Abstract
Study design:
This study is a cross-sectional, face-to-face interview.
Objectives:
To examine the sexual activity in a sample of Malaysian women with traumatic spinal cord injuries (SCIs), identify the physical and psychological barriers to it, and explore their experiences with sexual counseling and rehabilitation.
Setting:
This study was conducted at the Spinal Rehabilitation Unit of a teaching hospital.
Methods:
All women who attended scheduled check-ups, over 1 year, and who met the inclusion criteria (age above 18 years, spinal injury of traumatic aetiology, living in the community and having completed the rehabilitation) were consecutively included in a face-to-face interview using a self-constructed questionnaire. Sociodemographic and disability-related variables, barriers to sexual activity/satisfaction and experiences of sexual rehabilitation services were obtained.
Results:
During the study period, 33/36 subjects were recruited. Although 67% indicated interest in sexual activity, only 24% was sexually active. The frequency of sexual activity declined after the injury, from 4.6 times per month to 1.5 times per month. Feeling unattractive, unable to satisfy the partner and less confident about sexual ability were top three psychological barriers to sexual activity, and the top three physical barriers were impaired genital sensation, positioning and vaginal lubrication. In all, 50% received some sexual information during rehabilitation. Rehabilitation professionals were expected to initiate sexual counseling by 62.5% of subjects.
Conclusion:
The effect of SCIs on sexual function is tremendous. Sexual counseling services must be improved and take into account the impact of psychological factors.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) gives rise to multiple comorbidities, not only affecting one's physical and physiological functions, but also causing detrimental psychological consequences and sexual dysfunction.1, 2, 3 The extent of sexual dysfunction is influenced by the severity of the neurological lesion, the presence of bladder and bowel incontinence, pain and spasticity, as well as difficulties with interpersonal and social relationships.4
Sexuality issues in females with SCI have not received as much attention as their male counterparts, likely because women traditionally have a passive role in sexual intercourse and because their fertility is not affected.5, 6 Studies have shown that 65 to 80% of such women continue to be sexually active after the injury but with reduced frequency and lower sexual satisfaction.7, 8, 9, 10, 11 Women with SCI consistently express their dissatisfaction with the quality of sexual rehabilitation services during their therapy,5, 8, 9, 10 which is poor, fragmented and male oriented.9, 10
There is sparse literature on sexuality and disabilities involving Asian women; in fact, no such reports exist in Malaysia. A qualitative study of Chinese women with spinal cord impairments in Hong Kong10 concluded that they were inclined to have negative attitudes toward their sexuality. Although Indian women with SCI have near-normal sexual function, they frequently experience sexual problems and concerns over living with a disability.9
How sexuality is perceived and practised by the disabled population in Malaysia has never been examined. The aim of this study was to identify physical and psychological barriers to sexual activity in women with traumatic spinal cord injuries, and to explore their experiences with sexual counselling and rehabilitation.
Subjects and methods
The subjects were women with traumatic SCIs who were attending the Spinal Rehabilitation Clinic of a tertiary hospital. Those who attended scheduled check-ups, over 1 year, and who met the inclusion criteria (age above 18 years, living in the community and completing rehabilitation) were consecutively included. The exclusion criteria were known recovery and concurrent traumatic brain injury and psychiatric illness.
One to one interview was carried out by a female doctor (SO Aiza) in the Spinal Rehabilitation Unit. The questionnaire consisted of sociodemographic and disability-related variables, 15 factors that might have interfered with their sexual activity or satisfaction in the last 4 weeks, and questions pertaining to sexual information and counselling.
The subjects were notified of the purpose of the study and were assured confidentiality of their data. Written consent was obtained from all subjects. This study was approved by the medical ethics committee of the University Malaya Medical Centre.
Results
In all, 33 subjects with traumatic SCIs were interviewed. Their backgrounds and clinical characteristics are listed in Tables 1 and 2. A total of 67% indicated they remained interested in sexual activity after the injury. Although 40% had sexual activity after the injury, only 24% was involved in a sexual relationship at the time of the study. For five subjects, sexual activity had ceased. Of those who were engaged in sexual activity, 38% had sex within 6 months after the injury, 15% had between 6 months and 2 years, and the remaining 47% had at more than 2 years after the injury. The frequency of intercourse after SCI declined from an average of 4.6 times per month to 1.5 times per month. The problems that were experienced during sexual intercourse are shown in Table 3.
In all, 6 of the 33 subjects confided their sexual issues in others, of whom four discussed their sexual problems with their doctors. The three most frequent reasons for not discussing were: (1) sex is not important anymore (46%), (2) embarrassment (36%) and (3) it is acceptable to have these problems following SCI (21%). We also gathered subjects’ opinions on the most appropriate time for sexual counselling. A total of 52% preferred to receive information between 6 months and at 2 years after the injury, 31% preferred it within 6 months and 17% wanted it at more than 2 years after the injury.
Some sexual information was given to 53% of the subjects. At the time of the study, 70% wished to receive sexual information during their rehabilitation. In terms of content, most (78%) would have liked to have received information on the effects of SCIs on sexual function, followed by pregnancy and labour issues (74%), fertility (70%) and managing bladder and bowel functions for sexual activity (70%). A total of 62% of subjects expected rehabilitation clinicians to initiate and offer sexual counselling. A total of 56% stated that talking to someone who had similar experiences would be helpful.
Discussion
The percentage of women with SCIs who were sexually active in this sample was much lower compared with previous studies,7, 8, 9, 12 but we do not know whether this difference is germane to the Asian population because similar reports are scarce. Although an Indian study population observed a higher percentage, only 40 of 117 eligible respondents volunteered to participate. In contrast to Kreuter et al.,8 in which half of the sample had sex within 6 months, half of our sample first had sex at more than 2 years after the injury. We did not explore the reason for this delay, which might have been because of the reduced desire, medical condition, cultural beliefs or the availability of sexual partners.
The decline in the frequency of sexual activity from 4.6 to 1.5 times per month in our study is consistent with other studies.7, 8, 12, 13 The physical barrier that interfered most with their sexual activity was reduced genital sensation. Indeed, decreased or lack of genital sensitivity is associated with reduced sexual desire and activity.1, 7, 8, 10
Sexual positioning was also noted as a barrier to sexual activity. Difficulties in achieving or maintaining the desired position, both during foreplay and sexual intercourse, can be attributed to muscle weakness and spasticity.1, 7, 8, 10 Apart from these barriers, inadequate vaginal lubrication also interfered with sexual activity in one-third of our sample, compared with 65.5% in a study by Anderson et al.11 Our results might fail to reflect the true extent of this problem, because it is based on patient recall and, further, most of our participants had reduced genital sensation, which is important for one's awareness of vaginal lubrication.
It is notable that few subjects reported urinary and bowel incontinence as barriers to sexual activity, as both dysfunctions are significant physical problems and have negative impact on self-image and sexual adjustment.2, 8, 11, 12 It is possible that subjects who were sexually active in our sample had learned how to manage their incontinence, explaining the low frequency reported.
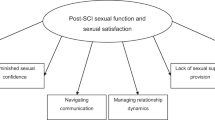
Psychological factors have been shown to limit sexual activity more than physical impairments.1, 2, 3, 8, 11 This is evident from our findings, whereby the frequency of psychological factors identified as barriers to sexual activity exceeded that of physical factors. The women in our study perceived themselves to be less attractive, less confident of themselves, feeling dependant and have a concern over satisfying their partners, and these are consistent with earlier studies.1, 9, 10, 13 At the same time, however, it should be noted that satisfying one's sexual partner can have slightly different meanings among Asians.
The Malaysian population comprises of multiethnic groups and there is tremendous heterogeneity in social and cultural norms. Having sex with an ill or a physically challenged woman might be against such norms, thus, prompting some women to give false accounts of their sexual activity, deny aspects of their lives that they regard as unacceptable or reply in a manner that is considered socially desirable.9 There is a patent need to understand the deeper meanings of sexuality and its expectations among physically challenged women and their partners in diverse cultural backgrounds.
The majority of the sample desired to receive more information on sexually related matters, such as fertility, pregnancy and labour issues, which are deemed important in the Asian population, as women are expected to reproduce, particularly in a conservative society. Pamphlets containing information on reproductive matters is important in helping these women cope with their sexual health.
There is no specific time after the injury that is most appropriate for initiating sexual counselling. As one is still trying to accept their disability, physical recovery is thus a priority in the initial stage. It was felt that the appropriate time for sexual counselling was after discharge, between 6 months and at 2 years after the injury when they are then aware and have to deal with their sexual problems. Thus, initial counselling should include an understanding of the consequences of a SCI and its effects on sexual functioning. Subsequently, after engaging in sexual activity, solutions to their sexual-related problems are warranted for those who face obstacles. Therefore, healthcare professionals need to consider sexual rehabilitation in dealing with disabilities, such as SCI.
A support group was also deemed necessary as a coping strategy. Women who ‘were getting on with their lives’ were considered welcome role models,5 as they are able to offer invaluable practical tips and strategies in their daily activities and not merely on sexual issues. It was also less embarrassing to discuss intimate subjects with another woman who had experienced the same problems.5, 10
This study is not without its limitations. One has to be cautious in interpreting the findings as the sample size is small. Nevertheless, we present novel information with regards to improving sexual rehabilitation services to women with SCIs. The study needs to be replicated on a wider scale to determine its generalisability to a wider population and help us understand the influence of psychosocial determinants in sexual health outcomes.
Further, the tremendous heterogeneity in multiethnic societies in Malaysia requires us to acknowledge that each culture may view sexual needs differently. Subsequent studies should examine culture and sexuality among the physically challenged community in our society.
Conclusion
Fewer than half of the women with SCI in this study led active sexual lives after sustaining an SCI. It is evident that an individual's psychological well-being has a significant affect on sexual activity. Future research is warranted to expand and update the current knowledge base in this area, particularly with regard to our understanding of the influence of psychosocial determinants in the sexual rehabilitation outcomes for women with SCIs.
References
Kreuter M, Taft C, Siösteen A, Biering-Sørensen F . Women's sexual functioning and sex life after spinal cord injury. Spinal Cord 2010; 48: 1–7.
Anderson KD, Borosoff JF, Johnson RD, Stiens SA, Elliott SL . The impact of spinal cord injury on sexual function: concerns of the general population. Spinal Cord 2007; 45: 328–337.
Samuel VM, Moses J, North N, Smith H, Thorne K . Spinal cord injury rehabilitation: the experience of women. Spinal Cord 2007; 45: 758–764.
Lombardi G, Del Popolo G, Mencarini M, Celso M . Sexual rehabilitation in women with spinal cord injury: a critical review of literature. Spinal Cord 2010; 48: 1–8.
Forsythe E, Horsewell JE . Sexual rehabilitation of women with a spinal cord injury. Spinal Cord 2006; 44: 234–241.
Charlifue SW, Gehart KA, Menter RR, Whitenack CG, Manley MJ . Sexual issues of women with spinal cord injuries. Paraplegia 1992; 30: 192–199.
Ferreiro-Velasco ME, Barca-Buyo A, Salvador de la Barrera S, Montoto-Marques A, Miguens Vazquez X, Rodriguez-Sotillo A . Sexual issues in a sample of women with spinal cord injury. Spinal Cord 2005; 43: 51–55.
Kreuter M, Siosteen A, Biering-Sorensen F . Sexuality and sexual life in women with spinal cord injury: a controlled study. J Rehabil Med 2008; 40: 61–69.
Roop S, Sharma SC . Sexuality and women with spinal cord injury. Sex Disabil 2005; 23: 21–33.
Li CM, Yau MK . Sexual issues and concerns: tales of Chinese women with spinal cord impairments. Sex Disabil 2006; 24: 1–26.
Anderson KD, Borisoff JF, Johnson RD, Steins SA, Elliott SL . Spinal cord injury influences psychogenic as well as physical components of female sexual ability. Spinal Cord 2006; 45: 1–11.
Jackson AB, Wadley V . A multicenter study of women's self-reported reproductive health after spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1420–1428.
Fisher TL, Laud PW, Byfield MG, Brown TT, Hayat MJ, Fiedler IG . Sexual health after spinal cord injury: a longitudinal study. Arch Phys Med Rehabil 2002; 83: 1043–1051.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Julia, P., Othman, A. Barriers to sexual activity: counselling spinal cord injured women in Malaysia. Spinal Cord 49, 791–794 (2011). https://doi.org/10.1038/sc.2011.4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.4
Keywords
This article is cited by
-
Sexuality Support After Spinal Cord Injury: What is Provided in Australian Practice Settings?
Sexuality and Disability (2022)
-
Sexuality After Spinal Cord Injury. Which Factors Influence Sexual Activity and Satisfaction?
Sexuality and Disability (2022)
-
The Sexual Health Needs of Women with Spinal Cord Injury: A Qualitative Study
Sexuality and Disability (2017)
-
Sexual satisfaction in women with spinal cord injuries
Spinal Cord (2015)
-
Sexual activity and sexual satisfaction in Korean men with spinal cord injury
Spinal Cord (2015)