Abstract
Neoantigens are tumour-specific antigens that arise from non-synonymous mutations in tumour cells. However, their effect on immune responses in the tumour microenvironment remains unclear in breast cancer. We performed whole exome and RNA sequencing of 31 fresh breast cancer tissues and neoantigen prediction from non-synonymous single nucleotide variants (nsSNVs) among exonic mutations. Neoantigen profiles were determined by predictive HLA binding affinity (IC50 < 500 nM) and mRNA expression with a read count of ≥ 1. We evaluated the association between neoantigen load and expression levels of immune-related genes. Moreover, using primary tumour cells established from pleural fluid of a breast cancer patient with carcinomatous pleurisy, we induced cytotoxic T lymphocytes (CTLs) by coculturing neoantigen peptide-pulsed dendritic cells (DCs) with autologous peripheral lymphocytes. The functions of CTLs were examined by cytotoxicity and IFN-γ ELISpot assays. Neoantigen load ranged from 6 to 440 (mean, 95) and was positively correlated to the total number of nsSNVs. Although no associations between neoantigen load and mRNA expression of T cell markers were observed, the coculture of neoantigen-pulsed DCs and lymphocytes successfully induced CTLs ex vivo. These results suggest that neoantigen analysis may have utility in developing strategies to elicit T cell responses.
Similar content being viewed by others
Introduction
Treatment of breast cancer has advanced significantly in recent decades because of the development of new drug therapies1,2. However, many breast cancer patients still die, especially from drug resistance3,4. Therefore, the development of new therapeutic strategies for breast cancer is critical.
Recently, immune checkpoint inhibitors (ICIs) have shown anti-tumour efficacy in many cancer types5,6,7. Although the response rate to ICIs is limited and ICIs have been associated with immune-related adverse events, the response to ICIs is sometimes durable8,9. Notably, the existence of tumour antigen-specific T lymphocytes is an important factor for ICIs to be effective10,11. Among tumour antigens, peptides that contain amino acid substitutions caused by somatic non-synonymous mutations in tumour cells, but not in non-tumour cells, are called neoantigens.
A high number of neoantigens is expected to elicit a strong immune reaction in the tumour microenvironment. A recent study of multiple cancer types including breast cancer showed that increased numbers of neoantigens are associated with higher CD8A expression12. Another study showed that the number of neoantigens has a positive correlation to cytolytic activity in breast cancer, which is based on transcription levels of GZMA and PRF113. Conversely, other studies have shown a negative effect of high neoantigen load on the immune response in breast cancer14,15. Therefore, the effect of neoantigen burden on the immune response in breast cancer remains controversial.
Current research has focused on developing treatments that target neoantigens16,17. A recent study has reported the remarkable effect of adaptive transfer of neoantigen-specific T cells in a hormone-positive metastatic breast cancer patient18. Another study has demonstrated that neoantigens induce anti-tumour immunity in xenograft models19. However, studies on the therapeutic application of neoantigens in breast cancer remain limited and further evidence is required.
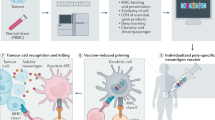
In the current study, we performed neoantigen profiling of fresh tumour tissues from 31 breast cancer patients and examined the correlation between neoantigen load and the immune environment in breast cancer. We also examined whether dendritic cells (DCs) pulsed with in silico-predicted neoantigen peptides induce tumour-specific T lymphocytes in an ex vivo model.
Results
Mutational landscape of breast cancer patients
To perform neoantigen prediction, we first detected tumour-specific gene mutations by whole exome sequencing of 31 fresh breast cancer tissues and paired samples of peripheral blood mononuclear cells (PBMCs). The clinical characteristics of the 31 breast cancer patients are shown in Table 1. We performed neoantigen prediction only on nsSNVs among exonic mutations. A total of 1976 nsSNV mutations were found in the samples from the 31 patients and nsSNVs accounted for approximately 62.4% of the total exonic mutations (Fig. 1a), which showed a strong linear correlation with total exonic mutations (r = 0.99, p < 0.0001, Fig. 1b). The top three most frequent genes with nsSNVs were TP53 (13 cases), PIK3CA (5 cases), and TTN (5 cases), and five identical paired nsSNVs (AKT1, ARAP3, NOTCH3, PIK3CA, and SLC35E2) were identified (Table 2).
Exonic mutation landscape in breast cancer determined by whole exome sequencing of tumour tissues and peripheral blood mononuclear cells. (a) The numbers of total exonic mutations and mutation types in the 31 breast cancer patients. (b) The number of total exonic mutations was highly correlated to the number of nsSNVs. INDEL: insertion/deletion; sSNV: synonymous single nucleotide variant; nsSNV nonsynonymous single nucleotide variant.
Neoantigen landscape of breast cancer patients
We created neoantigen profiles by predicting the binding affinity of possible 8–11mer amino acid sequences generated by each nsSNV to patient-specific HLA class I molecules. The number of neoantigen peptides with a binding affinity of IC50 < 500 nM ranged from 9 to 834 (mean, 192), which showed a linear correlation to the number of nsSNVs (r = 0.78, p < 0.0001, Fig. 2a). By considering the importance of endogenous neoantigen peptides to elicit immune reactions in vivo, we added the mRNA read count, which covered the mutated site, to these criteria with a read count of ≥ 1. We refer to the number of neoantigens detected by these criteria as “neoantigen load.” The neoantigen load ranged from 6 to 440 (mean, 95) and showed a high linear correlation to the number of nsSNVs (r = 0.725, p < 0.0001, Fig. 2b). The neoantigen load was significantly higher in TNBC cases (n = 13; median = 150, range: 9–440) than in non-TNBC cases (n = 18; median = 51, range: 6–196) (p < 0.05, Fig. 2c).
Neoantigen landscape in breast cancer determined by a computational HLA class I-binding assay and RNA sequencing. (a) The number of predicted neoantigens (IC50 < 500 nM) was highly correlated to the number of nsSNVs (r = 0.78, p < 0.0001). (b) The number of predicted neoantigens (IC50 < 500 nM, read count ≥ 1) was highly correlated to the number of nsSNVs (r = 0.72, p < 0.0001). (c) The number of predicted neoantigens (IC50 < 500 nM, read count ≥ 1) in TNBC was statistically higher than that in non-TNBC. TNBC: triple negative breast cancer.
Association between the number of neoantigen peptides and immune-related gene expression
To investigate the effect of neoantigen load on the immune environment in breast cancer, the expression of immune-related genes was analysed by RNA-seq using the same sample that had been subjected to neoantigen analysis. There was no significant association between mRNA expression levels of T cell markers CD8a, CD4, and TCRB and the total number of nsSNVs and neoantigen load (Additional file 1). Expression levels of GZMA, GZMB and PRF1, which encode T cell activation markers, also did not show significant correlations (Additional file 1).
Induction of CTLs by synthesized neoantigen peptides
Neoantigen profiles can be applied to therapeutic applications such as cancer vaccines. Therefore, we examined whether CTLs were induced by coculturing lymphocytes with autologous DCs pulsed with the predicted neoantigen peptides. First, we performed neoantigen analysis of primary tumour cells established from pleural fluid of a TNBC patient with carcinomatous pleurisy. We synthesized 10 mutant peptides from the neoantigen profiles, which showed high affinity for HLA-A02:06 and mRNA expression with a read count of ≥ 2 (Table 3). We also synthesized a wildtype peptide as a control. After coculturing autologous peripheral lymphocytes with synthesized peptide-pulsed mDCs for 48 h, we quantified IFNγ-producing lymphocytes by an ELISpot assay. Although the results did not show statistical significance, lymphocytes pulsed with two peptides (peptides 3 and 9) showed a > 50% higher response compared with the control without peptide pulsation (Fig. 3a). We performed the same experiments using various concentrations of the two peptides and confirmed that the IFNγ-producing reaction was increased in a concentration-dependent manner (Fig. 3b). Therefore, we speculated that naïve T lymphocytes capable of reacting with peptides 3 and 9 were already present among peripheral lymphocytes. We next cultured peripheral lymphocytes with mDCs pulsed with these two peptides under low concentrations of recombinant human IL-2 for 4 weeks to induce CTLs. CTLs generated by coculture with peptide 9-pulsed mDCs showed significantly higher cytotoxicity than the wildtype peptide control in a calcein releasing assay (p < 0.01, Fig. 3c). The same CTLs also showed a significantly higher IFNγ-producing ability against the autologous tumour cells than the wildtype control (p < 0.05, Fig. 3d).
Response of cytotoxic T lymphocytes stimulated by neoantigen peptide-pulsed mature dendritic cells (mDCs). (a) IFN-γ ELISpot response of peripheral blood lymphocytes stimulated by neoantigen peptide-pulsed mDCs. The final concentration of peptide was 50 µg/ml. The mean number of IFN-γ ELISpots ± SEM is shown (n = 2). (b) Dose-dependent increase in the IFN-γ ELISpot response of peripheral blood lymphocytes stimulated by peptide 3- or 9-pulsed mDCs. The final concentrations of peptides were 5, 50, and 100 µg/ml. The mean number of IFN-γ ELISpots ± SEM is shown (n = 2). (c) Cytotoxicity assay of CTLs induced by 4 weeks of coculture with neoantigen-pulsed mDCs. Numbers of calcein-positive living tumour cells were significantly decreased by co-culture with CTLs stimulated with peptide 9-pulsed DCs. The mean % of cytotoxicity ± SEM is shown (n = 3–5). (d) IFNγ-release responses by peptide 9-pulsed mDC stimulated with CTLs against autologous tumour cells. Ly: lymphocyte; mDC, mature dendritic cell; TC, tumour cell; CTL/P9, CTLs induced by peptide 9-pulsed DCs; CTL/WT, CTLs induced by wildtype peptide-pulsed DCs. The mean number of IFN-γ ELISpot ± SEM. is shown (n = 2–3).
Discussion
We conducted neoantigen profiling of 31 breast cancers using an in silico prediction pipeline and analysed the correlation of neoantigen load with immune-related gene expression. We also performed ex vivo CTL induction experiments using TNBC patient-derived primary tumour cells and autologous PBMCs along with the predicted neoantigen peptides. In this study, we obtained the following findings: (1) the neoantigen profiles were highly unique among individuals; (2) neoantigen load showed a linear correlation with the total number of nsSNVs; (3) neoantigen load was not correlated to immune-related gene expression; (4) DCs pulsed with synthetic peptides predicted from our neoantigen analysis successfully induced CTLs ex vivo.
In silico neoantigen prediction analysis has recently been widely performed for many cancers, which is considered to be a potentially useful tool for clinical parameters and immunotherapies20,21. Previous studies have shown that 8–11mer peptides with a high affinity for HLA-class I elicit CD8 + CTLs that are the most effective cells to eliminate cancer22. Here, we performed neoantigen profiling of 31 breast cancer specimens based on the binding affinity of possible 8–11mer peptides, which harboured substituted amino acids altered by nsSNVs, to HLA class I molecules and mRNA expression levels of mutated genes. We succeeded in detecting neoantigens in all cases, which indicated good feasibility of neoantigen analysis in breast cancer regardless of the specimen site. Among the 1976 nsSNVs detected in the 31 cases, five pairs of identical nsSNVs were observed. Of these five genes, only AKT1 in both BC1 and BC14 remained as neoantigen candidates. Although frequently mutated genes such as TP53, PIK3CA, and TTN were found, there was only one pair of identical nsSNVs in PIK3CA. Accordingly, among the 1976 nsSNVs, only a pair of AKT1 remained as an identical neoantigen candidate. This result is consistent with a previous report showing that the majority of neoantigens are specific to the individual23. Considering that most neoantigens are derived from nsSNVs, the set of neoantigens in each patient varies greatly. This result indicates that neoantigen profiling may be important in developing highly personalized therapies.
Although there are no common criteria to predict neoantigens, a binding affinity of IC50 < 500 nM to HLA molecules is widely used24,25. In this study, we used two criteria: binding affinity of IC50 < 500 nM and RNA-seq data with one or more read counts that contained the mutated position. Although the RNA level required to elicit a T cell reaction is unclear, a study has shown that a single peptide-MHC complex induces cytotoxic T cells, which indicates that a very low expression level may be sufficient for T cell activation26. Therefore, we consider that even only one read count of RNA-seq can be a marker for a neoantigen peptide to elicit a T cell response. In this study, we referred to the number of neoantigen peptides predicted by not only the binding affinity to HLA class I molecules, but also RNA expression as “neoantigen load”. Both neoantigen load and the numbers of neoantigens predicted only by binding affinity to HLA class I molecules were positively correlated to the total number of nsSNVs. This is consistent with previous TCGA-based neoantigen analyses of breast cancers15,24. This result suggests that tumour mutation burden (TMB) simply reflects an increased opportunity of gaining neoantigens and that TMB can be a surrogate marker for neoantigen load. In the analysis by subgroup, we found that the neoantigen load was higher in TNBC cases than non-TNBC cases, which was consistent with previous reports15,24. Although the mechanism underlying the higher neoantigen load in TNBC compared with non-TNBC has not been elucidated, a possible cause is that, compared with luminal type breast cancer, which has specific tumorigenic factors such as signalling pathways via hormone receptors, TNBC requires a higher rate of mutations to gain tumour-driving mutations.
In contrast to our expectation, neoantigen load did not show positive correlations with mRNA expression of T cell markers or activated T cell markers. Consistent with our results, another report revealed an inverse association between immune metagene expression and TMB or neoantigen load in TNBC and the HER2-positive type14. Another report also showed that a low TMB and neoantigen load were associated with high immune cell infiltration in TNBC15. Moreover, this trend has been reported in multiple tumour types27. One reason for the inability of a high neoantigen load to elicit immune-related gene expression may be the complexity of immunity in the tumour microenvironment, which includes multiple immune cell populations and cytokines28,29. Even if neoantigens are endogenously expressed and a immune response occurs, the existence of immune suppressive factors, such as regulatory T cells, myeloid derived suppressor cells, and immune suppressive cytokines, may counteract the immunogenicity of neoantigens. Another reason may be the neoantigen heterogeneity in breast cancers30,31. Several studies have demonstrated that tumour heterogeneity correlates with a reduced immune response15,32. Collectively, although neoantigens themselves induce immune responses, many other factors in the tumour microenvironment may cancel the immunogenicity of neoantigens.
The relationship between neoantigen load and tumour-infiltrating lymphocytes (TILs) is a very interesting research area33. However, in about half of the cases in the current study, we were unable to evaluate TILs because of the limited biopsy specimens that were available and prioritized them for neoantigen analysis. TIL evaluation of limited samples suggested no significant correlation between TILs and neoantigen load (data not shown). Consistent with this result, a recent study has shown no correlation between the number of nsSNVs and stromal TILs within each subtype of breast cancer34. We believe that the presence of neoantigen-specific TILs is more important than the number of TILs or neoantigen load and further analyses are required to address this issue.
In addition to the use of neoantigen profiles as a clinical immune parameter, there is great interest in their therapeutic use, such as for neoantigen vaccines and adaptive immunotherapy of neoantigen-specific CTLs16,17. Using autologous tumour cells, monocyte-derived DCs, peripheral lymphocytes, and synthetic neoantigen peptides, we were able to successfully induce CTLs ex vivo. Importantly, CTLs releasing IFN-γ against autologous tumour cells indicated that the neoepitope predicted by our pipeline was expressed on the surface of tumour cells in the context of HLA class I molecules. If the neoantigen elicits effective anti-tumour immune responses in the tumour microenvironment, the tumour should not grow in patients. As we stated above, because of several immune suppressive factors in the tumour microenvironment, a neoantigen may not be able to elicit an immune response. Eliciting an immune response against a tumour-specific neoantigen ex vivo, where we can eliminate immune suppressive factors by adoptive neoantigen-specific CTL therapy as an example, may be a useful strategy to enforce a neoantigen-specific response. Although we recognize the limitations of a single preclinical model, these results demonstrated the theoretical rationale for clinical application of neoantigen peptides.
Several limitations in this study should be stated. First, we predicted neoantigens only for each nonsynonymous SNV depending on the binding affinity for HLA class I. Because INDELs including gene fusions are reported to be good resources of highly immunogenic neoantigens35,36 and neoantigens with high affinity for HLA class II are reported to have an important role in the anti-tumour response37,38, these factors should be included in predicting neoantigens in future studies. Second, the proportion of tumour cells in the specimen probably affected the neoantigen load because a mutation was called for an mRNA read count relative to that of normal sequences. In the future, a neoantigen analysis system should be developed, which takes into account the tumour purity of specimens. Third, the number of specimens was small. Because breast cancers are reported to consist of multiple cancer subtypes39, a study should ideally be performed based on subtypes and a large number of specimens are needed for such analyses. Finally, we did not check whether the predicted neoantigen peptides were expressed on the tumour surface with MHC class I molecules and elicited specific CTLs in the tumour microenvironment. In pursuing the therapeutic application of neoantigen peptides, this may be an important direction to explore.
Conclusions
We performed neoantigen analysis of fresh tumour specimens from breast cancer patients. The neoantigen load was not positively correlated to immune-related gene expression. However, synthesized neoantigen peptide-pulsed DCs induced CTLs from peripheral lymphocytes ex vivo. Collectively, these results indicate that endogenous neoantigens in the tumour microenvironment of breast cancer may be insufficient to elicit an immune response in the tumour microenvironment. Therefore, inducing neoantigen-specific immune responses outside the tumour microenvironment by adoptive neoantigen-specific CTLs or neoantigen-pulsed DC vaccines may be alternative strategies to use neoantigen prediction analysis.
Methods
All methods in this study were approved by the Ethical Committees of Kyushu University Hospital (No. 128) and Fukuoka General Cancer Clinic (FGCC-EC001) based on the Act on Securement of Safety on Regenerative Medicine in Japan. This study complied with the Declaration of Helsinki and written informed consent was obtained from all patients.
Breast cancer patients and samples
This study included 31 patients with histologically confirmed breast cancer from Kyushu University and Fukuoka General Cancer Clinic. Fresh breast cancer specimens were obtained immediately after biopsies or tumour resection and placed in microtubes that contained the RNA stabilization solution RNAlater (Thermo Fisher Scientific Inc., Tokyo, Japan). PBMCs were obtained by leukapheresis procedure using Haemonetics CCS (Haemonetics, MA, USA) in accordance with the manufacturer’s instructions. The leukapheresis product was diluted with RPMI-1640 medium (Kojin-Bio Inc., Saitama, Japan) for density gradient isolation on Ficoll-Hypaque. After isolation, the cells were washed three times with RPMI-1640 medium and the obtained PBMCs were cryopreserved at − 80 °C. Tumour specimens and PBMCs were obtained at various time points from patients after diagnosis (as shown in Table 1).
Establishment of primary breast cancer cells from a patient with chemo-refractory metastatic triple negative breast cancer (TNBC)
Pleural fluid associated with carcinomatous pleurisy and PBMCs were obtained from a 33-year-old woman with chemo-refractory TNBC, who was diagnosed and treated at Kyushu University. Cytology of the pleural fluid revealed numerous tumour cells. The cells were first cultured in DMEM/F12 (Life Technologies, Grand Island, NY, USA). After formation of colonies, they were cultured in DMEM/F12 supplemented with 10% fetal bovine serum (Thermo Fisher Scientific, Waltham, MA, USA) and cryopreserved at − 80 °C. We have previously reported the phenotype of the established primary breast cancer cells (MUK-BC1)40.
Whole exome sequencing and RNA sequencing (RNA-seq)
Genomic DNA and total RNA were extracted from fresh tumours in RNAlater using the AllPrep DNA/RNA mini kit (Qiagen Inc., Venlo, Netherlands) in accordance with the manufacturer’s instructions. Control genomic DNA was extracted from patient-matched PBMCs. Whole exome libraries were prepared from 200 to 3000 ng genomic DNA using the SureSelect Human All Exon V6 kit (Agilent Technologies Inc., Santa Clara, CA, USA) in accordance with the manufacturer’s instructions. RNA-seq libraries were prepared using the TruSeq Stranded mRNA Library Prep kit (Illumina Inc., San Diego, CA, USA). The prepared whole exome and RNA-seq libraries were sequenced by a HiSeq 4000 at 2 × 100 bp or NovaSeq 6000 sequencer at 2 × 150 bp (Illumina). To analyse RNA-seq data, we used Cufflinks software41 and FPKM (fragments per kilobase of transcript per million mapped reads) values were calculated for immune-related gene expression analysis.
Read mapping and variant calling
Sequence alignment and mutation calling were performed as described previously42. For whole exome sequencing, the sequence reads were mapped to the human reference genome GRCh37/hg19 using Burrows–Wheeler Aligner (v0.7.10)43. Possible PCR duplicates, read pairs with a mapping quality of < 30, and mismatches of more than 5% were excluded. For RNA-seq, the sequence reads were mapped to the human reference genome GRCh37/hg19 using STAR (v2.4.0a)44. Somatic variants were called using Fisher’s exact test-based methods in accordance with the following parameters as described previously42: (1) base quality of ≥ 15; (2) sequence depth of ≥ 10; (3) variant depth of ≥ 4; (4) variant frequency in tumour of ≥ 10%; (5) variant frequency in normal samples of < 2%; (6) Fisher P-value of < 0.05. SNVs, indels, and splicing region were annotated using ANNOVAR45. We classified the somatic mutations as follows: (1) non-synonymous SNVs (nsSNVs); (2) splicing; (3) stop gain; (4) stop loss; (5) insertion/deletion (INDEL); (6) synonymous SNVs (sSNVs). Splicing mutation indicates that a single nucleotide variation occurred at the position of the splicing acceptor of the donor site.
We next used RNA-seq data of tumours to examine gene expression. The actual counts of sequence reads that covered the somatic mutated position were used to confirm mRNA expression of mutated genes46. This strategy was used, as if the FPKM value was used, the mRNA expression level would be calculated from the sum of mutated and non-mutated genes. The total RNA-seq read counts were > 20,000,000 per specimen.
Prediction of HLA class I-binding peptides
On the basis of whole exome sequencing data from normal DNA of PBMCs, HLA class I genotypes (HLA-A, -B, and -C) were determined by the OptiType algorithm47. We used only nsSNVs derived from possible peptides to predict HLA genotype-restricted neoantigens because the number of INDELs and fusions, if detected by RNA-seq, was much lower than that of nsSNVs and our neoantigen prediction algorithm for INDELs/fusions was under development and not yet validated42. Briefly, we examined all possible 8–11-mer peptides that harboured each substituted amino acid by filtering with the predicted binding affinity to HLA-A, -B, and -C of IC50 < 500 nM using NetMHCv3.4 and NetMHCpanv2.8 software48,49.
In the selection of neoantigen epitopes, we also considered the mRNA expression level of mutated genes by counting RNA-seq reads that contained the nsSNVs.
Generation of DCs from PBMCs
DCs were generated from cryopreserved PBMCs. PBMCs were thawed and cultured in 6-well plates (BD FALCON) that contained RPMI-1640 medium for 30 min. After removal of floating cells and washing the plate with RPMI-1640 medium, adherent cells were cultured in complete DC medium that consisted of RPMI-1640 medium with recombinant human granulocyte/monocyte colony-stimulating factor (GM-CSF; 100 ng/ml; Primmune Inc., Kobe, Japan) and recombinant human interleukin-4 (IL-4; 50 ng/ml; Primmune Inc.). On day 6, the cells were stimulated with a maturation cytokine cocktail that contained human recombinant tumour necrosis factor-α (TNF-α; 500 U/ml; PeproTech Inc., NJ, USA) and interferon-α (IFN-α; 500 U/ml; Dainippon Pharma, Osaka, Japan) for 18 h. Morphological changes were monitored by light microscopy and cells were examined by flow cytometric analysis. DCs that expressed high levels of HLA class I, HLA-DR, CD40, and a costimulatory molecule (CD86) with negative expression of CD14 (data not shown) were used for further experiments and referred to as mature DCs (mDCs).
Generation of neoantigen peptide-pulsed cytotoxic T lymphocytes (CTLs) ex vivo
After pulsing mDCs with the indicated synthesized neoantigen peptides (Table 3, closed square) for 4 h, we cocultured peptide-pulsed mDCs with peripheral lymphocytes obtained by excluding plastic-adherent monocytes from PBMCs. RPMI-1640 medium that contained 10% healthy human serum and recombinant human interleukin-2 (IL-2; 40 U/ml; Primmune Inc.) was used as the culture medium. We exchanged the medium once every 3–4 days. After 2 weeks of coculture, we harvested the lymphocytes and cocultured them with newly generated peptide-pulsed mDCs for another 2 weeks under the same culture condition used for the first coculture. The lymphocytes were then harvested and used as CTLs for further experiments.
ELISpot assay
The ELISpot assay was performed using the Human IFN-γ ELISpotplus kit (MABTECH, Cincinnati, OH, USA) in accordance with the manufacturer’s instructions. Briefly, 96-well plates with nitrocellulose membranes (Millipore, Molshelm, France) precoated with a primary anti-IFN-γ antibody were pretreated with RPMI-1640 medium that containrf 10% autologous serum at 4 °C overnight. A total of 1 × 104 autologous immature DCs were added to each well along with the DC maturation cocktail and the cells were incubated overnight. Synthesized neoantigen peptide (final concentrations of 5, 50, and 100 µg/ml) was added to each well and the cells were incubated for 4 h. After three washes with RPMI-1640 medium, 1.0 × 105 or 1.5 × 105 autologous peripheral lymphocytes were added to each well and the cells were incubated for 48 h. After three washes with PBS, the secondary antibody was added to each well and the cells were incubated for 2 h. The plates were incubated with HRP reagent and stained with TNB (MABTECH). Spots were captured and analysed by an automated ELISpot reader 08 classic (AID GmbH, Strasberg, Germany) and positivity of the neoantigen-specific T cell response was quantitatively defined as specific spots.
We also performed an ELISpot assay to examine the IFNγ-releasing ability of CTLs against autologous tumour. Briefly, target tumour cells (5 × 103 per well) were seeded in ELISpot 96-well plates prepared as described above and cultured overnight. CTLs were then added to the wells (5 × 104 per well) and the cells were incubated for 4 h at 37 °C, followed by the same procedure to detect IFN-γ spots as described above.
Calcein-release cytotoxicity assay and cell imaging
Target tumour cells (5 × 103 per well) were seeded in a 96-well flat-bottom plate and cultured overnight. The cells were then incubated at 37 °C for 1 h in the presence of calcein-AM. CTLs were then added to the wells (5 × 104 per well) and the cells were incubated with tumour cells for 4 h at 37 °C. Images were captured under a conventional fluorescence microscope (IX81; Olympus, Tokyo, Japan) equipped with a colour CCD camera (DPI72; Olympus) and objective lens (LUC plan FLN; Olympus). All procedures were performed at 20–25 °C. Images were analysed using Lumina Vision software. The cytotoxicity percentage was calculated as (control fluorescence—sample fluorescence)/control × 100%.
Statistical analyses
All data are expressed as the mean ± standard error of the mean (SEM). Differences between groups were assessed for statistical significance using the paired Student’s t-test. Pearson correlation (r) was used for correlation analysis between all examined parameters. A p-value of < 0.05 was considered statistically significant. Statistical analyses were performed using GraphPad Prism Version 8.3.0 (GraphPad software, La Jolla, CA, USA).
Ethics approval and consent to participate
This study was approved by the Ethics Committees of Kyushu University Hospital (No. 128) and Fukuoka General Cancer Clinic (FGCC-EC001).
Data availability
The datasets used and/or analysed during the current study are available from the first or corresponding author on reasonable request.
Abbreviations
- CTL:
-
Cytotoxic T lymphocyte
- DC:
-
Dendritic cell
- FPKM:
-
Fragments per kilobase of transcript per million mapped reads
- ICI:
-
Immune checkpoint inhibitor
- INDEL:
-
Insertion/deletion
- nsSNV:
-
Nonsynonymous single nucleotide variant
- PBMC:
-
Peripheral blood mononuclear cell
- sSNV:
-
Synonymous single nucleotide variant
- TIL:
-
Tumour-infiltrating lymphocyte
- TMB:
-
Tumour mutation burden
- TNBC:
-
Triple negative breast cancer
References
Waks, A. G. & Winer, E. P. Breast cancer treatment: a review. JAMA 321(3), 288–300 (2019).
Marra, A., Viale, G. & Curigliano, G. Recent advances in triple negative breast cancer: the immunotherapy era. BMC Med. 17(1), 90 (2019).
Rivera, E. & Gomez, H. Chemotherapy resistance in metastatic breast cancer: the evolving role of ixabepilone. Breast Cancer Res. 12(Suppl 2), S2 (2010).
Bai, X., Ni, J., Beretov, J., Graham, P. & Li, Y. Cancer stem cell in breast cancer therapeutic resistance. Cancer Treat. Rev. 69, 152–163 (2018).
Topalian, S. L. et al. Survival, durable tumor remission, and long-term safety in patients with advanced melanoma receiving nivolumab. J. Clin. Oncol. 32(10), 1020–1030 (2014).
Borghaei, H. et al. Nivolumab versus docetaxel in advanced nonsquamous non-small-cell lung cancer. N. Engl. J. Med. 373(17), 1627–1639 (2015).
Topalian, S. L. et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N. Engl. J. Med. 366(26), 2443–2454 (2012).
Larkin, J., Hodi, F. S. & Wolchok, J. D. Combined nivolumab and ipilimumab or monotherapy in untreated melanoma. N. Engl. J. Med. 373(13), 1270–1271 (2015).
Snyder, A. et al. Genetic basis for clinical response to CTLA-4 blockade in melanoma. N Engl J Med. 371(23), 2189–2199 (2014).
Sharma, P. & Allison, J. P. The future of immune checkpoint therapy. Science 348(6230), 56–61 (2015).
Pardoll, D. M. The blockade of immune checkpoints in cancer immunotherapy. Nat. Rev. Cancer. 12(4), 252–264 (2012).
Brown, S. D. et al. Neo-antigens predicted by tumor genome meta-analysis correlate with increased patient survival. Genome Res. 24(5), 743–750 (2014).
Rooney, M. S., Shukla, S. A., Wu, C. J., Getz, G. & Hacohen, N. Molecular and genetic properties of tumors associated with local immune cytolytic activity. Cell 160(1–2), 48–61 (2015).
Safonov, A. et al. Immune gene expression is associated with genomic aberrations in breast cancer. Cancer Res. 77(12), 3317–3324 (2017).
Karn, T. et al. Association between genomic metrics and immune infiltration in triple-negative breast cancer. JAMA Oncol. 3(12), 1707–1711 (2017).
McGranahan, N. et al. Clonal neoantigens elicit T cell immunoreactivity and sensitivity to immune checkpoint blockade. Science 351(6280), 1463–1469 (2016).
Yarchoan, M., Johnson, B. A. 3rd., Lutz, E. R., Laheru, D. A. & Jaffee, E. M. Targeting neoantigens to augment antitumour immunity. Nat. Rev. Cancer. 17(4), 209–222 (2017).
Zacharakis, N. et al. Immune recognition of somatic mutations leading to complete durable regression in metastatic breast cancer. Nat. Med. 24(6), 724–730 (2018).
Zhang, X. et al. Breast cancer neoantigens can induce CD8(+) T-cell responses and antitumor immunity. Cancer Immunol. Res. 5(7), 516–523 (2017).
Schumacher, T. N., Scheper, W. & Kvistborg, P. Cancer neoantigens. Annu. Rev. Immunol. 37, 173–200 (2019).
Balachandran, V. P. et al. Identification of unique neoantigen qualities in long-term survivors of pancreatic cancer. Nature 551(7681), 512–516 (2017).
Durgeau, A., Virk, Y., Corgnac, S. & Mami-Chouaib, F. Recent advances in targeting CD8 T-cell immunity for more effective cancer immunotherapy. Front. Immunol. 9, 14 (2018).
Schumacher, T. N. & Schreiber, R. D. Neoantigens in cancer immunotherapy. Science 348(6230), 69–74 (2015).
Narang, P., Chen, M., Sharma, A. A., Anderson, K. S. & Wilson, M. A. The neoepitope landscape of breast cancer: implications for immunotherapy. BMC Cancer 19(1), 200 (2019).
Lauss, M. et al. Mutational and putative neoantigen load predict clinical benefit of adoptive T cell therapy in melanoma. Nat. Commun. 8(1), 1738 (2017).
Sykulev, Y., Joo, M., Vturina, I., Tsomides, T. J. & Eisen, H. N. Evidence that a single peptide-MHC complex on a target cell can elicit a cytolytic T cell response. Immunity 4(6), 565–571 (1996).
Wang, X. & Li, M. Correlate tumor mutation burden with immune signatures in human cancers. BMC Immunol. 20(1), 4 (2019).
Binnewies, M. et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat. Med. 24(5), 541–550 (2018).
Chen, M. L. et al. Regulatory T cells suppress tumor-specific CD8 T cell cytotoxicity through TGF-beta signals in vivo. Proc. Natl. Acad. Sci. USA 102(2), 419–424 (2005).
Martelotto, L. G., Ng, C. K., Piscuoglio, S., Weigelt, B. & Reis-Filho, J. S. Breast cancer intra-tumor heterogeneity. Breast Cancer Res. 16(3), 210 (2014).
Kato, T. et al. Integrated analysis of somatic mutations and immune microenvironment of multiple regions in breast cancers. Oncotarget 8(37), 62029–62038 (2017).
McDonald, K. A. et al. Tumor heterogeneity correlates with less immune response and worse survival in breast cancer patients. Ann. Surg. Oncol. 26(7), 2191–2199 (2019).
Salgado, R. et al. The evaluation of tumor-infiltrating lymphocytes (TILs) in breast cancer: recommendations by an International TILs Working Group 2014. Ann. Oncol. 26(2), 259–271 (2015).
Luen, S., Virassamy, B., Savas, P., Salgado, R. & Loi, S. The genomic landscape of breast cancer and its interaction with host immunity. The Breast. 29, 241–250 (2016).
Turajlic, S. et al. Insertion-and-deletion-derived tumour-specific neoantigens and the immunogenic phenotype: a pan-cancer analysis. Lancet Oncol. 18(8), 1009–1021 (2017).
Yang, W. et al. Immunogenic neoantigens derived from gene fusions stimulate T cell responses. Nat. Med. 25(5), 767–775 (2019).
Alspach E, Lussier DM, Miceli AP, Kizhvatov I, DuPage M, Luoma AM, et al. MHC-II neoantigens shape tumour immunity and response to immunotherapy. Nature 574(7780), 696–701 (2017).
Tran, E. et al. Cancer immunotherapy based on mutation-specific CD4+ T cells in a patient with epithelial cancer. Science 344(6184), 641–645 (2014).
Yeo, S. K. & Guan, J. L. Breast cancer: multiple subtypes within a tumor? Trends Cancer. 3(11), 753–760 (2017).
Kubo, M. et al. Catumaxomab with activated T-cells efficiently lyses chemoresistant EpCAM-positive triple-negative breast cancer cell lines. Anticancer Res. 38(7), 4273–4279 (2018).
Trapnell, C. et al. Transcript assembly and quantification by RNA-Seq reveals unannotated transcripts and isoform switching during cell differentiation. Nat. Biotechnol. 28(5), 511–515 (2010).
Kiyotani, K. et al. Integrated analysis of somatic mutations and immune microenvironment in malignant pleural mesothelioma. Oncoimmunology 6(2), e1278330 (2017).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25(14), 1754–1760 (2009).
Dobin, A. et al. STAR: ultrafast universal RNA-seq aligner. Bioinformatics 29(1), 15–21 (2013).
Wang, K., Li, M. & Hakonarson, H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 38(16), e164 (2010).
Kiyotani, K., Chan, H. T. & Nakamura, Y. Immunopharmacogenomics towards personalized cancer immunotherapy targeting neoantigens. Cancer Sci. 109(3), 542–549 (2018).
Szolek, A. et al. OptiType: precision HLA typing from next-generation sequencing data. Bioinformatics 30(23), 3310–3316 (2014).
Lundegaard, C., Lund, O. & Nielsen, M. Accurate approximation method for prediction of class I MHC affinities for peptides of length 8, 10 and 11 using prediction tools trained on 9mers. Bioinformatics 24(11), 1397–1398 (2008).
Hoof, I. et al. NetMHCpan, a method for MHC class I binding prediction beyond humans. Immunogenetics 61(1), 1–13 (2009).
Acknowledgements
We thank Mitchell Arico from Edanz Group (https://en-author-services.edanz.com/ac) for editing a draft of this manuscript. The authors thank Shoko Sadatomi, Tamaki Nakagaki, Nobuhiro Torata, Midori Kojyo, Emi Nagao, Kaori Nomiyama, and Hideko Morisaki for technical assistance.
Funding
The research was supported by a Grant-in-Aid for Scientific Research (KAKENHI) (Grant Number JP18K08577).
Author information
Authors and Affiliations
Contributions
T.M. and M.K. designed the study, analysed the data, and wrote the manuscript. T.M., M.K., M.K., and M.Y. contributed to acquisition of breast cancer specimens and data collection. P.Y.Y., S.Y., J.H.P., and K.K. developed and/or contributed to the computational neoantigen prediction analysis. T.M. and M.U. conducted the ex vivo experiment. T.M., M.K., P.Y.Y., S.Y., J.H.P., K.K., Y.O., Y.N., T.M., and M.N. provided material support and study supervision and were major contributors to reviewing and editing the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Morisaki, T., Kubo, M., Umebayashi, M. et al. Neoantigens elicit T cell responses in breast cancer. Sci Rep 11, 13590 (2021). https://doi.org/10.1038/s41598-021-91358-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-91358-1
This article is cited by
-
Stimulating T cell responses against patient-derived breast cancer cells with neoantigen peptide-loaded peripheral blood mononuclear cells
Cancer Immunology, Immunotherapy (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.