Key Points
-
Coeliac disease is a chronic autoimmune-mediated enteropathy, caused by exposure to dietary gluten in genetically predisposed individuals.
-
Despite increased awareness, the majority of patients still remain undiagnosed.
-
Dentists should be aware of coeliac disease when symmetric enamel defects are observed.
Abstract
Coeliac disease is a chronic autoimmune-mediated enteropathy, caused by exposure to dietary gluten in genetically predisposed individuals that affects approximately 0.5-1% of the western population. Despite increased awareness of the disease, the majority of patients still remain undiagnosed. Disease frequently manifests in early childhood, but a significant proportion of patients are nowadays diagnosed above the age of 50. Timely diagnosis is important in order to start a gluten-free diet and prevent complications. Symptoms of coeliac disease vary widely and are certainly not restricted to the intestine. They may include, among others, dental and oral manifestations. Most of them are nonspecific but symmetric enamel defects are very specific to coeliac disease. It is important to recognise this relationship since it may help to identify unrecognised patients.
Similar content being viewed by others
Introduction
Coeliac disease is a chronic autoimmune-mediated enteropathy of the small bowel, caused by the dietary intake of gluten in genetically predisposed individuals.1 In these patients, the response towards gluten peptides causes an influx of lymphocytes in the duodenal epithelium, resulting in villous atrophy and consequently a decreased absorptive surface of the duodenum. The latter may result in malabsorption and deficiencies in nutrients and vitamin uptake.
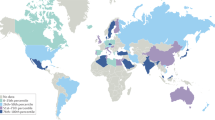
Physicians have recognised the symptoms of coeliac disease for over 100 years, in 1941 it was the Dutch physician Willem-Karel Dicke who described the relation between gluten intake and the clinical symptoms of coeliac disease for the first time.2 The prevalence of coeliac disease is approximately 0.5-1% in Western societies, Northern Africa, the Middle East and India.3,4
In most cases, the diagnosis is readily established and patients promptly improve after commencing a gluten-free diet. However, in some, the diagnosis is not straightforward and presents a challenge to clinicians. This may in part be due to the fact that coeliac disease can present with a wide variety of symptoms that may not be restricted to the gastrointestinal tract, which underscores the systemic nature of the disease.
Pathophysiology
Gluten are proteins found in wheat, barley, rye and some related cereals that are relatively resistant to proteolysis in the stomach. Large protein fragments enter the duodenal mucosa, where the gliadin part of gluten is deamidated by the enzyme tissue transglutaminase type 2 (tTG2). The gliadin peptides are presented by human leucocyte antigen (HLA) class II DQ2.5 (or, less commonly, HLA-DQ8 or HLA-DQ2.2) proteins to gluten-specific T cells. The presence of one of these genetic risk factors is necessary to develop the disease but not sufficient since approximately 40% of the Caucasian population is HLA-DQ2 or DQ8 positive. Vice versa, since >95% of patients carries at least one of these risk factors, the absence of these risk factors virtually rules out the possibility to develop coeliac disease.5 CD4+ T helper cells recognise the HLA-bound gliadin peptides and stimulate B cells to generate antibodies against both tTG2 and (deamidated) gliadin. This cascade of cellular interactions and subsequent cytokine production results in damage to the small bowel epithelium to such an extent that villous atrophy occurs6 (Fig. 1).
Clinical presentation and risk factors
The clinical features of coeliac disease are highly variable and reflect its systemic nature. Symptoms may be related to malabsorption, including chronic diarrhoea, weight loss, and abdominal distension. Other manifestations include iron deficiency with or without anaemia, reduced bone mineral density, aphthous stomatitis, short stature, elevated aminotransferase levels, dermatitis herpetiformis and chronic fatigue. Similar to other autoimmune diseases, there is a female preponderance. Notably, clinically silent coeliac disease has been increasingly detected by means of serologic screening, and in fact such studies have shown that the number of unrecognised coeliac patients outnumbers clinically recognised patients by a ratio of 7 to 1.7
Young children generally present with diarrhoea, bloating and failure to thrive. However, vomiting, agitation and even obstipation can be the only symptoms present. Older children and adolescents also frequently experience extra intestinal symptoms including growth retardation, fatigue caused by anaemia and neurological signs including migraine or even epilepsy.3,8
The classical symptoms of diarrhoea and abdominal pain occur in only 50% of adult coeliac patients. Other common (extra intestinal) symptoms include osteoporosis, complaints due to anaemia and (involuntary) weight loss. Less common symptoms include constipation, neurological symptoms, dermatitis herpetiformis, hypoproteinaemia and elevated transaminases.3 A significant proportion of coeliac patients is erroneously diagnosed with irritable bowel syndrome before the correct diagnosis.
The risk of developing coeliac disease is elevated in patients suffering from other autoimmune diseases including Hashimoto thyroiditis, type 1 diabetes, dermatitis herpetiformis, IgA-deficiency and autoimmune mediated liver diseases. The prevalence of coeliac disease is increased in individuals with Down syndrome, Williams syndrome, and in those having a first grade family member with coeliac disease.4,6
Diagnostic work-up
The presentation of coeliac disease can differ greatly between patients and serological testing is an essential tool in diagnosis. The most important serological markers include IgA antibodies against the enzyme tissue transglutaminase (TGA). For TGA the sensitivity and specificity are both 98%.9 A positive test outcome can be confirmed by testing for antibodies against endomysium (EMA) which has a comparable sensitivity and specificity. Determining the HLA-DQ genotype can lend further weight to the diagnosis or help to rule out the diagnosis. Analysis of the HLA-DQ genotype is also useful in screening family members of coeliac patients since first degree relatives that carry one of these genetic risk factors have a 10% risk to develop coeliac disease.
A positive test for TGA or EMA is an indication to perform a gastroduodenoscopy. Macroscopic abnormalities of the mucosa are often found during endoscopic evaluation (Fig. 2), but are not sufficient to establish the diagnosis. Histologic analysis remains the gold standard in diagnosing coeliac disease (Fig. 3). Histologic findings include intra epithelial lymphocytosis, crypt hyperplasia and varying degrees of villous atrophy that are scored according to the Marsh classification.6
According to recent guidelines from the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN), histological confirmation to establish the diagnosis is no longer mandatory in those children who have strongly elevated antibodies, positive HLA-DQ genotype and a clear clinical presentation.10
Treatment
The only recognised and accepted treatment of coeliac disease is a life-long gluten-free diet, i.e., foods that contain wheat, barley, rye, spelt or kamut. Adherence to this diet may be more difficult than frequently thought since gluten can be found in many processed foods, for example, salad dressing, soy sauce, chips, soups, candy, medication, and ice cream.
A growing number of individuals report complaints after eating gluten without having coeliac disease, referred to as 'non-coeliac gluten sensitivity' (NCGS).11 What causes symptoms in these patients is a matter of ongoing research but it cannot be excluded that other substances than gluten, for instance certain carbohydrates, are responsible for the complaints in these individuals.
Finally, there is currently a growing perception among a significant part of the population that a gluten-free diet is healthier than consuming gluten containing foods. Although there is no scientific basis that lends support to this, the number of individuals that embrace a gluten-free diet without a medical need is rapidly growing and has sparked the market for gluten-free products.
Complications
When coeliac disease is diagnosed early and the gluten-free diet is accurately followed, the mucosal architecture will restore and severe complications are uncommon. A very rare and feared complication includes enteropathy associated T cell lymphoma (EATL) and its precursor lesion, refractory coeliac disease type II (RCD II).12 Patients with RCD II, who are almost always over 50 years of age, have persistent villous atrophy despite strict adherence to a gluten-free diet resulting in a severe malabsorption syndrome.13 The prognosis of this condition is cumbersome since many will progress to an overt lymphoma.
Oral manifestations
Oral manifestations, including dental problems, can be part of the spectrum of coeliac disease. The most well-known are symmetric enamel defects. In 1990, Aine demonstrated that patients with coeliac disease have significantly more such defects when compared to healthy controls (83% versus 4%) and developed a classification for such defects (Table 1 and Figure 4).14 Studies differ in prevalence of enamel defects in both deciduous and permanent teeth.15,16 The pathophysiology of these enamel defects is unknown and several hypotheses are suggested. One hypothesis is the enamel defects could be a consequence of malabsorption in coeliac disease leading to hypocalcaemia. This has also been hypothesised to play a role in enamel anomalies in children with chronic disorders of calcium and phosphate homeostasis like hereditary vitamin D dependency rickets, X-linked hypophosphatemia and hypoparathyroidism.17 Another hypothesis includes the role of immunogenetic factors and is based on the knowledge that mineralisation of deciduous teeth in contrast to permanent teeth has been completed before birth and anomalies are also found in deciduous teeth.16 Remarkably, there is also a relatively high prevalence in first relatives of coeliac patients.18 An in vitro study showed that gliadin specific antibodies react with proteins in the enamel matrix (amelogenin and ameloblastin) which might play a role as well.19
In most coeliac patients only subtle enamel defects are seen, whereas the more severe defects are rare.4,20 Molars, incisors and cuspidates are most frequently affected. Remarkably, these enamel defects are also seen in so-called potential coeliac disease patients, that is, patients with positive coeliac serology and genetic phenotype but without duodenal damage.21
Recurrent aphthous stomatitis is also more often seen in coeliac patients and potential coeliac patients compared to healthy controls.4,22 Aphthous lesions are especially located at the labial mucosa and the tongue's lateral margins. Iron, folic acid and vitamin B12 deficiencies appear to play a role in the pathogenesis.15
Finally, 15–25% of children with coeliac disease develop atrophic glossitis and, consequently, difficulties with chewing, swallowing and sometimes even speaking.21 Box 1 shows all oral findings related to coeliac disease.
Future perspectives
As alluded to above, a strict gluten-free diet is currently the only available treatment for coeliac disease but may be difficult to adhere to. The improved understanding of coeliac disease pathogenesis has enabled researchers to suggest alternative strategies to treat the disorder. In this respect, enzymes have been identified that can break down gluten into harmless small peptide fragments within the acidic environment of the stomach, that is, before they reach the duodenal mucosa. The practical use is so far restricted by the sheer amount that has to be taken to ensure neutralisation of all the gluten. Interestingly, a recent in vitro study showed that certain oral microbes can digest gluten.22 These bacteria were found in dental plaque and saliva and are generally harmless. Especially Rothia mucilaginosa Human Oral Taxon-681 (HOT681), present in the oropharynx, oral cavity and duodenum, and Rothia aeria HOT-188 showed the ability to break down gluten into sufficiently small pieces that are harmless for coeliac patients. Identification of the enzyme responsible for this break down could form the basis of a new drug for coeliac disease patients.
Conclusion
Coeliac disease is a systemic disorder associated with a wide variety of different symptoms that are not restricted to the intestinal tract and is not a disease of young children. More and more patients are diagnosed in adulthood and it is known that many patients are undiagnosed. Extra-intestinal symptoms of relevance for dentists include symmetric enamel defects and recurrent aphthous stomatitis. Since oral and dental manifestations can be the only signs of coeliac disease, dentists should be aware of coeliac disease and if indicated refer patients to their general practitioner to perform a further diagnostic work up.
References
Ludvigsson J F, Leffler D A, Bai J C et al. The Oslo definitions for coeliac disease and related terms. Gut 2013; 62: 43–52.
Berge-Henegouwen G P van, Mulder C J . Pioneer in the gluten free diet: Willem-Karel Dicke 1905–1962, over 50 years of gluten free diet. Gut 1993; 34: 1473–1475.
Green P H, Cellier C . Coeliac disease. N Engl J Med 2007; 357: 1731–1743.
Krzywicka B, Herman K, Kowalczyk-Zając M, Pytrus T . Coeliac disease and its impact on the oral health status review of the literature. Adv Clin Exp Med 2014; 23: 675–681.
Al-Toma A, Goerres M S, Meijer J W, Peña A S, Crusius J B, Mulder C J . Human leucocyte antigen-DQ2 homozygosity and the development of refractory coeliac disease and enteropathy-associated Tcell lymphoma. Clin Gastroenterol Hepatol 2006; 4: 315–319.
Castillo N E, Theethira T G, Leffler D A . The present and the future in the diagnosis and management of coeliac disease. Gastroenterol Rep (Oxf) 2015; 3: 3–11.
Catassi C, Fabiani E, Rätsch I M et al. The coeliac iceberg in Italy. A multicentre antigliadin antibodies screening for coeliac disease in school-age subjects. Acta Paediatr Suppl 1996; 412: 29–35.
Maloney W J, Raymond G, Hershkowitz D, Rochlen G . Oral and dental manifestations of coeliac disease. N Y State Dent J 2014; 80: 45–48.
Leffler D A, Schuppan D . Update on serologic testing in coeliac disease. Am J Gastroenterol 2010; 105: 2520–2524.
Husby S, Koletzko S, Korponay-Szabó I R et al. European Society for Paediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Paediatr Gastroenterol Nutr 2012; 54: 136–160.
Nijeboer P, Bontkes H J, Mulder C J, Bouma G . Non-coeliac gluten sensitivity. Is it in the gluten or the grain? J Gastrointestin Liver Dis 2013; 22: 435–440.
van Gils T, Nijeboer P, Wanrooij R L . Mechanisms and management of refractory coeliac disease. Nat Rev Gastroenterol Hepatol 2015; 12: 572–579.
Daum S, Cellier C, Mulder C J . Refractory coeliac disease. Best Pract Res Clin Gastroenterol 2005; 19: m413–m424.
Aine L, Mäki M, Collin P, Keyriläinen O . Dental enamel defects in coeliac disease. J Oral Pathol Med 1990; 19: 241–245.
Pastore L, Corrocio A, Compilato D, Panzarella V, Serpico R, Muzio, Lorenzo L. Oral manifestations of celiac disease. J Clin Gastroenterol 2008; 42: 224–232.
Paéz E O, Lafuente P J, García P B et al. Prevalence of dental enamel defects in celiac patients with deciduous dentition: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 106: 74–78.
Nikiforuk G, Fraser D . The aetiology of enamel hypoplasia: a unifying concept. J Paediatr 1981; 98: 888–893.
Mäki M, Aine L, Lipsanen V, Koskimies S . Dental enamel defects in first-degree relatives of coeliac disease patients. Lancet 1991; 337: 763–764.
Muñoz F, Del Rió N, Sóñora C, Tiscornia I, Marco A, Hernández A . Enamel defects associated with coeliac disease: putative role of antibodies against gliadin in pathogenesis. Eur J Oral Sci 2012; 120: 104–112.
Trotta L, Biagi F, Bianchi P I et al. Dental enamel defects in adult coeliac disease: prevalence and correlation with symptoms and age at diagnosis. Eur J Intern Med 2013; 24: 832–834.
Bramanti E, Cicciù M, Matacena G, Costa S, Magazzù G . Clinical evaluation of specific oral manifestations in paediatric patients with ascertained versus potential coeliac disease: a cross-sectional study. Gastroenterol Res Pract 2014; 934159.
Fernandez-Feo M, Wei G, Blumenkranz G et al. The cultivable human oral gluten-degrading microbiome and its potential implications in coeliac disease and gluten sensitivity. Clin Microbiol Infect 2013; 19: E386–E394.
Rashid M, Zarkadas M, Anca A, Limeback H . Oral manifestations of coeliac disease: a clinical guide for dentists. J Can Dent Assoc 2011; 77: b39.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
van Gils, T., Brand, H., de Boer, N. et al. Gastrointestinal diseases and their oro-dental manifestations: Part 3: Coeliac disease. Br Dent J 222, 126–129 (2017). https://doi.org/10.1038/sj.bdj.2017.80
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2017.80
This article is cited by
-
Oral and dental manifestations of celiac disease in children: a case–control study
BMC Oral Health (2021)