Abstract
Background:
Diagnostic surgical breast biopsies have several disadvantages, therefore, they should be used with hesitation. We determined time trends in types of breast biopsies for the workup of abnormalities detected at screening mammography. We also examined diagnostic delays.
Methods:
In a Dutch breast cancer screening region 6230 women were referred for an abnormal screening mammogram between 1 January 1997 and 1 January 2011. During two year follow-up clinical data, breast imaging-, biopsy-, surgery- and pathology-reports were collected of these women. Furthermore, breast cancers diagnosed >3 months after referral (delays) were examined, this included review of mammograms and pathology specimens to determine the cause of the delays.
Results:
In 41.1% (1997–1998) and in 44.8% (2009–2010) of referred women imaging was sufficient for making the diagnosis (P<0.0001). Fine-needle aspiration cytology decreased from 12.7% (1997–1998) to 4.7% (2009–2010) (P<0.0001), percutaneous core-needle biopsies (CBs) increased from 8.0 to 49.1% (P<0.0001) and surgical biopsies decreased from 37.8 to 1.4% (P<0.0001). Delays in breast cancer diagnosis decreased from 6.7 to 1.8% (P=0.003).
Conclusion:
The use of diagnostic surgical breast biopsies has decreased substantially. They have mostly been replaced by percutaneous CBs and this replacement did not result in an increase of diagnostic delays.
Similar content being viewed by others
Main
Breast cancer is worldwide the most frequently diagnosed cancer, and the leading cause of cancer death among females (Jemal et al, 2011). Also in the Netherlands, breast cancer is an important threat for public health. Breast cancer incidence in the Netherlands is among the highest in the world with the age-standardised rate being 128 out of 100 000 person years (European Standardised Rate) and the incidence is still increasing (IKCnet, 2012). Breast cancer survival has, fortunately, improved over the last decades (Louwman et al, 2008; Autier et al, 2010; Youlden et al, 2012), and this improved survival is probably due to the introduction of mammography screening and improvements in breast cancer treatment (Louwman et al, 2007; Autier et al, 2010). In the Netherlands, women aged 50–75 years are invited every 2 years to undergo mammography screening and in case of a mammographic abnormality, women are referred to a hospital for further diagnostic workup. This workup may consist of additional imaging and biopsy. There are various breast biopsy procedures, including percutaneous fine-needle aspiration cytology (FNAC), percutaneous core-needle biopsy (CB) (ultrasound-guided or stereotactic vacuum-assisted) and invasive surgical biopsy. Surgical biopsies for diagnostic purposes should be omitted, as they increase unnecessary psychological distress in false-positive referrals (Brett and Austoker, 2001; Bond et al, 2012) and benign breast surgery complicates interpretation of subsequent mammograms due to postoperative changes (Brenner and Pfaff, 1996; Banks et al, 2004; Taplin et al, 2010; van Breest Smallenburg et al, 2012a). Surgical biopsy should also not be used for histological confirmation of a radiologically suspicious or malignant lesion. Confirmation of breast cancer by percutaneous biopsy allows a better preoperative planning (White et al, 2001; James et al, 2012) and it is associated with a lower likelihood of multiple breast surgeries (Duijm et al, 2009; Friese et al, 2009). In the current population-based study, we determined time trends in types of breast biopsies for abnormalities detected at screening mammography. We also determined the proportion of referred women who experienced a delay in breast cancer diagnosis and examined the causes of these delays.
Materials and Methods
Study population
We included all women who were referred after screening mammography at one of two specialised screening units (one fixed unit and one mobile unit) in a breast cancer screening region in the south of the Netherlands between 1 January 1997 and 1 January 2011. Women participating in the Dutch screening programme are asked to give written informed consent regarding the use of their screening and follow-up data for evaluation purposes. All women, except for three, approved. The three women who did not approve were not included in our study population. According to the Dutch Central Committee on Research involving Human subjects, institutional review board approval was not required for our type of study.
Screening procedure and diagnostic workup
Details of the nation-wide breast cancer screening programme have been described previously (Fracheboud et al, 1998; Duijm et al, 2004). The Dutch nation-wide breast cancer screening programme offers biennial screening mammography to women aged 50–75 years. Digitisation of the breast cancer screening programme has recently been completed and in our breast screening region, transformation from analogue to digital screening took place in May 2009. All mammograms in this study were obtained by specialised screening mammography radiographers, and the examinations were independently double read by a group consisting of 12 certified screening radiologists. Each of the screening radiologists evaluates at least 5000 screening mammograms yearly. From 2003, in addition to radiologist double reading, the radiographers also actively participated in the assessment of the screening mammograms (Duijm et al, 2007a). Prior screening mammograms were always available for comparison in case of subsequent screening. In case of suspicious or malignant findings at screening mammography, the woman was referred by her general practitioner to a surgical oncologist at a regional hospital. A total of 16 hospitals were involved in the diagnostic workup of the referred women. The women underwent a physical examination by an oncologist, which was followed by mammographic workup of all suspect areas. The radiologist classified the radiological findings according to the American College of Radiology BI-RADS (D’Orsi et al, 2003) and decided whether additional procedures such as breast ultrasonography, MRI and/or biopsy were indicated. The choice of additional procedures depended on the diagnostic workup protocols and the facilities available at the specific hospital involved in the workup. The radiologists’ decision furthermore depended on national guidelines. In 2000, the first Dutch national guideline for breast cancer screening was published. This guideline required a target for preoperative diagnoses in women with suspected breast cancer of at least 70%. The guideline also suggested that one should use a percutaneous method, either FNAC or CB, for making the preoperative diagnosis (Rutgers and Tuut, 2001). In 2008, a new guideline increased the target for preoperative diagnoses to 90% (NABON, 2008). Biopsy of non-palpable lesions in our study population was always performed by radiologists, whereas sampling of palpable lesions was done either by surgeons or radiologists. During the 14-year period of our study, various breast biopsy procedures were used for the diagnostic workup, including FNAC, CB (ultrasound-guided or stereotactic vacuum-assisted) and open surgical biopsy. Between 1999 and 2007, out-patient breast clinics became available at the hospitals involved in this study and between 2002 and 2007 multidisciplinary teams were implemented for the routine evaluation of the clinical, radiological and biopsy results of all referred women.
Follow-up procedure
For each referred woman, we collected data on radiology, pathology and surgical procedures at the hospitals where the mammographic screening abnormalities were evaluated. The follow-up period for all screened women included the time through the next screening round (the screening interval was ∼2 years).
Delay in breast cancer diagnosis
A definite diagnosis of breast cancer >3 months after referral was considered as a diagnostic delay (Richards et al, 1999). To determine whether a diagnostic delay could be attributed to an erroneous radiologic assessment, two breast radiologists (LD, FJ) independently reviewed the clinical breast images of all women with a diagnostic delay. Each reviewer classified the lesions according to BI-RADS and discrepant assessments were resolved by consensus reading. To determine whether a delay in cancer diagnosis could be attributed to a false-negative histopathological result, a pathologist reviewed the biopsy specimen of women with a delay in breast cancer diagnosis who had had a prior breast biopsy with benign outcome. False-negative results due to erroneous pathologic assessments and due to sampling errors were both regarded as false-negative biopsy results. At review, both the radiologists and the pathologist knew that they reassessed cases with a delay in cancer diagnosis.
Statistical analysis
Statistical analyses was performed per 2-year screening periods. The primary outcome measures were the time trends of imaging only, FNAC, percutaneous CBs, surgical biopsies at workup and the percentage of women who experienced a delay in breast cancer diagnosis. All data were entered into a computerised spreadsheet (Excel; Microsoft, Redmond, WA, USA). Statistics were performed using the SAS programme version 9.1.3 (Statistical Analysis Software; SAS/STAT Software, Cary, NC, USA). A χ2-test was used to test the differences between categorical variables. Mean age according to hopital was tested using the ANOVA model. A regression analysis was performed to calculate odds ratios and their confidence intervals for determination of time trends in various breast biopsy types, adjusting for age and hospital.The significance level was set at 5%.
Results
Overall screening results
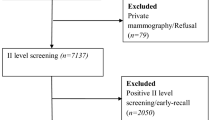
From 1 January 1 1997 to 1 January 2011 a total of 417 013 screening examinations had been performed (Figure 1). Altogether, 6230 women were referred for further diagnostic workup of a mammographic abnormality (referral rate, 1.5%). Breast cancer was diagnosed in 2214 referred women, yielding a cancer detection rate of 5.3 per 1000 screening examinations and a true-positive referral rate of 35.5%. Nine women had either not been referred by their general practitioner or their follow-up was unknown, and 4007 (64.4%) women had a benign outcome (i.e., false-positive referrals).
Diagnostic workup after referral
In 2486 (40.0%) of the 6230 referred women, evaluation of the abnormality detected at screening mammography consisted of imaging only (additional mammographic views, breast ultrasonography and/or MRI). In the remaining 3731 (60.0%) women, imaging was not sufficient for the establishment of a final diagnosis. Many women underwent a combination of biopsy types because of inconclusive results from FNAC and/or percutaneous CB (Table 1). A final diagnosis was obtained by FNAC in 704 (11.3%) referred women, by CB in 2399 (38.6%) women and by surgical biopsy in 628 (10.1%) women (Table 1). The use of FNAC sharply decreased in the final years of the study period; in 1997–1998 12.7% (68 out of 535) of the diagnoses was made by FNAC, compared with 4.7% (84 out of 1777) in 2009–2010 (P<0.0001) (Figure 2). The percentage of women with a diagnosis obtained by CB increased from 8.0% (202 out of 535) in 1997–1998 to 49.1% (24 out of 1777) in 2009–2010 (P<0.0001). Simultaneously, the percentage with a diagnosis made by surgical biopsy decreased from 37.8% (70 out of 535) in 1997–1998 to 1.4% (20 out of 1777) in 2009–2010 (P<0.0001) (Table 1, Figure 2). Also after adjustment for age and hospital, FNAC significantly decreased, diagnoses made by percutaneous CBs significantly increased and surgical biopsies significantly decreased (Table 2). The mean age of referred women was 60 and this was comparable between the 16 hospitals (P=0.3). Main reasons for performing a surgical biopsy in women referred in 2009–2010 were possible (pre)cancerous lesions or inconclusive results at FNAC or CB (19 out of 24, 79.2%).
Diagnostic delays
In 96 of the 2214 women with breast cancer (4.3%), the diagnosis was made >3 months after referral. This delay in breast cancer diagnosis was 4–6 months in 26 (27.1%) women, 7–12 months in 36 women (37.5%), 13–24 months in 21 women (21.9%) and >24 months (24–28 months) in 13 women (13.8%). Most women presented with a delay within 12 months because a follow-up had been recommended at the assessment after referral from screening. The causes of the delays, the tumour stage distribution and axillary lymph node status are presented in Table 3. A total of 27 women with a delay (28.1%) had an advanced tumour stage at the time of diagnosis (advanced cancers were defined as invasive cancers with a tumour size >20 mm (T2) and/or the presence of metastasis in axillary lymph nodes). The total amount of women with a diagnostic delay decreased, from 6.7% (15 out of 224) in 1997–1998 to 1.8% (8 out of 344) in 2009–2010 (P=0.003). The majority of the diagnostic delays resulted from an erroneous BI-RADS assessment (57.3%, 55 out of 96) or false-negative biopsy result (32.3%, 31 out of 96). Ten delays resulted from other reasons, including errors made by surgeons and patient-related delays. The majority of the delays (68.8%) that resulted from false-negative biopsies consisted of CB. Details of the biopsy procedures are also presented in Table 3. The pathologist reported that all false-negative biopsy results were due to sampling errors and not the result of erroneous pathologic assessments.
Discussion
Surgical biopsies for diagnostic purposes have several disadvantages. We have reported in earlier studies that benign breast surgery, including surgical biopsy, can result in a lower sensitivity for breast cancer detection at subsequent screening mammography (van Breest Smallenburg et al, 2012a; b). Furthermore, invasive assessments increase the unnecessary psychological distress of false-positive referrals (Brett and Austoker, 2001; Bond et al, 2012). In malignant cases, it is also desirable to avoid diagnostic surgical biopsies as a preoperative confirmation of breast cancer gives the patient and surgeon the possibility to discuss treatment options. A preoperative diagnosis also allows a better surgery planning (White et al, 2001; James et al, 2012) and it is associated with a lower likelihood of multiple breast surgeries (Duijm et al, 2009; Friese et al, 2009). During the 14-year period of our study, the use of FNAC fluctuated and then decreased in the most recent years. Fine-needle aspiration cytology is important for the assessment of cystic lesions and is, therefore, still useful in the workup of breast abnormalities (NABON, 2008). However, for solid lesions, FNAC has a higher insufficient sample rate and a lower diagnostic accuracy than other biopsy methods. Additional CB is frequently required following inconclusive FNAC results (Pisano et al, 2001; Duijm et al, 2007b; Willems et al, 2012), thus extending the period of anxiety and uncertainty before the final diagnosis has been made. For these reasons, FNAC should not be considered the diagnostic procedure of first choice for solid breast lesions. We attribute the strong decrease of FNAC in 2009 and 2010 to the implementation of digital screening in 2009. Digital screening especially increased the referral rate of women with suspicious microcalcifications (Nederend et al, 2012), which in turn resulted in an increase in the use of stereotactic-guided percutaneous vacuum-assisted CBs. The diagnostic workup of suspicious breast lesions by percutaneous CBs showed a substantial increase during the 14-year period of our study, whereas surgical biopsies became rare. Percutaneous CBs are equally accurate to surgical biopsies and have several advantages over surgical biopsy, including lower costs, a more rapid way of providing a diagnosis and lower complication rates (Verkooijen, 2002; Fajardo et al, 2004; Golub et al, 2004; Bruening et al, 2010). As a result, percutaneous CB is currently a widely used technique for evaluating breast abnormalities and CB has worldwide been accepted as a reliable alternative to surgical biopsy (Meyer et al, 1999; Brenner et al, 2001; Crowe et al, 2002). Despite the high diagnostic accuracy of CBs, equivocal biopsy results or discordance between radiological and histological findings is present in ∼10% of core-needle biopsy procedures, necessitating repeated biopsy (Youk et al, 2007). Obviously, it is desirable to obtain a diagnosis in one biopsy session. More than one tissue sample should be taken and it is also advisable to assess the characteristics of these samples at biopsy. If the core sample is stiff, predominantly white, and sinks as soon as it is put in formalin, it is likely a diagnostic biopsy (Youk et al, 2007). Only in a limited number of cases surgical biopsies still have an additional value. A surgical biopsy is, for example, justified in case of a non-representative CB and in cases showing high-risk lesions or premalignant findings at CB (Shin and Rosen, 2002; Sydnor et al, 2007; NABON, 2008). Furthermore, a surgical biopsy can be the biopsy-method of choice when patient characteristics (for example, extreme obesity or dementia) impede percutaneous biopsy. The replacement of surgical biopsies by percutaneous CBs was probably mainly the result of the introduction and revision of Dutch breast cancer guidelines. As mentioned before, the 2000 guideline required a target for a preoperative diagnosis in women with suspected breast cancer of at least 70% by using either FNAC or CB (Rutgers and Tuut, 2001), and the 2008 guideline increased this target to 90% (NABON, 2008).
Besides the trends in biopsies, we also determined the frequency and causes of diagnostic delays in referred women, because the replacement of surgical biopsies by CBs may hypothetically have resulted in more false-negative biopsies and a higher proportion of women that experienced a delay in breast cancer diagnosis. The amount of delays in breast cancer diagnosis in our study population, however, decreased from 6.7 to 1.8% (P=0.003). The introduction of breast-care units and multidisciplinary teams in the Dutch hospitals probably mainly explains this decline in delays. Also the introduction of breast cancer guidelines and the growing importance of quality indicators in Dutch breast cancer care have probably contributed to the decline in delays. The importance of multidisciplinary teams to improve the assessment of breast lesions has been described in several studies and the use of these teams is also recommended by breast cancer guidelines (Rabinowitz, 2004; Pruthi et al, 2007; NABON, 2008). The majority of diagnostic delays in our study resulted from erroneous BI-RADS assessments (57.3%) and false-negative biopsy results (32.3%). Diagnostic delays due to erroneous mammographic assessments are not uncommon, lesions can be missed, misinterpreted or overlooked (Ganry et al, 2004; Ciatto et al, 2007; Giess et al, 2012). Also false-negative biopsy results are known as probable causes of diagnostic delays (Youk et al, 2007). The majority of false-negative biopsy results in our study consisted of CBs (68.8%), all were due to sampling errors. Researchers describe that ∼4% of CB results, both ultrasound- and stereotactic guided, are false negative (NABON, 2008). Therefore, attention for radiologic–histologic correlation is very important (Berg et al, 1996; Parikh and Tickman, 2005; Youk et al, 2007) and sometimes a repeated biopsy is needed. False-negative results and delays in diagnosis from both erroneous BI-RADS assessments and false-negative biopsies can be reduced with optimisation of multidisciplinary approach and clear post-biopsy protocols. An additional time trend finding of our study was the increase of false-positive referrals from 57.9 to 75.5%. The most important explanation for this finding is probably the transition from screen-film mammography to full-field digital mammography screening in 2009, which resulted in increased referral rates, with a concomitant increase in both cancer detection rate and false-positive referral (Nederend et al, 2012).
There are certain strengths and limitations of our study. First, both the radiologists and the pathologist knew that they reassessed cases with a delay in cancer diagnosis. The pathologist did not find any erroneous pathologic assessments, however, radiologist review bias may have resulted in a higher amount of cases judged as ‘missed cancers’ due to erroneous BI-RADS assessments. Second, extrapolation of our results to other screening programmes may be limited by the fact that the design of the Dutch breast cancer screening programme and workup strategies differ from other countries. The Dutch referral rate of 1.5–2.5% is much lower than the 3–6% referral rates observed in other European countries and the referral rate of 10% or more in the United States (Perry et al, 2008; Dowling et al, 2010). Furthermore, the incidence of open surgical biopsy is much higher in the United States than in the United Kingdom and the Netherlands. Recent data suggest that in the United States, 30–40% of diagnostic breast biopsies still consist of surgical biopsies (Clarke-Pearson et al, 2009; Gutwein et al, 2011).
A strength of our study is that with the information on biopsy time trends we are able to verify whether national guidelines are followed at our screening region. Furthermore, women who attend the screening programme can now be optimally informed on the steps that will be taken following referral.
We conclude that women in a southern screening region of the Netherlands are nowadays rarely confronted with a diagnostic surgical biopsy for the workup of a screening mammography abnormality. Diagnostic surgical biopsies have mostly been replaced by percutaneous CBs. The replacement of surgical biopsies by percutaneous CBs did not increase the amount of delays in breast cancer diagnosis.
Change history
09 July 2013
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Autier P, Boniol M, La Vecchia C, Vatten L, Gavin A, Hery C, Heanue M (2010) Disparities in breast cancer mortality trends between 30 European countries: retrospective trend analysis of WHO mortality database. BMJ 341: c3620.
Banks E, Reeves G, Beral V, Bull D, Crossley B, Simmonds M, Hilton E, Bailey S, Barrett N, Briers P, English R, Jackson A, Kutt E, Lavelle J, Rockall L, Wallis MG, Wilson M, Patnick J (2004) Influence of personal characteristics of individual women on sensitivity and specificity of mammography in the Million Women Study: cohort study. BMJ 329 (7464): 477.
Berg WA, Hruban RH, Kumar D, Singh HR, Brem RF, Gatewood OM (1996) Lessons from mammographic-histopathologic correlation of large-core needle breast biopsy. Radiographics 16 (5): 1111–1130.
Bond M, Pavey T, Welch K, Cooper C, Garside R, Dean S, Hyde CJ (2012) Psychological consequences of false-positive screening mammograms in the UK. Evid Based Med 18 (2): 54–61.
Brenner RJ, Bassett LW, Fajardo LL, Dershaw DD, Evans WP 3rd, Hunt R, Lee C, Tocino I, Fisher P, McCombs M, Jackson VP, Feig SA, Mendelson EB, Margolin FR, Bird R, Sayre J (2001) Stereotactic core-needle breast biopsy: a multi-institutional prospective trial. Radiology 218 (3): 866–872.
Brenner RJ, Pfaff JM (1996) Mammographic changes after excisional breast biopsy for benign disease. AJR Am. J. Roentgenol 167 (4): 1047–1052.
Brett J, Austoker J (2001) Women who are recalled for further investigation for breast screening: psychological consequences 3 years after recall and factors affecting re-attendance. J Public Health Med 23 (4): 292–300.
Bruening W, Fontanarosa J, Tipton K, Treadwell JR, Launders J, Schoelles K (2010) Systematic review: comparative effectiveness of core-needle and open surgical biopsy to diagnose breast lesions. Ann Intern Med 152 (4): 238–246.
Ciatto S, Houssami N, Ambrogetti D, Bonardi R, Collini G, Del Turco MR (2007) Minority report-false negative breast assessment in women recalled for suspicious screening mammography: imaging and pathological features, and associated delay in diagnosis. Breast Cancer Res Treat 105 (1): 37–43.
Clarke-Pearson EM, Jacobson AF, Boolbol SK, Leitman IM, Friedmann P, Lavarias V, Feldman SM (2009) Quality assurance initiative at one institution for minimally invasive breast biopsy as the initial diagnostic technique. J Am Coll Surg 208 (1): 75–78.
Crowe JP Jr, Rim A, Patrick R, Rybicki L, Grundfest S, Kim J, Lee K, Levy L (2002) A prospective review of the decline of excisional breast biopsy. Am J Surg 184 (4): 353–355.
Dowling EC, Klabunde C, Patnick J, Ballard-Barbash R (2010) Breast and cervical cancer screening programme implementation in 16 countries. J Med Screen 17 (3): 139–146.
Duijm LE, Groenewoud JH, de Koning HJ, Coebergh JW, van Beek M, Hooijen MJ, van de Poll-Franse LV (2009) Delayed diagnosis of breast cancer in women recalled for suspicious screening mammography. Eur J Cancer 45 (5): 774–781.
Duijm LE, Groenewoud JH, Fracheboud J, de Koning HJ (2007a) Additional double reading of screening mammograms by radiologic technologists: impact on screening performance parameters. J Natl Cancer Inst 99 (15): 1162–1170.
Duijm LE, Groenewoud JH, Hendriks JH, de Koning HJ (2004) Independent double reading of screening mammograms in The Netherlands: effect of arbitration following reader disagreements. Radiology 231 (2): 564–570.
Duijm LE, Groenewoud JH, Roumen RM, de Koning HJ, Plaisier ML, Fracheboud J (2007b) A decade of breast cancer screening in The Netherlands: trends in the preoperative diagnosis of breast cancer. Breast Cancer Res Treat 106 (1): 113–119.
D’Orsi CJ, Mendelson EB, Ikeda DM et al (2003) Breast Imaging Reporting and Data System: ACR BI-RADS-Breast Imaging Atlas. American College of Radiology: Reston, VA, USA.
Fajardo LL, Pisano ED, Caudry DJ, Gatsonis CA, Berg WA, Connolly J, Schnitt S, Page DL, McNeil BJ (2004) Stereotactic and sonographic large-core biopsy of nonpalpable breast lesions: results of the Radiologic Diagnostic Oncology Group V study. Acad Radiol 11 (3): 293–308.
Fracheboud J, de Koning HJ, Beemsterboer PM, Boer R, Hendriks JH, Verbeek AL, van Ineveld BM, de Bruyn AE, van der Maas PJ (1998) Nation-wide breast cancer screening in The Netherlands: results of initial and subsequent screening 1990-1995. National Evaluation Team for Breast Cancer Screening. Int J Cancer 75 (5): 694–698.
Friese CR, Neville BA, Edge SB, Hassett MJ, Earle CC (2009) Breast biopsy patterns and outcomes in Surveillance, Epidemiology, and End Results-Medicare data. Cancer 115 (4): 716–724.
Ganry O, Peng J, Dubreuil A (2004) Influence of abnormal screens on delays and prognostic indicators of screen-detected breast carcinoma. J Med Screening 11 (1): 28–31.
Giess CS, Frost EP, Birdwell RL (2012) Difficulties and errors in diagnosis of breast neoplasms. Seminars in ultrasound, CT, and MR 33 (4): 288–299.
Golub RM, Bennett CL, Stinson T, Venta L, Morrow M (2004) Cost minimization study of image-guided core biopsy versus surgical excisional biopsy for women with abnormal mammograms. J Clin Oncol 22 (12): 2430–2437.
Gutwein LG, Ang DN, Liu H, Marshall JK, Hochwald SN, Copeland EM, Grobmyer SR (2011) Utilization of minimally invasive breast biopsy for the evaluation of suspicious breast lesions. Am J Surgery 202 (2): 127–132.
IKCnet. http://www.ikcnet.nl (accessed July 2012).
James TA, Mace JL, Virnig BA, Geller BM (2012) Preoperative needle biopsy improves the quality of breast cancer surgery. J Am Coll Surg 215 (4): 562–568.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA: A Cancer Journal for Clinicians 61 (2): 69–90.
Louwman WJ, van de Poll-Franse LV, Fracheboud J, Roukema JA, Coebergh JW (2007) Impact of a programme of mass mammography screening for breast cancer on socio-economic variation in survival: a population-based study. Breast Cancer Res Treat 105 (3): 369–375.
Louwman WJ, Voogd AC, van Dijck JA, Nieuwenhuijzen GA, Ribot J, Pruijt JF, Coebergh JW (2008) On the rising trends of incidence and prognosis for breast cancer patients diagnosed 1975-2004: a long-term population-based study in southeastern Netherlands. Cancer Causes Control 19 (1): 97–106.
Meyer JE, Smith DN, Lester SC, Kaelin C, DiPiro PJ, Denison CM, Christian RL, Harvey SC, Selland DL, Durfee SM (1999) Large-core needle biopsy of nonpalpable breast lesions. JAMA 281 (17): 1638–1641.
NABON (2008) Consensus based Dutch Breast Cancer Guidelines. NABON: Amsterdam (in Dutch).
Nederend J, Duijm LE, Louwman MW, Groenewoud JH, Donkers-van Rossum AB, Voogd AC (2012) Impact of transition from analog screening mammography to digital screening mammography on screening outcome in The Netherlands: a population-based study. Ann Oncol 23 (12): 3098–3103.
Parikh J, Tickman R (2005) Image-guided tissue sampling: where radiology meets pathology. Breast J 11 (6): 403–409.
Perry N, Broeders M, de Wolf C, Tornberg S, Holland R, von Karsa L (2008) European guidelines for quality assurance in breast cancer screening and diagnosis. Fourth edition--summary document. Ann Oncol 19 (4): 614–622.
Pisano ED, Fajardo LL, Caudry DJ, Sneige N, Frable WJ, Berg WA, Tocino I, Schnitt SJ, Connolly JL, Gatsonis CA, McNeil BJ (2001) Fine-needle aspiration biopsy of nonpalpable breast lesions in a multicenter clinical trial: results from the radiologic diagnostic oncology group V. Radiology 219 (3): 785–792.
Pruthi S, Brandt KR, Degnim AC, Goetz MP, Perez EA, Reynolds CA, Schomberg PJ, Dy GK, Ingle JN (2007) A multidisciplinary approach to the management of breast cancer, part 1: prevention and diagnosis. Mayo Clinic Proceedings 82 (8): 999–1012.
Rabinowitz B (2004) Interdisciplinary breast cancer care: declaring and improving the standard. Oncology (Williston Park) 18 (10): 1263–1268, (discussion 1268–70, 1275).
Richards MA, Westcombe AM, Love SB, Littlejohns P, Ramirez AJ (1999) Influence of delay on survival in patients with breast cancer: a systematic review. Lancet 353 (9159): 1119–1126.
Rutgers EJ, Tuut MK (2001) [CBO guideline 'Breast cancer: screening and diagnosis']. Nederlands tijdschrift voor geneeskunde 145 (3): 115–119, (in Dutch).
Shin SJ, Rosen PP (2002) Excisional biopsy should be performed if lobular carcinoma in situ is seen on needle core biopsy. Arch Pathol Lab Med 126 (6): 697–701.
Sydnor MK, Wilson JD, Hijaz TA, Massey HD, Shaw de Paredes ES (2007) Underestimation of the presence of breast carcinoma in papillary lesions initially diagnosed at core-needle biopsy. Radiology 242 (1): 58–62.
Taplin SH, Abraham L, Geller BM, Yankaskas BC, Buist DS, Smith-Bindman R, Lehman C, Weaver D, Carney PA, Barlow WE (2010) Effect of previous benign breast biopsy on the interpretive performance of subsequent screening mammography. J Natl Cancer Inst 102 (14): 1040–1051.
van Breest Smallenburg V, Duijm LE, Voogd AC, Groenewoud JH, Jansen FH, van Beek M, Louwman MW (2012a) Lower sensitivity of screening mammography after previous benign breast surgery. Int J Cancer 130 (1): 122–128.
van Breest Smallenburg V, Duijm LE, Voogd AC, Jansen FH, Louwman MW (2012b) Mammographic changes resulting from benign breast surgery impair breast cancer detection at screening mammography. Eur J Cancer 48 (14): 2097–2103.
Verkooijen HM (2002) Diagnostic accuracy of stereotactic large-core needle biopsy for nonpalpable breast disease: results of a multicenter prospective study with 95% surgical confirmation. Int J Cancer 99 (6): 853–859.
White RR, Halperin TJ, Olson JA Jr., Soo MS, Bentley RC, Seigler HF (2001) Impact of core-needle breast biopsy on the surgical management of mammographic abnormalities. Ann Surg 233 (6): 769–777.
Willems SM, van Deurzen CH, van Diest PJ (2012) Diagnosis of breast lesions: fine-needle aspiration cytology or core needle biopsy? A review. J Clin Pathol 65 (4): 287–292.
Youk JH, Kim EK, Kim MJ, Lee JY, Oh KK (2007) Missed breast cancers at US-guided core needle biopsy: how to reduce them. Radiographics 27 (1): 79–94.
Youlden DR, Cramb SM, Dunn NA, Muller JM, Pyke CM, Baade PD (2012) The descriptive epidemiology of female breast cancer: an international comparison of screening, incidence, survival and mortality. Cancer Epidemiol 36 (3): 237–248.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
van Breest Smallenburg, V., Nederend, J., Voogd, A. et al. Trends in breast biopsies for abnormalities detected at screening mammography: a population-based study in the Netherlands. Br J Cancer 109, 242–248 (2013). https://doi.org/10.1038/bjc.2013.253
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2013.253
Keywords
This article is cited by
-
Image-guided breast biopsy and localisation: recommendations for information to women and referring physicians by the European Society of Breast Imaging
Insights into Imaging (2020)
-
Position paper on screening for breast cancer by the European Society of Breast Imaging (EUSOBI) and 30 national breast radiology bodies from Austria, Belgium, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Denmark, Estonia, Finland, France, Germany, Greece, Hungary, Iceland, Ireland, Italy, Israel, Lithuania, Moldova, The Netherlands, Norway, Poland, Portugal, Romania, Serbia, Slovakia, Spain, Sweden, Switzerland and Turkey
European Radiology (2017)