Abstract
Background:
Circulating tumour cells (CTCs) can provide information on patient prognosis and treatment efficacy. However, there is no universal method to detect CTC currently available. Here, we compared the performance of two CTC detection systems based on the expression of the EpCAM antigen (CellSearch assay) or on cell size (ISET assay).
Methods:
Circulating tumour cells were enumerated in 60 patients with metastatic carcinomas of breast, prostate and lung origins using CellSearch according to the manufacturer's protocol and ISET by studying cytomorphology and immunolabelling with anti-cytokeratin or lineage-specific antibodies.
Results:
Concordant results were obtained in 55% (11 out of 20) of the patients with breast cancer, in 60% (12 out of 20) of the patients with prostate cancer and in only 20% (4 out of 20) of lung cancer patients.
Conclusion:
Our results highlight important discrepancies between the numbers of CTC enumerated by both techniques. These differences depend mostly on the tumour type. These results suggest that technologies limiting CTC capture to EpCAM-positive cells, may present important limitations, especially in patients with metastatic lung carcinoma.
Similar content being viewed by others
Main
Metastatic dissemination of malignant solid tumours is the main cause of death by cancer in the developed countries. The metastatic cascade is defined as a series of biological events that cancer cells from the primary neoplasia must complete to develop a new malignancy at a distant site, including the crucial step consisting in the release and survival of tumour cells in the peripheral blood (Sahai, 2007). These circulating tumour cells (CTCs) consist in a heterogeneous population of very rare cells native of either the primary tumour or its own metastasis (Mocellin et al, 2006; Sahai, 2007; Alix-Panabières et al, 2008). Key molecular events involved in metastatic progression are likely to have considerable effects on the number and on the phenotype of CTC. In this regard, experimental data suggest that biological processes such as the epithelial-to-mesenchymal transition (EMT), associated with the acquisition of cancer stem cell properties and resistance to conventional therapy, might have a role in the generation of more aggressive sub-populations of CTC (Polyak and Weinberg, 2009; Mego et al, 2010). Although the existence of CTC has been known for over a hundred of years, only the recent advent of novel cytometric (i.e., whole cell based) technologies have enabled significant progress in detecting and quantifying these cells. Using the CellSearch platform (Veridex, Warren, NJ, USA), several groups have shown an association between the counts of CTC identified by the assay and patients’ clinical outcome (Cristofanilli et al, 2004; Cohen et al, 2008; De Bono et al, 2008). Circulating tumour cell levels were indeed prospectively demonstrated to be an independent prognostic factor in patients with advanced breast, prostate and colorectal cancers treated by conventional and/or hormonal therapy (Cristofanilli et al, 2004; Cohen et al, 2008; De Bono et al, 2008). Moreover, longitudinal monitoring also indicated a potential role for enumerating CTC as an endpoint biomarker making it possible to predict, at an early stage, whether a patient benefits or not from anticancer treatment (Hayes et al, 2006). In addition to prognostic and predictive utility, CTC also represent a unique non-invasive source of tumour material susceptible to provide real-time information on the patient's current disease status. New possibilities with important clinical implications therefore concern the molecular characterisation of CTC since it could be incorporated in future clinical designs to monitor the efficacy of or resistance to targeted therapy.
Numerous technical efforts have been made to reliably detect and quantify CTC, but the development of a universal assay has proven quite difficult. Circulating tumour cells are indeed very rare events, occurring at rates as low as one cell per 106 or 107 leukocytes and most methods rely on the combination of two steps, that is, enrichment followed by detection to increase the sensitivity of the assay (Mostert et al, 2009). Another major technical challenge concerns tumour heterogeneity. Gene-expression profiling has highlighted the remarkable heterogeneity of malignant cells not only within a given histological subtype but also among tumour cells of any given patient. In addition to genetic instability inherent to most neoplastic cell types, emerging data suggest that cell-biological changes during metastatic progression, such as the transition between epithelial-to-mesenchymal states, can also generate distinct multiple cellular sub-populations contributing to intratumoural heterogeneity (Polyak and Weinberg, 2009; Thiery et al, 2009; Mego et al, 2010). Owing to this heterogeneity, the assay used for CTC detection could strongly impact on the biomarker value of CTC, and data regarding CTC should therefore be interpreted in the context of this method.
A rather limited number of studies comparing the performance of different assays and providing data to support the choice of a given method have been published (Lambrechts et al, 1999; Smith et al, 2000; Ring et al, 2005; Van der Auwera et al, 2010). This study was designed to directly compare the performance of two cytometric (i.e., CellSearch and ISET) systems based on different CTC properties, namely the expression of an epithelial antigen membrane vs cell size. The standardised and semi-automated CellSearch platform is the only assay currently approved by the Food and Drug Administration. Circulating tumour cell enrichment by CellSearch is based on the expression of the epithelial-lineage marker EpCAM (epithelial cell adhesion molecule). EpCAM-positive cells are enriched by immunomagnetic separation using EpCAM-specific antibodies conjugated to magnetic particles and then stained with fluorescent anti-cytokeratin and 4′,6-diamino-2-phenylindole (DAPI), while hematopoietic cells are stained with anti-CD45 antibodies. Cytokeratin and DAPI-positive, and CD45-negative CTC are finally counted by using a semi-automated fluorescent microscope (Cristofanilli et al, 2004; Hayes et al, 2006; Cohen et al, 2008; De Bono et al, 2008). ISET (isolation by size of epithelial tumour cells) makes it possible to collect tumour cells based on their larger size as cells are enriched by blood filtration through filtering membranes with calibrated pores 8 μm in diameter (Vona et al, 2000, 2004; Paterlini-Brechot and Benali, 2007). Enriched cells are stained on the filter for cytomorphological examination or further characterised by immunocytochemistry. As the performance of CTC detection assays may also be influenced by intrinsic characteristics of different tumour types, this study comprises 60 patients with metastatic carcinomas of breast, prostate and lung origins.
Patients and methods
Blood sample collection
This study was approved by our institutional review board and local ethics committee. Informed and written consent was obtained from all patients. Peripheral blood samples were collected from 60 patients with histologically or cytologically confirmed metastatic breast (n=20), prostate (n=20) or non-small cell lung cancer (n=20). Clinico-pathologic information was recorded for all patients. For each patient, 10 ml of blood was collected in EDTA tubes (Terumo, Leuven, Belgium) for CTC enumeration by ISET and 7.5 ml was collected in CellSave collection tubes (Immunicon Inc., Huntingdon Valley, PA, USA) for the CellSearch test.
Enumeration of CTC by CellSearch
Circulating tumour cell enumeration using the CellSearch system (Veridex LLC, Raritan, NJ, USA) was carried out according to the manufacturer's protocol and training. Blood samples were processed on the CellTracks Autoprep within 72 h. Epithelial cells were immunomagnetically enriched using ferrofluids coated with EpCAM-specific antibodies, then permeabilised and fluorescently labelled with phycoerythrin-conjugated antibodies directed against cytokeratin 8, 18 and 19, an allophycocyanin-conjugated antibody to CD45 and the nuclear dye DAPI. After transfer to a cartridge in a MagNest, labelled cells were analysed on the CellTracks Analyser II, a four-colour semi-automated fluorescent microscope that captures images of the entire surface of the cartridge for the four fluorescent dyes. From the captured images, a gallery of objects was presented to a trained operator (technician) who interprets each object. According to manufacturer guidelines, an object defined as a CTC should meet all of the following criteria: (i) an intact cell with a round to oval morphology and at least 4 μm in size; (ii) positive for DAPI with a nucleus inside the cytoplasm (of at least >50%) and a nucleus area smaller than the cytoplasm; (iii) positive for cytokeratins (bright or moderate) and negative for CD45 and the blank channel. Each sample was analysed independently by two trained technicians (NV and NJ).
Enumeration of CTC by ISET
ISET was carried out as previously reported (Vona et al, 2000, 2004; Paterlini-Brechot and Benali, 2007). Blood samples (10 ml) were processed within 4 h, diluted 1 : 10 in an erythrocyte-lysis buffer and filtered on the ISET device. The module filtration had a membrane of 10 wells making it possible to process blood samples of 10 ml (i.e., 100 ml of diluted blood). After filtration, membranes were washed with PBS, disassembled from the filtration module, allowed to air-dry overnight and stored at −20 °C until staining. Before staining, membranes were thawed, hydrated in TBS (Dako, Glostrup, Denmark), and treated at 98 °C in EDTA pH: 9.9, for 20 min, for antigenic retrieval. After being rinsed in TBS and dried at room temperature, membranes were permeabilised 5 min in the presence of TBS containing 0.2% Triton X100 (Roche, Mannheim, Germany) and incubated in methanol containing 3% H202 to block endogenous peroxydase. Membranes of patients with breast or lung cancer were incubated overnight at 4 °C in wet chambers, with an antibody raised against cytokeratin 7 (Dako), a keratin usually expressed in both malignant breast and lung tumours whereas those of patients with prostate cancer were stained with an anti-p504S antibody (Dako) directed to alpha-methylacyl coenzyme A racemase, a marker specifically and highly expressed in prostate adenocarcinoma. After rinsing in TBS, membranes were incubated with a secondary antibody labelled with peroxydase (Dako) for 45 min at room temperature. Finally, membranes were rinsed again in TBS, treated with diaminobenzidine (Dako) for 10 min and counterstained. Each immunostaining experiment included positive (a positive cell line stained with the specific antibody) and negative (the positive cell line stained with a nonspecific antibody of the same isotype and at the same concentration than the specific antibody) controls. Stained membranes were examined by a trained technician using light microscopy in two steps: (i) screening at × 20 magnification to locate cells, (ii) observation at × 63 magnification with oil immersion for detailed cytomorphological analysis. Isolated and/or clusters of cells of interest (immunostained or not) were selected, digitised, and examined by an experienced cytopathologist (PV). Circulating tumour cells were defined as cells presenting all the following criteria: (i) nuclear size equal or larger than two pores (i.e., equal or larger than 16 μ M); (ii) irregularity of the nuclear contour; (iii) presence of a visible cytoplasm; and (iv) high nuclear-to-cytoplasmic ratio (>0.8). When one or several of the above criteria were missing, cells were classified as atypical. Samples of 10 ml were usually processed on ISET, and calculations were made in order to express CTC in 7.5 ml.
Statistical methods
As CTC levels in patients were not normally distributed, results were presented as counts and medians with the corresponding percentages and ranges. Linear regression plots were computed for CTC counts obtained by the CellSearch and ISET techniques. As a result of the low number of patients and of CTC count distribution, CTC values determined using both CellSearch and ISET technique were correlated by the Spearman test.
Results
Each of the 60 patients with metastatic breast (MBC), prostate (MPC) and lung (MLC) carcinomas had blood collected for CTC enumeration by both the CellSearch and ISET techniques. Tables 1, 2 and 3 respectively show the clinico-pathological characteristics of the patients with MBC (n=20), MPC (n=20) and MLC (n=20), as well as their respective CTC counts obtained by both techniques. Representative examples of isolated CTC (panels A and B) and of a CTC cluster (panel C) detected by ISET are shown in Figure 1.
Microscopic analysis of CTC by ISET. (A–C) Examples of isolated CTC (A, B) and of a cluster of CTC (C) detected in a patient with metastatic prostate adenocarcinoma. Circulating tumour cells were enriched using the ISET device and stained with the anti-p504S monoclonal antibody. Circulating tumour cells were identified according to the following cytomorphological criteria: (i) nuclear size equal to or larger than two pores (i.e., equal to or larger than 16 μ M); (ii) the irregularity of the nuclear contour; (iii) the presence of a visible cytoplasm; (iv) a high nuclear-to-cytoplasmic ratio (>0.8). The 8 μm width pores are visible on (A–C).
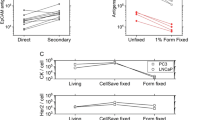
The median CTC count was of 2 CTC/7.5 ml for both techniques (range, 0–25 500 for CellSearch, range, 0–20 for ISET) in MBC patients. Circulating tumour cell counts for the two methods obtained were weakly correlated (r=0.46, P=0.04) (Figure 2A). Of the 20 patients with MBC, eight (40%) had CTC counts equivalent or superior to 5/7.5 ml by CellSearch while five (20%) had CTC counts ⩾5/7.5 ml by ISET (Table 1). Among the five negative patients using CellSearch, three were found positive by ISET, whereas of the three patients negative using ISET, one patient was found positive by CellSearch. Only two (10%) patients were negative using both techniques while discordant findings were obtained in four (15%) patients (Figure 2A). In patients with CTC detectable by both techniques, CTC counts were generally higher using CellSearch than by ISET. To further examine the concordance of both techniques, patients were classified according to the numbers of CTC detected by each technique: (i) patients with no detectable CTC (group 1); (ii) patients with CTC levels ranging from 1 to 4 CTC/7.5 ml (group 2); and (iii) patients with CTC levels equal or superior to 5 CTC/7.5 ml (group 3). Data are shown in Figure 3A. Eleven patients were found in the same group indicating a good concordance between both techniques in approximately half of the patients. In contrast, six patients had higher CTC counts using CellSearch than by ISET, while three patients had CTC counts higher using ISET than by CellSearch. Of the five patients with triple-negative breast cancer for ER, PR and HER2, a phenotype that has been reported to express cancer-stem cell and mesenchymal markers, and exhibit a more aggressive phenotype possibly associated with the EMT process and the downregulation of epithelial markers (Sarrió et al, 2008; Qi et al, 2010), two patients (B1, B5) had higher CTC counts using CellSearch than those obtained by ISET. Therefore, in contrast to a recent report using tumour cell lines spiked in normal blood samples (Sieuwerts et al, 2009), our study suggests that the capacity of the CellSearch system does not fail to detect CTCs in such patients.
Circulating tumour cells counts by CellSearch and ISET in patients with metastatic carcinomas of breast (MBC), prostate (MPC) and of lung (MLC) origin. (A) Circulating tumour cell counts by CellSearch and ISET in patients with MBC. (B) Circulating tumour cell counts by CellSearch and ISET in patients with MPC. (C) Circulating tumour cell counts by CellSearch and ISET in patients with MLC.
Classification of patients according to the numbers of CTC detected by CellSearch and ISET. (A) Classification of MBC patients according to the numbers of CTC detected by CellSearch and ISET. (B) Classification of MPC patients according to the numbers of CTC detected by CellSearch and ISET. (C) Classification of MLC patients according to the numbers of CTC detected by CellSearch and ISET. For each technique, patients with no detectable CTC were classified in group 1, patients with CTC levels ranging from 1 to 4 CTC/7.5 ml were classified in group 2 and patients with CTC levels equal or superior to 5 CTC/7.5 ml were classified in group 3.
In MPC patients, the median CTC count was of 8 CTC/7.5 ml (range, 0–1621) for CellSearch) and 17 CTC/7.5 ml (range, 1–248) for ISET. Circulating tumour cell counts for the two methods were again weakly correlated (r=0.46, P=0.04) (Figure 2B). Of the 20 MPC patients, 12 (60%) had CTC counts ⩾5/7.5 ml according to CellSearch while 15 (75%) had CTC counts ⩾5/7.5 ml using ISET (Table 2). All patients had detectable CTC by ISET while two patients were negative by CellSearch (P7 and P15 with 4 and 2 CTC/7.5 ml by ISET, respectively) (Table 2, Figure 2B). According to the classification already depicted, Figure 3B shows that 13 patients were classified in the same group indicating that concordant results were observed in 60% of the patients. Furthermore, six patients (30%) had CTC counts markedly higher according to ISET than CellSearch. Only one patient (P8) had 1 CTC/7.5 ml using ISET and 1621 CTC/7.5 ml according to CellSearch. No relationship was observed between clinico-pathological characteristics of these patients and their respective counts of CTC measured by each technique.
The median CTC count was of 0 CTC/7.5 ml (range, 0–13 500) for CellSearch and 5 CTC/7.5 ml (range, 1–100) for ISET in MLC patients. Circulating tumour cell counts obtained with both methods were moderately correlated (r=0.61, P=0.005) (Figure 2C). Of the 20 patients with MLC, 3 (15%) had CTC counts ⩾5/7.5 ml according to CellSearch, while 12 (60%) had CTC counts ⩾5/7.5 ml using ISET (Table 3). Eleven (55%) patients were negative according to CellSearch, while all patients were positive using ISET. Figure 3C shows that concordant results were obtained in only 4 patients (20%) while 16 (80%) patients had CTC counts markedly higher with ISET than CellSearch. In particular, four patients had CTC counts ⩾5/7.5 ml according to ISET and were negative using CellSearch. In one patient (L11), CTC counts were higher with CellSearch than with ISET (46 vs 14 CTCs/7.5 ml).
Discussion
Our prospective and comparative study of 60 patients with metastatic carcinoma demonstrates quite considerable discrepancies between the number of CTC enumerated by the CellSearch and the ISET systems. In all, 30% of patients (18 out of 60) were negative according to CellSearch while only 5% (3 out of 60) were negative using ISET. Concordant results only concern 28 of 60 patients (47%), whereas discordant results consist of patients with CTC counts higher according to ISET (25 out of 60; 42%) or with CTC counts higher using CellSearch (7 out of 60; 12%). Interestingly, these differences mostly depend on the type of tumour that the patient is harbouring.
In patients with MBC, CTC counts are generally higher by CellSearch than by ISET. The lower detection using ISET may be explained by the loss of CTC at different times of the process: (i) through the pores of 8 μ M during the procedure of filtration; (ii) during antigenic retrieval performed at 98 °C in an alkaline (pH: 9.9) buffer before immunolabelling, and/or; (iii) during the sequential washes used during the immunostaining procedure performed after filtration. Alternatively, CTC identified by CellSearch may not be true CTC. Indeed, CTC are detected by CellSearch on the basis of the expression of an epithelial marker (EpCAM), which does not formally establish the malignant nature of circulating cells in the blood retained as CTC. However, the specificity of CellSearch has been reliably documented in normal individuals and in patients with benign tumours (Allard et al, 2004). Therefore, the lower CTC counts obtained by ISET compared with CellSearch, likely results from cell loss during the ISET procedure. In order to minimise this cell loss, we currently bypass the critical antigen retrieval step and use more sensitive methods with immunofluorescent antibodies.
Overall, our results indicate a better detection of CTC in patients with MPC and MLC, via ISET than CellSearch. Low count of CTC with CellSearch has already been reported by other groups in MLC (Allard et al 2004; Okumura et al 2009). However, this study provides direct evidence for the first time that CTCs are underestimated by CellSearch in MPC and MLC patients because higher CTC levels are detected using another technique. All patients with MPC and 17 out of 20 patients with MLC had primary carcinomas of glandular origin, usually expressing the EpCAM antigen. These results may, in part, reflect data observed in experimental tumour models suggesting a continuum during the so-called EMT with the development of discrete tumour phenotypes, ranging from epithelial differentiation to mesenchymal phenotype and including patterns with various epithelio–mesenchymal mixed phenotypes (Mego et al, 2010). As tumour cells undergoing the EMT process are mainly characterised by the loss of epithelial markers, the neoexpression of cytoplasmic mesenchymal markers and of additional markers not detectable by CellSearch, the ISET system may be much more efficient in identifying all the cells of interest involved in the process. This has been recently shown in a series of patients with resectable lung cancer, where a significant proportion of CTC identified by ISET either co-expressed cytokeratins and vimentin or expressed vimentin alone (Hofman et al, 2011a). In this context, the use of alternative morphology-based enrichment technique such as ISET may offer significant advantages. However, this assay is still cumbersome, time consuming, and despite recent efforts (Hofman et al, 2011b) not standardised enough in its current form to be routinely applicable in clinical studies.
The criteria used by CellSearch for identifying CTC are mainly based on the size of the cytokeratin fluorescent signal that should be superior to 4 μm and on the location of the DAPI signal, which should be at least 50% inside the cytokeratin signal. It is noteworthy that CTC detection by CellSearch does not rely on any true morphological criteria. In contrast, CTC detected by ISET were identified by an experienced cytopathologist (PV) according to basic morphologic criteria such as a nucleus with a size equal to or larger than two pores (16 μm), irregularity of the nuclear contour, the presence of a visible cytoplasm and a high nuclear-to-cytoplasmic ratio (>0.8). The size of a normal eukaryotic cell usually ranges from 8 to 100 μm and tumour cells are generally bigger than their normal counterpart. The threshold of 16 μm (two-fold the diameter of a filter pore and the size of the smallest normal cell) was set to exclude most of the normal circulating blood cells. Several cells were classified as atypical because they either presented some but not all cytomorphological criteria (for example, nucleus size smaller than 16 μm) or were damaged. We obviously assume that some of these atypical cells may be malignant leading to an underestimation of CTC counts by ISET. Future studies combining morphological, phenotypical and molecular characterisation will provide additional information assessing or not their tumoural origin. We also decided to retain as CTC cells those that presented all the expected cytomorphological criteria required to establish the diagnosis of tumour cells, even if they were not stained by specific antibodies (data not shown). As we used an aggressive staining procedure based on antigenic retrieval to improve immunostaining, it is possible that some of these unstained cells were CTC negative for the selected marker thus potentially reflecting tumour cell phenotypic heterogeneity. Microemboli (namely, clusters of CTCs) that are rarely detectable by CellSearch were frequently observed by ISET (Figure 1). Within these microemboli, CTC counting was quite difficult and may have been underestimated in some patients.
In conclusion, by directly comparing CellSearch and a morphology-based enrichment technique (ISET), our study provides strong evidence that the CellSearch system, as well as potentially other current technologies that limit CTC capture to EpCAM-positive cells, does present important limitations. The limitations of the CellSearch system mainly concern patients with MLC, supporting the hypothesis of a phenotypic heterogeneity possibly linked to downregulation of the epithelial phenotype in these patients. Whether ISET is a more appropriate technique to enumerate and characterise CTC in patients bearing certain types of metastatic tumours such as MLC, is still a matter of debate. Our study did not compare the clinical relevance of both methods. Further studies on larger cohorts of patients are obviously needed to assess this important issue. ISET could indeed represent a more accurate clinical tool for predicting patient's outcome in certain tumour types, and provide a significant advantage for performing molecular analyses in the era of personalised medicine.
Change history
29 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Alix-Panabières C, Riethdorf S, Pantel K (2008) Circulating tumor cells and bone marrow micrometastasis. Clin Cancer Res 14: 5013–5021
Allard WJ, Matera J, Miller MC, Repollet M, Connelly MC, Rao C, Tibbe AG, Uhr JW, Terstappen LW (2004) Tumor cells circulate in the peripheral blood of all major carcinomas but not in healthy subjects or patients with nonmalignant diseases. Clin Cancer Res 10: 6897–6904
Cohen SJ, Punt CJ, Iannotti N, Saidman BH, Sabbath KD, Gabrail NY, Picus J, Morse M, Mitchell E, Miller MC, Doyle GV, Tissing H, Terstappen LW, Meropol NJ (2008) Relationship of circulating tumor cells to tumor response, progression-free survival, and overall survival in patients with metastatic colorectal cancer. J Clin Oncol 26: 3213–3221
Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Matera J, Miller MC, Reuben JM, Doyle GV, Allard WJ, Terstappen LW, Hayes DF (2004) Circulating tumor cells, disease progression, and survival in metastatic breast cancer. N Engl J Med 351: 781–791
De Bono JS, Scher HI, Montgomery RB, Parker C, Miller MC, Tissing H, Doyle GV, Terstappen LW, Pienta KJ, Raghavan D (2008) Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin Cancer Res 14: 6302–6309
Hayes DF, Cristofanilli M, Budd GT, Ellis MJ, Stopeck A, Miller MC, Matera J, Allard WJ, Doyle GV, Terstappen LW (2006) Circulating tumor cells at each follow-up time point during therapy of metastatic breast cancer patients predict progression-free and overall survival. Clin Cancer Res 15: 4218–4224
Hofman V, Bonnetaud C, Ilie MI, Vielh P, Vignaud JM, Fléjou JF, Lantuejoul S, Piaton E, Mourad N, Butori C, Selva E, Poudenx M, Sibon S, Kelhef S, Vénissac N, Jais JP, Mouroux J, Molina TJ, Hofman P (2011a) Preoperative circulating tumor cell detection using the isolation by size of epithelial tumor cell method for patients with lung cancer is a new prognostic biomarker. Clin Cancer Res 17: 827–835
Hofman VJ, Ilie MI, Bonnetaud C, Selva E, Long E, Molina T, Vignaud JM, Fléjou JF, Lantuejoul S, Piaton E, Butori C, Mourad N, Poudenx M, Bahadoran P, Sibon S, Guevara N, Santini J, Vénissac N, Mouroux J, Vielh P, Hofman PM (2011b) Cytopathologic detection of circulating tumor cells using the isolation by size of epithelial tumor cell method: promises and pitfalls. Am J Clin Pathol 135: 146–156
Lambrechts AC, Bosma AJ, Klaver SG Top B, Perebolte L, van' t Veer LJ, Rodenhuis S (1999) Comparison of immunocytochemistry, reverse transcriptase polymerase chain reaction, and nucleic acid sequence-based amplification for the detection of circulating breast cancer cells. Breast Cancer Res Treat 56: 219–231
Mego M, Mani SA, Cristofanilli M (2010) Molecular mechanisms of metastasis in breast cancer-clinical applications. Nat Rev Clin Oncol 7: 693–701
Mocellin S, Keilholz U, Rossi CR, Nitti D (2006) Circulating tumor cells: the ‘leukemic phase’ of solid cancers. Trends Mol Med 12: 130–1399
Mostert B, Sleijfer S, Foekens JA, Gratama JW (2009) Circulating tumor cells (CTCs): detection methods and their clinical relevance in breast cancer. Cancer Treat Rev 35: 463–474
Okumura Y, Tanaka F, Yoneda K, Hashimoto M, Takuwa T, Kondo N, Hasegawa S (2009) Circulating tumor cells in pulmonary venous blood of primary lung cancer patients. Ann Thorac Surg 87: 1669–1675
Paterlini-Brechot P, Benali NL (2007) Circulating tumor cells (CTC) detection: clinical impact and future directions. Cancer Lett 253: 180–204
Polyak K, Weinberg RA (2009) Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer 9: 265–273
Qi X, Yang X, Fan L, Zhang Y, Zhang F, Jiang J. (2010) Association between the spread of circulating tumor cells and breast cancer subtypes. Br Cancer Res 12: 402–403
Ring AE, Zabaglo L, Ormerod MG, Smith IE, Dowsett M (2005) Detection of circulating epithelial cells in the blood of patients with breast cancer: comparison of three techniques. Br J Cancer 92: 906–912
Sahai E (2007) Illuminating the metastatic process. Nat Rev Cancer; 7: 737–749
Sarrio D, Rodriguez-Pinilla SM, Hardisson D, Cano A, Moreno-Bueno G, Palacios J (2008) Epithelial-mesenchymal transition in breast cancer relates to the basal-like phenotype. Cancer Res 68: 989–997
Sieuwerts AM, Kraan J, Bolt J, van der Spoel P, Elstrodt F, Schutte M, Martens JW, Gratama JW, Sleijfer S, Foekens JA (2009) Anti-epithelial cell adhesion molecule antibodies and the detection of circulating normal-like breast tumor cells. J Natl Cancer Inst 101: 61–66
Smith BM, Slade MJ, English J, Graham H, Lüchtenborg M, Sinnett HD, Cross NC, Coombes RC (2000) Response of circulating tumor cells to systemic therapy in patients with metastatic breast cancer: comparison of quantitative polymerase chain reaction and immunocytochemical techniques. J Clin Oncol 18: 1432–1439
Thiery JP, Acloque H, Huang RY, Nieto MA (2009) Epithelial-mesenchymal transitions in development and disease. Cell 139: 871–890
Van der Auwera I, Peeters D, Benoy IH, Elst HJ, Van Laere SJ, Prové A, Maes H, Huget P, van Dam P, Vermeulen PB, Dirix LY (2010) Circulating tumour cell detection: a direct comparison between the CellSearch System, the AdnaTest and CK 19/mammaglobin RT-PCR in patients with metastatic breast cancer. Br J Cancer 102: 276–284
Vona G, Estepa L, Béroud C Damotte D, Capron F, Nalpas B, Mineur A, Franco D, Lacour B, Pol S, Bréchot C, Paterlini-Bréchot P (2004) Impact of cytomorphological detection of circulating tumor cells in patients with liver cancer. Hepatology 39: 792–797
Vona G, Sabile A, Louha M, Sitruk V, Romana S, Schütze K, Capron F, Franco D, Pazzagli M, Vekemans M, Lacour B, Bréchot C, Paterlini-Bréchot P (2000) Isolation by size of epithelial tumor cells: a new method for the immunomorphological and molecular characterization of circulating tumor cells. Am J Pathol 156: 57–63
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Farace, F., Massard, C., Vimond, N. et al. A direct comparison of CellSearch and ISET for circulating tumour-cell detection in patients with metastatic carcinomas. Br J Cancer 105, 847–853 (2011). https://doi.org/10.1038/bjc.2011.294
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2011.294
Keywords
This article is cited by
-
Comparative application of microfluidic systems in circulating tumor cells and extracellular vesicles isolation; a review
Biomedical Microdevices (2023)
-
Integrated microdevice with a windmill-like hole array for the clog-free, efficient, and self-mixing enrichment of circulating tumor cells
Microsystems & Nanoengineering (2022)
-
Current challenges in metastasis research and future innovation for clinical translation
Clinical & Experimental Metastasis (2022)
-
Label-free separation of neuroblastoma patient-derived xenograft (PDX) cells from hematopoietic progenitor cell products by acoustophoresis
Stem Cell Research & Therapy (2021)
-
Circulating tumor cell copy-number heterogeneity in ALK-rearranged non-small-cell lung cancer resistant to ALK inhibitors
npj Precision Oncology (2021)