Abstract
Background:
There are limited data comparing the prognosis and fertility outcomes of the patients with early cervical cancer treated by trans-vaginal radical trachelectomy (VRT) or abdominal radical trachelectomy (ART).The objective of this study was to compare the surgical and pathologic characteristics, the prognosis and fertility outcomes of the patients treated by VRT or ART.
Methods:
Matched-case study based on a prospectively maintained database of patients underwent radical trachelectomy in 10 centres of China was designed to compare the prognosis and fertility outcomes of the patients treated by VRT or ART.
Results:
Totally 150 cases, 77 in the VRT and 73 in the ART group, were included. VRT and ART provide similar surgical and pathological outcomes except larger specimens obtained by ART. In the ART group, no patient developed recurrent diseases, but, in the VRT group, 7 (9.8%) patients developed recurrent diseases and 2 (1.6%) patients died of the tumours (P=0.035). The rate of pregnancy in the VRT group was significantly higher than those of ART (39.5% vs 8.8%; P=0.003). The patients with tumour size >2 cm showed significant higher recurrent rate (11.6% vs 2.4%, P<0.05) and lower pregnant rate (12.5% vs 32.1%, P=0.094) compared with the patients with tumour size <2 cm.
Conclusion:
Patients treated by ART obtained better oncology results, but their fertility outcomes were unfavourable compared with VRT. Tumour size <2 cm should be emphasised as an indication for radical trachelectomy for improving the outcome of fertility and prognosis.
Similar content being viewed by others
Materials and methods
Patient’s information
A prospectively maintained database of patients undergoing RT in 10 centres in China was established and analysed. Patients’ information was collected from standard case report forms, which represented a standard protocol followed by all centres. In this prospective, multi-center, comparative research, the inclusion criteria into the study were as follows: (1) patients aged between 18 and 40; (2) pathologically confirmed invasive cervical cancer; (3) strong desire to preserve fertility; (4) FIGO stage IA1 with lymph vascular space invasion (LVSI), stage IA2 or IB1 with tumour size <4 cm (assessed clinically or by MRI); and (5) no evidence of disease outside the cervix. Patients’ data, including age, symptoms, clinical features, FIGO stage, histological types, surgical parameters, perioperative complications, results of follow-up, pregnancy rate and fertility outcomes, were collected from the clinical database and patients’ medical records. Data were comparatively analysed as a cohort for the purpose of this study.
Protocol approvals and patient consents
The study protocal was approved by each site’s board review and the ethics committee. The written informed consent was obtained from each patient.
Treatment plan
After the histological diagnosis and a signed consent form were obtained, the patient was operated by RT either vaginally or abdominally according to the patient’s desire and surgeon’s skills. The detailed techniques for VRT and ART have been described in previous reports (Shen et al, 2006; Li et al, 2011), but we stopped performing cervical cerclage after 2007. Both VRTs and ARTs were performed by experienced gynaecological oncologists. Duration of surgery was measured from the time of skin incision to suture of the skin or the vagina. Volume of blood loss was measured during each operation. Perioperative complications, such as injuries to the vessels, bowels, bladder or ureters, and postoperative complications, such as massive bleeding, infections, bladder dysfunction, intestinal obstruction, or cervical stenosis, were recorded.
All specimens were reviewed independently by two pathologists. A third pathologist was consulted if the previous two pathologists made different diagnosis. We used the average parametrical width of both sides measured by pathologists and recorded in the final pathology report in order to eliminate surgeon bias. The average length of the excised cervical specimens and the median lymph nodes obtained from both sides were also extracted from the final pathology report. The average parametrical width and the length of the excised cervix were obtained from the formaldehyde-fixed specimens, which were measured by pathologists who were blind to the surgical procedure. Adjuvant chemotherapy was offered to patients with at least one of these three risk factors: (1) cervical stromal invasion more than 1/2; (2) less than 5 mm uninvolved endocervical or vaginal margin; and (3) parametrial LVSI. Before the RT, 13 patients in the VRT group and 4 patients in the ART group were offered neo-adjuvant chemotherapy because of tumour size >2 cm. In order to preserve the fertility, adjuvant chemotherapy was given to four patients in the VRT group and to three in the ART group postoperatively, all of these having at least one of the risk factors described above. Regimen TP (paclitaxol 175 mg m−2 plus cisplatin 70 mg m−2, repeated every 3 weeks) or PF (cisplatin 70 mg m−2 d1 plus fluorouracil 1000 mg m−2 d1-4, repeated every 4 weeks) was used as NACT or adjuvant chemotherapy.
Evaluation of the patients after radical trachelectomy
Regular follow-up was carried out for all patients after RT by a gynaecological oncologist. Patients were followed-up every 2–3 months for 2 years, every 6 months for 3 years and then yearly. Each follow-up visit included a physical and pelvic examination, Pap smear test for new external os, pelvic ultrasound examination and serum tumour marker (SCC antigen for squamous cell cancer or CA125 for adenocarcinoma). Colposcopic examination and biopsy were performed for patients with abnormal pap smear. Positron emission tomography scan (PET-CT) was performed in cases of suspected recurrence. Follow-up duration was measured from the day of operation to the day of last follow-up, death or lost to follow-up. Recurrence was confirmed by biopsy or positive PET-CT scan.
After a 6-month follow-up period without any evidence of residual or recurrent disease, patients were advised to try to conceive. When pregnancy was confirmed using HCG assay and ultrasonography, patients were referred to obstetric clinic for perinatal assessment. Pregnant women were followed-up by an obstetrician and their gynaecological oncologist during and after the pregnancy. Cervical cytology was regularly assessed before, during and after pregnancy. A detailed gynecologic and colposcopic evaluation was carried out if there was any abnormal cervical cytological finding. Infertility work-up and artificial reproductive techniques (ART) were performed if the patients failed to conceive 2 years after RT procedure.
Statistical analysis
Statistical analyses were performed using the SPSS 17.0 software (Chicago, IL, USA). Student’s t tests were used to compare the continuous variables, and χ2-tests were used for categorical data. Fisher’s exact test was used when it was necessary. Statistical significance was set at P<0.05.
Results
Characteristics of the patients
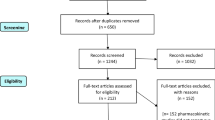
Between December 2003 and December 2012, a total of 160 patients were recruited in 10 centres in China. Ten cases were excluded: seven cases were actually underwent laparoscopic RT and three received radiotherapy after surgery because of positive upper endo-cervical margin or/and positive pelvic lymph nodes. Finally, 150 patients (77 VRT and 73 ART) were included for analyses in this study.
The average age of patients in the groups VRT and ART was 29.7 (range 18 to 38) and 31.0 (range 22 to 39) years, respectively. In all, 59 (76.4%) patients in the group VRT and 53 (72.6%) in the ART were nulliparous. The histological type, FIGO stage and tumour size listed in Table 1 were similar, and no statistical difference was observed between the two groups.
Comparison of surgical data
As shown in Table 2, the mean operating time of the two groups was similar, with a median of 204 min with VRT and 177 min with ART. There was a trend for higher blood loss during surgery with VRT (almost 110 ml more than ART), but the difference did not reach statistical significance. The number of patients who had complications was not significantly different between the two groups. In the VRT group, three patients had iliac vessel damage during laparoscopic lymphadenectomy, which needed a conversion to laparotomy to repair the vessels and a blood transfusion, one patient had postoperative active bleeding, which was managed by embolism of uterine artery, one had incomplete bowel obstruction and one had urinary retention. In the ART group, one patient had damage to pelvic vein requiring blood transfusion.
Comparison of pathological data
After RT, 80.7% (121/150) had pathological evidence of residual invasive cancer, with 75.3% in the VRT group and 86.3% in the ART group (P>0.05). Among all patients, 6.0% (9/150) had evidence of CIN (cervical intraepithelial carcinoma)/CIS (carcinoma in situ) and 13.3% (20/150) had no residual lesion. In 58 specimens of trachelectomy after conization, 32.8% (19/58) cases had no residual lesion. In specimens with measurable parametria, the average width of the paracervical tissue in the VRT group was 1.9 cm, compared with 2.8 cm in the ART group (P<0.01); median length of the excised cervix was 2.6 cm with VRT vs 3.6 cm with ART (P<0.01). The median number of lymph nodes obtained from both sides was 21 in the VRT group vs 26 in the ART group (P=0.310). Among patients in the VRT group, 9.1% presented specimens with high-risk factors, compared with 8.2% in the ART group. Comparisons of surgical and pathological data between the two groups are presented in Table 2.
Comparison of oncologic outcomes
Of 150 cases, 24 cases were just received RT, and no follow-up data were available. Totally 126 patients were followed-up for no <6 months. The mean follow-up duration was 34.4 months for VRT and 20.6 months for ART. Follow-up results are shown in Table 3. Among all 126 cases, seven patients developed recurrences and all occurred in the VRT group. The recurrence rate was 9.8% in the VRT group vs 0 in the ART group (P=0.018). For tumours no >2 cm, the recurrence rate was 4.2% with VRT and 0 with ART (P>0.05). However, in patients with tumour size >2 cm, the recurrence rate was 21.7% and 0% with VRT and ART, respectively (P=0.040). The recurrence sites were four in parametria, two in pelvic lymph nodes and one in vaginal fornix. Six of the seven recurrences occurred during the first 24 months of follow-up. Two (1.7%) patients died from the recurrence of their tumour after a follow-up of 27 and 46 months, respectively. Five of the seven recurrent tumours were well controlled using radiotherapy and are currently disease free.
Comparison of fertility outcomes
During follow-up, only 77 patients attempted to conceive. The others did not desire to conceive because of personal reasons, such as divorced, still unmarried or being afraid of sexual intercourse or recurrence. Twenty women had 24 pregnancies, as shown in Table 4, the pregnancy rate was 26.0%. Seventeen out of 20 pregnant women were in the VRT group and only three were in the ART group. The pregnancy rate in patients who attempted to conceive after VRT was 39.5%, which was significantly higher than the 8.8% observed in the ART group. Among those 24 pregnancies, there were five elective terminations of pregnancy in the first trimester, two first-trimester miscarriages, two second-trimester miscarriage and one ectopic pregnancy, who underwent laparoscopic surgery, and 13 women had 14 pregnancies delivered during the third trimester. Rate of delivered infants with live birth was 16.9%. Of those, four delivered before 37 weeks. Ten babies were delivered at full term (⩾37 weeks of gestational age). All deliveries were by Caesarean section.
Comparison between patients with different tumour sizes
In the present study, 48 patients had a tumour >2 cm, 24 in the VRT group and 24 in the ART group. Their median surgery time and blood loss during operation showed no difference compared with the smaller tumour size group (shown in Table 5). The frequency of residual invasive cancer after RT was significantly higher in patients with larger tumour (93.8% vs 76.7%). During almost the same follow-up interval, the patients with tumour size larger than 2 cm showed a higher recurrence rate (11.6% vs 2.4%, P=0.032) and lower pregnancy rate (12.5% vs 32.1%, P=0.094), compared with patients with tumour size no >2 cm.
Discussion
With the change of medical model from a biomedical to a bio-psycho-social one and with the development of value-based medicine, quality of life should be considered in making clinical decision especially for cancer treatment. In the recent two decades, with the widespread use of cervical cancer screening programs, there has been an increase in early-stage cervical cancers diagnosed in younger women who are still of childbearing age and who often request to preserve their fertility. Hence, RT has become one of the best options for young women with early cervical cancer.
VRT in combination with a laparoscopic pelvic lymphadenectomy, known as Dargent’s surgery, is the most common and accepted fertility-preserving procedure for young women with early cervical cancer. In literature, more than 800 cases of VRT have been reported as an oncologically safe procedure with a comparable recurrence rate compared with radical hysterectomies and an encouraging live birth rate (Han et al, 2011; Plante et al, 2011). But VRT demands that surgeons are skilled in laparoscopic lymphadenectomy and in vaginal radical surgery (Schauta’s procedure), which are not acquired by the majority of gynaecological oncologists. ART, however, is very similar to abdominal radical hysterectomy and does not need any special surgical training or instruments, making it a more accessible procedure that can technically be performed by any trained gynaecological oncologist in many countries (Hurst et al, 2010; Sato et al, 2011). The choice of ART may also be owing to other indications such as paediatric patients, bulky exophytic cervical cancer and abnormal vaginal anatomy (Abu-Rustum et al, 2005; Cibula et al, 2008). The objectives of fertility preserving treatment in patients with cervical cancer are not only the cancer control but also the childbearing. Hence, the end points of evaluation in radical trachelectomy should include oncologic and fertility outcomes together. However, so far, very few studies have compared the oncological and fertility outcome between the VRT and ART systemically (Einstein et al, 2009).
Our study is one of the largest comparative studies of vaginal vs abdominal radical trachelectomy focusing not only on the surgical data but also on the oncological and fertility outcomes. There was no difference in postoperative residual lesion, number of lymph nodes excised and incidence of complications between ART and VRT. However, we obtained larger specimens using ART in terms of both the parametrical width and cervical length of excised cervix. The difference was even more important in a previous study by Einstein et al (2009).
In the relatively limited studies on ART, the oncological outcome is usually good with overall recurrence rates comparable to VRT, which is <5% (Cibula et al, 2009; Nishio et al, 2009; Li et al, 2011). In our study, no recurrence occurred in the ART group, and all of the seven recurrent cases were from the VRT group. There was significant difference in recurrent rate between the ART and VRT groups (P=0.013). Although the lower recurrent rate in the group ART may partially because of its shorter follow-up duration (almost 14 months shorter than VRT), we can say the oncologic results of ART are at least no worse than VRT. However, there was no difference statistically in recurrent rate between the two groups (P=0.504) when the patients were stratified with the tumour size <2 cm. For tumour >2 cm, recurrence rate in the ART group was much lower than that in the VRT group (P=0.040). Thus, ART, in terms of oncological outcomes, is at least not worse than VRT for tumours <2 cm and better than VRT for tumours >2 cm. In four of seven recurrences, the recurrent sites after VRT were found to locate in the parametrical tissue. Hence, the benefit of ART for patients with larger tumours could possibly be due to wider parametrical removal during ART. But this benefit still needs to be confirmed by larger series of randomised clinical trials.
Our research revealed that ART had better oncology control compared with VRT, but it doesn’t mean that ART is a better method than VRT as a fertility preserving treatment in young women with early cervical cancer because fertility outcome is another important end point of evaluation for the treatment efficiencies. It has been reported that the pregnancy rate after VRT can be as high as 70% (Boss et al, 2005) in the women who do attempt to conceive and differs from 30 to 48% in all women after VRT (Plante, 2008); 62% of these pregnancies will reach the third trimester (Hertel et al, 2006; Shepherd et al, 2006). Whereas the obstetric results after ART are proved not encouraging with pregnancy rate no more than 20% (Li et al, 2011; Rob et al, 2011). In our study, the pregnancy rate was 26% and the live birth rate was 16.9% in all women who attempted to conceive after operation. The relative lower pregnancy rate in our study may due to several reasons including psychosocial factors such as sexual dysfunction due to depression and stress, lack of concerning and consultation on fertility during follow-up and inadequate-assisted reproductive techniques. In the VRT group, the rates of pregnancy and live birth were relatively higher than those of ART. The factors that can further affect fertility after ART are higher risk of adhesions after abdominal approach, greater disruption of pelvic nerve innervations to the uterus, abnormality of fallopian tubes by larger resection of the paracervix tissue and shorter follow-up duration. The patients with tumour size <2 cm showed lower pregnant rate compared with the patients with smaller tumours. In terms of fertility outcome, our research revealed that patients with tumour size <2 cm treated by VRT may obtain better fertility results.
The tumour size <2 cm is originally an indication for Dargent’s surgery, but in 2010 NCCN guideline it stated that radical trachelectomy can be performed in patients with tumour size <4 cm. The treatment of radical trachelectomy for patients with tumour size >2 cm stage IB1 cervical cancer has been controversial because the oncological results are still doubted. In our study, the patients with tumour size >2 cm showed significant higher recurrence rate than those with smaller tumours (11.6% vs 2.4%, P <0.05). Even in ART, a recent review showed similar results: 1.9% recurrences in tumours <2 cm vs 20% in those >2 cm (Rob et al, 2011). Our research demonstrated clearly that tumour size <2 cm should be still considered as an indication for radical trachelectomy.
In summary, using standardised techniques, VRT and ART provide similar surgical and pathological outcomes except larger specimens obtained by ART with wider and longer cervix removed. Patients treated by ART achieved better oncological results, but their fertility outcomes were unfavourable. Tumour size <2 cm should be emphasised as a strict indication for RT in order to optimise fertility and prognosis outcomes.
Change history
26 November 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abu-Rustum NR, Su W, Levine DA, Boyd J, Sonoda Y, Laquaglia MP (2005) Pediatric radical abdominal trachelectomy for cervical clear cell carcinoma: a novel surgical approach. Gynecol Oncol 97: 296–300.
Boss EA, van Golde RJ, Beerendonk CC, Massuger LF (2005) Pregnancy after radical trachelectomy: a real option? Gynecol Oncol 99: S152–S156.
Cibula D, Slama J, Fischerova D (2008) Update on abdominal radical trachelectomy. Gynecol Oncol 111: S111–S115.
Cibula D, Sláma J, Svárovský J, Fischerova D, Freitag P, Zikán M, Pinkavová I, Pavlista D, Dundr P, Hill M (2009) Abdominal radical trachelectomy in fertility-sparing treatment of early-stage cervical cancer. Int J Gynecol Cancer 19: 1407–1411.
Einstein MH, Park KJ, Sonoda Y, Carter J, Chi DS, Barakat RR, Abu-Rustum NR (2009) Radical vaginal versus abdominal trachelectomy for stage IB1 cervical cancer: a comparison of surgical and pathologic outcomes. Gynecol Oncol 112: 73–77.
Han L, Yang XY, Zheng A, Wang L, Chu YX, Wang Y (2011) Systematic comparison of radical vaginal trachelectomy and radical hysterectomy in the treatment of early-stage cervical cancer. Int J Gynaecol Obstet 112: 149–153.
Hertel H, Köhler C, Grund D, Hillemanns P, Possover M, Michels W, Schneider A German Association of Gynecologic Oncologists (AGO) (2006) Radical vaginal trachelectomy (RVT) combined with laparoscopic pelvic lymphadenectomy: prospective multicenter study of 100 patients with early cervical cancer. Gynecol Oncol 103: 506–511.
Hurst SA, Del Priore G, Ungar L, Smith JR (2010) Experiences in abdominal radical trachelectomy. Am J Obstet Gynecol 202: e8–e9.
Li J, Li Z, Wang H, Zang R, Zhou Y, Ju X, Ke G, Wu X (2011) Radical abdominal trachelectomy for cervical malignancies: surgical, oncological and fertility outcomes in 62 patients. Gynecol Oncol 121: 565–570.
Lintner B, Saso S, Tarnai L, Novak Z, Palfalvi L, Del Priore G, Smith JR, Ungar L (2013) Use of abdominal radical trachelectomy to treat cervical cancer greater than 2 cm in diameter. Int J Gynecol Cancer 23: 1065–1070.
Nishio H, Fujii T, Kameyama K, Susumu N, Nakamura M, Iwata T, Aoki D (2009) Abdominal radical trachelectomy as a fertility-sparing procedure in women with early-stage cervical cancer in a series of 61 women. Gynecol Oncol 115: 51–55.
Plante M (2008) Vaginal radical trachelectomy: an update. Gynecol Oncol 111: S105–S110.
Plante M, Gregoire J, Renaud MC, Roy M (2011) The vaginal radical trachelectomy: an update of a series of 125 cases and 106 pregnancies. Gynecol Oncol 121: 290–297.
Rob L, Skapa P, Robova H (2011) Fertility-sparing surgery in patients with cervical cancer. Lancet Oncol 12: 192–200.
Saso S, Ghaem-Maghami S, Chatterjee J, Naji O, Farthing A, Mason P, McIndoe A, Hird V, Ungar L (2012) Abdominal radical trachelectomy in West London. Int J Gynecol Cancer 119: 187–193.
Sato S, Aoki D, Kobayashi H, Saito T, Nishimura R, Nagano T, Yaegashi N, Enomoto T, Kigawa J (2011) Questionnaire survey of the current status of radical trachelectomy in Japan. Int J Clin Oncol 16: 141–144.
Shen K, Lang JH, Yang JX, Chen YL, Xiang Y, Hua KQ, Huang HF, Pan LY, Wu M, Feng YJ (2006) Analysis of 16 patients with early cervical cancer treated by laparoscopic vaginal radical trachelectomy. Zhonghua Fu Chan Ke Za Zhi 41: 222–225.
Shepherd JH, Spencer C, Herod J, Ind TE (2006) Radical vaginal trachelectomy as a fertility-sparing procedure in women with early-stage cervical cancer-cumulative pregnancy rate in a series of 123 women. BJOG 113: 719–724.
Acknowledgements
This study was supported by the National Science and Technology Infrastructure Program ‘The National Key Technologies R&D Program of China’ (Grant 2008BAI57B02).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Cao, D., Yang, J., Wu, X. et al. Comparisons of vaginal and abdominal radical trachelectomy for early-stage cervical cancer: preliminary results of a multi-center research in China. Br J Cancer 109, 2778–2782 (2013). https://doi.org/10.1038/bjc.2013.656
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.656
Keywords
This article is cited by
-
A meta-analysis of treatment for early-stage cervical cancer: open versus minimally invasive radical trachelectomy
BMC Pregnancy and Childbirth (2023)
-
Cervical cancer prognosis and related risk factors for patients with cervical cancer: a long-term retrospective cohort study
Scientific Reports (2022)
-
Minimally invasive versus open radical trachelectomy for early-stage cervical cancer: protocol for a multicenter randomized controlled trial in China
Trials (2020)
-
Reproductive outcomes following treatment for a gynecological cancer diagnosis: a systematic review
Journal of Cancer Survivorship (2019)
-
Short- and long term outcomes after abdominal radical trachelectomy versus radical hysterectomy for early stage cervical cancer: a systematic review of the literature and meta-analysis
Archives of Gynecology and Obstetrics (2019)