Abstract
Background
Oesophageal cancer is frequently accompanied with malnutrition. We aimed to evaluate if early support from dietitians and patient’s level of satisfaction with the support from dietitians are associated with better outcomes for weight loss and nutrition impact symptoms (NIS).
Methods
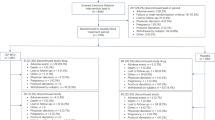
A nationwide and prospective cohort study on patients operated for oesophageal cancer in Sweden from 2013 onwards, included one year after surgery. Study exposures were (1) preoperative dietitian support (yes vs no) and, (2) patient reported satisfaction with dietitian support (high vs low) and outcomes were postoperative (1) percentage weight loss and (2) NIS score (range 0–24); one year after surgery. An ANCOVA model adjusted for predefined confounders was used and presented as mean differences (MD) with 95% confidence intervals (CI).
Results
Among 245 patients, as many as 57% had received preoperative dietitian support. Preoperative dietitian support was not associated with statistically significant differences in mean postoperative weight loss (MD 0.2 [95% CI −2.6 to 2.9]) and mean NIS score (MD 0.1 [95% CI: −0.8 to 1.0]). Likewise, satisfaction with the dietitian support was not associated with significant differences in mean postoperative weight loss (MD 1.4 [95% CI: −1.5 to 4.3]) and NIS score (MD −0.1 [95% CI: −1 to 0.8]).
Conclusions
Long-term postoperative weight loss and NIS were not influenced based on whether dietitian support was initiated preoperatively or not and patient’s satisfaction level with dietitian support. Similarity in results may reflect effective screening of malnutrition and dietitian support in centres treating oesophageal cancer in Sweden.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Anandavadivelan P, Lagergren P. Cachexia in patients with oesophageal cancer. Nat Rev Clin Oncol. 2016;13:185–98. https://doi.org/10.1038/nrclinonc.2015.200.
Shapiro J, van Lanschot JJ, Hulshof MC, van Hagen P, van Berge Henegouwen MI, Wijnhoven BP, et al. Neoadjuvant chemoradiotherapy plus surgery versus surgery alone for oesophageal or junctional cancer (CROSS): long-term results of a randomised controlled trial. Lancet Oncol. 2015;16:1090–8. https://doi.org/10.1016/s1470-2045(15)00040-6.
van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N. Engl J Med. 2012;366:2074–84. https://doi.org/10.1056/NEJMoa1112088.
Adenis A, Tresch E, Dewas S, Romano O, Messager M, Amela E, et al. Clinical complete responders to definite chemoradiation or radiation therapy for oesophageal cancer: predictors of outcome. BMC Cancer. 2013;13:413. https://doi.org/10.1186/1471-2407-13-413.
Lagergren J, Smyth E, Cunningham D, Lagergren P. Oesophageal cancer. Lancet. 2017;390:2383–96. https://doi.org/10.1016/s0140-6736(17)31462-9.
Omlin A, Blum D, Wierecky J, Haile SR, Ottery FD, Strasser F. Nutrition impact symptoms in advanced cancer patients: frequency and specific interventions, a case-control study. J Cachexia Sarcopenia Muscle. 2013;4:55–61. https://doi.org/10.1007/s13539-012-0099-x.
Viklund P, Wengstrom Y, Rouvelas I, Lindblad M, Lagergren J. Quality of life and persisting symptoms after oesophageal cancer surgery. Eur J Cancer. 2006;42:1407–14. https://doi.org/10.1016/j.ejca.2006.02.005.
Martin L, Lagergren J, Lindblad M, Rouvelas I, Lagergren P. Malnutrition after oesophageal cancer surgery in Sweden. Br J Surg. 2007;94:1496–1500. https://doi.org/10.1002/bjs.5881.
Hynes O, Anandavadivelan P, Gossage J, Johar AM, Lagergren J, Lagergren P. The impact of pre- and post-operative weight loss and body mass index on prognosis in patients with oesophageal cancer. Eur J Surgical Oncol: J Eur Soc Surgical Oncol Br Assoc Surgical Oncol. 2017;43:1559–65. https://doi.org/10.1016/j.ejso.2017.05.023.
Murphy PM, Modi P, Rahamim J, Wheatley T, Lewis SJ. An investigation into the current peri-operative nutritional management of oesophageal carcinoma patients in major carcinoma centres in England. Ann R Coll Surg Engl. 2006;88:358–62. https://doi.org/10.1308/003588406x106522.
Schandl A, Johar A, Anandavadivelan P, Vikstrom K, Malberg K, Lagergren P. Patient-reported outcomes 1 year after oesophageal cancer surgery. Acta Oncologica. 2020: 1–7; https://doi.org/10.1080/0284186x.2020.1741677.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J chronic Dis. 1987;40:373–83.
Greene FL, Sobin LH. A worldwide approach to the TNM staging system: collaborative efforts of the AJCC and UICC. J Surg Oncol. 2009;99:269–72. https://doi.org/10.1002/jso.21237.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Likert R. A technique for the measurement of attitudes. Arch Psychol. 1932;22:55–55.
Abbott J, Teleni L, McKavanagh D, Watson J, McCarthy AL, Isenring E. Patient-Generated Subjective Global Assessment Short Form (PG-SGA SF) is a valid screening tool in chemotherapy outpatients. Support Care Cancer. 2016;24:3883–7. https://doi.org/10.1007/s00520-016-3196-0.
Douven I. A Bayesian perspective on Likert scales and central tendency. Psychonomic Bull Rev. 2018;25:1203–11. https://doi.org/10.3758/s13423-017-1344-2.
Arends J, Bachmann P, Baracos V, Barthelemy N, Bertz H, Bozzetti F, et al. ESPEN guidelines on nutrition in cancer patients. Clin Nutr. 2016. https://doi.org/10.1016/j.clnu.2016.07.015.
Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260:1743–8.
Bleich SN, Ozaltin E, Murray CK. How does satisfaction with the health-care system relate to patient experience? Bull World Health Organ. 2009;87:271–8.
Soriano TT, Eslick GD, Vanniasinkam T. Long-term nutritional outcome and health related quality of life of patients following esophageal cancer surgery: a meta-analysis. Nutr Cancer. 2018;70:192–203. https://doi.org/10.1080/01635581.2018.1412471.
Heneghan HM, Zaborowski A, Fanning M, McHugh A, Doyle S, Moore J, et al. Prospective study of malabsorption and malnutrition after esophageal and gastric cancer surgery. Ann Surg. 2015;262:803–7. https://doi.org/10.1097/SLA.0000000000001445. Discussion 807-808.
Huerter ME, Charles EJ, Downs EA, Hu Y, Lau CL, Isbell JM, et al. Enteral access is not required for esophageal cancer patients undergoing neoadjuvant therapy. Ann Thorac Surg. 2016;102:948–54. https://doi.org/10.1016/j.athoracsur.2016.03.041.
Silvers MA, Savva J, Huggins CE, Truby H, Haines T. Potential benefits of early nutritional intervention in adults with upper gastrointestinal cancer: a pilot randomised trial. Support Care Cancer. 2014;22:3035–44. https://doi.org/10.1007/s00520-014-2311-3.
Furness K, Silvers MA, Savva J, Huggins CE, Truby H, Haines T. Long-term follow-up of the potential benefits of early nutritional intervention in adults with upper gastrointestinal cancer: a pilot randomised trial. Support Care Cancer. 2017;25:3587–93. https://doi.org/10.1007/s00520-017-3789-2.
Funding
The Swedish Research Council (grant number 521-2012-2824), the Swedish Cancer Society (grant number 180685), Avtal om Läkarutbildning och Forskning (grant number ALF: LS 2018-1157), The Cancer Research Foundations of Radiumhemmet (grant number 171103).
Author information
Authors and Affiliations
Contributions
PL conceived and planned the project and developed methods for data collection and is the principal investigators of the project. PA, AW, KM, HR, AJ and PL participated in study design. AJ conducted the statistical analysis. All authors contributed to the refinement of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anandavadivelan, P., Wikman, A., Mälberg, K. et al. Role of dietitian support in improving weight loss and nutrition impact symptoms after oesophageal cancer surgery. Eur J Clin Nutr 75, 1134–1141 (2021). https://doi.org/10.1038/s41430-020-00830-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-020-00830-0