Abstract
Purpose:
Monoallelic germ-line deleterious mutations of PALB2 (partner and localizer of BRCA2) are associated with breast cancer risk and have been found in several populations, with carrier frequencies of ~1−2%. Initially, these mutations were considered to have moderate penetrance, but accumulating evidence now indicates that they are associated with much higher risk.
Methods:
In this study, we sequenced the PALB2 coding regions unlinked to BRCA (breast cancer) genes in 575 probands from Italian breast cancer families recruited in Milan.
Results:
We found 12 carriers (2.1%) of deleterious mutations, and none of the mutations was found in 784 controls collected in Milan. One of these mutations, the c.1027C>T (p.Gln343X), was found to be recurrent in the province of Bergamo in northern Italy, being detected in 6/113 (5.3%) familial breast cancer cases and 2/477 (0.4%) controls recruited in this area (Fisher’s exact test: P < 0.01).
Conclusions:
Our data provide confirmatory findings that, in the Italian population also, deleterious mutations of PALB2 are relatively frequent predisposing factors for breast cancer and may be associated with high risk of the disease.
Genet Med 16 9, 688–694.
Similar content being viewed by others
Main
Breast cancer is a fairly common and heterogeneous disease, and both environmental and genetic factors are involved in its etiology. In recent years, genetic factors have been discovered at an increasing rate. Several genome-wide association studies described a few dozen single-nucleotide polymorphisms associated with low risk for breast cancer. A particularly extensive recent genome-wide association study identified numerous additional loci and suggested that these markers are promising for the identification of at-risk individuals in the general population.1
In terms of risk prediction in mutation carriers and their families, germ-line mutations with high penetrance are clinically relevant. These account for a substantial proportion of familial clusters (up to 25%) and occur mainly in the BRCA1 and BRCA2 genes that are routinely tested in clinical practice. Moreover, a small fraction of cases are explained by high-risk mutations in genes associated with syndromic diseases in which breast cancer is one of the clinical features, including TP53 (Li–Fraumeni syndrome), PTEN (Cowden syndrome), and STK11 (Peutz–Jeghers syndrome).2
Mutations with moderate/intermediate penetrance are of increasing importance for the estimate of familial breast cancer risk. These were originally found in genes tested as candidate breast cancer loci because the encoded proteins were involved in BRCA (breast cancer) gene pathways. These genes include CHEK2,3 ATM,4 and some of the genes causing Fanconi anemia (FA) syndrome. In addition to BRCA2, which was found to be the same as the FA gene FANCD1,5 two other FA-associated genes, BRIP1/FANCJ and PALB2/FANCN, have a clear impact on breast cancer risk,6,7 although together they account for a much smaller fraction of cases than those ascribable to BRCA genes.2 Mutations in the RAD51C/FANCO gene were originally found in breast/ovarian cancer families.8 However, subsequent studies indicated that RAD51C mutations may confer a higher risk for ovarian cancer than for breast cancer.9 Sequencing performed in other FA genes, including FANCL, FANCM, FANCI, and SLX4/FANCP, initially suggested that they have no impact on breast cancer risk.10,11,12,13 However, subsequent analyses allowed the identification of (i) three unique SLX4-truncating mutations,14,15,16 indicating these mutations are very rare in familial cases, and (ii) a nonsense mutation in FANCM, whose frequency in cases was, however, not significantly higher than that in controls.17 Finally, deleterious mutations in the FA gene XRCC2 were detected in families with breast cancer ascertained mainly in Australia.18 The extent of the impact of this gene on breast cancer risk was questioned by a subsequent study.19
The PALB2 (partner and localizer of BRCA2) gene, which encodes a direct interactor of BRCA2—namely, RAD51—and other proteins,20 has been actively studied as a breast cancer risk factor, and sequencing of its coding regions revealed that deleterious mutations are present in several populations. The first study that indicated that PALB2 is a breast cancer gene reported germ-line truncating mutations in 10/923 (1.1%) English familial breast cancer cases.7 Additional studies found carriers of truncating mutations with a frequency of ~1−2% in Spanish, Chinese, South African, Russian, German, Italian, African-American, Australasian, and Malaysian familial or early-onset breast cancer cases.10,20,21,22,23,24 A similar frequency was observed in population-based studies of Australians and mixed-ethnicity breast cancer cases.20,25,26 A mutation-carrier frequency of 3.4% was reported in familial cases from the United States. This frequency, apparently higher as compared with that reported in other studies, might be due to the examined sample being enriched in a few founder mutations.27 No mutations were identified in Jewish families of either Ashkenazi or non-Ashkenazi origin.27,28
To date, PALB2 recurrent mutations have been reported in four populations. The Finnish c.1592delT (p.Leu531fs) mutation was investigated in two studies29,30 and identified in 3/113 (2.7%) and 19/947 (2.0%) familial cases and in 6/2,501 (0.2%) and 2/1,079 (0.2%) controls, respectively. The c.2323C>T (p.Gln775X) mutation was detected in 4/564 (0.7%) French–Canadian early-onset cases and in 0/6,443 newborn infant controls.31 The Polish c.509_510delGA (p.Arg170fs) mutation was found in 4/648 (0.6%) familial cases and in 1/1,310 (0.1%) controls.32 Finally, the c.3113G>A (p.Trp1038X) mutation was recurrent in Australians, found in 5/1,403 (0.4%) cases and in 0/764 controls from a population-based study25 and in 8/871 (0.9%) high-risk familial cases.33
PALB2 mutations were found with similar frequencies in all populations tested—the only exception being the Jewish population—and were found to be associated with increased risk of developing breast cancer. Although initially these mutations were referred to as risk factors with moderate penetrance, several studies demonstrated that at least some of these mutations confer a much higher risk.20 In the current study, we aimed to assess the involvement of PALB2 in Italian families with breast cancer by sequencing the entire gene-coding region in a large series of cases. In all, 575 probands were analyzed and 12 carriers of deleterious mutations were detected. One of these mutations was found to be recurrent in families from the province of Bergamo in northern Italy.
Materials and Methods
Study population
The study included individuals with evidence of a genetic predisposition to breast cancer who had been previously selected for mutation testing in BRCA1 and BRCA2—based on the criteria reported in the Supplementary Material online—at the Medical Genetics Unit of the Fondazione IRCCS Istituto Nazionale dei Tumori (INT) and the Division of Cancer Prevention and Genetics of the Istituto Europeo di Oncologia (IEO) in Milan and at the Unit of Medical Oncology of the Azienda Ospedaliera Papa Giovanni XXIII of Bergamo (AO-BG). Only individuals who tested negative for disease-causing mutations in BRCA genes, as described in the Supplementary Material online, and who were affected with breast cancer as the first diagnosed malignancy (BRCAX cases) were considered. Normal controls were consecutive female blood donors recruited by the Unit of Immunohematology and Transfusion Medicine of INT and the Associazione Volontari Italiani Sangue of Milan and of Bergamo. All individuals participating in this study signed an informed consent to the use of their biological samples for research projects aimed at the identification and the study of genetic factors associated with breast cancer risk. The study was approved by the Ethics Committee of the Fondazione IRCCS Istituto Nazionale dei Tumori and the Bioethics Committee of Azienda Ospedaliera Papa Giovanni XXIII of Bergamo.
PALB2 mutation analysis
DNA samples were obtained from peripheral blood, using the Gentra Puregene extraction kit (Qiagen, Hilden, Germany). All 13 PALB2 exons and intron/exon boundaries were amplified by PCR and Sanger sequencing in 575 cases recruited in Milan by using primers reported elsewhere.34 A search for large genomic rearrangements was not performed. PCR fragments that included deleterious mutations identified in cases were also tested by sequencing in 784 controls from Milan. The c.72delG (p.Arg26fs) and the c.1027C>T (p.Gln343X) recurrent mutations were genotyped by Taqman assay in an additional 332 cases from Milan and 113 cases and 477 controls from Bergamo. Probes and experimental conditions are available on request.
In silico analyses
Analyses of candidate splicing aberrations were performed using different computational programs, including Automated Splice Site and Exon Definition Analyses (http://splice.uwo.ca), Splice View (http://zeus2.itb.cnr.it/~webgene/www.spliceview_ex.html), and the five tools integrated in the Alamut application (Interactive Biosoftware, Roven, France; http://www.interactive-biosoftware.com/software/alamut/overview). The predicted effect of missense mutations on protein structure and function was assessed using Polymorphism Phenotyping, version 2 (PolyPhen2; http://genetics.bwh.harvard.edu/pph2/); Sorting Intolerant From Tolerant (SIFT; http://sift.jcvi.org/); Single-Nucleotide Polymorphisms and Gene Ontology (SNPs&GO; http://snps.biofold.org/snps-and-go/snps-and-go.html); alignment Using Grantham Variation and Grantham Deviation (Align-GVGD; http://agvgd.iarc.fr); Protein Variation Effect Analyzer (PROVEAN; http://provean.jcvi.org/index.php); and Mutation Assessor (http://mutationassessor.org) tools.
In vitro analyses of the c.48G>A splicing mutation
Establishment and culture of the lymphoblastoid cell line derived from the mutation carrier, total RNA purification, and cDNA synthesis were performed as described.35 PCR amplification was carried out with a forward primer in PALB2 exon 1 (5′-GCTGCTCTTTTCGTTCTGTC-3′) and a reverse primer in PALB2 exon 3 (5′-GGTGAGAGATCCTGCTGAGAC-3′). An LCL negative for the c.48G>A mutation, three LCLs with mutations in other genes, and seven LCLs from blood donors were used as negative controls. The amplification products were visualized on an agarose gel and characterized by direct sequencing.
Statistical methods
The confidence interval of the proportion of each considered mutation was computed by means of exact methods. We used the Fisher’s exact test to assess possible associations between genotype frequency and disease status (cases and controls). With the purpose of comparing our results with those reported by other authors, we estimated the odds ratios (ORs) and their 95% confidence intervals by resorting to a logistic regression model with age as adjustment covariate. All statistical analyses were performed with the SAS software (version 9.2; SAS Institute, Cary, NC).
Results
The PALB2 coding region was sequenced in 575 BRCAX cases recruited at INT and IEO in Milan, and a total of 34 different variants were detected. Of these, eight were common, previously annotated polymorphisms ( Table 1 ) and 26 were rare or unique variants ( Tables 2 and 3 ). Of these 26 variants, 7 mutations (3 frameshift and 4 nonsense) introduced a premature termination codon and 1, c.3497delG, was a frameshift mutation that changed the last 21 amino acids of the protein’s C terminus, causing the loss of the stop codon and the addition of three new residues ( Table 2 ). This change modifies the conserved WD40 protein domain interacting with BRCA220 and, therefore, is considered to be deleterious. Three of the deleterious mutations were previously described in a subanalysis of the same sample set.36
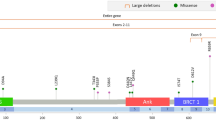
The remaining 18 variants were analyzed in silico using the bioinformatics tools described in the Materials and Methods section to identify potential splicing mutations. The c.48G>A mutation, located at the last base of exon 1, was predicted to affect the canonical mRNA splicing by causing the loss of the natural donor splice site by all five bioinformatics tools that correctly detected the site. To verify this prediction, a RT-PCR analysis was performed. A cDNA fragment spanning the junction of exons 1 and 2 was amplified from an LCL established from the mutation carrier, and an aberrant transcript, which was not present in a mutation-negative cDNA, was observed ( Figure 1a ). In addition, the aberrant transcript was not detected in three LCLs from individuals with mutations in other genes and seven LCLs from blood donors (data not shown), indicating that the observed alternative splicing is caused by the c.48G>A mutation and is not a naturally occurring PALB2 isoform. Sequencing of the amplification products showed that this transcript lacked 17 nucleotides at the 3′ end of exon 1 ( Figure 1b ). These results indicate that the c.48G>A mutation abolishes the canonical donor splice site and activates an alternative site within exon 1, causing the loss of the reading frame and the formation of a premature termination codon at the amino acid residue 36 (p.Cys11fs; Table 2 ). Furthermore, the c.2379C>T (p.Gly793Gly) variant was predicted to create a novel donor site by six of the seven bioinformatics tools considered. No source of RNA from the mutation carrier was available to verify these outputs.
Characterization of the mRNA transcripts produced as a result of the PALB2 c.48G>A mutation. (a) RT–PCR results. M, molecular marker (ΦX-174 HaeIII); lane 1, no template; lane 2, genomic DNA used as negative control of the RT–PCR reaction; lane 3, cDNA (cDNA) from a PALB2 wild-type lymphoblastoid cell line (LCL) used as a normal control for the RT–PCR reaction; lane 4, cDNA from the LCL carrying the heterozygous PALB2 c. 48G>A mutation. The sizes of the full-length (FL) and aberrant (Ex1_17bp del) transcripts are indicated. The additional band due to the improper annealing of the two transcripts is indicated by the asterisk. (b) Sequencing results. The mutated cDNA (upper panel) shows two overlapping sequences, one corresponding to the FL transcript (the unique fragment present in the normal control cDNA, lower panel) and one corresponding to the aberrant transcript due to the skipping of 17 nucleotides (GTGAGGAGAAGGAAAAG) at the 5′ end of exon 1. The sequencing reaction was performed using the reverse primer.
The nine deleterious mutations were tested by sequencing the corresponding fragments in 784 blood donors recruited at INT and Associazione Volontari Italiani Sangue in Milan, and no carriers were identified. Through analysis of these fragments, we genotyped five of the common polymorphisms and nine of the rare variants identified in cases. The frequencies of the five polymorphisms in controls were found by Fisher’s exact test to be not different from those observed in cases, in keeping with the notion that they are probably neutral polymorphisms ( Table 1 ). Five of the nine rare variants were detected in controls ( Table 3 ).
In silico analyses were also performed to investigate all the missense mutations ( Table 3 ). In this analysis, two mutations—the c.2792T>G (p.Leu931Arg) and the c.2816G>T (p.Leu939Trp)—were classified as damaging or possibly damaging by all tools reported in the Materials and Methods section. Of note, both the leucine amino acids at positions 931 and 939 are conserved in all species, from Homo sapiens to Danio rerio, and are located in the WD40-repeat domain responsible for binding to BRCA2 and in a region that mediates the binding with RAD51.20 Of these two mutations, only p.Leu931Arg was not annotated and not found in controls from this study or other previously published studies. Thus, of all PALB2 missense mutations we detected, p.Leu931Arg seems to have the highest probability of being deleterious.
Each of the nine deleterious mutations was found in a single index case, except for the c.72delG and the c.1027C>T mutations, which were detected in two and three cases, respectively. Therefore, in our survey of 575 BRCAX cases, a total of 12 families with PALB2 deleterious mutations were detected, for an overall frequency of 2.1%.
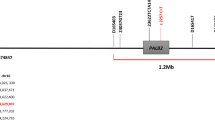
We further genotyped the two c.72delG and the c.1027C>T recurrent mutations in 332 additional BRCAX cases ascertained at INT and IEO, but no other carriers of these mutations were found, for an overall frequency of 0.22% (2/907) and 0.33% (3/907), respectively. However, we noticed that two of the three c.1027C>T mutation carriers self-reported as being originally from the province of Bergamo in northern Italy. To explore the possibility that the c.1027C>T was recurrent in this area, 113 BRCAX cases recruited at AO-BG were genotyped, and 6 carriers were detected (5.3%). The mutation was also tested in 477 female blood donors recruited through Associazione Volontari Italiani Sangue in Bergamo, and 2 carriers (0.4%) were identified.
Hence, a total of 18 probands with deleterious PALB2 mutations were found. The pedigrees are reported in Supplementary Figure S1 online as they were reconstructed at genetic counseling (12 in the Milan group and 6 in the Bergamo group). In five families, relatives of the proband were also available for mutation testing.
Discussion
The sequencing of all coding exons and splice sites of PALB2 in 575 Italian BRCAX cases detected 34 variants. Eight were previously found common polymorphisms, 17 were rare or unique variants of unclear significance, and 9 were deleterious mutations. The last were identified in a total of 12 BRCAX cases (2.1%) and not observed in 784 healthy controls recruited in Milan. Interestingly, one deleterious mutation, c.1027C>T, had a frequency of 5.3% in 113 BRCAX cases recruited at Bergamo city hospital (AO-BG). This was more than 15 fold higher than the frequency of 0.33% observed among 907 BRCAX patients recruited in Milan, (including the 575 cases of the original set and 332 additional cases specifically genotyped for the mutation). The two proportions differ significantly as confirmed by their exact 95% confidence intervals: 1.97−11.20% and 0.07−0.96%, respectively.
Milan is the largest city in northern Italy and one of the urban areas with the greatest immigration from other regions of the country during the past decades. Moreover, both INT and IEO are among the largest and most recognized Italian institutions for cancer treatment and serve patients from all over the country. On the other hand, more than 80% of BRCAX patients recruited in Bergamo, including all carriers of the c.1027C>T mutation, were born in Bergamo or in its province. Hence, the increased frequency of a few specific cancer–predisposing mutations observed in cases from Bergamo, with respect to those from Milan, indicates that this region may be characterized by lower genetic heterogeneity as compared with the rest of the country and may therefore be possibly enriched in individuals from a genetically isolated population. This could be due, among other factors, to the particular conformation of the territory, characterized by secluded deep valleys, which might have straitened genetic admixture. Of note, two other mutations in breast cancer–predisposing genes, the c.190C>T (p.Cys64Arg) in BRCA1 and the c.6132_6135delAGTC (p.Val1969fs) in BRCA2, were found to be recurrent in the Bergamo area (P.R., unpublished data). The preferential geographical distribution of the PALB2 c.1027C>T mutation is further confirmed by the finding that, although absent in blood donors recruited in Milan (n = 784), it occurred in two of the 477 female blood donors recruited in Bergamo, for a frequency of 0.4%.
The overall frequency of deleterious mutations found in Milan cases, 12/575 carriers (2.1%) vs. none in 784 controls, suggested that PALB2-truncating mutations are relevant factors for breast cancer risk. An estimate of the risk conferred by PALB2-truncating variants was derived by comparing the frequencies of c.1027C>T in BRCAX (5.3%) and controls (0.4%) ascertained in Bergamo. These frequencies were found to differ significantly (Fisher’s exact test: P < 0.01). With the purpose of comparing our results with those reported by other authors, we estimated the age-adjusted OR of these frequencies by resorting to a logistic regression model. The OR value of 13.4 (95% confidence interval: 2.7−67.4) that we found was similar to those previously observed for mutations recurrent in other countries. An OR of ~11 was estimated in Finnish familial cases and controls in two separate studies for the c.1592delT mutation.29,30 The French–Canadian c.2323C>T mutation was tested in early-onset cases and controls, yielding an OR of 103. This OR value was most likely overestimated, given that no mutation carriers were found among controls.31 Finally, cumulative risks similar to those observed in BRCA2 mutation carriers (49% to age 50 and 91% to age 70) were estimated for the c.3113G>A truncating mutation based on analysis of the relatives of five carriers identified in a population-based PALB2 screening.25 Together with these previous observations, our data reinforce the growing knowledge that PALB2 is a high-risk factor for breast cancer.
Our survey of a large number of Italian BRCAX cases provides further evidence of the association of PALB2 mutations with breast cancer susceptibility and indicates that the proportion of at-risk families attributable to these mutations in Italy is roughly similar to that ascertained in other populations. In addition, this study, while confirming the high degree of heterogeneity of PALB2 mutations both within the same and among different populations, is the first report describing a PALB2 recurrent mutation in Italian individuals. This mutation, c.1027C>T (p.Gln343X), appears to preferentially occur in families from a restricted geographical area in the north of the country, and comparison of its frequency in cases versus controls indicates that it is associated with high risk for breast cancer. Further analyses are required to verify whether genotyping for this specific mutation can be proposed as a cost-effective strategy for the rapid identification of genetically predisposed subjects in this area.
Disclosure
The authors declare no conflict of interest.
References
Michailidou K, Hall P, Gonzalez-Neira A, et al. Large-scale genotyping identifies 41 new loci associated with breast cancer risk. Nat Genet 2013;45:353–361.
Mavaddat N, Antoniou AC, Easton DF, Garcia-Closas M . Genetic susceptibility to breast cancer. Mol Oncol 2010;4:174–191.
Meijers-Heijboer H, van den Ouweland A, Klijn J, et al.; CHEK2-Breast Cancer Consortium. Low-penetrance susceptibility to breast cancer due to CHEK2(*)1100delC in noncarriers of BRCA1 or BRCA2 mutations. Nat Genet 2002;31:55–59.
Renwick A, Thompson D, Seal S, et al.; Breast Cancer Susceptibility Collaboration (UK). ATM mutations that cause ataxia-telangiectasia are breast cancer susceptibility alleles. Nat Genet 2006;38:873–875.
Howlett NG, Taniguchi T, Olson S, et al. Biallelic inactivation of BRCA2 in Fanconi anemia. Science 2002;297:606–609.
Seal S, Thompson D, Renwick A, et al.; Breast Cancer Susceptibility Collaboration (UK). Truncating mutations in the Fanconi anemia J gene BRIP1 are low-penetrance breast cancer susceptibility alleles. Nat Genet 2006;38:1239–1241.
Rahman N, Seal S, Thompson D, et al.; Breast Cancer Susceptibility Collaboration (UK). PALB2, which encodes a BRCA2-interacting protein, is a breast cancer susceptibility gene. Nat Genet 2007;39:165–167.
Meindl A, Hellebrand H, Wiek C, et al. Germline mutations in breast and ovarian cancer pedigrees establish RAD51C as a human cancer susceptibility gene. Nat Genet 2010;42:410–414.
Loveday C, Turnbull C, Ruark E, et al.; Breast Cancer Susceptibility Collaboration (UK). Germline RAD51C mutations confer susceptibility to ovarian cancer. Nat Genet 2012;44:475–6; author reply 476.
García MJ, Fernández V, Osorio A, et al. Analysis of FANCB and FANCN/PALB2 fanconi anemia genes in BRCA1/2-negative Spanish breast cancer families. Breast Cancer Res Treat 2009;113:545–551.
Landwehr R, Bogdanova NV, Antonenkova N, et al. Mutation analysis of the SLX4/FANCP gene in hereditary breast cancer. Breast Cancer Res Treat 2011;130:1021–1028.
Catucci I, Colombo M, Verderio P, et al. Sequencing analysis of SLX4/FANCP gene in Italian familial breast cancer cases. PLoS ONE 2012;7:e31038.
Fernández-Rodríguez J, Quiles F, Blanco I, et al. Analysis of SLX4/FANCP in non-BRCA1/2-mutated breast cancer families. BMC Cancer 2012;12:84.
Bakker JL, van Mil SE, Crossan G, et al. Analysis of the novel fanconi anemia gene SLX4/FANCP in familial breast cancer cases. Hum Mutat 2013;34:70–73.
Shah S, Kim Y, Ostrovnaya I, et al. Assessment of SLX4 Mutations in Hereditary Breast Cancers. PLoS ONE 2013;8:e66961.
de Garibay GR, Díaz A, Gaviña B, et al. Low prevalence of SLX4 loss-of-function mutations in non-BRCA1/2 breast and/or ovarian cancer families. Eur J Hum Genet 2013;21:883–886.
Gracia-Aznarez FJ, Fernandez V, Pita G, et al. Whole exome sequencing suggests much of non-BRCA1/BRCA2 familial breast cancer is due to moderate and low penetrance susceptibility alleles. PLoS ONE 2013;8:e55681.
Park DJ, Lesueur F, Nguyen-Dumont T, et al.; Breast Cancer Family Registry; Kathleen Cuningham Foundation Consortium for Research into Familial Breast Cancer. Rare mutations in XRCC2 increase the risk of breast cancer. Am J Hum Genet 2012;90:734–739.
Hilbers FS, Wijnen JT, Hoogerbrugge N, et al. Rare variants in XRCC2 as breast cancer susceptibility alleles. J Med Genet 2012;49:618–620.
Southey MC, Teo ZL, Winship I . PALB2 and breast cancer: ready for clinical translation! Appl Clin Genet 2013;6:43–52.
Blanco A, de la Hoya M, Balmaña J, et al. Detection of a large rearrangement in PALB2 in Spanish breast cancer families with male breast cancer. Breast Cancer Res Treat 2012;132:307–315.
Pern F, Bogdanova N, Schürmann P, et al. Mutation analysis of BRCA1, BRCA2, PALB2 and BRD7 in a hospital-based series of German patients with triple-negative breast cancer. PLoS ONE 2012;7:e47993.
Phuah SY, Lee SY, Kang P, et al. Prevalence of PALB2 mutations in breast cancer patients in multi-ethnic Asian population in Malaysia and Singapore. PLoS ONE 2013;8:e73638.
Hellebrand H, Sutter C, Honisch E, et al. Germline mutations in the PALB2 gene are population specific and occur with low frequencies in familial breast cancer. Hum Mutat 2011;32:E2176–E2188.
Southey MC, Teo ZL, Dowty JG, et al.; kConFab for the Beast Cancer Family Registry. A PALB2 mutation associated with high risk of breast cancer. Breast Cancer Res 2010;12:R109.
Tischkowitz M, Capanu M, Sabbaghian N, et al.; WECARE Study Collaborative Group. Rare germline mutations in PALB2 and breast cancer risk: a population-based study. Hum Mutat 2012;33:674–680.
Casadei S, Norquist BM, Walsh T, et al. Contribution of inherited mutations in the BRCA2-interacting protein PALB2 to familial breast cancer. Cancer Res 2011;71:2222–2229.
Catucci I, Milgrom R, Kushnir A, et al. Germline mutations in BRIP1 and PALB2 in Jewish high cancer risk families. Fam Cancer 2012;11:483–491.
Erkko H, Xia B, Nikkilä J, et al. A recurrent mutation in PALB2 in Finnish cancer families. Nature 2007;446:316–319.
Heikkinen T, Kärkkäinen H, Aaltonen K, et al. The breast cancer susceptibility mutation PALB2 1592delT is associated with an aggressive tumor phenotype. Clin Cancer Res 2009;15:3214–3222.
Ghadirian P, Robidoux A, Zhang P, et al. The contribution of founder mutations to early-onset breast cancer in French-Canadian women. Clin Genet 2009;76:421–426.
Dansonka-Mieszkowska A, Kluska A, Moes J, et al. A novel germline PALB2 deletion in Polish breast and ovarian cancer patients. BMC Med Genet 2010;11:20.
Teo ZL, Sawyer SD, James PA, et al. The incidence of PALB2 c.3113G>A in women with a strong family history of breast and ovarian cancer attending familial cancer centres in Australia. Fam Cancer 2013;12:587–595.
Reid S, Schindler D, Hanenberg H, et al. Biallelic mutations in PALB2 cause Fanconi anemia subtype FA-N and predispose to childhood cancer. Nat Genet 2007;39:162–164.
Colombo M, De Vecchi G, Caleca L, et al. Comparative in vitro and in silico analyses of variants in splicing regions of BRCA1 and BRCA2 genes and characterization of novel pathogenic mutations. PLoS ONE 2013;8:e57173.
Peterlongo P, Catucci I, Pasquini G, et al. PALB2 germline mutations in familial breast cancer cases with personal and family history of pancreatic cancer. Breast Cancer Res Treat 2011;126:825–828.
Acknowledgements
We are particularly grateful to all individuals who participated in this study. We also thank Irene Feroce and Alessandra Rossi (Division of Cancer Prevention and Genetics, Istituto Europeo di Oncologia, Milan, Italy) for their collaboration in the study. This work was partially supported by grants from the Associazione Italiana per la Ricerca sul Cancro (AIRC) to P.P. (IG 12821) and A.F. (5 per mille 12,237), funds from Italian citizens who allocated a 5 per mile share of their tax payment in support of the Fondazione IRCCS Istituto Nazionale Tumori, according to Italian laws (INT-Institutional strategic projects “5x1000”), to S.M., and the Associazione Italiana Volontari Sangue provinciale Bergamo, Italy.
Author information
Authors and Affiliations
Corresponding author
Supplementary information
Supplementary Figure S1
(PDF 635 kb)
Supplementary Material
(DOC 29 kb)
Rights and permissions
About this article
Cite this article
Catucci, I., Peterlongo, P., Ciceri, S. et al. PALB2 sequencing in Italian familial breast cancer cases reveals a high-risk mutation recurrent in the province of Bergamo. Genet Med 16, 688–694 (2014). https://doi.org/10.1038/gim.2014.13
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/gim.2014.13
Keywords
This article is cited by
-
Rare variants in FANCA induce premature ovarian insufficiency
Human Genetics (2019)
-
A synonymous germline variant PALB2 c.18G>T (p.Gly6=) disrupts normal splicing in a family with pancreatic and breast cancers
Breast Cancer Research and Treatment (2019)
-
The PALB2 p.Leu939Trp mutation is not associated with breast cancer risk
Breast Cancer Research (2016)
-
Analysis of PALB2 mutations in 155 Japanese patients with breast and/or ovarian cancer
International Journal of Clinical Oncology (2016)
-
Haplotype analyses of the c.1027C>T and c.2167_2168delAT recurrent truncating mutations in the breast cancer-predisposing gene PALB2
Breast Cancer Research and Treatment (2016)