Abstract
Although proximal gastrectomy (PG) provides superior nutritional outcomes over total gastrectomy (TG) in upper-third early gastric cancer (EGC), surgeons are reluctant to perform PG due to the high rate of postoperative reflux. This meta-analysis aimed to comprehensively compare operative outcomes, nutritional outcomes, and quality of life-related complications between TG and PG performed with esophagogastrostomy (EG), jejunal interposition, or double-tract reconstruction (DTR) to reduce reflux after PG. After searching PubMed, Embase, Medline, and Web of Science databases, 25 studies comparing PG with TG in upper-third EGC published up to October 2020 were identified. PG with DTR was similar to TG regarding operative outcomes. Patients who underwent PG with DTR had less weight reduction (weighted mean difference [WMD] 4.29; 95% confidence interval [0.51–8.07]), reduced hemoglobin loss (WMD 5.74; [2.56–8.93]), and reduced vitamin B12 supplementation requirement (odds ratio [OR] 0.06; [0.00–0.89]) compared to patients who underwent TG. PG with EG caused more reflux (OR 5.18; [2.03–13.24]) and anastomotic stenosis (OR 3.94; [2.40–6.46]) than TG. However, PG with DTR was similar to TG regarding quality of life-related complications including reflux, anastomotic stenosis, and leakage. Hence, PG with DTR can be recommended for patients with upper-third EGC considering its superior postoperative nutritional outcomes.
Similar content being viewed by others
Introduction
Nationwide surveys from East Asia have reported that the number of early gastric cancer (EGC) and upper-third gastric cancer cases has increased1,2,3, despite the decreasing incidence of gastric cancer globally4,5. According to the treatment guidelines by Korean and Japanese Gastric Cancer Associations, proximal gastrectomy (PG) and total gastrectomy (TG) can be considered an effective curative treatment for clinical stage IA cancer in the upper-third of the stomach6,7. However, in Korea, which has the highest incidence of gastric cancer worldwide, PG accounted for only 1.1% of all gastric cancer surgeries, while upper-third gastric cancer accounted for 16.0% of all gastric cancer cases in 20141.
TG is known to cause nutritional disadvantages compared to PG, especially in vitamin B12 because of the decrease in the intrinsic factor secreted by parietal cells located in the distal stomach8. Moreover, lesser post-gastrectomy syndromes occur after PG because of the retained storage capacity of the distal stomach and preserved function of the pylorus9. Despite the advantages in preserving the distal stomach, surgeons are reluctant to perform PG with esophagogastrostomy (EG) because of the notorious gastroesophageal reflux that occurs after PG10.
Several novel types of anastomosis to reduce gastroesophageal reflux have been created and tested including jejunal interposition (JI), jejunal pouch interposition (JPI), and double-tract reconstruction (DTR)11,12,13. Although DTR has gained popularity due to its easier laparoscopic approach than other methods, there is insufficient evidence regarding patient outcomes. Additionally, the choice of the method for anastomosis depends on the surgeons’ preference due to the unavailability of standardized guidelines14. To help surgeons decide regarding optimal anastomosis for patients with EGC undergoing PG, a comprehensive analysis of PG with several anastomotic methods is needed.
This systematic review and meta-analysis aimed to comprehensively compare TG and PG with several anastomotic methods to help surgeons choose the optimal anastomotic method and improve clinical outcomes in patients undergoing surgery. To achieve this goal, we analyzed operative outcomes, nutritional outcomes, and quality of life-related complications in patients with upper-third EGC who underwent either TG or PG, especially considering the various anastomotic methods.
Methods
Literature search strategy
This meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines to improve the quality of the systematic review15. A comprehensive literature search was performed using PubMed, Embase, Medline, and Web of Science databases. Related articles and the bibliography of the identified articles were also reviewed to prevent overlooking articles that may not have been indexed. Articles with suitable data published in English were included. Furthermore, articles published up to October 2020 were explored.
The search terms used were “early gastric cancer”, “proximal gastrectomy”, and “total gastrectomy” with the Medical Subject Headings (MeSH) terms, “Stomach Neoplasm” and “Gastrectomy”. Abstracts and full texts of all articles were screened and reviewed by two authors (I.H.L. and Y.J.O.) based on consensus agreement. The search was conducted up to October 22, 2020.
Study selection criteria
Studies that met the following criteria were included: (1) studies comparing PG and TG; (2) studies presenting the criteria for EGC including the stage or depth of invasion; and (3) studies including operative outcomes, nutritional outcomes, or quality of life-related complication. In cases where two studies were conducted using identical cohorts, the study with more comprehensive nutritional or operative outcomes was selected. The study by Kosuga et al. was selected over the study by Ichikawa et al. because it had more assessable data16,17.
Studies were excluded based on the following criteria: (1) lack of necessary statistical data such as variance; (2) non-English publications; (3) posters, review papers, comments, and abstract-only papers; (4) lack of criteria defining EGC according to stage and depth of invasion; and (5) the use of heterogeneous operation type. The studies by Kano et al. and Hayami et al., which compared TG and PG with EG combined with DFT, were excluded due to insufficient data and the heterogeneity in operative outcomes and gastroesophageal reflux due to the additional anti-reflux procedure of DFT18,19.
Data extraction and bias assessment
Data extraction from the included studies was performed by two authors independently (I.H.L. and Y.J.O.). The extracted data included (1) background of the study (author names, year of publication, study design, hospital location, nationality, and number of patients in each arm); (2) cohort characteristics (anastomosis type, age, sex, body mass index (BMI), and tumor size); (3) operative outcomes (operation time, intraoperative blood loss, postoperative complications, and postoperative hospital stay); (4) postoperative nutritional outcomes (weight change, hemoglobin change, postoperative vitamin B12 supplementation requirement, postoperative iron supplementation requirement, serum albumin change, and lymphocyte count change); and (5) postoperative quality of life-related complications (gastroesophageal reflux, anastomotic stenosis, and anastomotic leakage). Twenty-five non-randomized studies were assessed using the Risk of Bias In Non-Randomized Studies—of Interventions (ROBINS-I) tool, which is a useful tool for evaluating non-randomized studies20. Two studies were found to have serious bias due to bias in the measurement of outcomes and in the selection of the reported result (Table 1). Funnel plots were used to evaluate publication bias; and no bias was detected (see Supplementary Fig. S1 online).
Subgroup analysis and sensitivity analysis
In this meta-analysis, the included studies were divided into subgroups according to three types of anastomosis performed in PG: PG with DTR, PG with EG, and PG with JI. The PG with JI subgroup included PG with JI and PG with JPI; subgroup analyses were conducted in terms of operative outcomes, nutritional outcomes, and postoperative quality of life-related complications.
If a study included multiple types of anastomosis in PG without classification, the study was classified into the subgroup with the most common type accounting for more than 75% of the overall cohort. The studies by Furukawa et al. and Zhou et al. were classified into the DTR and EG subgroups respectively because the proportion of the most common type of anastomosis in the overall cohort was > 75% in both studies (78% and 89%, respectively)21,39. Considering the possibility of heterogeneity and bias imposed due to the classification, sensitivity analyses excluding the studies by Furukawa et al. and Zhou et al. were conducted in terms of operative outcomes, postoperative outcomes, and postoperative quality of life-related complications.
If a study included comparisons between TG and PG with two different types of anastomosis, the study was classified into both subgroups. Hence, the studies by Nomura et al. and Isobe et al. were classified into PG with two different subgroups; Nomura et al. (DTR and JI) and Isobe et al. (EG and JI)22,23. While performing subgroup analyses using these studies, it was inevitable to calculate the events in the TG group repeatedly because the data of two different subgroups were exploited. To minimize the bias incurred in repeatedly calculating the events in the TG group of the studies by Nomura et al. and Isobe et al., we performed additional analyses where the events in the TG and PG groups were counted only once by combining the data from each anastomosis type.
For operative parameters, subgroup analyses were conducted according to the type of surgery: open or laparoscopic surgery. For the postoperative complications, the onset and the severity measured according to the Clavien–Dindo (C–D) classification24. Subgroup analyses of gastroesophageal reflux were conducted according to the reported features (reflux symptoms or reflux esophagitis confirmed endoscopically), and their severity was measured using the Visick score or Los Angeles (LA) Classification System, respectively25,26.
Statistical analysis
All analyses were conducted using the statistical software Review Manager (RevMan Version 5.3; The Nordic Cochrane Centre, Copenhagen, Denmark). The outcomes of dichotomous variables are presented as odds ratios (ORs), while the outcomes of continuous variables are presented as weighted mean differences (WMDs). All results are presented with 95% confidence intervals (CIs) using the Mantel–Haenszel method27. Heterogeneity was measured using Higgins I2 statistics and the Cochran Q test28. The meta-analyses were performed using a random-effects model because the cohorts of the included studies from different institutions were not identical or homogenous29. If the only accessible data were median and interquartile ranges, the mean and standard deviation were estimated from the median, interquartile ranges, and the size of included studies according to the references30,31. A p-value of less than 0.05 was considered statistically significant.
Results
Study characteristics
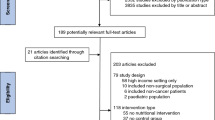
Twenty-five studies, including 3,058 patients (1,287 patients who underwent PG and 1,771 patients who underwent TG) were selected for the meta-analyses (Fig. 1 and Table 2). All studies were observational studies; 4 case-control studies and 21 retrospective cohort studies. PG with DTR was performed in 8 studies including 696 patients, while PG with non-DTR was performed in 18 studies including 2,392 patients. PG with EG was performed in 13 studies including 1,781 patients and PG with JI was performed in 6 studies including 649 patients.
The characteristics of the studies used in the meta-analyses are described in Table 216,21,22,23,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52. Age, sex, BMI, and tumor size are presented as mean ± standard deviation or median (interquartile range). Further, in one study, patients were categorized into 3 subgroups according to BMI (Supplementary Table S1 online). The criteria for EGC varied between studies, and the definition of EGC was clinical or pathological T1, or stage I gastric cancer in most studies. Three studies established the definition of EGC more narrowly as clinical or pathological stage IA35,37,52. In contrast, two studies defined EGC more widely as clinical or as pathological T1 or T2 gastric cancer32,39.
Operative outcomes
Operative time, intraoperative blood loss, postoperative complications, and duration of postoperative hospital stay were included in the meta-analysis of operative outcomes. In the analysis of the operative outcomes, the PG group was subdivided into PG with DTR, PG with EG, and PG with JI subgroups. The operative time was shorter in PG with EG (WMD − 42.53, CI − 50.74 to − 34.31; p < 0.01) than TG; however, there was no significant difference in the operative time between TG and PG with DTR (WMD − 2.23, CI − 17.67 to 13.21; p = 0.78) or PG with JI (WMD 1.18, CI − 15.42 to 17.77; p = 0.89) (Fig. 2a). Intraoperative blood loss was lower in PG with EG (WMD − 73.65, CI − 109.39 to − 37.90; p < 0.01) or PG with JI (WMD − 38.49, CI − 74.59 to − 2.39; p = 0.04) than in TG; however, there was no significant difference in intraoperative blood loss between PG with DTR and TG (WMD − 2.81, CI − 39.29 to 33.67; p = 0.88) (Fig. 2b). In addition, the duration of postoperative hospital stay was not significantly different between TG and PG with DTR (WMD − 0.67, CI − 2.00 to 0.67; p = 0.33), PG with EG (WMD 1.13, CI − 5.59 to 7.85; p = 0.74), or PG with JI (WMD − 1.59, CI − 4.70 to 1.52; p = 0.32) (Fig. 2c).
Forest plots for comparing operative outcomes between proximal gastrectomy and total gastrectomy including (a) operation time, (b) intraoperative blood loss, (c) postoperative hospital stay, and (d) postoperative complications. The meta-analyses were performed using the Mantel–Haenszel random-effect model. Weighted mean differences or odds ratios are shown with 95% confidence intervals. PG, proximal gastrectomy; TG, total gastrectomy; DTR, double-tract reconstruction; EG, esophagogastrostomy; JI, jejunal interposition.
In the analyses of postoperative complications, anastomotic leakage and stenosis were included in postoperative complications while gastroesophageal reflux was excluded. No significant difference was found between TG and PG with DTR (OR 0.76, CI 0.45–1.27; p = 0.29), PG with EG (OR 0.96, CI 0.44–2.07; p = 0.91), or PG with JI (OR 0.67, CI 0.42–1.07; p = 0.10) regarding postoperative complications (Fig. 2d). Specifically, there was no significant difference between TG and PG with DTR (OR 0.58, CI 0.32–1.05; p = 0.07), PG with EG (OR 0.60, CI 0.33–1.10; p = 0.10), and PG with JI (OR 0.69, CI 0.19–2.51; p = 0.57) in terms of early complications. Additionally, there was no significant difference between TG and PG with DTR (OR 0.55, CI 0.23–1.27; p = 0.16), PG with EG (OR 1.91, CI 0.49–7.50; p = 0.35), and PG with JI (OR 0.58, CI 0.25–1.37; p = 0.21) regarding late complications (see Supplementary Fig. S2 online). Severe complications (C–D grade ≥ III) occurred less frequently in PG with DTR than in TG (OR 0.42, CI 0.18–0.98; p = 0.05); however, there was no significant difference between TG and PG with DTR regarding less severe complications (C–D grade ≥ I, OR 0.80, CI 0.32–2.05; p = 0.65; and C–D grade ≥ II, OR 0.78, CI 0.46–1.31; p = 0.34) (see Supplementary Fig. S3 online).
In the analyses of operative outcomes, the included studies were subdivided into the laparoscopic and open surgery groups according to the types of PG and TG performed in each study. No studies compared open TG with open PG with DTR. The operative time was shorter in laparoscopic (WMD − 37.92, CI − 48.07 to − 27.76; p < 0.01) and open (WMD − 53.00, CI − 81.31 to − 24.69; p < 0.01) PG with EG compared to laparoscopic and open PG, respectively. Additionally, intraoperative blood loss was lower in laparoscopic PG with EG (WMD − 59.61, CI − 85.83 to − 33.39; p < 0.01) than in laparoscopic TG. However, there was no significant difference between open PG with EG (WMD − 217.62, CI − 525.66 to 90.43; p = 0.17) and open TG. All results of subgroup analyses of operative outcomes subdivided into the laparoscopic and open surgery groups are summarized in Supplementary Table S2 online.
Postoperative nutritional outcomes
The analyses of postoperative nutritional outcomes included postoperative weight change, change in hemoglobin level, and postoperative requirement for vitamin B12 supplementation. PG was subdivided into the PG with DTR, PG with EG, and PG with JI subgroups in these analyses. Patients who underwent PG with DTR (WMD 4.29, CI 0.51–8.07; p = 0.03), PG with EG (WMD 2.44, CI 0.41–4.46; p = 0.02), and PG with JI (WMD 4.53, CI 1.72–7.34; p < 0.01) had lesser reduction in weight 1 year postoperatively than patients underwent TG (Fig. 3a). In addition, patients who underwent PG with DTR (WMD 5.74, CI 2.56–8.93; p < 0.01), PG with EG (WMD 2.47, CI 1.89–3.04; p < 0.01), and PG with JI (WMD 2.70, CI 1.00–4.40; p < 0.01) had lower rates of hemoglobin reduction 1 year postoperatively than patients underwent TG (Fig. 3b). Moreover, postoperative vitamin B12 supplementation was required in fewer patients after PG with DTR (OR 0.06, CI 0.00–0.89; p = 0.04) and PG with EG (OR 0.00, CI 0.00–0.03; p < 0.01) compared to TG (Fig. 3c). Three studies stated that vitamin B12 supplementation was provided to patients whose serum vitamin B12 levels < 200 pg/mL33,34,36. The criterion for vitamin B12 supplementation was serum vitamin B12 level < 180 pg/mL in the study by Hosoda et al.; however, a definite criterion was not mentioned in the study by Kosuga et al16,42.
Forest plots for comparing postoperative nutritional outcomes between proximal gastrectomy and total gastrectomy including (a) weight change, (b) hemoglobin change at postoperative 1 year, and (c) postoperative vitamin B12 supplementation requirement. The meta-analyses were performed using the Mantel–Haenszel random-effect model. Weighted mean differences or odds ratios are shown with 95% confidence intervals. PG, proximal gastrectomy; TG, total gastrectomy; DTR, double-tract reconstruction; EG, esophagogastrostomy; JI, jejunal interposition.
Complications related to postoperative quality of life
The analyses of the complications related to postoperative quality of life consisted of three parts: gastroesophageal reflux, anastomotic stenosis, and anastomotic leakage. PG was subdivided into three subgroups: PG with DTR, PG with EG, and PG with JI. In terms of gastroesophageal reflux, TG and PG with DTR (OR 1.74, CI 0.63–4.80; p = 0.28) or PG with JI (OR 1.57, CI 0.89–2.75; p = 0.12) were comparable. However, PG with EG was more likely to cause gastroesophageal reflux than TG (OR 5.18, CI 2.03–13.24; p < 0.01) (Fig. 4a). To summarize, only PG with EG was more likely to cause reflux symptoms than TG (OR 5.91, CI 1.81–19.30; p < 0.01). Similarly, reflux esophagitis, which was confirmed endoscopically, was more likely to occur in PG with EG than in TG (OR 4.22, CI 1.43–12.40; p < 0.01) (see Supplementary Fig. S4 online).
Forest plots for comparing quality of life-related complications between proximal gastrectomy and total gastrectomy including (a) gastroesophageal reflux, (b) anastomotic stenosis, and (c) anastomotic leakage. The meta-analyses were performed using the Mantel–Haenszel random-effect model. Odds ratios are shown with 95% confidence intervals. PG, proximal gastrectomy; TG, total gastrectomy; DTR, double-tract reconstruction; EG, esophagogastrostomy; JI, jejunal interposition; JPI, jejunal pouch interposition.
In addition, the occurrence of anastomotic stenosis was similar between PG with DTR (OR 1.01, CI 0.38–2.66; p = 0.98) or PG with JI (OR 1.60, CI 0.66–3.90; p = 0.30) and TG; however, PG with EG was more likely to cause anastomotic stenosis than TG (OR 3.94, CI 2.40–6.46; p < 0.01) (Fig. 4b). Finally, there was no significant difference in the occurrence of anastomotic leakage between TG with PG with DTR (OR 0.91, CI 0.40–2.10; p = 0.83), PG with EG (OR 0.97, CI 0.39–2.43; p = 0.95), and PG with JI (OR 0.88; CI 0.16–4.93; p = 0.89) (Fig. 4c). All results are summarized in Supplementary Table S3. All results of subgroup analyses of postoperative complications and gastroesophageal reflux according to the onset and severity of postoperative complications and the reported type and severity of gastroesophageal reflux, respectively, are summarized in Supplementary Table S4 online.
Discussion
This study presents an updated summary of evidence regarding the comparison between PG and TG in the treatment of early gastric cancer. Because of the scarcity of prospective or randomized controlled studies on this topic, only retrospective studies were included, limiting the evidence of the study. However, to the best of our knowledge, this study provides clinicians with a detailed comparison between PG and TG regarding operative, nutritional, and postoperative aspects considering various anastomosis types in PG. Patients who underwent PG with EG or PG with DTR had lower weight loss, hemoglobin loss, and postoperative vitamin B12 supplementation requirement than those who underwent TG, signifying the nutritional benefit of PG with EG or PG with DTR. Although PG with EG had superior operative outcomes, including reduction in operative time and intraoperative blood loss, more postoperative gastroesophageal reflux and anastomotic leakage were reported after PG with EG than after TG. Therefore, PG with DTR was found to be the most beneficial for the treatment of early gastric cancer.
The surgical safety profiles were similar between PG with DTR and TG, including a shorter operative time, reduced intraoperative blood loss, a shorter postoperative hospital stay, and reduced postoperative complications. DTR is considered a relatively demanding technique because it takes more time to perform additional gastrojejunostomy compared with Roux-en-Y reconstruction. However, both PG with DTR and TG had comparable operation time because suprapyloric and infrapyloric lymph node dissections were usually performed in the latter while mostly reserved in the former. The safety of PG in EGC has been a concern owing to the limited lymph node dissection and the remnant stomach. However, the survival and recurrence rates after PG were reportedly similar to that after TG in recent meta-analyses53,54. In subgroup analyses according to open and laparoscopic approaches, PG with EG had a shorter operative time than TG, which could be attributable to its relatively less complicated surgical procedure in both laparoscopic and open approaches. Patients who underwent laparoscopic PG with EG experienced lesser intraoperative blood loss than those who underwent laparoscopic TG, which could be presumed based on the smallest operation range and the simplest anastomotic procedure among laparoscopic PG with the three anastomosis types and TG.
Furthermore, PG with DTR had less severe postoperative complications (C–D score ≥ III) than TG; this result is inconsistent with that reported in a previous study53, in which there was no significant difference between PG with DTR and TG with regard to postoperative complications. This inconsistency seems to have been caused by the fact that our meta-analysis included more studies. Ko et al. reported that 3 patients with TG experienced pancreatic fistula, while no patients who underwent PG with DTR experienced pancreatic fistula32. The occurrence of pancreatic fistula after TG can be attributed to infrapyloric lymph node dissection, which results in pancreatic injury55. Although infrapyloric lymph node dissection is usually performed in TG to reduce the likelihood of recurrence and metastasis, radical dissection of peripancreatic lymph nodes can lead to severe complications related to pancreatic injury.
Regarding postoperative nutritional outcomes, the present meta-analysis revealed that patients who underwent PG with DTR had lower weight loss, hemoglobin loss, and postoperative vitamin B12 supplementation requirement than those who underwent TG, which is consistent with the findings of previous meta-analyses53,54. The difference in the severity of weight loss is attributable to food passage through the duodenum in DTR. The preservation of duodenal food passage has physiological benefits in nutrient absorption with adequate chyme with bile and pancreatic juice and gastrointestinal hormonal regulation56. Hence, patients without duodenal food passage after undergoing PG with DTR experienced more weight loss in a previous study57. These nutritional characteristics could be beneficial for patients with cancer because weight loss is associated with shorter failure-free and overall survival and decreased response to chemotherapy, quality of life, and performance status. Given that patients with EGC do not receive chemotherapy, weight loss is one of the important factors determining the quality of life in patients with cancer58. In particular, more than 10% of weight loss after gastrectomy was related to disabling symptoms and had a negative impact on the quality of life59.
Additionally, patients who underwent PG were less likely to have vitamin B12 deficiency, which can be attributed to the remnant stomach where the intrinsic factor from parietal cells absorb vitamin B1260. Given that vitamin B12 deficiency is known to cause megaloblastic anemia and neuropsychiatric symptoms, the advantage of PG in ensuring vitamin B12 absorption has a clinically beneficial impact on the quality of life of patients8. Similarly, lower hemoglobin loss in PG than in TG 1 year after gastrectomy is likely to be related to the lower incidence of vitamin B12 deficiency in patients who underwent PG in the present study. However, previous studies reported that anemia, which occurs during the first few years after TG is mainly caused by iron deficiency, rather than vitamin B12 deficiency, because it takes a few years to deplete the human body’s stores of vitamin B1261,62. Future studies with long-term follow-up are needed to elucidate the different underlying mechanisms of anemia in patients who underwent PG or TG.
PG with DTR was also similar to TG in terms of postoperative complications related to the quality of life. Specifically, the incidence of gastroesophageal reflux or anastomotic stenosis was similar between PG with DTR or PG with JI and TG; however, the incidence was higher in PG with EG than in TG. The long Roux-en-Y limb functions as a barrier to the reflux in TG with Roux-en-Y reconstruction, while the mechanisms to prevent reflux are less effective in PG with EG10,63. The jejunal limb of DTR is also thought to have a similar function to the Roux-en-Y limb in TG, contributing to the lesser occurrence of reflux. Moreover, there was no difference in anastomotic leakage between TG and PG with DTR. Considering that DTR has 2 more anastomotic sites than EG, this result implicates the feasibility of DTR despite it being a more complicated surgical procedure. Hence, PG with DTR can be considered relatively safe to maintain an acceptable quality of life after surgery.
Among the three anastomosis types of PG, EG and JI have proved to be superior to TG in a few operative outcomes, such as operation time (EG) and intraoperative blood loss (EG and JI). However, the results of postoperative complications related to anastomosis and its symptoms differed depending on the specific type of anastomosis. When PG was performed with EG, anastomotic stenosis and gastroesophageal reflux occurred more frequently than in TG, leading to the conclusion that it is not an optimal treatment method for EGC. In contrast, there was no significant difference between PG with JI and TG in terms of anastomotic stenosis and reflux due to the function of JI as an alternative sphincter. However, PG with JI is not generally performed due to its technical difficulty during laparoscopic procedures64.
To overcome the limitations of EG like symptomatic reflux, several additional anti-reflux techniques have been designed, such as the double flap technique (DFT) during EG with valvuloplasty, in which a seromuscular flap is created to avoid reflux18,19. In a previous retrospective study performed by Hayami et al., anastomotic complications (4.7% vs. 17.2%) and severe reflux esophagitis with LA grade ≥ B (2.3% vs. 14.9%) occurred less frequently after EG with DFT than after TG, but the difference was not significant (p = 0.093 and p = 0.06, respectively)19. Although EG with DFT was excluded from the present meta-analysis because of insufficient data and the heterogeneity of EG combined with DFT due to EG in operative and reflux-related outcomes, the efficacy and safety of this technique should also be evaluated by comparing EG with DFT and other methods in future studies18,19,65.
In the bias assessment using the ROBINS-I tool, two studies were identified to have serious biases. In one study, the bias was due to the selection of the reported results regarding postoperative complications, while in the other study, the bias was due to the inconsistent frequency of postoperative upper endoscopic examination between PG and TG46,48. In the present meta-analysis, the studies by Furukawa et al. and Zhou et al., including multiple types of anastomosis in PG without classification, were classified into subgroups, with the most common type accounting for more than 75% of the overall cohort, which might cause bias. In this reason, additional analyses excluding the studies by Furukawa et al. and Zhou et al. were conducted to minimize heterogeneity and bias. In the analysis, there was no difference in the tendency of preference between PG and TG in all aspects. In addition, the studies by Nomura et al. and Isobe et al., comparing TG with PG with two different types of anastomosis, were classified into both subgroups, which might also increase bias because the events in the TG group would be repeatedly calculated in the process of synthesizing all subgroup analyses. Therefore, we performed additional analyses in which the events in the TG and PG groups were counted only once regardless of the number of anastomosis type in the study by combining the data from each anastomosis type. In the analysis, there was also no difference in the tendency of preference between PG and TG in all aspects. The results of additional analyses are provided in Supplementary Table S5 and S6 online.
Our meta-analysis has several limitations. First, there is a lack of prospective cohort studies and randomized controlled trials. Although four case-control studies were included, there is a possibility of selection and confounding bias. Although no publication bias was identified in the symmetry of funnel plots, it was difficult to exclude publication bias because other biases accompanying publication bias could not be excluded in the analyses of retrospective studies66. Second, both JI and JPI were included in the JI subgroup because of their similarity and the smaller number of studies evaluating them. Finally, although the present meta-analysis revealed a tendency of preference for PG in terms of hemoglobin change and vitamin B12 deficiency, the number of studies included in the analyses of hemoglobin change 1 year postoperatively and postoperative vitamin B12 supplementation requirement was insufficient to provide reliability. Considering that only a limited number of retrospective studies have been performed thus far, further studies are warranted to elucidate the metabolic impact of PG and TG. In addition, randomized controlled trials including comparison of nutritional outcomes between PG and TG and analyses comparing PG with JI and PG with JPI separately should be conducted to accumulate evidence and minimize bias.
In summary, PG with DTR is superior to TG in terms of nutritional outcomes, causing lesser weight reduction, and reduced hemoglobin loss, with reduced postoperative vitamin B12 supplementation requirement. Furthermore, PG with DTR has no disadvantage regarding operative outcomes and the postoperative complications related to quality of life such as gastroesophageal reflux and anastomotic leakage. In conclusion, PG with DTR can be a promising treatment option for patients with EGC without compromising nutritional requirements and postoperative quality of life. Considering the superiority of PG with EG regarding operative outcomes, the safety and efficacy of EG with anti-reflux procedures such as DFT should be evaluated in future studies.
Data availability
All data relevant to the present study are provided in the manuscript and supplementary materials.
References
Information Committee of Korean Gastric Cancer Association. Korean gastric cancer association nationwide survey on gastric cancer in 2014. J. Gastric. Cancer 16, 131–140. https://doi.org/10.5230/jgc.2016.16.3.131 (2016).
Blaser, M. J. & Saito, D. Trends in reported adenocarcinomas of the oesophagus and gastric cardia in Japan. Eur. J. Gastroenterol. Hepatol. 14, 107–113. https://doi.org/10.1097/00042737-200202000-00003 (2002).
Zhou, Y. et al. A rising trend of gastric cardia cancer in Gansu Province of China. Cancer Lett. 269, 18–25. https://doi.org/10.1016/j.canlet.2008.04.013 (2008).
de Martel, C., Forman, D. & Plummer, M. Gastric cancer: epidemiology and risk factors. Gastroenterol. Clin. North Am. 42, 219–240. https://doi.org/10.1016/j.gtc.2013.01.003 (2013).
Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 32 cancer groups, 1990 to 2015: a systematic analysis for the global burden of disease study. JAMA Oncol. 3, 524–548. https://doi.org/10.1001/jamaoncol.2016.5688 (2017).
Guideline Committee of the Korean Gastric Cancer Association (KGCA), Development Working Group & Review Panel. Korean practice guideline for gastric cancer 2018: an evidence-based, multi-disciplinary approach. J. Gastric. Cancer 19, 1–48. https://doi.org/10.5230/jgc.2019.19.e8 (2019).
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver 4). Gastric Cancer 20, 1–19. https://doi.org/10.1007/s10120-016-0622-4 (2017).
Hu, Y. et al. Vitamin B(12) deficiency after gastrectomy for gastric cancer: an analysis of clinical patterns and risk factors. Ann. Surg. 258, 970–975. https://doi.org/10.1097/SLA.0000000000000214 (2013).
Takiguchi, N. et al. Long-term quality-of-life comparison of total gastrectomy and proximal gastrectomy by postgastrectomy syndrome assessment scale (PGSAS-45): a nationwide multi-institutional study. Gastric Cancer 18, 407–416. https://doi.org/10.1007/s10120-014-0377-8 (2015).
Hsu, C. P. et al. Esophageal reflux after total or proximal gastrectomy in patients with adenocarcinoma of the gastric cardia. Am. J.Gastroenterol. 92, 1347–1350 (1997).
Kameyama, J. et al. Proximal gastrectomy reconstructed by interposition of a jejunal pouch. Surgical technique. Eur. J.Surg. 159, 491–493 (1993).
Mine, S., Nunobe, S. & Watanabe, M. A Novel technique of anti-reflux esophagogastrostomy following left thoracoabdominal esophagectomy for carcinoma of the esophagogastric Junction. World J. Surg. 39, 2359–2361. https://doi.org/10.1007/s00268-015-3079-4 (2015).
Aikou, T., Natsugoe, S., Shimazu, H. & Nishi, M. Antrum preserving double tract method for reconstruction following proximal gastrectomy. Jpn. J. Surg. 18, 114–115. https://doi.org/10.1007/BF02470857 (1988).
Yang, K. et al. Laparoscopic proximal gastrectomy with double-tract reconstruction by intracorporeal anastomosis with linear staplers. J. Am. Coll. Surg. 222, e39-45. https://doi.org/10.1016/j.jamcollsurg.2016.01.002 (2016).
Shamseer, L. et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 350, g7647. https://doi.org/10.1136/bmj.g7647 (2015).
Kosuga, T. et al. Feasibility and nutritional benefits of laparoscopic proximal gastrectomy for early gastric cancer in the upper stomach. Ann. Surg. Oncol. 22(Suppl 3), S929-935. https://doi.org/10.1245/s10434-015-4590-4 (2015).
Ichikawa, D. et al. Long-term outcomes of patients who underwent limited proximal gastrectomy. Gastric Cancer 17, 141–145. https://doi.org/10.1007/s10120-013-0257-7 (2014).
Kano, Y. et al. Oncological feasibility of laparoscopic subtotal gastrectomy compared with laparoscopic proximal or total gastrectomy for cT1N0M0 gastric cancer in the upper gastric body. Gastric Cancer 22, 1060–1068. https://doi.org/10.1007/s10120-019-00947-7 (2019).
Hayami, M. et al. Clinical outcomes and evaluation of laparoscopic proximal gastrectomy with double-flap technique for early gastric cancer in the upper third of the stomach. Ann. Surg. Oncol. 24, 1635–1642. https://doi.org/10.1245/s10434-017-5782-x (2017).
Sterne, J. A. et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 355, i4919. https://doi.org/10.1136/bmj.i4919 (2016).
Furukawa, H. et al. Short-term outcomes and nutritional status after laparoscopic subtotal gastrectomy with a very small remnant stomach for cStage I proximal gastric carcinoma. Gastric Cancer 21, 500–507. https://doi.org/10.1007/s10120-017-0755-0 (2018).
Nomura, E. et al. Functional evaluations comparing the double-tract method and the jejunal interposition method following laparoscopic proximal gastrectomy for gastric cancer: an investigation including laparoscopic total gastrectomy. Surg. Today 49, 38–48. https://doi.org/10.1007/s00595-018-1699-7 (2019).
Isobe, T. et al. Reconstruction methods and complications in proximal gastrectomy for gastric cancer, and a comparison with total gastrectomy. Kurume Med. J. 61, 23–29. https://doi.org/10.2739/kurumemedj.MS64003 (2014).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 240, 205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae (2004).
Visick, A. H. A study of the failures after gastrectomy. Ann. R. Coll. Surg. Engl. 3, 266–284 (1948).
Armstrong, D. et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology 111, 85–92. https://doi.org/10.1053/gast.1996.v111.pm8698230 (1996).
Mantel, N. & Haenszel, W. Statistical aspects of the analysis of data from retrospective studies of disease. J. Natl. Cancer Inst. 22, 719–748 (1959).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560. https://doi.org/10.1136/bmj.327.7414.557 (2003).
Borenstein, M., Hedges, L. V., Higgins, J. P. & Rothstein, H. R. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res. Synth. Methods 1, 97–111. https://doi.org/10.1002/jrsm.12 (2010).
Hozo, S. P., Djulbegovic, B. & Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 5, 13. https://doi.org/10.1186/1471-2288-5-13 (2005).
Wan, X., Wang, W., Liu, J. & Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 14, 135. https://doi.org/10.1186/1471-2288-14-135 (2014).
Ko, H. J. et al. Can proximal gastrectomy with double-tract reconstruction replace total gastrectomy? A propensity score matching analysis. J. Gastrointest Surg. 24, 516–524. https://doi.org/10.1007/s11605-019-04195-z (2020).
Cho, M. et al. Similar hematologic and nutritional outcomes after proximal gastrectomy with double-tract reconstruction in comparison to total gastrectomy for early upper gastric cancer. Surg. Endosc. 33, 1757–1768. https://doi.org/10.1007/s00464-018-6448-x (2019).
Park, J. Y., Park, K. B., Kwon, O. K. & Yu, W. Comparison of laparoscopic proximal gastrectomy with double-tract reconstruction and laparoscopic total gastrectomy in terms of nutritional status or quality of life in early gastric cancer patients. Eur. J. Surg. Oncol. 44, 1963–1970. https://doi.org/10.1016/j.ejso.2018.08.014+ (2018).
Sugiyama, M. et al. Laparoscopic proximal gastrectomy maintains body weight and skeletal muscle better than total gastrectomy. World J. Surg. 42, 3270–3276. https://doi.org/10.1007/s00268-018-4625-7 (2018).
Jung, D. H. et al. Laparoscopic proximal gastrectomy with double tract reconstruction is superior to laparoscopic total gastrectomy for proximal early gastric cancer. Surg. Endosc. 31, 3961–3969 (2017).
Kim, D. J. & Kim, W. Laparoscopy-assisted proximal gastrectomy with double tract anastomosis is beneficial for vitamin B12 and iron absorption. Anticancer Res. 36, 4753–4758. https://doi.org/10.21873/anticanres.11031 (2016).
Asaoka, R. et al. Changes in body weight, skeletal muscle and adipose tissue after gastrectomy: a comparison between proximal gastrectomy and total gastrectomy. ANZ J. Surg. 89, 79–83. https://doi.org/10.1111/ans.15023 (2019).
Zhu, Z. et al. Surgical choice of proximal gastric cancer in China: a retrospective study of a 30-year experience from a single center in China. Expert Rev. Gastroenterol. Hepatol. 13, 1123–1128. https://doi.org/10.1080/17474124.2019.1689816 (2019).
Ushimaru, Y. et al. Clinical outcomes of gastric cancer patients who underwent proximal or total gastrectomy: a propensity score-matched analysis. World J. Surg. 42, 1477–1484. https://doi.org/10.1007/s00268-017-4306-y (2018).
Nishigori, T. et al. Superiority of laparoscopic proximal gastrectomy with hand-sewn esophagogastrostomy over total gastrectomy in improving postoperative body weight loss and quality of life. Surg. Endosc. 31, 3664–3672. https://doi.org/10.1007/s00464-016-5403-y (2017).
Hosoda, K. et al. Potential benefits of laparoscopy-assisted proximal gastrectomy with esophagogastrostomy for cT1 upper-third gastric cancer. Surg. Endosc. 30, 3426–3436. https://doi.org/10.1007/s00464-015-4625-8 (2016).
Huh, Y. J. et al. Clinical outcome of modified laparoscopy-assisted proximal gastrectomy compared to conventional proximal gastrectomy or total gastrectomy for upper-third early gastric cancer with special references to postoperative reflux esophagitis. J. Gastric. Cancer 15, 191–200. https://doi.org/10.5230/jgc.2015.15.3.191 (2015).
Ohashi, M. et al. Functional advantages of proximal gastrectomy with jejunal interposition over total gastrectomy with Roux-en-Y esophagojejunostomy for early gastric cancer. World J. Surg. 39, 2726–2733. https://doi.org/10.1007/s00268-015-3180-8 (2015).
Masuzawa, T. et al. Comparison of perioperative and long-term outcomes of total and proximal gastrectomy for early gastric cancer: a multi-institutional retrospective study. World J. Surg. 38, 1100–1106. https://doi.org/10.1007/s00268-013-2370-5 (2014).
Son, M. W., Kim, Y. J., Jeong, G. A., Cho, G. S. & Lee, M. S. Long-term outcomes of proximal gastrectomy versus total gastrectomy for upper-third gastric cancer. J. Gastric. Cancer 14, 246–251. https://doi.org/10.5230/jgc.2014.14.4.246 (2014).
Ahn, S. H., Lee, J. H., Park, D. J. & Kim, H. H. Comparative study of clinical outcomes between laparoscopy-assisted proximal gastrectomy (LAPG) and laparoscopy-assisted total gastrectomy (LATG) for proximal gastric cancer. Gastric Cancer 16, 282–289. https://doi.org/10.1007/s10120-012-0178-x (2013).
Nozaki, I. et al. Long-term outcome after proximal gastrectomy with jejunal interposition for gastric cancer compared with total gastrectomy. World J. Surg. 37, 558–564. https://doi.org/10.1007/s00268-012-1894-4 (2013).
Namikawa, T. et al. Impact of jejunal pouch interposition reconstruction after proximal gastrectomy for early gastric cancer on quality of life: short- and long-term consequences. Am. J. Surg. 204, 203–209. https://doi.org/10.1016/j.amjsurg.2011.09.035 (2012).
An, J. Y. et al. The difficult choice between total and proximal gastrectomy in proximal early gastric cancer. Am. J. Surg. 196, 587–591. https://doi.org/10.1016/j.amjsurg.2007.09.040 (2008).
Kitano, S., Shiraishi, N., Uyama, I., Sugihara, K. & Tanigawa, N. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann. Surg. 245, 68–72. https://doi.org/10.1097/01.sla.0000225364.03133.f8 (2007).
Kondoh, Y. et al. Clinical outcome of proximal gastrectomy in patients with early gastric cancer in the upper third of the stomach. Tokai J. Exp. Clin. Med. 32, 48–53 (2007).
Li, S. et al. A meta-analysis of comparison of proximal gastrectomy with double-tract reconstruction and total gastrectomy for proximal early gastric cancer. BMC Surg. 19, 117. https://doi.org/10.1186/s12893-019-0584-7 (2019).
Xu, Y. et al. Proximal versus total gastrectomy for proximal early gastric cancer: a systematic review and meta-analysis. Medicine (Baltimore) 98, e15663. https://doi.org/10.1097/MD.0000000000015663 (2019).
Kobayashi, N. et al. Process of pancreas head as a risk factor for postoperative pancreatic fistula in laparoscopic gastric cancer surgery. World J. Surg. 40, 2194–2201. https://doi.org/10.1007/s00268-016-3536-8 (2016).
Schwarz, A. et al. Importance of the duodenal passage and pouch volume after total gastrectomy and reconstruction with the Ulm pouch: prospective randomized clinical study. World J. Surg. 20, 60–66. https://doi.org/10.1007/s002689900011 (1996).
Yamashita, K. et al. Preservation of physiological passage through the remnant stomach prevents postoperative malnutrition after proximal gastrectomy with double tract reconstruction. Surg. Today 49, 748–754. https://doi.org/10.1007/s00595-019-01799-5 (2019).
Andreyev, H. J., Norman, A. R., Oates, J. & Cunningham, D. Why do patients with weight loss have a worse outcome when undergoing chemotherapy for gastrointestinal malignancies?. Eur. J. Cancer 34, 503–509. https://doi.org/10.1016/s0959-8049(97)10090-9 (1998).
Climent, M. et al. Weight loss and quality of life in patients surviving 2 years after gastric cancer resection. Eur. J. Surg. Oncol. 43, 1337–1343. https://doi.org/10.1016/j.ejso.2017.01.239 (2017).
Andres, E. et al. Vitamin B12 (cobalamin) deficiency in elderly patients. Can. Med. Assoc. J. 171, 251–259. https://doi.org/10.1503/cmaj.1031155 (2004).
Lim, C. H. et al. Anemia after gastrectomy for early gastric cancer: long-term follow-up observational study. World. J. Gastroenterol. 18, 6114–6119. https://doi.org/10.3748/wjg.v18.i42.6114 (2012).
Maclean, L. D. & Sundberg, R. D. Incidence of megaloblastic anemia after total gastrectomy. N. Engl. J. Med. 254, 885–893. https://doi.org/10.1056/NEJM195605102541902 (1956).
Gustavsson, S., Ilstrup, D. M., Morrison, P. & Kelly, K. A. Roux-Y stasis syndrome after gastrectomy. Am. J. Surg. 155, 490–494. https://doi.org/10.1016/s0002-9610(88)80120-x (1988).
Kinoshita, T. et al. Laparoscopic proximal gastrectomy with jejunal interposition for gastric cancer in the proximal third of the stomach: a retrospective comparison with open surgery. Surg. Endosc. 27, 146–153. https://doi.org/10.1007/s00464-012-2401-6 (2013).
Hosoda, K. et al. Comparison of double-flap and OrVil techniques of laparoscopy-assisted proximal gastrectomy in preventing gastroesophageal reflux: a retrospective cohort study. Langenbecks Arch. Surg. 404, 81–91. https://doi.org/10.1007/s00423-018-1743-5 (2019).
Ioannidis, J. P. & Trikalinos, T. A. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. Can. Med. Assoc. J. 176, 1091–1096. https://doi.org/10.1503/cmaj.060410 (2007).
Acknowledgements
The first two authors contributed equally to this work. This work was supported by Korea University Grant (K1813051).
Author information
Authors and Affiliations
Contributions
I.H.L., Y.J.O., and S.S.P. designed the study, conducted the analyses, interpreted the data, and wrote the manuscript. I.H.L. and Y.J.O. performed the literature search, data acquisition, and bias assessment. S.H.P. and Y.K.K. contributed to the study design, interpretation, and drafting of the manuscript. All authors have reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, I., Oh, Y., Park, S.H. et al. Postoperative nutritional outcomes and quality of life-related complications of proximal versus total gastrectomy for upper-third early gastric cancer: a meta-analysis. Sci Rep 10, 21460 (2020). https://doi.org/10.1038/s41598-020-78458-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-78458-0
This article is cited by
-
Prognostic value of GLIM-defined malnutrition in combination with hand-grip strength or gait speed for the prediction of postoperative outcomes in gastric cancer patients with cachexia
BMC Cancer (2024)
-
Prognostic nomograms for gastric carcinoma after D2 + total gastrectomy to assist decision-making for postoperative treatment: based on Lasso regression
World Journal of Surgical Oncology (2023)
-
The comparison of long-term oncological outcomes and complications after proximal gastrectomy with double tract reconstruction versus total gastrectomy for proximal gastric cancer
World Journal of Surgical Oncology (2023)
-
Outcomes of Proximal Versus Total Gastrectomy for Proximal Gastric Cancer: A Propensity Score-Matched Analysis of a Western Center Experience
Journal of Gastrointestinal Surgery (2023)
-
Effects of proximal gastrectomy with narrow gastric tube anastomosis compared with total gastrectomy with Roux-en-Y anastomosis on upper gastric cancer
Langenbeck's Archives of Surgery (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.