Abstract
A vital step in the development of heart failure is the transition from compensatory cardiac hypertrophy to decompensated dilated cardiomyopathy (DCM) during cardiac remodeling under mechanical or pathological stress. However, the molecular mechanisms underlying the development of DCM and heart failure remain incompletely understood. In the present study, we investigate whether Gab1, a scaffolding adaptor protein, protects against hemodynamic stress-induced DCM and heat failure. We first observed that the protein levels of Gab1 were markedly reduced in hearts from human patients with DCM and from mice with experimental viral myocarditis in which DCM developed. Next, we generated cardiac-specific Gab1 knockout mice (Gab1-cKO) and found that Gab-cKO mice developed DCM in hemodynamic stress-dependent and age-dependent manners. Under transverse aorta constriction (TAC), Gab1-cKO mice rapidly developed decompensated DCM and heart failure, whereas Gab1 wild-type littermates exhibited adaptive left ventricular hypertrophy without changes in cardiac function. Mechanistically, we showed that Gab1-cKO mouse hearts displayed severe mitochondrial damages and increased cardiomyocyte apoptosis. Loss of cardiac Gab1 in mice impaired Gab1 downstream MAPK signaling pathways in the heart under TAC. Gene profiles further revealed that ablation of Gab1 in heart disrupts the balance of anti- and pro-apoptotic genes in cardiomyocytes. These results demonstrate that cardiomyocyte Gab1 is a critical regulator of the compensatory cardiac response to aging and hemodynamic stress. These findings may provide new mechanistic insights and potential therapeutic target for DCM and heart failure.
Similar content being viewed by others
Main
The progression of heart failure is associated with cardiac remodeling, the changes of cardiac structure and function in response to various stress conditions such as pressure overload-generated hemodynamic stress and aging-associated oxidative stress.1 Under hemodynamic stress, the heart undergoes a stage of compensated hypertrophy and then progresses into decompensated dilated cardiomyopathy (DCM) and heart failure.2 Cardiac hypertrophy is an adaptive, regulatory process, in which activation of cardiomyocyte survival pathways maintains cardiac homeostasis against external stress. During the transition from compensatory hypertrophy to DCM, cardiomyocyte death plays a critical role in development of heart failure.3, 4, 5, 6 However, the molecular mechanisms for controlling the balance of cell survival and cell death during cardiac remodeling remain poorly understood.
The Grb2-associated binder 1 (Gab1) is a member of the insulin receptor substrate-like multi-substrate docking protein family and expressed in various types of cells, including cardiomyocytes.7, 8, 9 It is a central mediator of growth factor receptor signaling.10, 11 Gab1 is phosphorylated by tyrosine kinases, and then phosphorylated Gab1 recruits and activates phosphatidylinositol 3-kinase (PI3K)/Akt and protein tyrosine phosphatase SHP2 (PTPN11)/mitogen-activated protein kinase (MAPK) pathways,10, 12, 13 both of which pathways are implicated in the transduction of signals governing cell proliferation, growth, survival and differentiation. Global Gab1 knockout (Gab1−/−) mice die between embryonic day e12.5 and e18.5, with multiple defects in the placenta, heart, liver, skin and muscular development. 14, 15 The abnormal placental development in Gab1−/− mice may cause the death of the Gab1−/− embryos and the resultant complex phenotypes. Recent studies with the generation of tissue-specific knockout mice provide more definitive clues regarding Gab1 functions in vivo. Our group and others have demonstrated that endothelial-specific Gab1 deficiency in mice impairs ischemia-induced angiogenesis.16, 17, 18 Moreover, in contrast to the defects in cardiac development observed in Gab1−/− mice, cardiomyocyte-specific Gab1 conditional knockout (Gab1-cKO) mice generated with the Cre-LoxP system are viable and display normal cardiac morphology at birth.19 Gab protein family has three members, Gab1, Gab2 and Gab3.7 It was reported that cardiomyocyte-specific Gab1/Gab2 double knockout mice displayed high mortality after birth with abnormal cardiac function. 19 However, the physiological and pathological functions of cardiac Gab1 in hemodynamic stress-induced cardiac remodeling in adult animals remain incompletely understood.
In the present study, we first observed that lower levels of cardiac Gab1 protein were associated with DCM in human and mouse hearts, and we further revealed that cardiac-specific Gab1 knockout (Gab1-cKO) mice developed age-dependent progressive DCM and aortic banding-induced heart failure without the phase of compensated cardiac hypertrophy associated with cardiomyocyte mitochondrial damages and apoptosis.
Results
The levels of Gab1 protein in both human and mouse heart with DCM were decreased
To determine whether the protein levels of Gab1 are changed in diseased heart, we performed western blot analysis on the samples of explanted human hearts from patients diagnosed with DCM undergoing cardiac transplantation (Supplementary Table S1). Donor hearts without cardiomyopathy were used as controls. As shown in Figure 1a, the levels of Gab1 protein were significantly diminished in DCM hearts than those in control hearts (Figure 1a).
Reduced protein levels of Gab1 in both human and mouse heart with dilated cardiomyopathy. (a and b) Western blot analysis of protein levels of Gab1 and GAPDH (loading control) in human heart samples collected from control donor heart (n=5) and explanted dilated cardiomyopathy heart; n=5. **P<0.01. (b) Myocarditis-susceptible A/J mice were infected with coxsackievirus B3 (n=6) or mock (the same volume of PBS without coxsackievirus B3, vehicle control) (n=3) treatment for 9 days. Western blotting was carried out for detection of protein levels of Gab1 and GAPDH (loading control) in infected mouse heart. The blots were quantified by using NIH ImageJ software (Bethesda, MD, USA) and normalized with GAPDH
Viral myocarditis is a common cause of DCM.20 We further examined the expression levels of Gab1 in the mouse model of coxsackievirus infection-induced myocarditis and DCM.21 We found that the levels of Gab1 protein were dramatically reduced in mouse hearts infected with coxsackievirus (Figure 1b). Collectively, these results suggest a possible role of Gab1 in the regulation of cardiac function and remodeling.
Characterization of cardiac-specific Gab1-cKO mice
To explore the role of cardiac Gab1 in vivo, we generated Gab1-cKO mice by crossing Gab1 flox mice22 with transgenic mice expressing mouse cardiac-specific α-myosin heavy chain (α-MHC) promoter-driven Cre recombinase (Supplementary Figure S1). Gab1-cKO (α-MHC-Cre; Gab1flox/flox) mice were viable and born at the expected Mendelian ratio (Supplementary Table S2). As expected, we observed the genetic Gab1 deletion specifically in the heart but not other tissues of Gab1-cKO mice. Consistent with the previous report,19 we detected two isoforms of Gab1 protein in mouse hearts, of which the high-molecular-weight Gab1 isoform is cardiac specific, whereas lower-molecular-weight Gab1 isoform is present in all tissues tested including heart, liver and lung (Supplementary Figure S2). Both isoforms of Gab1 were knocked down in cardiac Gab1 knockout mice (Supplementary Figure S2). To ask whether ablation of Gab1 in cardiomyocytes affects expression of downstream signaling molecule SHP2, we examined the level of SHP2 protein. There were no significant changes in cardiac SHP2 expression between Gab1-cKO and Gab1-wild type (Gab1-WT, Gab1flox/flox) mice (Supplementary Figure S2B). At the age of 6–8 weeks, phenotypically there were no obvious differences in body weight, the ratio of whole heart or left ventricular (LV) weight to body weight or tibia length between Gab1-cKO mice and Gab1-WT mice (Supplementary Table S3). The echocardiographic parameters such as end-diastolic/systolic LV internal dimension (LVIDd/LVIDs), ejection fraction (EF) or fractional shortening (FS), interventricular septal (IVS) thickness and LV posterior wall (LVPW) thickness were also not significantly different between two groups of mice. Moreover, hemodynamic data showed no significant differences in LV systolic pressure (LVSP), end-diastolic pressure (LVEDP), heart rate, the derivatives of LV pressure, contractility (LV dP/dt max) and relaxation (LV dP/dt min) between Gab1-cKO mice and Gab1-WT mice (Supplementary Table S3). Together, these results indicate that there were no significant differences in overall cardiac structure and function between Gab1-cKO and Gab1-WT mice at the age of 6–8 weeks.
Cardiac Gab1-deficient mice developed DCM and heart failure in response to pressure overload
We next examined the functional role of Gab1 in the heart under hemodynamic stress. Gab-cKO mice were subjected to transverse aorta constriction (TAC). Echocardiograph analysis was performed before and after TAC (Supplementary Table S4). Under 2 weeks of TAC, Gab1-WT mice developed compensatory hypertrophy (Figure 2a) with increased ratio of LV weight/tibia length (LVW/TL) (Figure 2b), LVPW thickening (Figure 2h), augmented cardiac fibrosis (Figure 2a lower panel, and Supplementary Figure S3 for the quantified results of cardiac fibrosis) and elevated expression of fetal response gene α-skeletal muscle actin (αSK) (Figure 2c), but still maintained normal cardiac structure and function without significant alterations in EF (Figures 2d and g). In contrast, Gab1-cKO mice developed severe ventricular dilation and heart failure after 2 weeks of TAC (Figure 2 and Supplementary Table S4). There were no significant differences of cardiac fibrosis between WT+TAC and Gab1-cKO+TAC groups (Figure 2a and Supplementary Figure S3). Echocardiography revealed a significant increase in LVW/TL, LVIDd and LVIDs and a significant decrease in EF and LVPW thickness in Gab1-cKO mice under TAC (Figures 2e–h, and Supplementary Table S4). Interestingly, αSK was downregulated in Gab1-cKO+TAC group compared with that in WT+TAC group, suggesting possible abnormal cardiac remodeling and decompensation in Gab1-cKO mice under hemodynamic stress (Figure 2c). In addition, because it has been reported that there might be cardiac toxicity because of Cre expression in heart, we used α-MHC-Cre mice as a Cre control as well. We found that there was no significant difference of cardiac function between mice expression Gab1-flox/flox (WT control) and mice expressing α-MHC-Cre (Cre control) alone (Supplementary Table S4). Echocardiography-derived LV mass (Supplementary Figure S4) was also significantly increased in Gab1-cKO+TAC group compared with that in WT+TAC group or Cre +TAC group, consistent with the results of LVW/TL.
Gab1-cKO mice developed severe ventricular dilation and heart failure in response to pressure overload. (a) Representative images of hearts from Gab1-WT and Gab1-cKO mice subjected to either sham operation (n=8) or transverse aortic constriction (TAC) for 2 weeks (n=12) (top panel). Histological sections stained with H&E (middle panel) and Masson’s trichrome for detection of fibrosis (bottom panel). Scale bars: top and middle, 2 mm; bottom, 50 μm. (b) Left ventricle weight/tibia length ratios (mean±S.E.M.) of Gab1-WT and Gab1-cKO mice were determined at 2 weeks after TAC or sham operation. (c) The α-skeletal actin (α-SK) mRNA expression after 2 weeks of TAC or sham operation. (d) Representative images of M-mode echocardiographic tracings from Gab1-WT and Gab1-cKO mice after 2 weeks of TAC or sham operation. (e–h) End-diastolic left ventricle internal diameter (LVIDd), end-systolic left ventricle internal diameter (LVIDs), ejection fraction (EF) and end-diastolic left ventricle posterior wall (LVPWd) of Gab1-WT and Gab1-cKO mice at 2 weeks after TAC or sham operation determined by echocardiography. One-way ANOVA for multiple groups followed by Bonferroni post hoc test *P<0.05; **P<0.01
Loss of cardiac Gab1 resulted in decreased ERK1/2 phosphorylation but increased p38 MAPK phosphorylation in the heart in response to pressure overload
It has been well established that Gab1 mediates growth factor-induced ERK1/2 activation through interacting with SHP2.23, 24, 25 It has also been reported that Gab1 attenuates proapoptotic cytokine tumor necrosis factor-triggered signaling via associating with and inhibiting Mekk3,26 an upstream protein kinase of p38 MAPK.27 Thus, we hypothesized that these MAPK signaling molecules are dysregulated in Gab1-cKO mice under TAC. We assessed the effects of cardiac Gab1 deletion on Gab1 downstream signaling in hearts of Gab1-cKO and Gab1-WT control mice after 2 weeks of TAC or sham operation. In agreement with previous studies,28, 29, 30 TAC increased ERK1/2 phosphorylation in Gab1-WT mice compared with sham control, but this response was impaired in Gab1-cKO mice (Figures 3a and b). TAC also induced p38MAPK phosphorylation in Gab1-WT mice, and this TAC-induced phosphorylation of p38MAPK was further enhanced in Gab1-cKO mice. However, there were no significant differences in Akt phosphorylation between Gab1-WT and Gab1-cKO mice subjected to either TAC or sham operation (Figures 3a and b). These findings indicate that cardiac-specific Gab1 deficiency leads to decreased ERK1/2 phosphorylation and increased p38MAPK phosphorylation in response to hemodynamic stress.
Impaired activation of MAPK pathway in heart from Gab1-cKO mice in response to pressure overload. (a) Representative western blots from cardiac lysates of Gab1-cKO mice and WT mice subjected to TAC or sham operation, probed with phospho-ERK1/2/total ERK1/2; phospho-p38MAPK/total p38MAPK; and phosphor-Akt/total Akt. (b) Quantification by densitometry of ratios of phospho-ERK1/2/total ERK1/2; phospho-p38MAPK/total p38MAPK; and phospho-Akt/total Akt. Each of the gels represented two mouse hearts in each group. The graphs represents n=6 of hearts for each group of mice. *P<0.05; **P<0.01
Cardiac-specific Gab1 deletion led to compromised mitochondrial structure and function and enhanced cardiomyocyte apoptosis in response to pressure overload
Because ERK1/2 activation generally promotes cell survival and p38MAPK activation is associated with cell apoptosis, we next asked whether Gab1 deficiency-induced downregulation of ERK1/2 activation and upgregulation of p38MAPK activation would lead to cardiomyocyte apoptosis. Terminal deoxynucleotidyl transferase dUTP nick end labeling (TUNEL) assays to detect apoptosis cells and wheat germ agglutinin (WGA) staining indicating cardiomyocyte membrane were performed for apoptosis detection. We found that the number of apoptotic cardiomyocytes was dramatically increased in response to TAC in Gab1-cKO mice compared with Gab1-WT mice (Figures 4a and b).
Increased cardiomyocyte apoptosis in Gab1-cKO mice in response to pressure overload. (a and b) Increased apoptosis of cardiomyocytes. TUNEL-positive cardiomyocytes (WGA staining for cardiomyocyte membrane) from the heart histological sections of WT and Gab1-cKO mice after 2 weeks of TAC or sham operation. (c and d) Decreased ratio of Bcl-2/Bax mRNA. The levels of anti-apoptosis gene Bcl-2 and pro-apoptosis gene Bax expression after 2 weeks of TAC or sham operation were analyzed by semiquantitative RT-PCR. Two individual heart samples from each group were presented in each gel; n=4 hearts for each group. *P<0.05; **P<0.01
To further understand the molecular mechanisms underlying cardiac dysfunction in Gab1-cKO mice, we performed gene microarray analysis. Among several hundreds of genes that were altered in the heart of Gab1-cKO under TAC conditions, we found that many pro-apoptotic genes, such as Bax (Bcl-2-associated X protein) and Bnip3 (Bcl-2 and adenovirus E1B-19 kDa-interacting protein 3, an apoptotic inducer),31, 32 were upregulated (Supplementary Table S5), whereas several anti-apoptotic genes, including Bcl-2 (B-cell CLL/lymphoma 2) and Egr1 (early growth response 1), were down-regulated (Supplementary Table S6). A major checkpoint in cell death pathway is the ratio of pro-apoptotic (Bax) to anti-apoptotic (Bcl-2) members. Thus, we further examined the mRNA levels of Bcl-2 and Bax in heart tissues by reverse-transcript PCR analysis. The ratio of the mitochondrial anti-apoptotic protein Bcl-2 to pro-apoptotic protein Bax was increased in Gab1-WT mice subjected to TAC, but this pro-survival mechanism was impaired in Gab1-cKO mice (Figures 4c and d). These results revealed that ablation of Gab1 in heart disrupted the balance of anti- and pro-apoptotic genes in cardiomyocytes, resulting in cell apoptosis. Consistent with the results of the Masson’s trichrome staining for fibrosis, the data from our gene microarray showed that there was no obvious changes of cardiac collagen genes in heart from Gab1-cKO mice+TAC compared with WT mice+TAC groups (Supplementary Table S7).
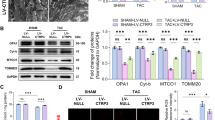
Mitochondrial dysfunction and caspase activation are two major execution programs downstream of Bcl-2/Bax in cell death pathway.33 Mitochondrial dysfunction includes a change in the mitochondrial membrane potential, production of reactive oxygen species, opening of the permeability transition pore and the release of cytochrome c. Released cytochrome c activates Apaf-1 that in turn activates a downstream caspase program. Thus, we examined mitochondria in cardiac muscle by the transmission electron microscope (TEM) studies. We observed normal Z-bands in cardiac muscle but damaged mitochondria associated with cristae lysis and abnormal internal membrane whorls in the hearts of Gab1-cKO mice after 2 weeks of TAC (Figure 5a and Supplementary Figures S5 and S6 showing high-resolution TEM images). The level of cleaved caspase-3, an enzymatic active form of caspase-3, was increased in Gab1-WT mice in response to TAC, and further enhanced in Gab1-cKO mice (Figures 5b and c). Together, these results suggest that mitochondrial function is compromised under hemodynamic stress conditions and exacerbated by the deletion of cardiac Gab1 that could trigger caspase activation and consequent apoptosis of cardiomyocytes and heart failure.34, 35
Severe mitochondrial damage and increased caspase-3 activation in heart of Gab1-cKO mice in response to pressure overload. (a) Transmission electronic microscopy of hearts from WT and Gab1-cKO mice after 2 weeks of TAC or sham operation. There were more frequently damaged mitochondria with cristae lysis and apparent abnormal internal membrane whorls in Gab1-cKO mice than those in WT mice. Z-bands were normal in both WT and Gab1-cKO mice. Scale bars: 1 μm (upper panel); 0.2 μm (lower panel). (b and c) The levels of activated caspase-3 (cleaved caspase-3) (uncleaved caspase-3 as a control for normalization) in Gab1-WT and Gab1-cKO hearts after 2 weeks of TAC or sham operation determined by western blots; n=4 of individual hearts per group. *P<0.05
Mice with cardiac Gab1 deficiency developed spontaneous DCM and heart failure by 3–6 months of age
Mitochondrial dysfunction and mitochondria oxidative stress have linked to age‐related heart diseases.36, 37, 38, 39 To examine the effects of age on heart function of Gab1-cKO mice, we continued to monitor cardiac function of Gab1-WT and Gab1-cKO mice via echocardiography as they aged from 4 weeks to 6 months. We found that at 3 months of age, Gab1-cKO mice exhibited a decreased EF and increased LVIDd, without obvious morphological changes and no apparent differences in LVPW compared with Gab1-WT mice. By 6 months of age, a severe DCM was observed in Gab1-cKO mice, with increased LVIDd and thinner LVPW compared with Gab1-WT mice (Figures 6a, b, d–f, and Supplementary Table S8). There were no apparent alterations in cardiac fibrosis between Gab1-cKO and Gab1-WT counterparts (see Figure 6c and Supplementary Figure S7 for the quantified results of cardiac fibrosis). Echocardiography-derived LV mass was significantly increased in Gab1-cKO mice at the age of 12 weeks and 6 months compared with those in WT mice (Supplementary Figure S8). At 6 months of age, caspase-3 cleavage was markedly increased in Gab1-cKO mice (Figures 7a and b), but there was no significant difference in both ERK and Akt phosphorylation between Gab1-cKO and Gab1-WT mice over time (Supplementary Figure S9). The TEM study also revealed the damaged mitochondria in Gab1-cKO mice at 6 months (Figure 7c), although not as severe as observed in young Gab1-cKO mice that underwent TAC.
Age-dependent progressive dilated cardiomyopathy and heart failure in Gab1-cKO mice. (a) Representative hearts from Gab1-WT and Gab1-cKO mice at 4, 8, 12 weeks and 6 months, respectively. (b) Corresponding histological sections stained with H&E. (c) Corresponding histological sections stained with Masson’s trichrome. (d–f) Ejection fraction (EF), end-diastolic left ventricle internal diameter (LVIDd) and the thickness of end-diastolic left ventricle posterior wall (LVPVd) were determined from the data of echocardiography. At age 3–6 months, EF in Gab1-cKO mice was considerably lower than those in Gab1-WT, and LVPVd was significantly thinner than those in Gab1-WT; n=8. *P<0.05; **P<0.01
Age-dependent activation of caspase-3 and mitochondrial damage in Gab1-cKO mice at age of 4 weeks to 6 months. (a) Representative western blots probed with cleaved caspase-3 antibody in the heart lysates at designated time points. (b) Statistical analysis of the ratio of cleaved to uncleaved caspase-3 between Gab1-cKO and WT mice at certain time points. At the age of 6 months, activation of caspase-3 significantly increased in Gab1-cKO mice as compared with WT mice; n=4, *P<0.05. (c) Transmission electronic microscopy of hearts from WT and Gab1-cKO mice at the age of 6 months. There were more frequently damaged mitochondria with cristae lysis and apparent abnormal internal membrane whorls in Gab1-cKO mice than those in WT mice. Z-bands were normal in both WT and Gab1-cKO mice. Scale bars: 1 μm (upper panel); 0.2 μm (lower panel)
Cardiac-specific Gab1 deletion in adulthood led to DCM and heart failure
To exclude the possibility of developmental abnormalities that may lead to adult phenotype manifestation, we crossed Gab1 floxed mice with αMHC-MerCreMer transgenic mice to generate an inducible, cardiac-specific Gab1-knockout (Gab1-icKO) mouse model. These mice were allowed to develop till 6–8 weeks at which time both Gab1-icKO mice and Gab1-WT mice were administered 35 mg/kg/day tamoxifen for 5 days to ablate Gab1 in the heart.40 We showed 70% knockdown of Gab1 protein expression in the heart from Gab1-icKO mice after tamoxifen treatment (Figures 8b and c). Gab1-icKO mice developed DCM in 2 weeks after tamoxifen treatment (Figure 8a). The ratio of LVW/TL in Gab1-icKO mice was significantly increased compared with that of Gab1-WT mice (Figure 8d). We also observed a 23% decrease of EF in Gab1-WT mice versus a 75% reduction of EF in Gab1-icKO mice at 2 weeks after tamoxifen treatment (Figure 8e). These results suggest that Gab1 deficiency in adult mice impairs cardiac function and potentially increased sensitivity to mild tamoxifen toxicity.41, 42
Inducible cardiac-specific deletion of Gab1 in adult mice leads to dilated cardiomyopathy and heart failure. (a) Representative hearts from Gab1-WT and Gab1 inducible-MHC-Cre knockout (Gab1-icKO) mice at 2 weeks after tamoxifen treatment for 5 consecutive days. (b) Representative western blots of Gab1 expressions from heart lysates of Gab1-WT or Gab1-icKO mice treated with tamoxifen. **P<0.01 versus WT group. (c) Gab1 expression was 70% knocked down after tamoxifen treatment in Gab1-icKO mice. (d) Ratio of heart weight to tibia length was significantly increased in Gab1-icKO mice after tamoxifen treatment. *P<0.05 versus WT group. (e) Ejection fraction was dramatically decreased in Gab1-icKO mice compared with Gab1-WT mice at 2 weeks after tamoxifen treatment; n=7. *P<0.05 versus WT without tamoxifen treatment; **P<0.01 versus WT treated with tamoxifen. (f) Working model for an in vivo role of Gab1 in regulation of cardiomyocyte apoptosis and DCM
Discussion
The major findings of the current study include: (1) Gab1 is downregulated in DCM heart; (2) loss of Gab1 in adult heart causes DCM under various pathological conditions, including pressure overload, aging and tamoxifen toxicity; (3) Gab1 is critical to maintain mitochondria integrity and function in cardiomyocytes; and (4) Gab1 deficiency impairs MAPK signaling pathways and disrupts the balance of anti-apoptotic and pro-apoptotic genes in adult heart, resulting in increased apoptosis. Beyond the previous report that Gab1 and Gab2 play an important role in the regulation of cardiac function in embryonic development and neonatal mice,8, 9, 19 our results demonstrate a novel signaling mechanism underlying pathological stress-induced DCM, in which Gab1 has emerged as a central regulator of adult cardiac function through maintaining mitochondrial integrity and cell survival to protect heart against DCM and heart failure (Figure 8f).
Gab1 plays a crucial role in the normal growth, differentiation and developmental programs,43 but the physiological and pathological functions of Gab1 in adult animals remain poorly understood. Global Gab1 knockout mice are embryonic lethal and die between e12.5 and e18.5 because of developmental defects in the heart, placenta and integument.15 In contrast, cardiac-specific Gab1 knockout mice are viable and have no obvious morphological and functional abnormality before 10 weeks.19 This is consistent with the phenotype of our Gab1-cKO mice at 6–8 weeks of age. Our results further showed that Gab1 is crucial for maintaining cardiac function under hemodynamic stress in adulthood. Specifically, Gab1-cKO mice at age 6–8 weeks exhibited DCM and heart failure shortly after TAC, whereas Gab1-WT mice displayed compensatory hypertrophy to maintain the normal function. Furthermore, we observed that Gab1-cKO mice developed age-related cardiomyopathy. In the absence of cardiac Gab1, mice at 6 months displayed a severe DCM with impaired systolic function and increased cardiac dilatation. In addition, ablation of cardiac Gab1 in adult Gab1-icKO mice also developed DCM in 2 weeks after tamoxifen treatment. Notably, the heart failure phenotype in Gab1-icKO mice developed much faster than Gab1-cKO mice. We used moderate amounts of tamoxifen (35 mg/kg/day) as many other laboratories described previously.44, 45, 46 In this dose of tamoxifen, its cardiac toxicity was minimal as reported by Bersell et al.42 Indeed, we observed a small but significant adverse effect of tamoxifen injection on cardiac ejection fraction of WT mice (Figure 8e). However, compared with Gab1-WT mice treated with tamoxifen, we found that Gab1-icKO mice treated with tamoxifen had much greater reduction of cardiac function (Figure 8e), and this could be because of intrinsic defects of cardiac function in Gab1-icKO mice or the intolerance of Gab1-icKO mice to mild tamoxifen cardiac toxicity. Collectively, our findings suggest that loss of cardiac Gab1 in adult causes DCM and heart failure under the pathological conditions such as abnormal hemodynamic stress.
Recent studies have demonstrated that signaling through MAPKs has crucial roles in cardiac biology. It was reported that gain-of-function mutations in PTPN11 (encoded SHP2)47, 48 and RAF149, 50 cause Noonan syndrome with hypertrophic cardiomyopathy, a genetic disorder in which the heart muscle becomes thick. In contrast, loss-of-function mutations of RAF1 in humans51 or genetic deletion of SHP228, 52 and Raf153 in mice cause DCM. As Gab1 is associated with SHP2 and regulates MAPK signaling, it is conceivable that loss of Gab1 could alter MAPK signaling, resulting in DCM. Indeed, our findings suggest that Gab1 is an essential component of the signaling pathways important for cardiomyocyte survival. In this study, we found that ERK1/2 phosphorylation significantly decreased but p38MAPK phosphorylation increased in Gab1-cKO mice compared with Gab1-WT mice under pressure overload. ERK1/2 phosphorylation is associated with concentric LV hypertrophy without signs of progression toward heart failure,54 and is thought to be a component of an consequential adaptive mechanism in the myocardium.55 The blunting of the ERK1/2 signaling using a dominant-negative Raf1 blocks adaptive cardiac hypertrophy, accompanied by an increase in apoptosis, and LV dysfunction, concluding with an enhancement in mortality rate when subjected to pressure overload.56 Genetic inhibition of cardiac ERK1/2 promotes stress-induced apoptosis and heart failure.57 Thus, the reduction of ERK1/2 activity could be part of the mechanisms by which cardiac Gab1 deficiency led to an increase in apoptosis and loss of hypertrophic growth in Gab1-cKO mice under TAC. On the other hand, p38 MAPK acts as an enhancer of myocyte apoptosis and cardiac pathologies and is believed to play a causative role in DCM in the cardiac stress responses.58, 59 It has been shown that gain of function of p38 MAPK in transgenic mice causes LV chamber dilation associated with reduced wall thickness, but no significant hypertrophy at the organ level,60, 61 consistent with the phenotype observed in Gab1-cKO mice under pressure overload. Taken together, our results suggest that dysregulation of the MAPK pathway could be the signaling mechanisms responsible for increased cardiomyocyte apoptosis and subsequent DCM observed in Gab1-cKO mice. Future studies are warranted to screen possible genome-wide association of Gab1 mutations with DCM in humans.
Mitochondrial integrity in cardiomyocytes is critical to maintain normal cardiac function, and abnormality of mitochondrial morphology and function is associated with LV dysfunction and heart failure.62 In this study, TEM analysis showed damaged mitochondria with cristae lysis and apparent abnormal internal membrane whorls, but normal Z-bands in the heart of Gab1-cKO mice after 2 weeks of TAC or at the age of 6 months. Furthermore, Gab1-cKO mice subjected to TAC also increased mitochondrial membrane potential. These findings indicate that cardiac-specific Gab1 deletion compromises mitochondrial integrity in response to pressure overload and during aging process. Mechanistically, DNA microarray showed a dramatically decreased level of Bcl-2 but no significant differences in the level of Bax in Gab1-cKO mice under TAC. The ratio of Bcl-2 to Bax determines survival or death after an apoptotic stimulus.63 We found that the Bcl-2/Bax ratio in Gab1-cKO mice was significantly lower than that in Gab1-WT mice. Furthermore, the activation of caspase-3 and the number of TUNEL-positive cells were significantly increased in the heart of Gab1-cKO mice under TAC. Together, our findings suggest that Gab1 is involved in the regulation of the function and structure of cardiac mitochondria that not only produce energy to maintain cardiac function but also tightly regulate cell survival and death.
The exact mechanism of the downregulation of Gab1 in human and mouse heart with DCM remains unclear. It was previously reported that long-term treatment with insulin-like growth factor-1 (IGF-1) results in decreased Gab1 protein expression.26 High levels of IGF-1 have been associated with heart failure and increased cardiac mortality.64, 65 Thus, it is postulated that downregulation of Gab1 is a result of increased IGF-1. Alternatively, the loss of Gab1 may be due to increased degradation through the ubiquitin–proteasome system. Recent studies have shown that in response to the treatment of hepatocyte growth factor Gab1 is ubiquitinated by the E3 ligase Cbl, and subsequently degraded by the 26S proteasome.66 Future investigation is required to precisely delineate the mechanism of the downregulation of Gab1 in the hearts with DCM. It would also be interesting to determine whether a decrease of Gab1 function in heart may contribute to the development of DCM in humans.
In conclusion, our results demonstrate that Gab1 protects the heart against DCM and heart failure, likely through maintaining mitochondrial integrity and cell survival. These findings may provide new mechanistic insights and potential therapeutic target for DCM and heart failure.
Materials and Methods
A detailed description of the methods used in the present study can be found in Supplementary Data.
Human heart tissues
Human frozen tissues from the LV free wall of explanted DCM hearts and donor hearts were obtained from the Cardiovascular Registry at the Centre for Heart Lung Innovation following approval by the University of British Columbia Research Ethics Board. Patient characteristics are summarized in Supplementary Table S1.
Animals and models
All experimental procedures involving animals were approved by the local animal care and use committees according to the Guide for the Care and Use of Laboratory Animals prepared by the US National Academy of Sciences (National Institutes of Health publication No. 85–23, revised 1996). Generation and characterization of Gab1-cKO mouse models are described in Results. Hypertrophy and DCM were induced by transverse aortic constriction in Gab1 WT and KO mice under C57BL/6 background.
Coxsackievirus infection in mice
A/J mice were purchased from the Jackson Laboratory (Bar Harbor, ME, USA). Male mice at age 4–5 weeks were either infected intraperitoneally (i.p.) with 105 plaque-forming units of coxsackievirus B3 (n=6) or mock (the same volume of PBS without coxsackievirus B3) vehicle treatment (n=3). On day 9 after virus infection, mice were killed and infected hearts were harvested. All procedures were approved by the Animal Care Committee at the University of British Columbia.
Echocardiography
Echocardiography was performed on unconscious mice lightly anesthetized by 1.5% isoflurane. Imaging was captured with a Visual Sonics Vevo 2100 High-Resolution Imaging System (Toronto, ON, Canada)67 along with recording of temperature, breathing rate and ECG. The echocardiographer was blinded to mouse genotypes.
Data analysis
All data are expressed as mean±S.E.M. Comparisons between experimental groups were performed with Student’s t-test for two groups or ANOVA for multiple groups followed by Bonferroni post hoc test. Statistical significance was set at P-value <0.05.
Abbreviations
- Gab1:
-
Grb2-associated binder 1
- DCM:
-
dilated cardiomyopathy
- Gab1-cKO:
-
cardiac-specific Gab1 knockout
- TAC:
-
transverse aorta constriction
- MAPK:
-
mitogen-activated protein kinases
- PI3K:
-
phosphatidylinositol 3-kinase
- WT:
-
wild type
- LV:
-
left ventricular
- LVIDd:
-
end-diastolic left ventricular internal dimension
- LVIDs:
-
end-systolic left ventricular internal dimension
- EF:
-
ejection fraction
- FS:
-
fractional shortening
- IVS:
-
interventricular septal thickness
- LVPW:
-
left ventricular posterior wall thickness
- LVSP:
-
left ventricular systolic pressure
- LVEDP:
-
left ventricular end-diastolic pressure
- LVW:
-
left ventricular weight
- TL:
-
tibia length
- αSK:
-
α-skeletal muscle actin
- p38 MAPK:
-
p38 mitogen-activated protein kinase
- TUNEL:
-
terminal deoxynucleotidyl transferase dUTP nick end labeling
- WGA:
-
wheat germ agglutinin
- Bax:
-
Bcl-2-associated X protein
- Bnip3:
-
Bcl-2 and adenovirus E1B-19 kDa-interacting protein 3
- Bcl-2:
-
B-cell CLL/lymphoma 2
- Egr1:
-
early growth response 1
- TEM:
-
transmission electron microscope
References
Hill JA, Olson EN . Cardiac plasticity. N Engl J Med 2008; 358: 1370–1380.
Kehat I, Molkentin JD . Molecular pathways underlying cardiac remodeling during pathophysiological stimulation. Circulation 2010; 122: 2727–2735.
Olivetti G, Abbi R, Quaini F, Kajstura J, Cheng W, Nitahara JA et al. Apoptosis in the failing human heart. N Engl J Med 1997; 336: 1131–1141.
Akyurek O, Akyurek N, Sayin T, Dincer I, Berkalp B, Akyol G et al. Association between the severity of heart failure and the susceptibility of myocytes to apoptosis in patients with idiopathic dilated cardiomyopathy. Int J Cardiol 2001; 80: 29–36.
Dorn GW 2nd . Mitochondrial pruning by Nix and BNip3: an essential function for cardiac-expressed death factors. J Cardiovasc Transl Res 2010; 3: 374–383.
Harvey PA, Leinwand LA . The cell biology of disease: cellular mechanisms of cardiomyopathy. J Cell Biol 2011; 194: 355–365.
Gu H, Neel BG . The ‘gab’ in signal transduction. Trends Cell Biol 2003; 13: 122–130.
Nakaoka Y, Nishida K, Fujio Y, Izumi M, Terai K, Oshima Y et al. Activation of gp130 transduces hypertrophic signal through interaction of scaffolding/docking protein Gab1 with tyrosine phosphatase SHP2 in cardiomyocytes. Circ Res 2003; 93: 221–229.
Wang Y . Fill a Gab(1) in cardiac hypertrophy signaling: search a missing link between gp130 and ERK5 in hypertrophic remodeling in heart. Circ Res 2003; 93: 186–188.
Holgado-Madruga M, Moscatello DK, Emlet DR, Dieterich R, Wong AJ . Grb2-associated binder-1 mediates phosphatidylinositol 3-kinase activation and the promotion of cell survival by nerve growth factor. Proc Natl Acad Sci USA 1997; 94: 12419–12424.
Weidner KM, Di Cesare S, Sachs M, Brinkmann V, Behrens J, Birchmeier W . Interaction between Gab1 and the c-Met receptor tyrosine kinase is responsible for epithelial morphogenesis. Nature 1996; 384: 173–176.
Holgado-Madruga M, Emlet DR, Moscatello DK, Godwin AK, Wong AJ . A Grb2-associated docking protein in EGF- and insulin-receptor signalling. Nature 1996; 379: 560–564.
Fixman ED, Holgado-Madruga M, Nguyen L, Kamikura DM, Fournier TM, Wong AJ et al. Efficient cellular transformation by the Met oncoprotein requires a functional Grb2 binding site and correlates with phosphorylation of the Grb2-associated proteins, Cbl and Gab1. J Biol Chem 1997; 272: 20167–20172.
Sachs M, Brohmann H, Zechner D, Muller T, Hulsken J, Walther I et al. Essential role of Gab1 for signaling by the c-Met receptor in vivo. J Cell Biol 2000; 150: 1375–1384.
Itoh M, Yoshida Y, Nishida K, Narimatsu M, Hibi M, Hirano T . Role of Gab1 in heart, placenta, and skin development and growth factor- and cytokine-induced extracellular signal-regulated kinase mitogen-activated protein kinase activation. Mol Cell Biol 2000; 20: 3695–3704.
Zhao J, Wang W, Ha CH, Kim JY, Wong C, Redmond EM et al. Endothelial Grb2-associated binder 1 is crucial for postnatal angiogenesis. Arterioscler Thromb Vasc Biol 2011; 31: 1016–1023.
Shioyama W, Nakaoka Y, Higuchi K, Minami T, Taniyama Y, Nishida K et al. Docking protein Gab1 is an essential component of postnatal angiogenesis after ischemia via HGF/c-met signaling. Circ Res 2011; 108: 664–675.
Lu Y, Xiong Y, Huo Y, Han J, Yang X, Zhang R et al. Grb-2-associated binder 1 (Gab1) regulates postnatal ischemic and VEGF-induced angiogenesis through the protein kinase A-endothelial NOS pathway. Proc Natl Acad Sci USA 2011; 108: 2957–2962.
Nakaoka Y, Nishida K, Narimatsu M, Kamiya A, Minami T, Sawa H et al. Gab family proteins are essential for postnatal maintenance of cardiac function via neuregulin-1/ErbB signaling. J Clin Invest 2007; 117: 1771–1781.
Pankuweit S, Klingel K . Viral myocarditis: from experimental models to molecular diagnosis in patients. Heart Fail Rev 2013; 18: 683–702.
Gao G, Zhang J, Si X, Wong J, Cheung C, McManus B et al. Proteasome inhibition attenuates coxsackievirus-induced myocardial damage in mice. Am J Physiol Heart Circ Physiol 2008; 295: H401–H408.
Bard-Chapeau EA, Hevener AL, Long S, Zhang EE, Olefsky JM, Feng GS . Deletion of Gab1 in the liver leads to enhanced glucose tolerance and improved hepatic insulin action. Nat Med 2005; 11: 567–571.
Nishida K, Yoshida Y, Itoh M, Fukada T, Ohtani T, Shirogane T et al. Gab-family adapter proteins act downstream of cytokine and growth factor receptors and T- and B-cell antigen receptors. Blood 1999; 93: 1809–1816.
Shi ZQ, Yu DH, Park M, Marshall M, Feng GS . Molecular mechanism for the SHP-2 tyrosine phosphatase function in promoting growth factor stimulation of ERK activity. Mol Cell Biol 2000; 20: 1526–1536.
Cunnick JM, Dorsey JF, Munoz-Antonia T, Mei L, Wu J . Requirement of SHP2 binding to Grb2-associated binder-1 for mitogen-activated protein kinase activation in response to lysophosphatidic acid and epidermal growth factor. J Biol Chem 2000; 275: 13842–13848.
Che W, Lerner-Marmarosh N, Huang Q, Osawa M, Ohta S, Yoshizumi M et al. Insulin-like growth factor-1 enhances inflammatory responses in endothelial cells: role of Gab1 and MEKK3 in TNF-alpha-induced c-Jun and NF-kappaB activation and adhesion molecule expression. Circ Res 2002; 90: 1222–1230.
Uhlik MT, Abell AN, Johnson NL, Sun W, Cuevas BD, Lobel-Rice KE et al. Rac-MEKK3-MKK3 scaffolding for p38 MAPK activation during hyperosmotic shock. Nat Cell Biol 2003; 5: 1104–1110.
Kontaridis MI, Yang W, Bence KK, Cullen D, Wang B, Bodyak N et al. Deletion of Ptpn11 (Shp2) in cardiomyocytes causes dilated cardiomyopathy via effects on the extracellular signal-regulated kinase/mitogen-activated protein kinase and RhoA signaling pathways. Circulation 2008; 117: 1423–1435.
De Acetis M, Notte A, Accornero F, Selvetella G, Brancaccio M, Vecchione C et al. Cardiac overexpression of melusin protects from dilated cardiomyopathy due to long-standing pressure overload. Circ Res 2005; 96: 1087–1094.
White DE, Coutu P, Shi YF, Tardif JC, Nattel S, St Arnaud R et al. Targeted ablation of ILK from the murine heart results in dilated cardiomyopathy and spontaneous heart failure. Genes Dev 2006; 20: 2355–2360.
Yussman MG, Toyokawa T, Odley A, Lynch RA, Wu G, Colbert MC et al. Mitochondrial death protein Nix is induced in cardiac hypertrophy and triggers apoptotic cardiomyopathy. Nat Med 2002; 8: 725–730.
Diwan A, Wansapura J, Syed FM, Matkovich SJ, Lorenz JN, Dorn GW 2nd . Nix-mediated apoptosis links myocardial fibrosis, cardiac remodeling, and hypertrophy decompensation. Circulation 2008; 117: 396–404.
Gross A, McDonnell JM, Korsmeyer SJ . Bcl-2 family members and the mitochondria in apoptosis. Genes Dev 1999; 13: 1899–1911.
Chan DC . Mitochondria: dynamic organelles in disease, aging, and development. Cell 2006; 125: 1241–1252.
Huss JM, Kelly DP . Mitochondrial energy metabolism in heart failure: a question of balance. J Clin Invest 2005; 115: 547–555.
Sachs HG, Colgan JA, Lazarus ML . Ultrastructure of the aging myocardium: a morphometric approach. Am J Anat 1977; 150: 63–71.
Jacoby JJ, Kalinowski A, Liu MG, Zhang SS, Gao Q, Chai GX et al. Cardiomyocyte-restricted knockout of STAT3 results in higher sensitivity to inflammation, cardiac fibrosis, and heart failure with advanced age. Proc Natl Acad Sci USA 2003; 100: 12929–12934.
Dutta D, Calvani R, Bernabei R, Leeuwenburgh C, Marzetti E . Contribution of impaired mitochondrial autophagy to cardiac aging: mechanisms and therapeutic opportunities. Circ Res 2012; 110: 1125–1138.
Yoshioka J . Thioredoxin Reductase 2 (Txnrd2) regulates mitochondrial integrity in the progression of age-related heart failure. J Am Heart Assoc 2015; 4: e002278.
Zhang D, Contu R, Latronico MV, Zhang J, Rizzi R, Catalucci D et al. MTORC1 regulates cardiac function and myocyte survival through 4E-BP1 inhibition in mice. J Clin Invest 120: 2805–2816.
Koitabashi N, Bedja D, Zaiman AL, Pinto YM, Zhang M, Gabrielson KL et al. Avoidance of transient cardiomyopathy in cardiomyocyte-targeted tamoxifen-induced mercremer gene deletion models. Circ Res 2009; 105: 12–15.
Bersell K, Choudhury S, Mollova M, Polizzotti BD, Ganapathy B, Walsh S et al. Moderate and high amounts of tamoxifen in alphamhc-mercremer mice induce a DNA damage response, leading to heart failure and death. Dis Model Mech 2013; 6: 1459–1469.
Liu Y, Rohrschneider LR . The gift of gab. FEBS Lett 2002; 515: 1–7.
Xiong D, Yajima T, Lim BK, Stenbit A, Dublin A, Dalton ND et al. Inducible cardiac-restricted expression of enteroviral protease 2A is sufficient to induce dilated cardiomyopathy. Circulation 2007; 115: 94–102.
Dong F, Harvey J, Finan A, Weber K, Agarwal U, Penn MS . Myocardial CXCR4 expression is required for mesenchymal stem cell mediated repair following acute myocardial infarction. Circulation 2012; 126: 314–324.
Perricone AJ, Bivona BJ, Jackson FR, Vander Heide RS . Conditional knockout of myocyte focal adhesion kinase abrogates ischemic preconditioning in adult murine hearts. J Am Heart Assoc 2013; 2: e000457.
Tartaglia M, Mehler EL, Goldberg R, Zampino G, Brunner HG, Kremer H et al. Mutations in PTPN11, encoding the protein tyrosine phosphatase SHP-2, cause Noonan syndrome. Nat Genet 2001; 29: 465–468.
Araki T, Mohi MG, Ismat FA, Bronson RT, Williams IR, Kutok JL et al. Mouse model of noonan syndrome reveals cell type- and gene dosage-dependent effects of PTPN11 mutation. Nat Med 2004; 10: 849–857.
Razzaque MA, Nishizawa T, Komoike Y, Yagi H, Furutani M, Amo R et al. Germline gain-of-function mutations in RAF1 cause Noonan syndrome. Nat Genet 2007; 39: 1013–1017.
Pandit B, Sarkozy A, Pennacchio LA, Carta C, Oishi K, Martinelli S et al. Gain-of-function RAF1 mutations cause Noonan and Leopard syndromes with hypertrophic cardiomyopathy. Nat Genet 2007; 39: 1007–1012.
Dhandapany PS, Razzaque MA, Muthusami U, Kunnoth S, Edwards JJ, Mulero-Navarro S et al. RAF1 mutations in childhood-onset dilated cardiomyopathy. Nat Genet 2014; 46: 635–639.
Princen F, Bard E, Sheikh F, Zhang SS, Wang J, Zago WM et al. Deletion of SHP2 tyrosine phosphatase in muscle leads to dilated cardiomyopathy, insulin resistance, and premature death. Mol Cell Biol 2009; 29: 378–388.
Yamaguchi O, Watanabe T, Nishida K, Kashiwase K, Higuchi Y, Takeda T et al. Cardiac-specific disruption of the c-raf-1 gene induces cardiac dysfunction and apoptosis. J Clin Invest 2004; 114: 937–943.
Bueno OF, De Windt LJ, Tymitz KM, Witt SA, Kimball TR, Klevitsky R et al. The MEK1-ERK1/2 signaling pathway promotes compensated cardiac hypertrophy in transgenic mice. EMBO J 2000; 19: 6341–6350.
Bueno OF, Molkentin JD . Involvement of extracellular signal-regulated kinases 1/2 in cardiac hypertrophy and cell death. Circ Res 2002; 91: 776–781.
Harris IS, Zhang S, Treskov I, Kovacs A, Weinheimer C, Muslin AJ . Raf-1 kinase is required for cardiac hypertrophy and cardiomyocyte survival in response to pressure overload. Circulation 2004; 110: 718–723.
Purcell NH, Wilkins BJ, York A, Saba-El-Leil MK, Meloche S, Robbins J et al. Genetic inhibition of cardiac ERK1/2 promotes stress-induced apoptosis and heart failure but has no effect on hypertrophy in vivo. Proc Natl Acad Sci USA 2007; 104: 14074–14079.
Liang Q, Molkentin JD . Redefining the roles of p38 and jnk signaling in cardiac hypertrophy: dichotomy between cultured myocytes and animal models. J Mol Cell Cardiol 2003; 35: 1385–1394.
Peter PS, Brady JE, Yan L, Chen W, Engelhardt S, Wang Y et al. Inhibition of p38 alpha MAPK rescues cardiomyopathy induced by overexpressed beta 2-adrenergic receptor, but not beta 1-adrenergic receptor. J Clin Invest 2007; 117: 1335–1343.
Liao P, Georgakopoulos D, Kovacs A, Zheng M, Lerner D, Pu H et al. The in vivo role of p38 map kinases in cardiac remodeling and restrictive cardiomyopathy. Proc Natl Acad Sci USA 2001; 98: 12283–12288.
Petrich BG, Wang Y . Stress-activated map kinases in cardiac remodeling and heart failure; new insights from transgenic studies. Trends Cardiovasc Med 2004; 14: 50–55.
Abel ED, Doenst T . Mitochondrial adaptations to physiological vs pathological cardiac hypertrophy. Cardiovasc Res 90: 234–242.
Oltvai ZN, Milliman CL, Korsmeyer SJ . Bcl-2 heterodimerizes in vivo with a conserved homolog, Bax, that accelerates programmed cell death. Cell 1993; 74: 609–619.
Chisalita SI, Dahlstrom U, Arnqvist HJ, Alehagen U . Increased IGF1 levels in relation to heart failure and cardiovascular mortality in an elderly population: impact of ACE inhibitors. Eur J Endocrinol 2011; 165: 891–898.
Sundaresan NR, Vasudevan P, Zhong L, Kim G, Samant S, Parekh V et al. The sirtuin SIRT6 blocks IGF-Akt signaling and development of cardiac hypertrophy by targeting c-Jun. Nat Med 2012; 18: 1643–1650.
Goormachtigh G, Ji Z, Le Goff A, Fafeur V . Degradation of the GAB1 adaptor by the ubiquitin-proteasome pathway hampers HGF/SF-MET signaling. Biochem Biophys Res Commun 2011; 411: 780–785.
Ram R, Mickelsen DM, Theodoropoulos C, Blaxall BC . New approaches in small animal echocardiography: imaging the sounds of silence. Am J Physiol Heart Circ Physiol 2011; 301: H1765–H1780.
Acknowledgements
We acknowledge technical assistance from Chelsea Wong for the histological studies, Deanne M Mickelsen and Kyung Ae Ko for the echocardiograph studies and Karen L Bentley for the electron microscopy studies. This work was supported by NIH Grants (HL80611, HL109502 and HL114570 to ZGJ), a Research Award from American Diabetes Association (7-12-BS-085 to ZGJ) and grants from the Canadian Institutes of Health Research (to HL).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Edited by JA Cidlowski
Supplementary Information accompanies this paper on Cell Death and Differentiation website
Supplementary information
Rights and permissions
About this article
Cite this article
Zhao, J., Yin, M., Deng, H. et al. Cardiac Gab1 deletion leads to dilated cardiomyopathy associated with mitochondrial damage and cardiomyocyte apoptosis. Cell Death Differ 23, 695–706 (2016). https://doi.org/10.1038/cdd.2015.143
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/cdd.2015.143
This article is cited by
-
Self-assembly of DNA nanostructure containing cell-specific aptamer as a precise drug delivery system for cancer therapy in non-small cell lung cancer
Journal of Nanobiotechnology (2022)
-
Gab1 Overexpression Attenuates Susceptibility to Ventricular Arrhythmias in Pressure Overloaded Heart Failure Mouse Hearts
Cardiovascular Drugs and Therapy (2022)
-
Advances in the role and mechanism of BAG3 in dilated cardiomyopathy
Heart Failure Reviews (2021)
-
Recent advances of adapter proteins in the regulation of heart diseases
Heart Failure Reviews (2017)