status. Of the 58 fetuses with documented oligohydramnios, 57 were exposed to ARBs at GW ⩾20, and 1910, 11, 12, 13, 18, 23, 25, 29, 33, 35, 37, 39, 40 exhibited resolution of oligohydramnios after cessation of ARBs. The time interval after the cessation of ARBs until confirmed resolution of oligohydramnios ranged from 113 to 6 weeks.11 Fifteen (63%) of the 24 fetuses without oligohydramnios at birth had favorable outcomes, whereas only 6 (15%) of the 39 with persistent oligohydramnios had favorable outcomes (P=0.000). As many as 22 (56%) of the 39 fetuses with oligohydramnios died, whereas three (13%) of the 24 fetuses without oligohydramnios died (P=0.001). When comparing the 24 and 39 fetuses without and with oligohydramnios at birth, respectively, ARBs were withheld at a significantly earlier GW (26.8±5.1 vs. 31.8±4.0, P=0.000), the time interval after cessation of ARBs until delivery was significantly longer (8.4±5.2 vs. 0.7±2.3, P=0.000), and delivery occurred at a significantly advanced GW (35.8±3.6 vs. 32.6±3.4, P=0.001).
Plasma renin and aldosterone concentration
Plasma renin concentration or plasma renin activity and plasma aldosterone concentration were reported in six surviving infants, including our case (Table 3). Both plasma renin concentration/plasma aldosterone concentration and plasma renin concentration appeared to be elevated at birth and gradually decreased thereafter. In two cases reported by Miura et al.,24 both plasma renin activity and plasma aldosterone concentration remained high at the ages of 2 and 6 years. These two cases were affected by salt-losing nephrogenic diabetes insipidus, short stature and mental retardation at that time.24
Discussion
The results of the present study indicated that >90% of fetuses experienced oligohydramnios after exposure to ARBs during and after the second trimester. In addition, this study confirmed that the degrees of injury due to ARBs may depend on the length of exposure. Predictors of favorable outcomes included no indication for prompt delivery when the fetus was identified as having been exposed to ARBs, no oligohydramnios or resolution of oligohydramnios after the cessation of ARBs, and a longer duration of gestation after cessation of ARBs.
Among 76 cases for whom their AFV status was described, as many as 93% of fetuses who exhibited oligohydramnios had been exposed to ARBs in this study. This figure of 93% was higher than that of 63% in the review by Bullo et al.1 and those of 17% (5/29) and 31% (5/16) of 29 women and 16 women, respectively, who ceased using ARBs at GW⩾20 (n=16) in a prospective study by Oppermann et al.40 Eighteen of 68 cases reviewed by Bullo et al.1 were only exposed to ARBs during the first trimester. Because the use of ARBs during only the first trimester may not adversely affect the fetus,3, 4, 5 the inclusion of these 18 cases diluted the effect of ARBs on AFV in their review. The prospective cohort by Oppermann et al.40 included pregnant women who asked about a drug of choice while taking ARBs, but information on outcomes, including prenatal diagnostics at the first contact, is unknown. Because prospective cohorts that are not selected by outcome allow an accurate estimation of the risk of oligohydramnios, the difference in the proportion of cases with oligohydramnios may have been attributable to this difference in the study methods: such cases with oligohydramnios were selectively reported after the detection of an oligohydramnios in many case reports examined in this study. However, both prospective and retrospective cases allow the sensitive period to be specified. In our retrospective cohort of 58 women who continued pregnancy with oligohydramnios, 57 (98%) woman ceased taking ARB at GW⩾20, whereas all five women with oligohydramnios exclusively did in the prospective cohort by Oppermann et al.40 in which none of the 13 women with cessation of ARB at GW<20 developed oligohydramnios. Thus, women with cessation of ARBs at GW<20 were less likely to develop oligohydramnios compared women with cessation of ARBs at GW⩾20.
The resolution of oligohydramnios after the cessation of ARBs is a predictor of favorable outcomes and suggests that the renal damage from ARBs was relatively mild in these patients. It took from 1 to 6 weeks to confirm that the oligohydramnios resolved after cessation of ARBs. This finding suggests that prompt medical intervention with early delivery is not indicated for these patients because of the absence of non-reassuring fetal status. Indeed, the time interval after cessation of ARBs until delivery was 8.4±5.2 weeks with GW of 35.8±3.6 at delivery for 24 cases with normal AFV or resolution of oligohydramnios, whereas these intervals were 0.7±2.3 weeks with a GW of 32.6±3.4 at delivery for 39 cases with oligohydramnios. Thus, most fetuses with oligohydramnios necessitated prompt delivery when exposure to ARBs was found. The majority of those fetuses with oligohydramnios had perhaps already been damaged enough to require ex utero treatment and should not remain in utero for maturation. Therefore, they were likely to have adverse outcomes due to ARB-induced damage and immaturity related to preterm birth. That is, a favorable outcome may be expected in infants who do not exhibit non-reassuring fetal status at presentation on ARBs and exhibit normal AFV or the resolution of oligohydramnios.
Twenty-four fetuses without oligohydramnios had significantly better outcomes than 39 with persisting oligohydramnios (Figure 2). In addition, as expected, ARBs were stopped at a significantly earlier GW in the former 24 fetuses than in the latter 39 fetuses with persisting oligohydramnios. This finding suggests that the rate of fetal survival with a favorable outcome is higher in pregnancies that were exposed to ARBs early during gestation. Indeed, none of the 13 infants whose mothers ceased taking ARBs at GW<20 did not exhibit fetopathy according to Oppermann et al.40 ARBs administered during the first trimester may not be teratogenic3, 4, 5 but should be substituted for other safe antihypertensive agents as soon as possible to minimize the adverse effects on the fetus.
Angiotensin II type 1 receptor autoantibodies are detected in the cord blood of neonates born to women with preeclampsia,46 in whom fetal growth restriction is frequent. The fetal growth restriction was also observed frequently in women with ARBs in this study. ARBs antagonize type 1 receptors (AT1 receptors) of angiotensin II, which is the main effector of the renin–angiotensin system.47 The expression of AT1 receptors is low during the early stage of renal development and increases later in pregnancy.48 Fetal abnormalities associated with the use of ARBs during the second and third trimesters of pregnancy are strikingly similar to those produced by maternal treatment with angiotensin-converting enzyme inhibitors during the second and third trimesters of pregnancy.47 Strong renin expression in the juxtaglomerular apparatus, arteriolar smooth muscle cells and glomerular mesangial cells was observed in a fetus who was exposed to valsartan.23 Serum renin and aldosterone levels appeared to be exclusively elevated in neonates who were exposed to ARBs in utero in this study (Table 3). Fetal oliguria leading to oligohydramnios was an initial and prevalent sign suggestive of fetopathy associated with ARBs in this study. All of these findings are consistent with the term ‘fetal renin–angiotensin system blockade syndrome’ proposed by Bullo et al. for fetopathy caused by both ARBs and angiotensin-converting enzyme inhibitors.1 Although gradual decreases in the renin and aldosterone levels were observed, some infants24 exhibited sustained high levels of these variables (Table 3), suggesting that the effects of in utero exposure to ARBs last a long time in later life.
Limitations of this study
First, the data analyzed in this study were based on single case reports and small case series in the literature, so publication bias is unavoidable as previously mentioned. This bias may have led to the accumulation of eventful pregnancies after exposure to ARBs. Although 93% (71/76) of fetuses with known AFV status exhibited oligohydramnios and 39% (27/69) of infants, after excluding 14 terminated pregnancies, died in this study, there may have been unreported and uneventful pregnancies after exposure to ARBs. Therefore, this study may have overestimated the risk of ARBs in pregnancy. This finding was confirmed by the prospective study by Oppermann et al.40 Second, uniform criteria were not applied to each case from among the 34 reports in determining the outcome, mainly because the length of the follow-up period varied markedly among cases. The follow-up period was <1 year in most cases, and the determination of impairment in motor and cognitive functions is generally difficult for children aged <1 year. Although one-third (23/69) of infants were judged to have a favorable outcome in this study, this finding does not imply that one-third of infants with exposure to ARBS in utero develop normally.
ARBs are contraindicated during pregnancy. Upon the commencement of ARBs, women should be advised not to continue taking ARBs after a pregnancy is established. However, because some pregnant women may continue to take ARBs, it is important to provide appropriate counseling to such women regarding the outcome of their infants. The results of this study may be helpful in such situations. Relatively favorable outcome of infants may be expected if the fetuses are not indicated for prompt delivery at presentation and exhibit normal AFV or spontaneous resolution of oligohydramnios after cessation of ARBs. However, long-term follow-up is needed to determine how the ARBs affect mental and physical development in those fetuses exposed to ARBs in utero.
References
Bullo M, Tschumi S, Bucher BS, Bianchetti MG, Simonetti GD . Pregnancy outcome following exposure to angiotensin-converting enzyme inhibitors or angiotensin receptor antagonists: a systematic review. Hypertension 2012; 60: 444–450.
Quan A . Fetopathy associated with exposure to angiotensin converting enzyme inhibitors and angiotensin receptor antagonists. Early Hum Dev 2006; 82: 23–28.
Porta M, Hainer JW, Jansson SO, Malm A, Bilous R, Chaturvedi N, Fuller JH, Klein R, Orchard T, Parving HH, Sjølie AK, DIRECT Study Group. Exposure to candesartan during the first trimester of pregnancy in type 1 diabetes: experience from the placebo-controlled DIabetic REtinopathy Candesartan Trials. Diabetologia 2011; 54: 1298–1303.
Diav-Citrin O, Shechtman S, Halberstadt Y, Finkel-Pekarsky V, Wajnberg R, Arnon J, Di Gianantonio E, Clementi M, Ornoy A . Pregnancy outcome after in utero exposure to angiotensin converting enzyme inhibitors or angiotensin receptor blockers. Reprod Toxicol 2011; 31: 540–545.
Karthikeyan VJ, Ferner RE, Baghdadi S, Lane DA, Lip GY, Beevers DG . Are angiotensin-converting enzyme inhibitors and angiotensin receptor blockers safe in pregnancy: a report of ninety-one pregnancies. J Hypertens 2011; 29: 396–399.
Forhead AJ, Whybrew K, Hughes P, Broughton Pipkin F, Sutherland M, Fowden AL . Comparison of angiotensin II type 1 receptor blockade and angiotensin-converting enzyme inhibition in pregnant sheep during late gestation. Br J Pharmacol 1996; 119: 393–401.
Hünseler C, Paneitz A, Friedrich D, Lindner U, Oberthuer A, Körber F, Schmitt K, Welzing L, Müller A, Herkenrath P, Hoppe B, Gortner L, Roth B, Kattner E, Schaible T . Angiotensin II receptor blocker induced fetopathy: 7 cases. Klin Padiatr 2011; 223: 10–14.
Bald M, Holder M, Zieger M, Vochem M, Leichter HE . Increased renal echogenicity in a preterm neonate: question and answer. Pediatr Nephrol 2005; 20: 1664–1668.
Bass JK, Faix RG . Gestational therapy with an angiotensin II receptor antagonist and transient renal failure in a premature infant. Am J Pathol 2006; 23: 313–317.
Berkane N, Carlier P, Verstraete L, Mathieu E, Heim N, Uzan S . Fetal toxicity of valsartan and possible reversible adverse side effects. Birth Defects Res A Clin Mol Teratol 2004; 70: 547–549.
Bos-Thompson M-A, Hillaire-Buys D, Muller F, Dechaud H, Mazurier E, Boulot P, Morin D . Fetal toxic effects of angiotensin II receptor antagonists: Case report and follow-up after birth. Ann Pharmacother 2005; 39: 157–161.
Briggs GG, Nageotte MP . Fatal fetal outcome with the combined use of valsartan and atenolol. Ann Pharmacother 2001; 35: 859–861.
Celentano C, Prefumo F, di Vera E, Iannicco A, Gallo DP, Liberati M . Reversible acute fetal renal failure due to maternal exposure to angiotensin receptor blocker. Pediatr Nephrol 2008; 23: 333–334.
Cox RM, Anderson JM, Cox P . Defective embryogenesis with angiotensin II receptor antagonists in pregnancy. BJOG 2003; 110: 1038–1040.
Daïkha-Dahmane F, Levy-Beff E, Jugie M, Lenclen R . Foetal kidney maldevelopment in maternal use of angiotensin II type I receptor antagonists. Pediatr Nephrol 2006; 21: 729–732.
Esposito F, Galfetti M, Lava SA, Balestra B, Bianchetti MG . Fetopathy probably associated to self-medication with a blocker of the renin-angiotensin system. Arch Gynecol Obstet 2011; 284: 1321.
Georgaki-Angelaki E, Stergiou N, Naoum E, Papassotiriou I, Anagnostakou M . Olmesartan medoxomil-induced acute renal failure in a premature newborn following maternal exposure during pregnancy: a case report and review of the literature. Nephrol Dial Transplant Plus 2009; 2: 295–297.
Gersak K, Cvijic M, Cerar LK . Angiotensin II receptor blockers in pregnancy: a report of five cases. Reprod Toxicol 2009; 28: 109–112.
Haaland K . Angiotensin II receptor antagonists against migraine in pregnancy: fatal outcome. J Headache Pain 2010; 11: 167–169.
Hinsberger A, Wingen A-M, Hoyer PF . Angiotensin-II-receptor inhibitors in pregnancy. Lancet 2001; 357: 1620.
Kato K, Okuda M, Ishikawa H, Takahashi T, Hirahara F . Oligohydramnios and pulmonary hypoplasia: a case in which involvement of an angiotensin II receptor antagonist was suspected. J Obstet Gynaecol Res 2008; 34: 242–246.
Lambot M-A, Vermeylen D, Noël J-C . Angiotensin-II-receptor inhibitors in pregnancy. Lancet 2001; 357: 1619–1620.
Martinovic J, Benachi A, Laurent N, Daikha-Dahmane F, Gubler MC . Fetal toxic effects and angiotensin-II-receptor antagonists. Lancet 2001; 358: 241–242.
Miura K, Sekine T, Iida A, Takahashi K, Igarashi T . Salt-losing nephrogenic diabetes insipidus caused by fetal exposure to angiotensin receptor blocker. Pediatr Nephrol 2009; 24: 1235–1238.
Munk PS, vonBrandis P, Larsen A . Reversible fetal renal failure after maternal treatment with Candesartan: a case report. Reprod Toxicol 2010; 29: 381–382.
Nayar B, Singhal A, Aggarwal R, Malhotra N . Losartan induced fetal toxicity. Ind J Pediatr 2003; 70: 923–924.
Pietrement C, Malot L, Santerne B, Roussel B, Motte J, Morville P . Neonatal acute renal failure secondary to maternal exposure to telmisartan, angiotensin II receptor antagonist. J Perinatol 2003; 23: 254–255.
Saji H, Yamanaka M, Hagiwara A, Ijiri R . Losartan and fetal toxic effects. Lancet 2001; 357: 363.
Schaefer C . Angiotensin II-receptor-antagonists: further evidence of fetotoxicity but not teratogenicity. Birth Defects Res A Clin Mol Teratol 2003; 67: 591–594.
Serreau R, Luton D, Macher M-A, Delezoide AL, Garel C, Jacqz-Aigrain E . Developmental toxicity of the angiotensin II type 1 receptor antagonists during human pregnancy: a report of 10 cases. BJOG 2005; 112: 710–712.
Simonetti GD, Baumann T, Pachlopnik JM, von Vigier RO, Bianchetti MG . Non-lethal fetal toxicity of the angiotensin receptor blocker candesartan. Pediatr Nephrol 2006; 21: 1329–1330.
Vendemmia M, Garcia-Meric P, Rizzottia A, Boubred F, Lacroze V, Liprandi A, Simeoni U . Fetal and neonatal consequences of antenatal exposure to type 1 angiotensin II receptor-antagonists. J Mater-Fetal Neonat Med 2005; 18: 137–140.
Bakkum JN, Brost BC, Johansen KL, Johnston BW, Watson WJ . In utero losartan withdrawal and subsequent development of fetal inferior vena cava thrombosis. Obstet Gynecol 2006; 108: 739–740.
Hasbún HJ, Valdés RE, San Martín OA, Catalán MJ, Salinas QS, Parra CM . Transient renal failure in a newborn due angiotensin receptor II antagonist use during pregnancy. Report of one case. Rev Méd Chile 2008; 136: 624–630 (in Spanish).
Spaggiari E, Heidet L, Grange G, Guimiot F, Dreux S, Delezoide A-L, Muller F . Prognosis and outcome of pregnancies exposed to renin–angiotensin system blockers. Prenat Diagn 2012; 32: 1071–1076.
Chung NA, Lip GY, Beevers M, Beevers DG . Angiotensin-II-receptor inhibitors in pregnancy. Lancet 2001; 357: 1620–1621.
Roger N, Popovic I, Madelenat P, Mahieu-Caputo D . Fetal toxicity of angiotensin-II-receptor inhibitors. Case report. Gynecol Obstet Fertil 2007; 35: 556–560 (in French).
Sinelli MT, Cattarelli D, Cortinovis S, Maroccolo D, Chirico G . Severe neonatal renal failure after maternal use of angiotensin II type I receptor antagonists. Pediatr Med Chir 2008; 30: 306–308.
Markfeld-Erol F, Farthmann J, Prömpeler H, Kunze M . Fetal renal failure after intrauterine exposure to inhibitors of the renin-angiotensin system. Dtsch Med Wochenschr 2012; 137: 1297–1300 (in German).
Oppermann M, Padberg S, Kayser A, Weber-Schoendorfer C, Schaefer C . Angiotensin-II receptor 1 antagonist fetopathy—risk assessment, critical time period and vena cava thrombosis as a possible new feature. Br J Clin Pharmacol 2013; 75: 822–830.
Boix E, Zapater P, Pico A, Moreno O . Teratogenicity with angiotensin II receptor antagonists in pregnancy. J Endocrinol Invest 2005; 28: 1029–1031.
Mann R, Mackay F, Pearce G, Freemantle S, Wilton L . Losartan: a study of pharmacovigilance data on 14 522 patients. J Hum Hypertens 1999; 13: 551–557.
Velazquez-Armenta EY, Han JY, Choi JS, Yang KM, Nava-Ocampo AA . Angiotensin II receptor blockers in pregnancy: a case report and systematic review of the literature. Hypertens Pregnancy 2007; 26: 51–66.
Biswas PN, Wilton LV, Shakir SW . The safety of valsartan: results of a postmarketing surveillance study on 12 881 patients in England. J Hum Hypertens 2002; 16: 795–803.
Morgan M, De Jong-van den Berg LT, Jordan S . Drug safety in pregnancy monitoring congenital anomalies. J Nurs Manag 2011; 19: 305–310.
Sahay AS, Patil VV, Sundrani DP, Joshi AA, Wagh GN, Gupte SA, Joshi SR . A longitudinal study of circulating angiogenic and antiangiogenic factors and AT1-AA levels in preelcampsia. Hypertens Res 2014; 37: 753–758.
Alwan S, Polifka JE, Friedman JM . Angiotensin II receptor antagonist treatment during pregnancy. Birth Defects Res Part A 2005; 73: 123–130.
Grone HJ, Simon M, Fuchs E . Autoradiographic characterization of angiotensin receptor subtypes in fetal and adult human kidney. Am J Physiol 1992; 262 (Pt 2): F326–F331.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Shimada, C., Akaishi, R., Cho, K. et al. Outcomes of 83 fetuses exposed to angiotensin receptor blockers during the second or third trimesters: a literature review. Hypertens Res 38, 308–313 (2015). https://doi.org/10.1038/hr.2015.12
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.12
Keywords
This article is cited by
-
Roles of angiotensin II type 2 receptor in mice with fetal growth restriction
Hypertension Research (2018)