Abstract
To examine preoperative use of intravitreal dexamethasone implant in patients with refractory diabetic macular edema (DME) undergoing cataract surgery. Participants in this study were 17 patients with DME refractory to previous treatment with anti-vascular endothelial growth factor agents or dexamethasone implant, and co-existent cataract. All participants received intravitreal dexamethasone implant at baseline and underwent phacoemulsification within one month after its insertion. Best-corrected visual acuity (BCVA) and central subfield thickness (CST) changes between baseline, time of cataract surgery and postoperative months 1, 2 and 3 were evaluated. At month 1 after surgery, BCVA improved significantly from 42.3 ± 9.6 to 58.7 ± 11.9 letters compared to baseline (p < 0.001) and the improvement was sustained at month 2 and month 3 postoperatively. One month postoperatively, CST improved significantly compared to baseline (p < 0.001) and the improvement was sustained at month 2 (p < 0.001), while at month 3 CST started to increase, but remained significantly lower than baseline (p = 0.003). At month 3 postoperatively, 35.3% of patients presented recurrence of ME. Patients with refractory DME and cataract can safely undergo phacoemulsification when dexamethasone implant is inserted one month prior to surgery to ensure adequate control of postoperative inflammation and prevent deterioration of ME.
Similar content being viewed by others
Introduction
Diabetic macular edema (DME) is a common complication of diabetes mellitus, affecting about 20% of patients with diabetic retinopathy, and can lead to visual loss if left untreated1,2. Patients with diabetes mellitus seem to develop cataract more frequently and earlier compared to non-diabetic population, because of the inherent metabolic condition of the disease3,4,5. It is worthy to note that cataract surgery in diabetic patients has been associated with higher risk of complications, including postoperative macular edema (Irvine-Gass syndrome) or worsening of pre-existing DME, especially in the presence of unstable diabetic retinopathy6,7,8,9,10,11,12. In fact, it has been reported that about 22% of diabetic patients, who undergo cataract surgery, develop macular edema7.
Previous studies have shown that intravitreal injection of anti-vascular endothelial growth factor (anti-VEGF) agents or triamcinolone pre-operatively, post-operatively or at the time of phacoemulsification may reduce the development of postoperative DME, although rapid recurrence of macular edema occurred and in case of triamcinolone the risk of intraocular pressure (IOP) increase may also exist13,14,15,16,17,18,19,20,21,22.
Intravitreal dexamethasone implant (Ozurdex, Allergan) is a biodegradable corticosteroid implant, which provides sustained-release of 700 μg dexamethasone into the vitreous for up to 6 months23. It has been successfully applied for the treatment of DME, retinal vein occlusion and non-infectious posterior uveitis24,25,26. There are few studies using intravitreal dexamethasone implant to control postoperative macular edema in patients affected by DME, showing promising results27,28,29,30,31,32. Most studies reported the use of implant at the same time of cataract operation. Specifically, Panozzo et al. have found that DME occurred in 1 out of 19 patients with DME and cataract one month after surgery, and in 74% of patients at month 4–5 postoperatively, in patients who were treated with phacoemulsification and dexamethasone implant at the time of cataract operation29. Malclès et al. in their retrospective study described the application of dexamethasone implant one month before cataract surgery32.
In light of the above, the purpose of this study was to examine the anatomical and functional results in patients with refractory DME and cataract, who received intravitreal dexamethasone implant and subsequently underwent phacoemulsification one month thereafter. The rationale of the use of intravitreal dexamethasone one month prior to cataract surgery is to benefit from its peak of action, so as to prevent deterioration of DME more effectively or even improve macular edema postoperatively.
Results
Table 1 shows the demographic and clinical characteristics of our study sample. The mean age of patients was 72.3 ± 7.1 years. 8 patients (47.1%) were male and 9 (52.9%) female. The mean HbA1c was 7.3 ± 0.7% and patients had a mean duration of diabetes mellitus of 14.1 ± 5.3 years. 14 patients (82.4%) presented non-proliferative diabetic retinopathy and 3 patients (17.6%) non-active proliferative diabetic retinopathy previously treated with pan-retinal photocoagulation. Hypertension was present in 14 patients (82.4%) and hyperlipidaemia in 9 patients (52.9%). All patients had received previously at least 3 intravitreal ranibizumab injections with a mean number of 6.9 ± 5.8 injections (range: 3–25 injections), while 6 patients (35.3%) were previously treated with one intravitreal dexamethasone implant (at least 6 months before recruitment for this study) and 3 patients (17.6%) with macular focal/grid laser. Regarding the lens status, 10 patients (58.8%) had nuclear cataract, 3 patients (17.6%) cortical cataract and 4 patients (23.6%) posterior subcapsular cataract.
At baseline, the mean BCVA was 42.3 ± 9.6 letters and remained stable until cataract surgery (42.3 ± 9.4 letters). At month 1 after cataract surgery, BCVA improved significantly to 58.7 ± 11.9 letters compared to baseline (p < 0.001) and the improvement was sustained at postoperative month 2 (60.2 ± 12.1 letters, p < 0.001) and month 3 (58.9 ± 11.8 letters, p < 0.001) compared to baseline. The evolution of BCVA over time is depicted in Fig. 1A.
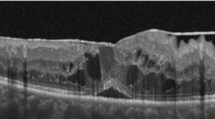
(A) Evolution of best corrected visual acuity over time. The bars represent mean±standard error. Stars show statistical significance (p < 0.05) compared to baseline. (B) Evolution of central subfield thickness over time in patients with diabetic macular edema and concurrent cataract, treated with intravitreal dexamethasone one month prior to cataract surgery. The bars represent mean±standard error. Stars show statistical significance (p < 0.05) compared to baseline.
At baseline, the mean CST was 479.3 ± 89.7 μm and improved significantly to 386.2 ± 76.9 μm one month after injection, at the day of cataract surgery (p < 0.001). At month 1 after cataract surgery, CST improved significantly to 339.1 ± 96.7 μm compared to baseline (p < 0.001) and the improvement was sustained at postoperative month 2 (342.3 ± 95.2 μm, p < 0.001 compared to baseline), while at month 3 postoperatively CST started to increase but remained significantly lower than baseline (400.8 ± 102.9 μm, p = 0.003). The evolution of CST over time is depicted in Fig. 1B. At months 1 and 2 postoperatively, all patients showed improvement or even total absorption of macular edema. Specifically, 8 out of 17 patients (47.1%) at month 1 postoperatively and 7 out of 17 patients (41.2%) at month 2 postoperatively presented total resolution of macular edema (CST < 320 μm). At postoperative month 3 (4 months after intravitreal dexamethasone implant insertion), 5 out of 17 patients (29.4%) had resolution of macular edema, while 6 out of 17 patients (35.3%) presented recurrence of macular edema, as it is detected on SD-OCT. It is worthy to note that only one out of 6 eyes with recurrent macular edema had received previous treatment with dexamethasone implant.
As far as the complications are concerned, no serious systemic side effects were reported from any of the patients in the study. No thromboembolic or cardiovascular events were mentioned. In addition, there was no inflammatory reaction, endophthalmitis or retinal tears. One patient (5.9%) had raised IOP (>35 mmHg) two months postoperatively, which was controlled with topical anti-hypertensive agents.
Discussion
The principal message of this prospective study was that intravitreal dexamethasone implant used one month prior to cataract surgery was an effective and safe strategy to deal with patients with refractory DME and concurrent cataract. Specifically, there was significant improvement in BCVA and CST postoperatively until the 3-month follow-up after surgery, without serious ocular complications, suggesting that such patients benefit from cataract surgery and did not experience deterioration of DME secondary to potential postoperative inflammation.
It is worthy to mention that CST decreased significantly one month after the implant insertion (just before scheduled cataract operation), although visual acuity remained the same, suggesting that the presence of cataract was indeed a sight limiting factor that did not allow the anatomical improvement in the fovea to be reflected in the functional outcome. Moreover, one month after cataract surgery (two months after the implant insertion) CST improved significantly further compared to baseline and to preoperative measurement, indicating that the effect of the dexamethasone not only halted worsening of macular edema due to the inflammatory process that evolves intraoperatively and at the immediate post-cataract period, but also facilitated further resolution of the edema. Furthermore, since VA improved significantly only after cataract surgery compared to baseline, we suggested that patients with DME and advanced cataract do benefit from cataract surgery, even in cases with a history of resistant DME to either anti-VEGF or dexamethasone implant.
Previous studies have shown that DME may worsen after cataract surgery8,9,10,11,12, while macular edema may also occur postoperatively in patients without previous macular impairment12. Intravitreal dexamethasone implant has been shown to have similar functional results compared to anti-VEGF agents in patients with DME, but with better anatomical response and fewer injections. Specifically, in a recent meta-analysis by He et al., intravitreal dexamethasone implant presented superior anatomic outcomes in 6 months with mean CST reduction of about 87 μm compared to anti-VEGF treatment (mean CST reduction of about 34 μm), similar to our results showing about 80 μm reduction of CST at month 3 postoperatively and 4 months after intravitreal dexamethasone implant33. In addition, the benefit of intravitreal dexamethasone implant in DME reached its peak at 4–8 weeks after insertion23, being a reasonable option in patients with DME and concurrent cataract, since it covers the time interval of presumed postoperative inflammatory reaction, apart from facilitating the resolution of pre-existing macular edema29.
Following the evolution of CST in our study, we have noticed that the maximum action of dexamethasone implant occurred at month 1 postoperatively, about 60 days after dexamethasone implant insertion. This can be explained based on the pharmacodynamics of the drug, showing that the mean reduction in CST reaches its highest point when dexamethasone reaches its highest concentration, happening about 30–60 days after implant23. This was also the time where the maximum increase in VA occurred, which can be attributed both to the cataract extraction and to the thinner CST, which can justify our initial hypothesis to insert the implant one month before surgery to maximize its protective role on macular edema. At month 3 postoperatively (four months after the implant injection), CST started to increase as the effect of the drug wears off, which is in accordance with the duration of action of the implant23,24,34. At that time recurrence of macular edema occurred in 35% of cases suggesting that re-insertion of dexamethasone implant may be needed. Accordingly, BCVA was significantly improved at month 1 after surgery and remained stable till the end of the follow-up, suggesting that patients with sight-limiting cataract may benefit from surgery, even in the presence of DME.
Regarding the optimal time of intravitreal dexamethasone implant insertion in patients with DME and cataract, there are various approaches. Previous studies have used dexamethasone implant either at the beginning or immediately after surgery in an attempt to prevent or control postoperative macular edema27,28,29,30,31,35. Agarwal et al. used intravitreal dexamethasone implant in 18 eyes with DME and cataract, at the beginning of phacoemulsification, reporting 15–18 letters gain in visual acuity compared to stable visual acuity in controls associated with a decrease in CMT35, while Sze et al. also showed improvement in BCVA and CST using dexamethasone implant just before initiation of cataract surgery, but about 10% of patients required further treatment due to recurrence of macular edema in about 21 weeks post-operation28. Other authors preferred to insert the intravitreal dexamethasone implant at the end of the surgery, when potential intraoperative complications were overcome and a better visualization of the implant in the vitreous was possible, also demonstrated good anatomical and functional outcomes27,29,30,31. In our study, however, about 35% of patients presented recurrent macular edema 3 months postoperatively, suggesting that re-insertion of dexamethasone implant may be needed. The discrepancy of our results and those of previous studies could be potentially attributed to the variation of population, to the difference in macular edema specific features and probably to the difference in the timing of implant insertion.
An interesting point that should be taken into account pertains to the distinction between DME and postoperative macular edema (Irvine-Gass syndrome), which is challenging in such patients. However, the incidence of Irvine-Gass syndrome after modern phacoemulsification is very low, ranging between 0.1–2.4%, although it is reported to be much higher in diabetic patients reaching 20%7,12,36. Moreover, in the majority of cases, Irvine-Gass syndrome occur between 4–10 weeks postoperatively, which is shorter than the mean time of recurrence of macular edema both in our study and in previous reports37,38, while other studies supported that the inflammatory signal process after cataract surgery is believed to be short-lived and macular edema may develop in as little as 1 month after surgery30,39. By inserting the implant one month prior to cataract surgery, the peak action of the drug (30–60 days) and duration of action of the drug (roughly 4 months) can theoretically control more effectively both diabetic macular edema and Irvine-Gass syndrome, especially in cases where either or both of them occurred within the first month after cataract surgery, as previously reported7,30,39.
This study reports the pre-operative use of intravitreal dexamethasone implant within one month prior to surgery to halt progression of macular edema postoperatively, showing improvement in BCVA and CST at the 3-month follow-up after surgery. Although we acknowledge the fact that an additional surgical procedure is needed if dexamethasone implant was inserted one month pre-operatively, a better timing for control of postoperative inflammation is ensured. A safer implant injection was also guaranteed, since insertion either at the beginning or at the end of the cataract procedure has potential risks. Specifically, if the implant is inserted at the beginning of cataract surgery, the surgeon has to remove the implant in case of posterior capsule rupture, to eliminate the possibility of its migration into the anterior chamber and its damaging effect on the cornea30. On the other hand, if the implant is inserted at the end of cataract surgery, there might be a risk of potential hazardous manipulations to the globe and to the anterior chamber stability that can endanger cataract surgery outcome28.
Potential limitations of the study were the small sample size and the lack of control group, but one should take into consideration ethical issues to recruit patients as controls and perform no treatment to DME. In addition, we did not included data on the parameters of phacoemulsification, which could help to estimate a correlation between the amount of energy used during surgery and postoperative retinal thickness. Nevertheless, the strengths of this study include the prospective design and the use of SD-OCT to detect macular edema.
In conclusion, this study demonstrated promising anatomical and functional results in cataract patients with DME, treated with intravitreal dexamethasone implant one month prior to scheduled cataract extraction, although it should be taken into account that this is a study without control group. Further studies with larger study sample and longer follow-up are needed to confirm further the pre-operative use of intravitreal dexamethasone implant in the treatment of DME patients undergoing cataract surgery.
Methods
This is a prospective study, which was conducted at the Korgialenio Benakio Hospital, Athens, Greece. Participants in the study were 17 patients (17 eyes) with type 2 diabetes mellitus and DME refractory to previous treatment with anti-VEGF agents or dexamethasone implant, who had co-existent cataract. Specifically, all participants had refractory DME to the affected eye (central subfield thickness – CST > 320 μm), which had been previously treated with at least 3 intravitreal ranibizumab injections or one dexamethasone implant, showing no response, defined as reduction in CST less than 50 μm. Patients with macular edema secondary to causes other than diabetes mellitus, patients with active proliferative diabetic retinopathy (PDR), ocular inflammation and advanced glaucoma were excluded from the study. The study was in accordance with the Tenets of Helsinki Declaration and was approved by the institutional review board of Red Cross “Korgialenio-Benakio” Hospital. Written informed consent was obtained from all participants before enrollment to the study.
All participants underwent a complete ophthalmic examination at baseline (before intravitreal dexamethasone implant insertion), including best corrected visual acuity (BCVA) measurement by means of ETDRS letters chart, slit-lamp examination, IOP measurement, dilated fundoscopy and spectral-domain optical coherence tomography to measure CST using Spectralis (SD-OCT; Spectralis HRA-OCT, Heidelberg Engineering, Heidelberg, Germany).
At the diagnosis of DME (baseline), all participants received intravitreal dexamethasone implant, which was performed under sterile protocol, which included the use of 5% povidone-iodine solution, topical anesthesia, eyelid-speculum application, intravitreal injection of 0.7 mg dexamethasone implant via pars plana in the infero-temporal quadrant at 4 mm from the limbus, followed by post-injection topical antibiotic eye-drops medication.
All patients underwent a standard uncomplicated phacoemulsification with posterior chamber intraocular lens (IOL) implantation under topical anesthesia, within one month after dexamethasone implant insertion, where BCVA, IOP and CST were also measured. Thereafter, we assessed BCVA, IOP and CST in all patients monthly postoperatively for at least 3 months. The main outcomes were BCVA and CST changes between baseline (dexamethasone implant insertion), time of cataract surgery and months 1, 2 and 3 post-cataract extraction. Safety was evaluated by documenting intraoperative or postoperative complications, changes in IOP, the use of IOP-lowering agents and any patient-reported or investigator-reported adverse events.
Statistical analysis was performed using SPSS 17.0 (SPSS Inc, Chicago, IL, USA). For the description of patients’ characteristics at baseline, mean ± standard deviation (SD) was used for continuous variables and counts with percentages for categorical variables. Shapiro-Wilk test was used to check the normality of variables. For longitudinal comparisons of BCVA and CST between baseline and each time point, the Wilcoxon matched-pairs signed-ranks test was used, since there was deviation from normality; given that four comparisons were done, the level of statistical significance was set at 0.05/4 = 0.012, according to the Bonferroni correction. A p value <0.05 was considered statistically significant, apart from cases where the Bonferroni correction was adopted, as declared above40.
References
Yau, J. et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care 35, 556–564 (2012).
Treatment techniques and clinical guidelines for photocoagulation of diabetic macular edema. Early Treatment Diabetic Retinopathy Study Report Number 2. Early Treatment Diabetic Retinopathy Study Research Group. Ophthalmology 94, 761–774 (1987).
Klein, B. et al. Incidence of cataract surgery in the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Am J Ophthalmol 119, 295–300 (1995).
Klein, B. E., Klein, R., Wang, Q. & Moss, S. E. Older-onset diabetes and lens opacities. The Beaver Dam Eye Study. Ophthalmic Epidemiol 2, 49–55 (1995).
Chan, A. W., Ho, Y. S., Chung, S. K. & Chung, S. S. Synergistic effect of osmotic and oxidative stress in slow-developing cataract formation. Exp Eye Res 87, 454–461 (2008).
Haddad, N. M., Sun, J. K., Abujaber, S., Schlossman, D. K. & Silva, P. S. Cataract surgery and its complications in diabetic patients. Semin Ophthalmol 29, 329–337 (2014).
Kim, S. J., Equi, R. & Bressler, N. M. Analysis of macular edema after cataract surgery in patients with diabetes using optical coherence tomography. Ophthalmology 114, 881–889 (2007).
Diabetic Retinopathy Clinical Research Network Authors/Writing Committee. Macular edema after cataract surgery in eyes without preoperative central-involved diabetic macular edema. JAMA Ophthalmol 131, 870–879 (2013).
Dowler, J. G., Sehmi, K. S., Hykin, P. G. & Hamilton, A. M. The natural history of macular edema after cataract surgery in diabetes. Ophthalmology 106, 663–668 (1999).
Sadiq, S. A., Sleep, T. & Amoaku, W. M. The visual results and changes in retinopathy in diabetic patients following cataract surgery. Eur J Ophthalmol 9, 14–20 (1999).
Denniston, A. K. et al. The UK Diabetic Retinopathy Electronic Medical Record (UK DR EMR) Users Group, Report 2: real-world data for the impact of cataract surgery on diabetic macular oedema. Br J Ophthalmol 101, 1673–1678 (2017).
Chu, C. J. et al. Risk Factors and Incidence of Macular Edema after Cataract Surgery: A Database Study of 81984 Eyes. Ophthalmology 123, 316–323 (2016).
Takamura, Y., Kubo, E. & Akagi, Y. Analysis of the effect of intravitreal bevacizumab injection on diabetic macular edema after cataract surgery. Ophthalmology 116, 1151–1157 (2009).
Wahab, S. & Ahmed, J. Management of cataract with macular oedema due to diabetes mellitus type-II and hypertension with grid laser prior to surgery and intra-vitreal bevacizumab (Avastin) peroperatively. J Pak Med Assoc 60, 836–839 (2010).
Udaondo, P., Garcia-Pous, M., Garcia-Delpech, S., Salom, D. & Diaz-Llopis, M. Prophylaxis of macular edema with intravitreal ranibizumab in patients with diabetic retinopathy after cataract surgery: a pilot study. J Ophthalmol 2011, 159436 (2011).
Salehi, A., Beni, A. N., Razmjoo, H. & Beni, Z. N. Phacoemulcification with intravitreal bevacizumab injection in patients with cataract and coexisting diabetic retinopathy: prospective randomized study. J Ocul Pharmacol Ther 28, 212–218 (2012).
Chae, J. B. et al. Effect of combined cataract surgery and ranibizumab injection in postoperative macular edema in nonproliferative diabetic retinopathy. Retina 34, 149–156 (2014).
Yumuşak, E. & Örnek, K. Comparison of Perioperative Ranibizumab Injections for Diabetic Macular Edema in Patients Undergoing Cataract Surgery. J Ophthalmol 2016, 7945619 (2016).
Rauen, P. I. et al. Intravitreal injection of ranibizumab during cataract surgery in patients with diabetic macular edema. Retina 32, 1799–1803 (2012).
Ozgur, O. R., Ozkurt, Y., Kulekci, Z. & Evciman, T. The combination of phacoemulsification surgery and intravitreal triamcinolone injection in patients with cataract and diabetic macular edema. Saudi J Ophthalmol 30, 33–38 (2016).
Lim, L. L. et al. Diabetic Macular Edema at the time of Cataract Surgery trial: a prospective, randomized clinical trial of intravitreous bevacizumab versus triamcinolone in patients with diabetic macular oedema at the time of cataract surgery - preliminary 6 month results. Clin Exp Ophthalmol 44, 233–242 (2016).
Tatsumi, T. et al. Comparison of the Efficacy of Sub-Tenon versus Intravitreal Triamcinolone Acetonide Injection during Cataract Surgery for Diabetic Macular Edema. Ophthalmologica 241, 17–23 (2019).
Chang-Lin, J. E. et al. Pharmacokinetics and pharmacodynamics of a sustained-release dexamethasone intravitreal implant. Invest Ophthalmol Vis Sci 52, 80–86 (2011).
Boyer, D. S. et al. Three-year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology 121, 1904–1914 (2014).
Haller, J. A. et al. Dexamethasone intravitreal implant in patients with macular edema related to branch or central retinal vein occlusion twelve-month study results. Ophthalmology 118, 2453–2460 (2011).
Lowder, C. et al. Dexamethasone intravitreal implant for noninfectious intermediate or posterior uveitis. Arch Ophthalmol 129, 545–553 (2011).
Furino, C., Boscia, F., Recchimurzo, N., Sborgia, C. & Alessio, G. Intravitreal dexamethasone implant for macular edema following uncomplicated phacoemulsification. Eur J Ophthalmol 24, 387–391 (2014).
Sze, A. M., Luk, F. O., Yip, T. P., Lee, G. K. & Chan, C. K. Use of intravitreal dexamethasone implant in patients with cataract and macular edema undergoing phacoemulsification. Eur J Ophthalmol 25, 168–172 (2015).
Panozzo, G. A., Gusson, E., Panozzo, G. & Dalla Mura, G. Dexamethasone intravitreal implant at the time of cataract surgery in eyes with diabetic macular edema. Eur J Ophthalmol 27, 433–437 (2016).
Calvo, P., Ferreras, A., Al Adel, F., Dangboon, W. & Brent, M. H. Effect of an intravitreal dexamethasone implant on diabetic macular edema after cataract surgery. Retina 38, 490–496 (2018).
Furino, C. et al. Combined Phacoemulsification and Intravitreal Dexamethasone Implant (Ozurdex®) in Diabetic Patients with Coexisting Cataract and Diabetic Macular Edema. J Ophthalmol 2017, 4896036 (2017).
Malclès, A. et al. Real-life study in diabetic macular edema treated with dexamethasone implant: The Reldex Study. Retina 37, 753–760 (2017).
He, Y., Ren, X. J., Hu, B. J., Lam, W. C. & Li, X. R. A meta-analysis of the effect of a dexamethasone intravitreal implant versus intravitreal anti-vascular endothelial growth factor treatment for diabetic macular edema. BMC Ophthalmol 18, 121 (2018).
Bonfiglio, V. et al. Widening use of dexamethasone implant for the treatment of macular edema. Drug Des Devel Ther 11, 2359–2372 (2017).
Agarwal, A., Gupta, V., Ram, J. & Gupta, A. Dexamethasone intravitreal implant during phacoemulsification. Ophthalmology 120, 211 (2013).
Khurana, R. N., Palmer, J. D., Porco, T. C. & Wieland, M. R. Dexamethasone intravitreal implant for pseudophakic cystoid macular edema in patients with diabetes. Ophthalmic Surg Lasers Imaging Retina 46, 56–61 (2015).
Gass, J. D. & Norton, E. W. Cystoid macular edema and papilledema following cataract extraction. A fluorescein fundoscopic and angiographic study. Arch Ophthalmol 76, 646–661 (1966).
Norregaard, J. C. et al. Intraoperative clinical practice and risk of early complications after cataract extraction in the United States, Canada, Denmark, and Spain. Ophthalmology 106, 42–48 (1999).
Kim, S. J. & Jampel, H. Prevention of Cystoid Macular Edema After Cataract Surgery in Non-Diabetic and Diabetic Patients: A Systematic Review and Meta-Analysis. Am J Ophthalmol 161, 221–222 (2016).
Chatziralli, I. et al. Dexamethasone Intravitreal Implant in Diabetic Macular Edema: Real-Life Data from a Prospective Study and Predictive Factors for Visual Outcome. Diabetes Ther 8, 1393–1404 (2017).
Acknowledgements
The publication fee of this article was funded by Allergan PLC. Allergan had no involvement in the content of this article.
Author information
Authors and Affiliations
Contributions
S.K. conceived and designed the study, collected data, analyzed and interpreted data, drafted and critically revised the manuscript; T.X. collected data; E.B. collected data; I.G. collected data; D.V. collected data; G.B. collected data; I.C. designed the study, collected data, analyzed and interpreted data, drafted and critically revised the manuscript. All authors are in agreement with the current version of the manuscript and approved the accuracy and integrity of the presented data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kabanarou, S.A., Xirou, T., Boutouri, E. et al. Pre-operative intravitreal dexamethasone implant in patients with refractory diabetic macular edema undergoing cataract surgery. Sci Rep 10, 5534 (2020). https://doi.org/10.1038/s41598-020-62561-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-62561-3
This article is cited by
-
Real-world experience on intravitreal dexamethasone implant in patients with macular edema scheduled to undergo cataract surgery
BMC Ophthalmology (2023)
-
Mid-term safety and effectiveness of macular peeling one month after intravitreal dexamethasone implant for tractional diabetic macular edema
Scientific Reports (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.