Abstract
Study Design:
Cross-sectional validation study.
Objectives:
To validate the Italian version of the Spinal Cord Independence Measure Self-Report (SCIM SR).
Setting:
Two spinal cord injury (SCI) rehabilitation facilities in Italy.
Methods:
The SCIM III comprises items on 19 daily tasks, grouped into three subscales: ‘Self-care,’ ‘Respiration and sphincter management’ and ‘Mobility’. The total SCIM score ranges between 0 and 100. The Italian self-reported version (SCIM SR) was translated from the German tool. We studied 116 patients on their first hospitalization for rehabilitation after an SCI. At the time of discharge, patients were evaluated by the rehabilitation team using the SCIM III and self-assessed their independence with regard to activities of daily living using the SCIM SR. Pearson's correlation, Bland-Altman method, and stratified and regression analyses were used to examine the differences between evaluations.
Results:
On the basis of Pearson's correlation, there was good agreement between the data from the SCIM III and SCIM SR (r=0.918 for ‘Self-care,’ 0.806 for ‘Respiration and sphincter management,’ 0.906 for ‘Mobility’ and 0.934 for total scores). By Bland-Altman analysis, patients rated their functioning nearly the same as professionals—the mean difference between SCIM III and SCIM SR scores was approximately 0 for all subscales and total scores. The stratified and regression analyses failed to identify any specific factor that was associated with differences between SCIM III and SCIM SR scores.
Conclusions:
These results support the validity of the Italian version of the SCIM SR, which can facilitate longer-term evaluations of the independence of individuals with SCIs.
Similar content being viewed by others
Introduction
The Spinal Cord Independence Measure version III (SCIM III) is a scale that rates the independence of patients with spinal cord injuries (SCIs)1 with regard to performing activities of daily living. This tool was developed specifically for SCI patients and has become a widely used instrument to measure functioning in activities of daily living. The chief advantage of this instrument, which was first published in 1997,2 is its sensitivity to changes in the performance on tasks that are relevant to patients with SCIs. The validity and reliability of the third version of the SCIM have been tested in multicenter studies, which have demonstrated it to have satisfactory psychometric properties.3, 4, 5
SCIM III comprises items on 19 daily tasks that are grouped into three subscales that assess ‘Self-care’ (6 items, range 0–20), ‘Respiration and sphincter management’ (4 items, range 0–40) and ‘Mobility’ (9 items, range 0–40). The total SCIM III score ranges from 0 to 100, and higher scores reflect better performance or greater independence of a person.3 Item scores are graded for increasing difficulty and weighted by clinical relevance. Each item has between 2 and 9 grades. SCIM III is ranked by a multidisciplinary team, primarily in inpatient settings; this procedure is time-consuming.
Recently, a self-reported version of the SCIM III (SCIM SR) was created6 and translated into German, Italian and French, but only the German version has been validated.
Self-administered questionnaires are the instrument of choice for data collection outside the hospital, because they require few resources, are faster and can be applied independently from the evaluation settings.6, 7, 8
Thus, the SCIM SR is invaluable because it monitors and detects any special health needs in SCI patients after discharge from the hospital and because it helps in the collection of data for research. The purpose of this study was to compare the Italian versions of the SCIM SR and SCIM III and assess their validity.
Materials and methods
Subjects
Consecutive patients who were admitted to the Spinal Unit of Montecatone Rehabilitation Institute (MRI) and the Spinal Unit of IRCCS Fondazione S. Lucia, Italy, were recruited between February and December 2013. The criteria for eligibility were a traumatic or a nontraumatic SCI (time since injury ⩾1 month), sufficient Italian language skills (as assessed by the clinical staff), and the ability to read and answer the self-report questions independently. People with severe health conditions or cognitive impairments were excluded.
The following information was collected from their medical records: age, gender, etiology, date of injury, level of lesion (paraplegia/tetraplegia) and American Spinal Injury Association (ASIA) Impairment Scale (AIS) grade.
Procedure and instrument development
Participants were asked to fill in a paper-pencil version of the SCIM SR questionnaire. If they had difficulties writing owing to limited hand function, their caregiver helped them complete the form but did not explain the items or assist in choosing an answer. On the same day, health professionals (including physicians, physiotherapists and nursing staff) with experience with SCIM III completed the Italian SCIM III9 (which is used routinely in both of the rehabilitation centers in this research) through observation of the participants.3
The English version of the SCIM SR has been translated into Italian by professional scientific translators (www.five.ch). Before being administered to the study subjects, the Italian draft version of the SCIM SR was tested in cognitive interviews of five individuals with SCIs who were recruited at IRCCS Fondazione S. Lucia. In addition, five Italian-speaking experts who have used the SCIM III in a clinical setting have been asked to comment on the draft version of SCIM SR. Cognitive interviews are important to determine the comprehensibility of questionnaires before being applied in surveys.10
The results of this pretest guided the final changes to the Italian draft version of the SCIM SR (Appendix A and B). Then, final modifications were made to establish the test version for the validation phase. We certify that all applicable institutional and governmental regulations that concern the ethical use of human volunteers were followed during this study.
Statistical analyses
Descriptive statistics on patient characteristics were expressed as mean and standard deviation or frequency and percentage. Descriptive statistics were also reported for the SCIM III and SCIM SR total and subscale scores, and the nonparametric Wilcoxon signed-rank test was used to analyze differences in medians.
Pearson’s correlation coefficients were calculated to analyze the linear relationship between SCIM III and SCIM SR. Moreover, intraclass correlation (ICC) was performed to assess the conformity of SCIM III and SCIM SR scores, because they represent two quantitative measurements by different observers (clinician and patient) on the same subject. The ICC coefficient takes into account interobserver and intraobserver variability and is a composite measure of these factors.11 According to previous work,12 a correlation of 0.80 is considered a fairly strong relationship, a correlation of 0.60 signifies a moderate relationship and a value of 0.20 indicates that the scores are weakly associated.
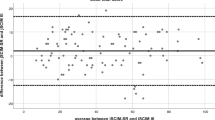
The Bland-Altman method was used to calculate the mean and limit of agreement (LOA) to describe the differences between SCIM III and SCIM SR scores. The mean difference and LOAs are reported in Bland-Altman plots that show the difference between SCIM SR and SCIM III scores against the mean scores of both measurements for each subject, which is useful for detecting outliers.13
For formal analyses, stratified mean differences between total SCIM III and SCIM SR scores were calculated and linear regression was performed, after the assumption of normal distribution was tested by the Shapiro test and normal QQ plot. In a stratified analysis, the mean difference is compared between variable categories; thus, age was grouped into three classes: youngest (<35 years), middle (35–54 years) and oldest (>54 years). In the regression analysis, we regressed the difference between the two total scores as continuous outcomes on select potential predictors, introduced as continuous (age and time) or categorical variables (gender, lesion level, AIS grade and etiology). Univariate and multivariate models were constructed. For each explanatory variable, the coefficient and its 95% confidence interval were computed, and the F test was performed to determine the significance of the association between predictors and outcome. Factors were considered to be meaningful at a significance level of 0.05.
The data were analyzed using R v3.0.2.
Results
We enrolled 116 patients (80 males, mean age 45.5 years), the characteristics of whom are presented in Table 1.
Overall, the cognitive interviews with patients and professionals demonstrated that the Italian SCIM SR was understandable and acceptable.
Table 2 lists the descriptive statistics of the SCIM III and SCIM SR scores and their P-values by the nonparametric Wilcoxon signed-rank test. There were no missing values for any scale score. The scores were not normally distributed (see Figure 1); thus, we could only compare the median values by the nonparametric Wilcoxon signed-rank test instead of the means. The means, medians and interquartile ranges were similar, and median total and subscale SCIM III and SCIM SR scores did not differ significantly (P-values>0.05).
Pearson's and ICC correlation coefficients between SCIM III and SCIM SR scores are shown in Table 3. Pearson's correlation coefficients ranged from 0.806 for the 'Respiration and sphincter management' subscale to 0.934 for the total score. Although 'Respiration and sphincter management' had the lowest coefficient, it was sufficiently high (>0.7) to demonstrate a linear relationship between SCIM III and SCIM SR. Also, the ICC values were high, approximating the linear correlation coefficients. The scores of the two measurements are plotted in Figure 2—the evaluations by the SCIM III and SCIM SR strongly agree, because the points are uniformly distributed around the line of equality (the bisect of each figure).
SCIM III and SCIM SR scores. The graph shows the plotting of the scores of the two measurements. The points are uniformly distributed around the line of equality (the bisect of each figure), thus demonstrating that the evaluations by the SCIM III and SCIM SR strongly agree. A full color version of this figure is available at the Spinal Cord journal online.
The difference between scores was estimated by the Bland-Altman method, as shown in Table 4. As expected, the mean differences were close to 0, confirming the agreement between SCIM III and SCIM SR scores. The LOAs can be interpreted as a reference interval—that is, the range in which most differences lie.13 12 In Table 4, we can see that this range is about ±5 for the subscale ‘Self-Care’, ±10 for the subScale ‘Respiration and sphincter management’, ±9 for ‘Mobility’ and ±16 for the total score. The ranges vary from 16.3%, 22.7% and 24.2% to 25.6%, respectively. The LOA included over 92% of the differences in all scales, and the Bland-Altman plots (Figure 3) showed that there were few outliers for each scale. In addition, the LOA for the total score included 95% of the observations, which were normally distributed as indicated in the normal Q-Q plot (Figure 4) and confirmed by the Shapiro test (P-value=0.102).
With the assumption of a normal distribution, we calculated the 95% confidence interval of the mean difference in total scores in the stratified analysis and generated regression models (Table 5). The difference between total scores was small for all classes and had a range of ±1. The largest disparity arose between the mean difference for AIS A (−1.33) and AIS C (1.54). However, because all 95% confidence intervals contain the 0 value, we conclude that there were no significant differences between total SCIM SR and SCIM III scores in any category. None of the explanatory variables was a significant predictor of the difference between SCIM III and SCIM SR scores based on both the models of the regression analysis (P-values).
Discussion
Our results support the validity of the criteria of the SCIM SR compared with the SCIM III.6 The patient feedback and cognitive interviews provided valuable data that we used to establish preliminary validity of the content of the SCIM SR in the self-evaluation of patients with SCIs.
The mean and median SCIM III and SCIM SR scores were similar for each scale, indicating that patients and clinicians judged the patient’s performance to be the same. The Pearson correlation and ICC coefficients of the total and subscale scores met the quality criterion (>0.7). 6, 14
Moreover, by Bland-Altman analysis, with mean differences of approximately 0, the self-evaluation by SCIM SR and the evaluations by professionals with SCIM III were very close for the total and the sub-items scores. This result differs from the validation study of the German version of SCIM SR,6 in which patients systematically rated their ‘mobility’ to be higher than did professionals.
In the regression analysis, we observed no association between the differences in scores and any explanatory variable—that is, there was no class patients who were at risk of completing the SCIM SR form differently from professionals. This result is an important finding, because it demonstrates the reliability of this tool for each type of patient, without regard to his sociodemographic or clinical characteristics.
As reported,6 item 6 (bladder management) has been changed in adapting SCIM SR to SCIM III. In the conversion table (Appendix B), score 3 is missing because of the inability to measure residual urine volume by self-report; score 6 is used in its place. This arrangement amplifies the score on item 6 in the SCIM SR and masks those cases in which patients judge themselves the same as clinicians do. Nevertheless, these results indicate high correlation between item 6 of the SCIM SR and SCIM III, as with the German version.6 However, this oversight can affect the results, because there are some cases in which a score of 6 is excessive and a score 0 is inappropriate. Thus, to increase the precision and accuracy, a new conversion table that takes into account a score of between 0 and 6 should be adopted.
Another drawback is that our study was limited to the time of discharge. To use this instrument for longer follow-ups, a specific and an appropriate validation study that at least performs test-retest correlation and comparison—with, for example, a quality of life measure—would be needed.
With regard to strengths, our sample size was sufficiently high for a validation study.6, 13 Moreover, our study included many patient characteristics and was thus representative of the study population and did not have missing data, increasing its reliability.
Finally, the number of negative differences, corresponding to patients who overestimated their functioning, compensated for the number of patients who underestimated their performance, supporting the hypothesis of contingency of the difference between measurements and highlighting the strength of SCIM SR instrument in assessing the performance of SCI patients after discharge from the hospital.
Conclusion
Our findings support the criterion validity of the SCIM SR, and, because SCIM III is the only comprehensive instrument that measures disability that has been developed specifically for individuals with SCIs,6 the self-reported version can be used for continued monitoring of daily activities in community-dwelling individuals and might detect special health-care needs in this population. The only precaution that must be taken concerns the reliability of the patients, which depends on their mental status.
Date archiving
There were no data to deposit.
References
Anderson K, Aito S, Atkins M, Biering-Sørensen F, Charlifue S, Curt A et al. Functional recovery measures for spinal cord injury: an evidence-based review for clinical practice and research. J Spinal Cord Med 2008; 31: 133–144.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A . SCIM—spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord 1997; 35: 850–856.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil 2007; 29: 1926–1933.
Anderson KD, Acuff ME, Arp BG, Backus D, Chun S, Fisher K et al. United States (US) multi-center study to assess the validity and reliability of the Spinal Cord Independence Measure (SCIM III). Spinal Cord 2011; 49: 880–885.
Fekete C, Eriks-Hoogland I, Baumberger M, Catz A, Itzkovich M, Lüthi H et al. Development and validation of a self-report version of the Spinal Cord Independence Measure (SCIM III). Spinal Cord 2013; 51: 40–47.
Hoenig H, Branch LG, McIntyre L, Hoff J, Horner RD . The validity in persons with spinal cord injury of a self-reported functional measure derived from the functional independence measure. Spine 1999; 24: 539–543.
Dorevitch M . The 'questionnaire' versus the 'direct observation' approach to functional assessment. Br J Rheumatol 1988; 27: 326–327.
Invernizzi M, Carda S, Milani P, Mattana F, Fletzer D, Iolascon G et al. Development and validation of the Italian version of the Spinal Cord Independence Measure III. Disabil Rehabil 2010; 32: 1194–1203.
Tourangeau R, Rips LJ, Rasinski K . The Psychology of Survey Response. Cambridge University Press: Cambridge, 2000.
Shrout PE, Fleiss JL . Intraclass correlations: uses in assessing rater reliability. Psychol Bull 1979; 86: 420–428.
Malgady RG, David E, Krebs DE . Understanding correlation coefficients and regression. Phys Ther 1986; 66: 110–120.
Bland JM, Altman DG . Measuring agreement in method comparison studies. Stat Methods Med Res 1999; 8: 135–160.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60: 34–42.
Acknowledgements
This work was supported by the Italian Ministry of Health (RC08G) and the European Commission in the Seventh Framework Program ICT-2013- 611626 SYMBITRON. The manuscript was reviewed for English language by ‘Blue Pencil’ Science.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendices
APPENDIX A
Italian version of SCIM III for Self-Reported.
Attività della vita quotidiana
Indichi p.f. per ogni domanda l’affermazione che meglio riflette la Sua situazione attuale. Legga attentamente le domande e scelga sempre solo una risposta.
1. Mangiare e bere
[0] ○ Necessito di alimentazione artificiale oppure ho una sonda gastrica.
[0] ○ Necessito di assistenza completa per mangiare/bere.
[1] ○ Necessito di assistenza parziale per mangiare/bere, oppure per mettere/togliere i mezzi d’ausilio.
[2] ○ Mangio/bevo autonomamente, ma necessito di mezzi d’ausilio o assistenza quando devo tagliare il cibo, versarmi da bere o aprire confezioni.
[3] ○ Mangio/bevo autonomamente senza assistenza né mezzi d’ausilio.
2.a. Lavare la parte superiore del corpo e la testa
Con lavare la parte superiore del corpo e della testa s’intende l’azione di insaponarsi e asciugarsi, nonché l’utilizzo del rubinetto dell’acqua.
[0] ○ Necessito di assistenza completa.
[1] ○ Necessito di assistenza parziale.
[2] ○ Sono autosufficiente, ma necessito di mezzi d’ausilio o di un’attrezzatura speciale (per es. barre di appoggio, sedia).
[3] ○ Sono autosufficiente e non necessito di mezzi d’ausilio né di un’attrezzatura speciale.
2.b. Lavare la parte inferiore del corpo
Con lavare la parte inferiore del corpo s’intende l’azione di insaponarsi e asciugarsi, nonché l’utilizzo del rubinetto dell’acqua.
[0] ○ Necessito di assistenza completa.
[1] ○ Necessito di assistenza parziale.
[2] ○ Sono autosufficiente, ma necessito di mezzi d’ausilio o di un’attrezzatura speciale (per es. barre di appoggio, sedia).
[3] ○ Sono autosufficiente e non necessito di mezzi d’ausilio né di un’attrezzatura speciale.
3.a. Vestire e svestire la parte superiore del corpo
Con vestire e svestire la parte superiore del corpo si intende l’azione di mettersi e togliersi indumenti quali magliette, camicie, reggiseno, sciarpe od ortesi (per es. tutori braccia, collari, corsetti).
Per indumenti facili da indossare si intendono indumenti senza bottoni, cerniera lampo o lacci.
Per indumenti difficili da indossare si intendono indumenti con bottoni, cerniera lampo o lacci.
[0] ○ Necessito di assistenza completa.
[1] ○ Necessito di assistenza parziale, anche se si tratta di indumenti facili da indossare.
[2] ○ Non necessito di assistenza se si tratta di indumenti facili da indossare, ma necessito di mezzi d’ausilio o di un’attrezzatura speciale.
[3] ○ Metto e tolgo gli indumenti in autonomia se si tratta di indumenti facili da indossare. Necessito di assistenza o mezzi d’ausilio o di un’attrezzatura speciale solo con indumenti difficili da indossare.
[4] ○ Metto e tolgo indumenti in totale autonomia.
3.b. Vestire e svestire la parte inferiore del corpo
Con vestire e svestire la parte inferiore del corpo si intende l’azione di mettere e togliere indumenti quali pantaloncini, pantaloni, scarpe, calze, cinture od ortesi (per es. tutori gamba).
Per indumenti facili da indossare si intendono indumenti senza bottoni, cerniera lampo o lacci.
Per indumenti difficili da indossare si intendono indumenti con bottoni, cerniera lampo o lacci.
[0] ○ Necessito di assistenza completa.
[1] ○ Necessito di assistenza parziale, anche se si tratta di indumenti facili da indossare.
[2] ○ Non necessito di assistenza se si tratta di indumenti facili da indossare, ma necessito di mezzi d’ausilio o di un’attrezzatura speciale.
[3] ○ Metto e tolgo indumenti in autonomia se si tratta di indumenti facili da indossare. Necessito di assistenza o mezzi d’ausilio o di un’attrezzatura speciale solo con indumenti difficili da indossare.
[4] ○ Metto e tolgo indumenti in totale autonomia.
4. Cura di viso e mani
Pensi p.f. ad attività come lavarsi mani, viso e denti, pettinarsi, radersi, truccarsi.
[0] ○ Necessito di assistenza completa.
[1] ○ Necessito di assistenza parziale.
[2] ○ Sono autosufficiente con l’utilizzo di mezzi d’ausilio.
[3] ○ Sono autosufficiente senza l’utilizzo di mezzi d’ausilio.
5. Respirazione
Necessito di una cannula per la respirazione (cannula tracheale)…
[0] ○ e di respirazione assistita permanente o periodica.
[2] ○ e di ossigeno supplementare nonché di una notevole assistenza nel tossire o nella gestione della cannula per la respirazione.
[4] ○ e di assistenza limitata nel tossire o nella gestione della cannula per la respirazione.
Non necessito della cannula per la respirazione (cannula tracheale)…
[6] ○ bensì di ossigeno supplementare o di notevole assistenza nel tossire o di una maschera (per es. PEEP) o di respirazione assistita periodica (per es. BIPAP).
[8] ○ e di assistenza limitata o stimolazione della tosse.
[10] ○ e riesco a respirare e tossire autonomamente senza assistenza o mezzi d’ausilio.
6. Svuotamento della vescica
Pensi p.f. al modo in cui Lei svuota la vescica.
6. a) Utilizzo di un catetere permanente
[0] ○ Sì >> Passare alla domanda 7.a.
[1] ○ No >> Passare alle domande 6.b e 6.c.
6. b) Cateterizzazione occasionale
[0] ○ Necessito di assistenza completa nell’esecuzione dell’operazione.
[1] ○ Riesco a eseguire l’operazione in autonomia con assistenza (autocateterizzazione).
[2] ○ Riesco a eseguire l’operazione in autonomia senza assistenza (autocateterizzazione).
[3] ○ Non la utilizzo.
6. c) Utilizzo di mezzi d’ausilio per la raccolta dell’urina
Per es. catetere del preservativo, pannolini o assorbenti
[0] ○ Li utilizzo con assistenza completa.
[1] ○ Li utilizzo con assistenza parziale.
[2] ○ Li utilizzo senza assistenza.
[3] ○ Non soffro di incontinenza urinaria e non utilizzo mezzi d’ausilio.
7. Svuotamento intestinale
7. a) Necessita di assistenza per lo svuotamento intestinale?
Per es. per mettere delle supposte
[0] ○ Sì
[1] ○ No
7. b) La frequenza di evacuazione è…
[0] ○ irregolare o rara (inferiore a una volta ogni tre giorni).
[1] ○ regolare (ogni tre giorni o più spesso).
7. c) L’incontinenza fecale si manifesta…
[0] ○ due volte al mese o più spesso.
[1] ○ una volta al mese.
[2] ○ mai.
8. Utilizzo della toilette
Per utilizzo della toilette si intende la pulizia delle parti intime e delle mani, la gestione degli indumenti e l’utilizzo di assorbenti o pannolini.
[0] ○ Necessito di assistenza completa.
[1] ○ Necessito di assistenza parziale e non sono in grado di lavarmi autonomamente.
[2] ○ Necessito di assistenza parziale, ma riesco a lavarmi autonomamente.
[4] ○ Non necessito di assistenza, ma necessito di mezzi d’ausilio (per es. barre di appoggio) o di un’attrezzatura speciale (per es. toilette idonea al passaggio della sedia a rotelle).
[5] ○ Non necessito di assistenza né di mezzi d‘ausilio o di attrezzatura speciale.
9. Quante delle seguenti attività riesce a svolgere senza assistenza o dispositivi elettrici? - Girarsi con la parte superiore del corpo nel letto - Girarsi con la parte inferiore del corpo nel letto - Mettersi seduto sul letto - Sollevarsi sulla sedia a rotelle (con o senza mezzi d’ausilio)
[0] ○ Nessuna; necessito di assistenza per tutte le suddette attività.
[2] ○ Una
[4] ○ Due o tre
[6] ○ Tutte
10. Trasferimento dal letto alla sedia a rotelle
[0] ○ Necessito di assistenza completa.
[1] ○ Necessito di assistenza, sorveglianza o mezzi d’ausilio (per es. ribaltina).
[2] ○ Non necessito di assistenza né di mezzi d’ausilio.
[2] ○ Non utilizzo la sedia a rotelle.
11. Trasferimento dalla sedia a rotelle sul water/nella vasca da bagno
Per trasferimento si intende anche il trasferimento dalla sedia a rotelle o dal letto alla sedia a rotelle per la toilette.
[0] ○ Necessito di assistenza completa.
[1] ○ Necessito di assistenza, sorveglianza o mezzi d’ausilio (per es. barre di appoggio).
[2] ○ Non necessito di assistenza né di mezzi d’ausilio.
[2] ○ Non utilizzo la sedia a rotelle.
12. Spostamenti nella propria abitazione
Utilizzo la sedia a rotelle. Per gli spostamenti...
[0] ○ necessito di assistenza completa.
[1] ○ necessito della sedia a rotelle elettrica o di parziale assistenza nello spostamento con la sedia a rotelle manuale.
[2] ○ non necessito di assistenza con la sedia a rotelle manuale.
In casa mi sposto a piedi e...
[3] ○ necessito di sorveglianza mentre cammino (con o senza strumenti di supporto per camminare).
[4] ○ cammino con il deambulatore o con le stampelle e porto i piedi avanti contemporaneamente.
[5] ○ cammino con le stampelle o con due bastoni e porto avanti prima un piede poi l’altro.
[6] ○ cammino con il bastone.
[7] ○ cammino solo con ortesi per le gambe (per es. tutore gamba).
[8] ○ cammino senza strumenti di supporto.
13. Spostamento per distanze di piccola/media lunghezza (10 - 100 metri)
Utilizzo la sedia a rotelle. Per gli spostamenti…
[0] ○ necessito di assistenza completa.
[1] ○ necessito della sedia a rotelle elettrica o di assistenza parziale per spostarmi con la sedia a rotelle manuale.
[2] ○ non necessito di assistenza con la sedia a rotelle manuale.
Percorro distanze di piccola/media lunghezza a piedi e...
[3] ○ necessito di sorveglianza mentre cammino (con o senza strumenti di supporto per camminare).
[4] ○ cammino con il deambulatore o con le stampelle e porto i piedi avanti contemporaneamente.
[5] ○ cammino con le stampelle o con due bastoni e porto avanti prima un piede poi l’altro.
[6] ○ cammino con il bastone.
[7] ○ cammino solo con ortesi per le gambe (per es. tutore gamba).
[8] ○ cammino senza strumenti di supporto.
14. Spostamenti fuori casa per oltre 100 metri
Utilizzo la sedia a rotelle. Per gli spostamenti…
[0] ○ necessito di assistenza completa.
[1] ○ necessito della sedia a rotelle elettrica o di assistenza parziale per spostarmi con la sedia a rotelle manuale.
[2] ○ non necessito di assistenza con la sedia a rotelle manuale.
Cammino per oltre 100 metri e...
[3] ○ necessito di sorveglianza mentre cammino (con o senza strumenti di supporto per camminare).
[4] ○ cammino con il deambulatore o con le stampelle e porto i piedi avanti contemporaneamente.
[5] ○ cammino con le stampelle o con due bastoni e porto avanti prima un piede poi l’altro.
[6] ○ cammino con il bastone.
[7] ○ cammino solo con ortesi per le gambe (per es. tutore gamba).
[8] ○ cammino senza strumenti di supporto.
15. Salire le scale
[0] ○ Non riesco né a salire né a scendere.
Riesco a salire e scendere almeno tre gradini…
[1] ○ ma solo se assistito o sorvegliato.
[2] ○ ma solo con mezzi d’ausilio (per es. corrimano, stampella o bastone).
[3] ○ senza assistenza, sorveglianza o mezzo d’ausilio.
16. Trasferimento dalla sedia a rotelle all‘automobile
Per trasferimento si intende anche il carico e lo scarico della sedia a rotelle.
[0] ○ Necessito di assistenza completa.
[1] ○ Necessito di assistenza, sorveglianza o mezzi d’ausilio.
[2] ○ Non necessito di assistenza né di mezzi d’ausilio.
[2] ○ Non utilizzo la sedia a rotelle.
17. Trasferimento dal pavimento alla sedia a rotelle
[0] ○ Necessito di assistenza.
[1] ○ Non necessito di assistenza.
[1] ○ Non utilizzo la sedia a rotelle.
APPENDIX B
Scoring of item 6 (Svuotamento della vescica) in SCIM SR
APPENDIX C
Scoring of item 7 (Svuotamento intestinale) in SCIM SR
Rights and permissions
About this article
Cite this article
Bonavita, J., Torre, M., China, S. et al. Validation of the Italian version of the Spinal Cord Independence Measure (SCIM III) Self-Report. Spinal Cord 54, 553–560 (2016). https://doi.org/10.1038/sc.2015.187
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.187
This article is cited by
-
Validation of the Thai version of the Spinal Cord Independence Measure Self-Report (SCIM-SR-Thai)
Spinal Cord (2022)
-
Functional independence in the Finnish spinal cord injury population
Spinal Cord (2022)
-
Cross-cultural adaptation and psychometric testing of the Thai version of the Spinal Cord Independence Measure III—Self Report
Spinal Cord (2021)
-
Adaptation and validation of the Japanese version of the Spinal Cord Independence Measure (SCIM III) self-report
Spinal Cord (2021)
-
Translation and validation of the Chinese version of the Spinal Cord Independence Measure (SCIM III) Self-Report
Spinal Cord (2021)