Abstract
Study design:
A cross-sectional study.
Objectives:
To translate and assess the reliability and discriminative ability of the Spinal Cord Independence Measure III (SCIM III), Thai version (Th-SCIM III).
Setting:
A tertiary rehabilitation center in Thailand.
Methods:
The SCIM III was translated into the Thai version with a forward–backward translation. The tool was then used by three physical therapists to assess 31 subjects with various degrees of spinal cord injury (SCI) during the first week after admission.
Results:
The Th-SCIM III had excellent inter-rater reliability (intraclass correlation coefficient >0.90) and good internal consistency (Cronbach’s alpha ⩾0.88), and could significantly discriminate between the performance of subjects with varying degrees of lesion severity. Scores of 50 and over could moderately discriminate between subjects with motor complete SCI and incomplete SCI (sensitivity 68.75%, specificity 66.67%, 95% confidence interval=0.62–0.95).
Conclusion:
The findings support the reliability and discriminative ability of the Th-SCIM III. The tool may benefit clinical assessments for overall aspects relating to SCI, particularly for Thai physical therapists. However, a further exploration of other psychometric properties may enhance the clinical utility of the tool.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) causes deterioration of motor, sensory and autonomic functions, with consequent profound effects on physical performance.1 Although patients with SCI can improve their performance after participation in a rehabilitation program,1, 2, 3 the dramatically decreased length of rehabilitation4 suggests a crucial need for an effective rehabilitation program and a thorough quantitative assessment to promote performance and to clearly quantify the functional alteration of patients.
The Spinal Cord Independence Measure (SCIM) is a quantitative tool specifically designed to assess overall performance relating to SCI. The tool was originally developed at the Loewenstein Rehabilitation Hospital by Catz et al.5 It was later modified (SCIM II) to separate bathing and dressing for upper and lower parts of the body, with minor changes in phrasing of the scoring criteria for other functions.6 The SCIM III, the latest version, was established in 2002 to include a new item (transfer: ground–wheelchair) and slightly modified the scores of various sub-items to keep the same total score (100).3
The SCIM III covers three areas of function associated with SCI, including self-care (subscore 0–20), respiration and sphincter management (subscore 0–40), and mobility (subscore 0–40).7, 8 The tool has been previously translated into many languages (that is, Italian, Turkish, Brazilian Portuguese and Spanish) with subsequent assessments of its applicability.9, 10, 11, 12 To enable the utility of the tool for Thai health professionals, this study primarily aimed to translate the SCIM III into Thai (Th-SCIM III) and to assess the reliability of the tool. In addition, the study secondarily investigated the discriminative ability of the tool in patients with various degrees of lesion severity.
Materials and Methods
Subjects
The subjects were patients with SCI who were admitted to the rehabilitation ward of a tertiary rehabilitation center in Thailand, with an age at least 18 years. The inclusion criteria were SCI from a traumatic cause or nonprogressive disease, both complete and incomplete lesions (as determined using the criteria from the American Spinal Injury Association Impairment Scale (AIS)), and at a subacute or chronic stage of injury. The patients were excluded if they had any problems affecting their ability to perform daily activities, such as pain at rest or with movement with a pain score of more than 5 out of 10 on a visual analog scale, or other deformities that affected movements (Table 1). According to sample-size estimation for the primary objective, the study required 30 subjects.13 Before participation, subjects signed an informed consent document approved by the Office of the Khon Kaen University Ethics Committee in Human Research (HE541320).
Research protocols
The study contained two phases: (1) translation and adaptation of the tool; and (2) data collection. Details of each phase are as follows.
Translation and adaptation phase
The Th-SCIM III was translated through the method of forward and backward translation by native speakers in both languages who were not familiar with the tool.10 First, the SCIM III was translated from English to Thai by a Thai physical therapist who was fluent in English. It was then translated back into English by a native English speaker who had more than 20 years experience in Thai but was not familiar with the SCIM III. Next, the original and backward-translated versions were reviewed and compared by another native English speaker who worked in the area of biomedical sciences, but who was not familiar with the tool. Finally, the tool was refined before being used for data collection (see Appendix).
Data-collection phase
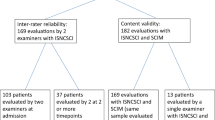
Subjects were interviewed and assessed for their demographics (including age, gender, weight and height) and SCI characteristics (including cause, stage, level and severity of SCI).14 They were then concurrently assessed for overall aspects relating to SCI using the Th-SCIM III by three physical therapists who had good clinical experience with SCI patients during the first week after admission.
Data analysis
Descriptive statistics were applied to explain the demographics and SCI characteristics of the subjects, as well as the findings of the study. The inter-rater reliability of the Th-SCIM III was analyzed using the intraclass correlation coefficient (ICC). An ICC of more than 0.75 was regarded as good reliability, between 0.5 and 0.75 was regarded as moderate reliability, and less than 0.5 referred to poor reliability.15 The internal consistency was assessed using Cronbach’s alpha coefficients. The discriminative ability of the tool was analyzed using one-way analysis of variance. The receiver-operating characteristic curves were used to explore an optimal cutoff score, sensitivity, specificity and area under the receiver-operating characteristic curve (AUC) to discriminate the performance of subjects with motor complete and incomplete SCI.16 The level of significant differences was set at P<0.05.
Results
Subject characteristics
Thirty-one subjects with SCI participated in the study. Fifteen had motor complete SCI (AIS A and B) and the other 16 had motor incomplete SCI (AIS C=8 and AIS D=8; Table 1). Most of the subjects were males (n=20) at a chronic stage of injury (average post-injury time=42.32±53.58 months) and most had paraplegia (n=22). All subjects with motor complete SCI and four of those with AIS C were wheelchair bound, another subject walked with a standard walker and a personal assistant, and the other three subjects were able to walk with a standard walker over a short distance (<100 m). For those with AIS D, most (n=6) could walk independently without any assistance or walking devices (Table 1).
Inter-rater reliability
The tool demonstrated excellent inter-rater reliability both when analyzed for overall items and separately for each subscale, and for subjects with both motor complete and motor incomplete SCI (ICC>0.90; Table 2).
Internal consistency
The Cronbach’s alpha coefficients for all items were >0.80 for all raters (Table 3). However, when analyzed for subscales, the Cronbach’s alpha values ranged from 0.50 to 0.94, with the lowest values for respiration and sphincter management (Table 3).
Discriminative ability
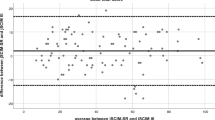
Subjects with AIS D had the highest Th-SCIM III scores, followed by those with AIS C, and AIS A and B, respectively (Table 4). The scores of subjects with AIS D also showed significant differences from the other groups, both when analyzed for all items and separately for each subscale, except for self-care activities. In contrast, the scores for those with AIS C were not significantly different from those with motor complete lesions (Table 4). The receiver-operating characteristic analysis demonstrated that Th-SCIM III scores of 50 and over could discriminate between subjects with motor complete and incomplete SCI (sensitivity 68.75%, specificity 66.67%, AUC=0.78, 95% confidence interval=0.62–0.95).
Discussion
The Th-SCIM III was translated and then assessed its reliability and discriminative ability among 31 subjects with motor complete and incomplete SCI. The findings showed that the tool had excellent inter-rater reliability and good internal consistency, and could significantly discriminate performance of subjects with different SCI severity (Tables 2, 3, 4). However, when analyzed for individual subscales, the scores for respiration and sphincter management had poor internal consistency (Table 3), and the scores for self-care activities were unable to discriminate performance of subjects with different degrees of lesion severity (Table 4).
Previously, the SCIM III has been translated into various languages, such as Brazilian Portuguese, Italian, Spanish and Turkish. Each version demonstrated high inter-rater reliability (ICC range 0.72–0.97), acceptable to good internal consistency (Cronbach’s alpha coefficients >0.70).9, 10, 11, 12 In addition, the tool has shown high reliability when used by health professionals with different levels of experience and backgrounds, that is, physicians, nurses, physical therapists and occupational therapists.11 Except for the respiration and sphincter management subscale, the poor internal consistency may imply that the items in this subscale (that is, respiration, sphincter management for bladder and bowel and toileting) are weakly correlated to each other. In addition, the raters in the current study were physical therapists, which may have difficulties assessing bladder and bowel management that subsequently reduces internal consistency of the items.
To investigate the discriminative ability of the tool, subjects were categorized into groups according to the standard criteria of AIS classification. Subjects with AIS A and B (motor complete SCI) were those who did not have any motor function below the level of the lesion. In contrast, subjects with AIS C and D (motor incomplete SCI) were those who had partially preserved motor functions below the level of injury at nonfunctional and functional grades, respectively.14 The data of Th-SCIM III demonstrated that subjects with motor incomplete SCI, particularly those with AIS D, had scores higher than those with motor complete SCI (Table 4). The findings were in accordance with those reported previously.9 However, subjects with AIS C had rather low functional ability, with four of them wheelchair bound and one walked nonfunctionally (that is, could walk only a short distance with a standard walker and a personal assistant). Thus, the Th-SCIM scores that are normally used to measure the function, not impairments, showed no significant differences between subjects with AIS A and B, and C who were similarly lack functional movements below the neurological levels (Table 4). Such characteristics may also interfere with the discriminative ability of the scores for subjects with motor complete and incomplete SCI (sensitivity 68.75%, specificity 66.67%, AUC=0.78, 95% confidence interval=0.62–0.95).
Findings of the current study suggest the utility of the translated tool (Th-SCIM III) for Thai health professionals. However, the findings contain some limitations. First, the number of subjects was estimated according to the primary objective (reliability test),13 and subjects in each AIS class had various levels of the lesion. Second, all raters were physical therapists and the scores of some items (bathing, dressing, and bowel and bladder management) were not directly observed; but derived from interviewing the subjects. However, the researchers attempted to minimize errors of the information given by the confirmation with their caregivers, and medical and nursing records. Riberto et al.11 reported that the SCIM III can be used by health professionals with different levels of experience and different backgrounds. The scores can be obtained by an interview or by direct observation of the subject while he or she performs the tasks.11 The researchers in the present study believe that further studies with a larger number of subjects with various degrees of lesion severity and levels of the lesion, or multicenter trials, as well as exploration of other psychometric properties (that is, intra-rater reliability, discriminative ability in subjects with different levels of the lesion, smallest real difference and s.e. of measurement) may fulfill the utility of the Th-SCIM III in clinical practice.
Conclusion
Findings of this study support the use of the Th-SCIM III to assess daily functions of patients with SCI. Therefore, these findings may be useful for Thai health professionals who are not fluent in English. However, further research is needed to confirm the clinical implications of this tool.
Data Archiving
There were no data to deposit.
References
van den Berg-Emons RJ, Bussmann JB, Haisma JA, Sluis TA, van der Woude LH, Bergen MP et al. A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch Phys Med Rehabil 2008; 89: 2094–2101.
Haisma JA, Bussmann JB, Stam HJ, Sluis TA, Bergen MP, Dallmeijer AJ et al. Changes in physical capacity during and after inpatient rehabilitation in subjects with a spinal cord injury. Arch Phys Med Rehabil 2006; 87: 741–748.
Wirth B, van Hedel H, Kometer B, Dietz V, Curt A . Changes in activity after a complete spinal cord injury as measured by the spinal cord independence measure II (SCIM II). Neurorehabil Neural Repair 2008; 22: 145–153.
Cardenas DD, Hoffman JM, Kirshblum S, McKinley W . Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil 2004; 85: 1757–1763.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A . SCIM-spinal cord independence measure: a new disability scale for patients with spinal cord lesions. Spinal Cord 1997; 35: 850–856.
Catz A, Itzkovich M, Steinberg F, Philo O, Ring H, Ronen J et al. The Catz-Itzkovich SCIM: a revised version of the Spinal Cord Independence Measure. Disabil Rehabil 2001; 23: 263–268.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multicenter international study on the Spinal Cord Independence Measure, version III: Rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil 2007; 29: 1926–1933.
Invernizzi M, Carda S, Milani P, Mattana F, Fletzer D, Iolascon G et al. Development and validation of the Italian version of the Spinal Cord Independence Measure III. Disabil Rehabil 2010; 32: 1194–1203.
Kesiktas N, Paker N, Bugdayci D, Sencan S, Karan A, Muslumanoglu L . Turkish adaptation of Spinal Cord Independence Measure-version III. Int J Rehabil Res 2012; 35: 88–91.
Riberto M, Tavares DA, Rimoli JR, Castineira CP, Dias RV, Franzoi AC et al. Validation of the Brazilian version of the Spinal Cord Independence Measure III. Arq Neuropsiquiatr 2014; 72: 439–444.
Zarco-Perinan MJ, Barrera-Chacon MJ, Garcia-Obrero I, Mendez-Ferrer JB, Alarcon LE, Echevarria-Ruiz de Vargas C . Development of the Spanish version of the Spinal Cord Independence Measure version III: cross-cultural adaptation and reliability and validity study. Disabil Rehabil 2014; 36: 1644–1651.
Morrow JR, Jackson AW . How "significant" is your reliability? Res Q Exerc Sport 1993; 64: 352–355.
Maynard FM Jr, Bracken MB, Creasey G, Ditunno JF Jr, Donovan WH, Ducker TB et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Portney LG, Watkins MP . Fountations of Clinical Research: Applications to Practice. Prentice Hall: Upper Saddle River, NJ, USA. 2009.
Akobeng AK . Understanding diagnostic tests 3: receiver operating characteristic curves. Acta Paediatr 2007; 96: 644–647.
Acknowledgements
This study was supported by the Improvement of Physical Performance and Quality of Life (IPQ) research groups at Khon Kaen University. The researchers thank Mr Ian Thomas and Dr Jeffrey Roy Johns for their help in translation of the tool.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Appendix
Appendix




Rights and permissions
About this article
Cite this article
Wannapakhe, J., Saensook, W., Keawjoho, C. et al. Reliability and discriminative ability of the spinal cord independence measure III (Thai version). Spinal Cord 54, 213–220 (2016). https://doi.org/10.1038/sc.2015.114
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.114
This article is cited by
-
Reliability and concurrent validity of the Spinal Cord Independence Measure III among rehabilitation professionals
Spinal Cord (2022)
-
Test-retest reliability and validity of the Sitting Balance Measure-Korean in individuals with incomplete spinal cord injury
Spinal Cord (2022)
-
Validation of the Thai version of the Spinal Cord Independence Measure Self-Report (SCIM-SR-Thai)
Spinal Cord (2022)
-
Cross-cultural adaptation and psychometric testing of the Thai version of the Spinal Cord Independence Measure III—Self Report
Spinal Cord (2021)
-
Development of Persian version of the Spinal Cord Independence Measure III assessed by interview: a psychometric study
Spinal Cord (2018)